Professional Documents
Culture Documents
Nursing Care Plan For Stroke Patients
Uploaded by
_cezca_85%(89)85% found this document useful (89 votes)
261K views7 pages.,this is a sample nursing care plan for patients with cerebral infarction (stroke). I have used this is our case study presentation (individual). It consist of 3 nursing care plan. Check it out!,
Original Title
Nursing Care Plan for stroke patients
Copyright
© Attribution Non-Commercial (BY-NC)
Available Formats
DOC, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Document.,this is a sample nursing care plan for patients with cerebral infarction (stroke). I have used this is our case study presentation (individual). It consist of 3 nursing care plan. Check it out!,
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOC, PDF, TXT or read online from Scribd
85%(89)85% found this document useful (89 votes)
261K views7 pagesNursing Care Plan For Stroke Patients
Uploaded by
_cezca_.,this is a sample nursing care plan for patients with cerebral infarction (stroke). I have used this is our case study presentation (individual). It consist of 3 nursing care plan. Check it out!,
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOC, PDF, TXT or read online from Scribd
You are on page 1of 7
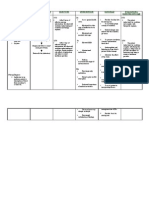
NURSING CARE PLAN
ASSESSMENT NURSING INFERENCE PLANNING INTERVENTION RATIONALE EVALUATION
DIAGNOSIS
Subjective: > Impaired bed Trauma After the rotation determine To identify After the rotation
mobility related (slipping) and nursing diagnoses that causative/ and nursing
“Hindi siya to pain secondary intervention the contribute to contributing intervention the
makatagilid to bone fracture at significant other immobility (e.g. factors. significant other
sumasakit daw musculoskeletal pelvic bone of the patient fractures, of the patient
ung bali niya sa impairment. will: hemi/para/tetra/q will:
may bewang Disruptions of uadripegia)
kapag periosteum and a. Verbalize Note individual a. Verbalize
gumagalaw” as blood vessels understanding risk factors and understanding
verbalized by the of the current situation, of the
sn of the patient. Destruction if situation /risk such pain, age, situation /risk
tissue factors, general factors,
Objective: individual weakness, individual
Bleeding occurs therapeutic debilitation therapeutic
Impaired regimen and Determine regimen and
ability to turn Pain safety perceptual/ safety
side to side measures. cognitive measures.
Impaired Impaired bed b. Demonstrate impairment to b. Demonstrate
ability to mobility techniques/ follow directions techniques/
move from behaviors that Determine To assess behaviors that
supine to will enable functional level patients will enable
sitting vise safe classification functional safe
versa. repositioning ability repositioning
(+) presence c. Maintain Note presence of c. Maintain
of pelvic position of complications position of
fracture function and related to function and
(+) General skin integrity immobility skin integrity
of the patient of the patient
weakness Observe skin for To reduce
Tremors as evidenced friction, as evidenced
reddened
noted on left by absence of maintain safe by absence of
areas/shearing.
arm and contractures, skin/tissue contractures,
Provide
hands foot drop, pressures and foot drop,
appropriate
decubitus, etc. wick away decubitus, etc.
pressure to relief
moisture
Provide regular To prevent
skin care if complications
appropriate
Assist with To promote
activities of optimal level
hygiene, of functioning
toileting,
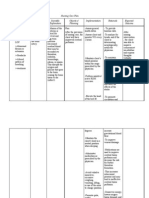
ASSESSMENT NURSING INFERENCE PLANNING INTERVENTION RATIONALE EVALUATION
DIAGNOSIS
Subjective: > Impaired Hypertension After the Determine To identify After the rotation
physical ˇ rotation and diagnosis that causative/ and nursing
“Hindi na mobility related Occlusion within nursing contributes to contributing intervention the
makagalaw si to vessels of the brain intervention the immobility factors. patient will:
nanay simula Neuromuscular parenchyma patient will: (e.g. fractures,
nung na-stroke impairment ˇ hemi/ para/ c. Maintain
siya ” as Disruption of blood a. Maintain tetra/ position and
verbalize by the supply in the brain position and quadriplegia) function and
son of the patient area function and Assess skin integrity
ˇ skin nutritional as evidenced
Obective: Tissue and cell integrity as status and S/O by absence of
necrosis evidenced others report of contractures,
(+) General ˇ by absence energy level. foot drop,
body Destruction of of Determine To assess decubitus and
weakness Neuromuscular contractures, degree of functional so forth.
Tremors junctions foot drop, immobility in ability d. S/O will
noted on left ˇ decubitus relation to demonstrate
arm and Interruption in and so forth. functional level techniques/
hands transportation of b. S/O will scale behaviors that
Inability to electrical impulses to demonstrate Assist or have To prevent will enable
perform the neuromuscular techniques/ significant complication safe
gross/fine receptors behaviors other reposition repositioning
motor skills ˇ that will client on a
(+) Paralysis MYALGIA/QUADRI enable safe regular
of left side of OR HEMIPLEGIA repositionin schedule (turn
the body g to side every 2
functional hours) as
level scale: ordered by the
4 (does not physician
participate in Provides safety To provide
activity) measures (side safety
rails up, using
pillows to
support body
part)
Encourage Enhances
patient’s S/O’s commitment
involvement in to plan
decision optimizing
making as outcomes
much as
possible
Involve S/O in To impart
care, assisting health
them to learns teaching.
ways of
managing
problems of
immobility.
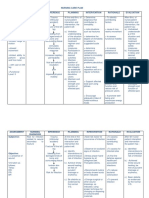
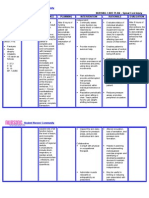
ASSESSMENT NURSING INFERENCE PLANNING INTERVENTION RATIONALE EVALUATION
DIAGNOSIS
Subjective: Self care deficit : Hypertension After the rotation Provide enteric To meet After the rotation
“Simula nung na hygiene, ˇ and nursing nutrition VIA patient’s need and nursing
i-stroke si nanay, dressing and Occlusion within interventions. The NG Tube for an interventions.
na bedridden na grooming, vessels of the patient should: feeding. High adequate The patient
siya feeding and brain a. meet all fowlers for at nutritional should:
toileting related parenchyma therapeutic self least 15 intake. f. meet all
Objective: to ˇ care demands in minutes after therapeutic
(+) NGT insertion Neuromuscular Disruption of a complete feeding. self care
impairment blood supply in absence of self Careful I/O To establish demands in a
Patient is unable the brain area care agency Monitoring and careful complete
to: ˇ b. ABSENCE OF apply necessary assessment on absence of
[HYGIENE] Tissue and cell S&S OF dietary patients fluid self care
Access and necrosis NUTRITIONAL restrictions and agency
prepare bath ˇ DEFICIT. electrolyte g. ABSENCE
supplies Destruction of [Adequate . balance. OF S&S OF
Wash body Neuromuscular nutritional Change To prevent NUTRITION
Control junctions intake] position at least decubitus AL DEFICIT.
washing ˇ c. GOOD SKIN ONCE every ulcerations. [Adequate
mediums Interruption in TURGOR, two hours or nutritional
[DRESSING transportation of NORMAL more often intake]
AND electrical URINE when needed. h. GOOD SKIN
GROOMING] impulses to the OUTPUT, Provide To protect the TURGOR,
Obtain neuromuscular ABSENCE OF padding for the patient’s skin NORMAL
articles for receptors EDEMA, elbows, needs, integrity URINE
clothing ˇ HYPER AND ankles and maintaining OUTPUT,
Put on clothes MYALGIA/QUA HYPOVOLEMI other areas for his first line ABSENCE
DRI OR A [Fluid and possible skin of defense OF EDEMA,
Maintain
HEMIPLEGIA Electrolyte abrasion. against HYPER AND
appearance at
balance] sickness and HYPOVOLE
an acceptable
d. ABSENCE OF infection. MIA [Fluid
level
DECUBITUS An adult diaper To prevent and
[FEEDING]
ULCERS AND should be soiling of bed Electrolyte
Prepare/obtain FOUL ODORS balance]
food for WORN at all sheets,
IN BETWEEN times. Change clothes and i. ABSENCE
ingestion LINENS/CLOT OF
Handle the diaper as linens
HING AND soon as patient providing DECUBITUS
utensils SKIN [Clean, ULCERS
defecated. maximum
Bring food to Intact skin and AND FOUL
comfort and
mouth mucus ODORS IN
prevention of
Chew and membrane] skin irritation BETWEEN
swallow up e. ABSENCE OF if feces LINENS/CL
food ABDOMINAL remain in OTHING
Pick up food AND contact with AND SKIN
[TOILETING] BLADDER the patient’s [Clean, Intact
Go to the toilet DISTENTION, skin for a skin and
RECTAL long time. mucus
FULLNESS Promote an To conserve membrane]
AND Environment energy j. ABSENCE
PRESSURE, conducive to promoting OF
PAIN IN rest and rest and ABDOMINA
DEFECATION [ recovery. recovery. L AND
Meeting toileting Decrease BLADDER
demands ] stimuli and DISTENTIO
Metabolic N, RECTAL
demand of the FULLNESS
body. AND
Passive ROM This is to PRESSURE,
Exercises Early improve PAIN IN
morning once a circulation, DEFECATIO
day, 10 times reducing the N [ Meeting
targeting both risk of toileting
upper and atheromatous demands ]
lower formation.
extremities.
> Lastly, Do health 10. To educate
teaching when S/O the S/O what
is at the optimum factors have
level to receive contributed to the
information. client’s illness
and educating
them to decrease,
if not totally
eliminate those
contributory
factors to prevent
recurrence of the
disease and
promote change
for a healthy
lifestyle.
You might also like
- NCP (Impaired Physical Mobility)Document1 pageNCP (Impaired Physical Mobility)soclose0488% (26)
- Cerebrovascular Accident Nursing Care PlanDocument4 pagesCerebrovascular Accident Nursing Care PlanCyrus De Asis67% (12)
- Nursing Care Plans CVADocument6 pagesNursing Care Plans CVANicole Palarca92% (12)
- Impaired Verbal CommunicationDocument4 pagesImpaired Verbal CommunicationKM95% (19)
- NCP - Head InjuryDocument3 pagesNCP - Head Injurykaheliyala94% (33)
- Impaired Physical Mobility NCPDocument2 pagesImpaired Physical Mobility NCPMick De Leon67% (3)
- Nursing Care Plans of A Patient With StrokeDocument15 pagesNursing Care Plans of A Patient With StrokeJoy JarinNo ratings yet
- Dementia Nursing Care PlanDocument2 pagesDementia Nursing Care Planmp175767% (3)
- Nursing Care Plan - Spinal Cord InjuryDocument2 pagesNursing Care Plan - Spinal Cord Injuryderic92% (36)
- Nursing Care PlanDocument4 pagesNursing Care PlanJoy Callo100% (2)
- NCP For CVADocument18 pagesNCP For CVAmolukas101100% (6)
- NCP Cva Impaired Physical MobilityDocument2 pagesNCP Cva Impaired Physical Mobilityexcel2112180% (5)
- Impaired Verbal CommunicationDocument3 pagesImpaired Verbal CommunicationDesiree Deleon Guerrero0% (2)
- Anatomy and Physiology of CVADocument4 pagesAnatomy and Physiology of CVAKimsha ConcepcionNo ratings yet
- Impaired Verbal CommunicationDocument1 pageImpaired Verbal Communicationdana100% (3)
- Activity Intolerance NCPDocument7 pagesActivity Intolerance NCPMariquita BuenafeNo ratings yet
- NCP Head InjuryDocument3 pagesNCP Head InjuryAngel Mae Alsua100% (2)
- NCP CVDDocument5 pagesNCP CVDaejel1889% (9)
- Spinal Cord Injury NCPDocument2 pagesSpinal Cord Injury NCPEmmanuelRodriguez100% (1)
- CystoclysisDocument29 pagesCystoclysisKate PedzNo ratings yet
- Post Stroke Scalp AcupunctureDocument64 pagesPost Stroke Scalp AcupunctureJosé Mário91% (11)
- Impaired Physical MobilityDocument2 pagesImpaired Physical Mobilitybambem aevan100% (1)
- Assessment Nursing Diagnosis Scientific Explanation Goal of Care Intervention Rationale EvaluationDocument4 pagesAssessment Nursing Diagnosis Scientific Explanation Goal of Care Intervention Rationale EvaluationHowel CristobalNo ratings yet
- Nursing Care Plan CVADocument4 pagesNursing Care Plan CVAhermesdave175% (4)
- NCP For StrokeDocument4 pagesNCP For StrokeJASON OGALESCONo ratings yet
- NCP CvaDocument4 pagesNCP CvamannyV1990100% (1)
- NCP - BedriddenDocument4 pagesNCP - Bedriddenadelaigner_racho589475% (4)
- Nursing Care Plan TBIDocument5 pagesNursing Care Plan TBIChester Manalo87% (15)
- NCP StrokeDocument7 pagesNCP StrokeMonica Gagarin Cortez100% (1)
- Nursing Care Plan (CVA)Document2 pagesNursing Care Plan (CVA)Mel Rodolfo50% (2)
- Cva NCPDocument2 pagesCva NCPAkima Mulok0% (1)
- CVA NCPDocument3 pagesCVA NCPpaulaNo ratings yet
- Gender Dysphoria NCPDocument1 pageGender Dysphoria NCPSeann LorescoNo ratings yet
- NCP AneurysmDocument4 pagesNCP AneurysmJanielle Christine Monsalud100% (1)
- NCP CvaDocument3 pagesNCP CvaJey PangilinanNo ratings yet
- Stroke Nursing Care PlanDocument1 pageStroke Nursing Care PlanTracy PearlNo ratings yet
- Ncp-Impaired Verbal CommunicationDocument4 pagesNcp-Impaired Verbal CommunicationEzra TuanNo ratings yet
- Impaired Verbal CommunicationDocument3 pagesImpaired Verbal CommunicationChenee Mabulay100% (1)
- Assessment Diagnosis Planning Implementation Evaluation No Subjective Cues ObjectiveDocument3 pagesAssessment Diagnosis Planning Implementation Evaluation No Subjective Cues ObjectiveMaverick LimNo ratings yet
- Nursing Care PlanDocument22 pagesNursing Care PlanjamNo ratings yet
- NCP Impaired Physical Mobility-2Document4 pagesNCP Impaired Physical Mobility-2ejoanbNo ratings yet
- NCP - Tissue Perfusion (Cerebral)Document2 pagesNCP - Tissue Perfusion (Cerebral)moodlayers50% (6)
- Nursing Care Plan For Post Thyroidectomy and CholecystectomyDocument9 pagesNursing Care Plan For Post Thyroidectomy and Cholecystectomyirish m magracia100% (7)
- CVA-NCPDocument7 pagesCVA-NCPAiza Oronce0% (1)
- Nursing Care Plan SeizureDocument2 pagesNursing Care Plan Seizuretimie_reyes100% (1)
- (NCPS) Impaired Physical Mobility 2Document2 pages(NCPS) Impaired Physical Mobility 2roren100% (1)
- Nursing Care Plan Assessment Nursing Diagnosis Inference Planning Intervention Rationale Evaluation SubjectiveDocument2 pagesNursing Care Plan Assessment Nursing Diagnosis Inference Planning Intervention Rationale Evaluation SubjectiveGaurav GaikwadNo ratings yet
- Nursing Care Plan Assessment Nursing Diagnosis Inference Planning Intervention Rationale Evaluation SubjectiveDocument2 pagesNursing Care Plan Assessment Nursing Diagnosis Inference Planning Intervention Rationale Evaluation SubjectiveDat boiNo ratings yet
- Nursing Care Plan Assessment Nursing Diagnosis Inference Planning Intervention Rationale Evaluation SubjectiveDocument2 pagesNursing Care Plan Assessment Nursing Diagnosis Inference Planning Intervention Rationale Evaluation SubjectiveGaurav Gaikwad100% (3)
- Actual Nursing Care PlanDocument2 pagesActual Nursing Care Planshaileene bugayongNo ratings yet
- Nursing Care Plan: Short Term: Independent: Independent: Short TermDocument6 pagesNursing Care Plan: Short Term: Independent: Independent: Short TermSittie Sobaidah D. DimakutaNo ratings yet
- NCP - Risk For FallsDocument5 pagesNCP - Risk For FallsMae CeaesarNo ratings yet
- Nursing Care PlanDocument1 pageNursing Care Planapi-446022560No ratings yet
- Assessment Nursing Diagnosis Planning Intervention Rationale EvaluationDocument3 pagesAssessment Nursing Diagnosis Planning Intervention Rationale EvaluationKristine CastilloNo ratings yet
- NCP (BD)Document5 pagesNCP (BD)Nursing LectureNo ratings yet
- Student Nurses' Community: Nursing Care Plan AmputationDocument3 pagesStudent Nurses' Community: Nursing Care Plan AmputationNur faizah bt azmiNo ratings yet
- Nursing Care Plan: Cues Nursing Diagnosis Objective Intervention Rationale EvaluationDocument2 pagesNursing Care Plan: Cues Nursing Diagnosis Objective Intervention Rationale Evaluationmyer pasandalanNo ratings yet
- NCPDocument2 pagesNCPsphinx809100% (2)
- NCP 1 Ortho IMMOBILITYDocument1 pageNCP 1 Ortho IMMOBILITYAndrea Sibayan Soriano100% (1)
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument3 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationEllee HadesNo ratings yet
- Nursing Care PlanDocument1 pageNursing Care Planmhefistto_2210No ratings yet
- Cebu Institute of Technology - University College of NursingDocument2 pagesCebu Institute of Technology - University College of NursingSergi Lee OrateNo ratings yet
- Upload - PDs - 35717-KPI Guide For StaffDocument5 pagesUpload - PDs - 35717-KPI Guide For StaffBilal Salameh100% (1)
- Biopharmaceutical: What Is A ?Document6 pagesBiopharmaceutical: What Is A ?NarendrakumarNo ratings yet
- Cardiology BrochureDocument2 pagesCardiology Brochureong251183No ratings yet
- Curriculum Vitae MTDocument6 pagesCurriculum Vitae MTapi-273097827No ratings yet
- The Complete Guide To Weight Loss and FitnessDocument4 pagesThe Complete Guide To Weight Loss and FitnessOnika BoteroNo ratings yet
- Vivek Swaroop GautamDocument2 pagesVivek Swaroop GautamSrujana M0% (1)
- OB AssessmentDocument3 pagesOB AssessmentJoshua D ParkerNo ratings yet
- CD ListDocument80 pagesCD ListOFC accountNo ratings yet
- Liver Cancer Pathophysiology: Predisposing FactorDocument3 pagesLiver Cancer Pathophysiology: Predisposing FactorTarantado100% (2)
- Drug in PregnancyDocument49 pagesDrug in PregnancyGarry B GunawanNo ratings yet
- Transisi Demografi Dan Epidemiologi PTM 3Document29 pagesTransisi Demografi Dan Epidemiologi PTM 3erniNo ratings yet
- Sia - G1 - Act 1 - TlshipDocument2 pagesSia - G1 - Act 1 - Tlshiperjen gamingNo ratings yet
- Case 4 Reproductive Block PBLDocument9 pagesCase 4 Reproductive Block PBLFarisNo ratings yet
- Clinical LeadersDocument2 pagesClinical LeadersInfoJDJNo ratings yet
- Barangay Officials, SKS, Barangay Workers & Barangay TanodsDocument2 pagesBarangay Officials, SKS, Barangay Workers & Barangay TanodsCristina MelloriaNo ratings yet
- Discharge PlanDocument3 pagesDischarge PlanMaria Jubel Maceda CabahugNo ratings yet
- NCP HyperthermiaDocument2 pagesNCP HyperthermiaKirby ContaoiNo ratings yet
- Child Health Problems GlobalDocument86 pagesChild Health Problems GlobalBagus P Agen SuplierNo ratings yet
- Internal HemmorhoidsDocument5 pagesInternal Hemmorhoids2netvelasquezNo ratings yet
- Global: CDC Health StrategyDocument22 pagesGlobal: CDC Health StrategyBijay Kumar MahatoNo ratings yet
- Health Complications in Patient After COVID-19 RecoveryDocument14 pagesHealth Complications in Patient After COVID-19 RecoveryKhondoker AliNo ratings yet
- BREASTFEEDINGDocument2 pagesBREASTFEEDINGFianisa RizkaNo ratings yet
- Vehling Annika ResumeDocument1 pageVehling Annika Resumeapi-733364471No ratings yet
- Acog Uso de Aspriian en El Embarazo PDFDocument15 pagesAcog Uso de Aspriian en El Embarazo PDFAnghelino Jesus Meza CentenoNo ratings yet
- Module 4 PPT FinalDocument29 pagesModule 4 PPT FinalEl LahNo ratings yet
- HIQA Residential Care Standards 2008Document86 pagesHIQA Residential Care Standards 2008Debora Tolentino Grossi0% (1)
- Shah - Cancer of The Head and Neck PDFDocument12 pagesShah - Cancer of The Head and Neck PDFElizabetha SalzcenNo ratings yet
- LEUKOPNEADocument21 pagesLEUKOPNEAdaisyNo ratings yet