Professional Documents
Culture Documents
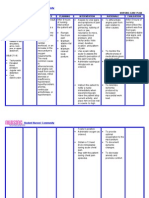
NCP Angina Coronary Artery Disease
Uploaded by
Ron Batacan De LeonCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NCP Angina Coronary Artery Disease
Uploaded by
Ron Batacan De LeonCopyright:
Available Formats
NCP Angina Coronary Artery Disease
The classic symptom of coronary artery disease (CAD) is anginapain caused by loss of oxygen and nutrients to the myocardial tissue because of inadequate coronary blood flow. In most but not all patients presenting with angina, CAD symptoms are caused by significant atherosclerosis. Unstable angina is sometimes grouped with MI under the diagnosis of acute coronary syndrome. Angina has three major forms: (1) stable (precipitated by effort, of short duration, and easily relieved), (2) unstable (longer lasting, more severe, may not be relieved by rest/nitroglycerin; may also be new onset of pain with exertion or recent acceleration in severity of pain), and (3) variant (chest pain at rest with ECG changes due to coronary artery spasm). The AHCPR guidelines of May 1994 state that unstable angina is a transitory syndrome that causes significant disability and death in the United States. CARE SETTING Patients judged to be at intermediate or high likelihood of significant CAD are often hospitalized for further evaluation and therapeutic intervention. Classification of angina (provided by Canadian Cardiovascular Society Classification [CCSC]) aids in determining the risk of adverse outcomes for patients with unstable angina and, therefore, level of treatment needs. Class III angina is identified as occurring if the patient walks less than two blocks and normal activity is markedly limited, and class IV angina occurs at rest or with minimal activity and level of activity is severely limited. These two classes may require inpatient evaluation/therapeutic adjustments. RELATED CONCERNS Cardiac surgery: postoperative care Dysrhythmias Heart failure: chronic Myocardial infarction Psychosocial aspects of care Patient Assessment Database
ACTIVITY/REST May report: Sedentary lifestyle, weakness Fatigue, feeling incapacitated after exercise Chest pain with exertion or at rest Awakened by chest pain May exhibit: Exertional dyspnea CIRCULATION May report: History of heart disease, hypertension, obesity in self/family May exhibit: Tachycardia, dysrhythmias Blood pressure normal, elevated, or decreased Heart sounds: May be normal; late S4 or transient late systolic murmur (papillary muscledysfunction) may be evident during pain Moist, cool, pale skin/mucous membranes in presence of vasoconstriction EGO INTEGRITY May report: Stressors of work, family, others May exhibit: Apprehension, uneasiness FOOD/FLUID May report: Nausea, heartburn/epigastric distress with eating Diet high in cholesterol/fats, salt, caffeine, liquor May exhibit: Belching, gastric distension PAIN/DISCOMFORT May report: Substernal or anterior chest pain that may radiate to jaw, neck, shoulders, and upper extremities (to left side more than right)
Quality: Varies from transient/mild to moderate, heavy pressure, tightness, squeezing, burning Duration: Usually less than 15 min, rarely more than 30 min (average 3 min) Precipitating factors: Physical exertion or great emotion, such as anger or sexual arousal; exercise in weather extremes; or may be unpredictable and/or occur during rest or sleep in unstable angina Relieving factors: Pain may be responsive to particular relief mechanisms (e.g., rest, antianginal medications) New or ongoing chest pain that has changed in frequency, duration, character, or predictability (i.e., unstable, variant, Prinzmetals) May exhibit: Facial grimacing, placing fist over midsternum, rubbing left arm, muscle tension, restlessness Autonomic responses, e.g., tachycardia, blood pressure changes RESPIRATION May report: Dyspnea worse with exertion History of smoking May exhibit: Respirations: Increased rate/rhythm and alteration in depth TEACHING/LEARNING May report: Family history or risk factors of CAD, hypertension, stroke, diabetes, cigarette smoking, hyperlipidemia Use/misuse of cardiac, hypertensive, or OTC drugs Regular alcohol use, illicit drug use, e.g., cocaine, amphetamines
Discharge plan DRG projected mean length of inpatient stay: 3.24.2 days considerations: Alteration in medication use/therapy Assistance with homemaker/maintenance tasks Changes in physical layout of home Refer to section at end of plan for postdischarge considerations. DIAGNOSTIC STUDIES ECG: Often normal when patient at rest or when pain-free; depression of the ST segment or T wave inversion signifies ischemia. Dysrhythmias and heart block may also be present. Significant Q waves are consistent with a prior MI. 24-hour ECG monitoring (Holter): Done to see whether pain episodes correlate with or change during exercise or activity. ST depression without pain is highly indicative of ischemia. Exercise or pharmacological stress electrocardiography: Provides more diagnostic information, such as duration and level of activity attained before onset of angina. A markedly positive test is indicative of severe CAD. Note: Studies have shown stress echo studies to be more accurate in some groups than exercise stress testing alone. Cardiac enzymes (AST, CPK, CK and CK-MB; LDH and isoenzymes LD1, LD2): Usually within normal limits (WNL); elevation indicates myocardial damage. Chest x-ray: Usually normal; however, infiltrates may be present, reflecting cardiac decompensation or pulmonary complications. PCO2, potassium, and myocardial lactate: May be elevated during anginal attack (all play a role in myocardial ischemia and may perpetuate it). Serum lipids (total lipids, lipoprotein electrophoresis, and isoenzymes cholesterols [HDL, LDL, VLDL]; triglycerides; phospholipids): May be elevated (CAD risk factor).
Echocardiogram: May reveal abnormal valvular action as cause of chest pain. Nuclear imaging studies (rest or stress scan): Thallium-201: Ischemic regions appear as areas of decreased thallium uptake. MUGA: Evaluates specific and general ventricle performance, regional wall motion, and ejection fraction. Cardiac catheterization with angiography: Definitive test for CAD in patients with known ischemic disease with angina or incapacitating chest pain, in patients with cholesterolemia and familial heart disease who are experiencing chest pain, and in patients with abnormal resting ECGs. Abnormal results are present in valvular disease, altered contractility, ventricular failure, and circulatory abnormalities. Note: Ten percent of patients with unstable angina have normal-appearing coronary arteries. Ergonovine (Ergotrate) injection: On occasion, may be used for patients who have angina at rest to demonstrate hyperspastic coronary vessels. (Patients with resting angina usually experience chest pain, ST elevation, or depression and/or pronounced rise in left ventricular end-diastolic pressure [LVEDP], fall in systemic systolic pressure, and/or high-grade coronary artery narrowing. Some patients may also have severe ventricular dysrhythmias.) NURSING PRIORITIES 1. Relieve/control pain. 2. Prevent/minimize development of myocardial complications. 3. Provide information about disease process/prognosis and treatment. 4. Support patient/SO in initiating necessary lifestyle/behavioral changes. DISCHARGE GOALS 1. Achieves desired activity level; meets self-care needs with minimal or no pain. 2. Free of complications. 3. Disease process/prognosis and therapeutic regimen understood.
4. Participating in treatment program, behavioral changes. 5. Plan in place to meet needs after discharge.
You might also like
- Nursing Care Plan For Heart Failure ChronicDocument26 pagesNursing Care Plan For Heart Failure ChronicbrantNo ratings yet
- NCP Acute PainDocument5 pagesNCP Acute PainEzra TuanNo ratings yet
- Nursing Care Plan Date Assessed: December 11, 2017 Nursing Diagnosis Nursing Objective Nursing Intervention Scientific Explanation EvaluationDocument2 pagesNursing Care Plan Date Assessed: December 11, 2017 Nursing Diagnosis Nursing Objective Nursing Intervention Scientific Explanation EvaluationCelyn Nicole Fernandez RollanNo ratings yet
- Assessing and Managing Cerebral Perfusion IssuesDocument3 pagesAssessing and Managing Cerebral Perfusion IssuesMicaela CrisostomoNo ratings yet
- NCP Total Hip ReplacementDocument11 pagesNCP Total Hip ReplacementDoneva Lyn MedinaNo ratings yet
- Case Study RespiDocument3 pagesCase Study RespiMark Jheran AlvarezNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term Goal: IndependentDocument4 pagesAssessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term Goal: IndependentNinaNo ratings yet
- NCP AnginaDocument3 pagesNCP AnginaShie LA100% (1)
- PathophysiologyDocument1 pagePathophysiologyHazel PalomaresNo ratings yet
- ISBAR DocumentationDocument1 pageISBAR DocumentationFrancorussNo ratings yet
- NCP Copd4Document15 pagesNCP Copd4Alessa Marie Crisostomo Salazar100% (1)
- NCP Ineffective Cardiopulmonary PerfusionDocument3 pagesNCP Ineffective Cardiopulmonary PerfusionjamiemapanaoNo ratings yet
- Tuberculous Meningitis Nursing AssessmentDocument1 pageTuberculous Meningitis Nursing AssessmentMark Adrian D. DizorNo ratings yet
- Cues Nursing Diagnosis Scientific Reason Objective Nursing Intervention Rationale EvaluationDocument4 pagesCues Nursing Diagnosis Scientific Reason Objective Nursing Intervention Rationale Evaluationjomsportg0% (1)
- Nursing Care Plans for Neurological PatientDocument9 pagesNursing Care Plans for Neurological PatientJam AbantaoNo ratings yet
- NCPDocument4 pagesNCPaviesoreal100% (1)
- Nursing Care PlanDocument10 pagesNursing Care PlanmariasomorayNo ratings yet
- Nursing Care PlanDocument22 pagesNursing Care PlanjamNo ratings yet
- Cardiac Case Study NDDocument11 pagesCardiac Case Study NDapi-313165458No ratings yet
- Ineffective Airway Clearance Nursing Care PlanDocument2 pagesIneffective Airway Clearance Nursing Care Planrois romaNo ratings yet
- Nursing Care PlanDocument14 pagesNursing Care PlanVin Landicho100% (1)
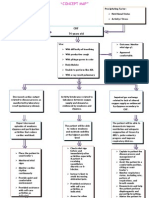
- Angina Pectoris PathophysiologyDocument2 pagesAngina Pectoris PathophysiologyALIANA KIMBERLY MALQUESTONo ratings yet
- NCP Decreased Cardiac Output 1Document2 pagesNCP Decreased Cardiac Output 1Arnel MacabalitaoNo ratings yet
- Cva NCPDocument1 pageCva NCPxiang jinNo ratings yet
- Acute Cardiac Pain Management GuideDocument31 pagesAcute Cardiac Pain Management Guidejan100% (1)
- St. Anthony's Nursing Care Plan for Acute Chest PainDocument1 pageSt. Anthony's Nursing Care Plan for Acute Chest PainjoegeNo ratings yet
- Case Study StemiDocument2 pagesCase Study StemiRajeswari SinnasamyNo ratings yet
- Gender Dysphoria NCPDocument1 pageGender Dysphoria NCPSeann LorescoNo ratings yet
- NCP 2 and Soapie 1Document5 pagesNCP 2 and Soapie 1narsD100% (1)
- Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective Short Term Short TermDocument2 pagesAssessment Diagnosis Planning Intervention Rationale Evaluation Subjective Short Term Short TermFrancis Xavier S. MendezNo ratings yet
- Decreased Cardiac OutputDocument5 pagesDecreased Cardiac Outputshuang81No ratings yet
- ACUTE RESPIRATORY DISTRESSDocument1 pageACUTE RESPIRATORY DISTRESSchristine louise bernardo100% (1)
- NCP IschemicDocument19 pagesNCP IschemicChristina Espiña EjercitoNo ratings yet
- Week 10 Drug Card - Hydrochlorothiazide (HCTZ)Document2 pagesWeek 10 Drug Card - Hydrochlorothiazide (HCTZ)RCurry09No ratings yet
- Scientific Explanation of Expected Outcomes and InterventionsDocument4 pagesScientific Explanation of Expected Outcomes and InterventionsGensen Cu RoxasNo ratings yet
- Reduce Cardiac Workload and Chest Pain Nursing Care PlanDocument8 pagesReduce Cardiac Workload and Chest Pain Nursing Care PlanryzaimaliaNo ratings yet
- NURSING CARE PLAN - Myocardial Infarction Assessment Diagnosis Inference Planning Intervention Rationale EvaluationDocument4 pagesNURSING CARE PLAN - Myocardial Infarction Assessment Diagnosis Inference Planning Intervention Rationale Evaluationsweethoney220% (1)
- Pulmonary HypertensionDocument10 pagesPulmonary HypertensionqingwenNo ratings yet
- Pulmonary EmbolismDocument8 pagesPulmonary EmbolismspoilttbrattNo ratings yet
- Pain NCP BillrothDocument2 pagesPain NCP BillrotharjayNo ratings yet
- Risk For Decreased Cardiac OutputDocument3 pagesRisk For Decreased Cardiac OutputSid Artemis FriasNo ratings yet
- Nursing Care Plan HF FinalDocument10 pagesNursing Care Plan HF FinalCristina L. JaysonNo ratings yet
- NCP PainDocument2 pagesNCP PainApril_Ivy_Raga_3835No ratings yet
- Nursing Diagnosis For Coronary Artery Disease - Acute PainDocument2 pagesNursing Diagnosis For Coronary Artery Disease - Acute PainAngie Mandeoya100% (1)
- Assessment Nursing Diagnosis Inference Objectives Nursing Intervention Rationale EvaluationDocument10 pagesAssessment Nursing Diagnosis Inference Objectives Nursing Intervention Rationale EvaluationJobelle AcenaNo ratings yet
- SOMBILLO Scenario 1 ANGINADocument2 pagesSOMBILLO Scenario 1 ANGINAKarla SombilloNo ratings yet
- Ineffective Cerebral Tissue Perfusion Related ToDocument7 pagesIneffective Cerebral Tissue Perfusion Related TohannahNo ratings yet
- Nanda NCP BasedDocument14 pagesNanda NCP Baseddeliejoyce100% (1)
- Impaired Skin IntegrityDocument2 pagesImpaired Skin IntegrityLilet Dela CruzNo ratings yet
- Anxiety R:T Death ThreatDocument8 pagesAnxiety R:T Death ThreatAlfredo BaulaNo ratings yet
- NCPDocument4 pagesNCPyasayayasay yasayNo ratings yet
- HCVDDocument5 pagesHCVDkhrizaleehNo ratings yet
- Nursing Care Plan for Spinal Cord InjuryDocument3 pagesNursing Care Plan for Spinal Cord InjuryDan Leo UnicoNo ratings yet
- Scribd 020922 Case Study-Oncology A&kDocument2 pagesScribd 020922 Case Study-Oncology A&kKellie DNo ratings yet
- Concept Map - Abby !Document2 pagesConcept Map - Abby !Abegail Abaygar100% (3)
- Ineffective Airway ClearanceDocument2 pagesIneffective Airway ClearanceHanya Bint PotawanNo ratings yet
- Angina PectorisDocument12 pagesAngina Pectorismardsz93% (14)
- Angina PectorisDocument12 pagesAngina Pectorisapi-3797941No ratings yet
- Angina (Coronary Artery Disease) : Care SettingDocument18 pagesAngina (Coronary Artery Disease) : Care SettingNom NomNo ratings yet
- Angina PectorisDocument36 pagesAngina PectorisBardahWasaLamahNo ratings yet
- CCHCS Approved AbbreviationsDocument43 pagesCCHCS Approved AbbreviationsLunaRuizNo ratings yet
- Ensure Healthy Blood PressureDocument6 pagesEnsure Healthy Blood PressureWindy Ng WMNo ratings yet
- Coronary Artery DiseaseDocument3 pagesCoronary Artery DiseaseMarta Luquez RNo ratings yet
- Non-Profit Organization Funds Gregory Grabovoi TeachingsDocument95 pagesNon-Profit Organization Funds Gregory Grabovoi Teachingsssss87va93% (27)
- Emergency Management of Cardiac Chest Pain: A ReviewDocument5 pagesEmergency Management of Cardiac Chest Pain: A Reviewahmad habibNo ratings yet
- 3.4 Cross-Sectional StudiesDocument4 pages3.4 Cross-Sectional StudiesRicardo Gomes100% (1)
- The Evolution and Future of ACC/AHA Clinical Practice Guidelines: A 30-Year JourneyDocument12 pagesThe Evolution and Future of ACC/AHA Clinical Practice Guidelines: A 30-Year JourneyYouyouNo ratings yet
- Koskinas, 2019Document11 pagesKoskinas, 2019Amro MahmoudNo ratings yet
- 23 HyperlipidemiaDocument85 pages23 HyperlipidemiaIhab MoustafaNo ratings yet
- Treatment GuidelinesDocument0 pagesTreatment GuidelinesFawad HameediNo ratings yet
- Abbreviations and SymbolsDocument73 pagesAbbreviations and Symbolsruzana1396No ratings yet
- Eci 12222Document9 pagesEci 12222Andikaputra Brahma WidiantoroNo ratings yet
- Soal Cardio VascularDocument27 pagesSoal Cardio VascularJonathan FebiantoNo ratings yet
- Medical 2021 Question Paper BSC NursingDocument24 pagesMedical 2021 Question Paper BSC NursingWinter BearNo ratings yet
- ED Internal Medicine Oral Exam TopicsDocument10 pagesED Internal Medicine Oral Exam TopicsalirbidiNo ratings yet
- Heart AtackDocument6 pagesHeart AtackUSMP FN ARCHIVOSNo ratings yet
- TahbsoDocument77 pagesTahbsoCzarina Charmaine DiwaNo ratings yet
- VorapaxarDocument21 pagesVorapaxarIoana GhirvuNo ratings yet
- The China Study - Fact or Fallacy - Raw Food SOSDocument137 pagesThe China Study - Fact or Fallacy - Raw Food SOSdrbb6No ratings yet
- HidrokinetoterapieDocument35 pagesHidrokinetoterapielauraNo ratings yet
- Cardiac PacingDocument4 pagesCardiac PacingmrygnvllNo ratings yet
- Relationship of Frontal QRS-T Angle With Syntax Score in Non-St Elevated Myocardial Infarction Patients in H. Adam Malik General Hospital MedanDocument8 pagesRelationship of Frontal QRS-T Angle With Syntax Score in Non-St Elevated Myocardial Infarction Patients in H. Adam Malik General Hospital MedanInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Medical Form AbcDocument4 pagesMedical Form Abcapi-351184488No ratings yet
- Update of The Nutri-Score AlgorithmDocument54 pagesUpdate of The Nutri-Score AlgorithmoestaniNo ratings yet
- Chest Pain: Jean J. Chatham, MDDocument40 pagesChest Pain: Jean J. Chatham, MDYermia RashaquatNo ratings yet
- Polyclinic AllDocument92 pagesPolyclinic AllFatima ShahNo ratings yet
- Written Report Coronary Heart DiseaseDocument5 pagesWritten Report Coronary Heart DiseaseJade WushuNo ratings yet
- Treadmill Stress TestDocument16 pagesTreadmill Stress TestMuhammad Yasir WahabNo ratings yet
- R U-ChnDocument16 pagesR U-ChnRichelle RodrigoNo ratings yet
- Guidelines For Diagnosis and Treatment of Patients With Vasospas 2014Document23 pagesGuidelines For Diagnosis and Treatment of Patients With Vasospas 2014he xuNo ratings yet