Professional Documents
Culture Documents
Feb Case Study Edited
Uploaded by
api-174496267Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Feb Case Study Edited
Uploaded by
api-174496267Copyright:
Available Formats
Amanuel Negussie Clinical Practicum I Feb 23, 2013 Metastatic Orbit History of Present Illness: HG is a 69-year-old male with
stage IVB diffuse large B cell lymphoma (DLBCL) with bone marrow involvement, generalized lymphadenopathy, massive splenomegally, right ureteral obstruction, and orbital involvement. He initially presented in August 2012 with an enlarged left cervical lymph node, elevated creatinine, and renal ultrasound revealing a mass. Fine needle aspiration (FNA) of his cervical spine revealed DLBCL. Computed tomography (CT) and positron emission tomography (PET) noted multiple areas of hypermetabolic adenopathy. HG took four lines of chemotherapy treatment since diagnosis, the most recent being Dexamethasone, Cytarabine, Platinum (DHAP). In follow up prior to his second cycle of DHAP, the patient complained on a one-week history of blurred vision, left eye pain, and open bottom eyelids. Ophthalmology evaluated the patient and noted bilateral lower and upper eyelid masses, consistent with orbital involvement and no sign of intra ocular involvement. Magnetic resonance imaging (MRI) was obtained which noted enhancement in his right lacrimal gland, left lacrimal gland, medial right orbit, right orbital wall, right orbital septum, right inferior and oblique muscles, left medial orbital wall, and bilateral inferior recti muscles. A week after the exam, HG noticed his left lower eyelid turned out and reported pressure and pain in his eyes bilaterally but worse on the left eye. He underwent ocular evaluation, which noted that the left eye was red with clear drainage. The patient also complained of being fatigued and slight dizziness when standing. Past Medical History: HG has a medical history of stage IV DLBCL, hyperlipidemia, diabetes mellitus type II, glaucoma, hammertoe, peripheral nerve disease, and cataract extraction. The patient has no known allergies. Diagnostic Imaging Studies: HG had orbit MRI with and without contrast and brain MRI with and without contrast. He also had a CT scan of the head region in radiation oncology during the simulation process. Family History: HGs mother had a cerebrovascular accident (CVA) in her 70s. The patient has a deceased father from lung cancer and a deceased brother for unknown reason. His sister has breast cancer and heart conditions.
Social History: HG is a retired mechanic who lives with his wife. The patient quit smoking tobacco 10 years ago and denied any alcohol and drug use. Medication: HG takes Acetaminophen, Dexamethasone, Guaifenesin, Insulin, Lorazepam, Magnesium Hydroxide, Morphine, Potassium Chloride, Prochlorperazine, Senokot, Timolol, Artificial Tears Solution, and Lubricating Ointment. He also takes Ondansetron and Vancomycine injection. Recommendations: Considering the signs and symptoms and the reports from ophthalmology, HG is a candidate for palliative radiation to his bilateral orbits. As a result, the patient was recommended to receive radiation therapy for the treatment of his orbits. Possible side effects of the treatment were discussed with the patient including erythema, fatigue, dry and red eyes, hair loss of the eyelashes and eyebrows, acute conjunctivitis, chronic keratitis, and possible long-term risk of radiation-induced cataracts. The Plan (Prescription): It is usually effective to treat palliative cases with a higher dose in fewer fractions and a larger field size that includes the entire tumor.1 As a result, the treatment was prescribed to 3060 centigray (cGy) at 180 cGy per fraction to the 100% isodose line for 17 fractions using three dimensional conformal radiation therapy (3D-CRT). Patient Setup/ Immobilization: HG was simulated in a supine position with his head towards the scanner. His head was fixed in a neutral position by using a headset. Aquaplastic mask was made by warming a thermoplastic mesh in a water bath and stretching it over the patients face and neck gently (Figure 1). After simulation, the mask was labeled with the patients name for identification purpose. This customized mask will be used to reproduce the same head position and restrict movements during his treatment. The patient was holding a plastic ring and had a small sponge under his knees for comfort. A Philips large bore 16-slice CT machine was used for the simulation. Head images were taken at 0.3 centimeter (cm) slices. Anatomic Contouring: After the simulation was completed, the CT slice images were imported to the Pinnacle3 9.0 radiation treatment planning system (TPS). The radiation oncologist then contoured the gross tumor volume (GTV) and planning target volume (PTV) using the TPS. The dosimetrist contoured the brain, left and right eyes, and left and right lenses. The purpose of these contours is to evaluate the dose delivered to the radiosensitive anatomical structures while planning to deliver the desired dose to the PTV.
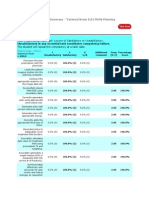
Beam Isocenter/ Arrangement: A Varian 21 IX 3501 linear accelerator (Linac) machine was used to treat the patient. During simulation, the radiation oncologist put the isocenter posterior from the nasal cavity. A four field, two right lateral and two left lateral, beam arrangement was used (see Figure 2). Each lateral field consisted a combination of 6 megavolts (MV) and 18MV energy photon beams. The gantry was set at 270o for the right lateral fields and 90o for the left lateral fields, and the collimator was set at 0o for all fields. Treatment Planning: Each field has a multileaf collimator (MLC) blocking pattern constructed by the physician to define the treatment field. The dosimetrist picked a new calculation point 3cm anterior from the isocenter, because the isocenter was located outside the treatment field (see Figure 3). The plan was primarily calculated with a two 6MV right and left lateral field weighted equally; but, the anterior part of the GTV was not getting adequate coverage of the dose. Therefore, a 0.5cm bolus was used to pull the dose anteriorly (see figure1). A field-in-field beam was created for both lateral fields using 18MV to reduce the maximum dose and decrease the hot spot (see figure 4). In addition, a 15o enhanced dynamic wedge (EDW) was used on all fields to account for the curvature of the head and reduce the hotspot. Both primary beams of the right lateral and left lateral were weighted 47% each; whereas, each field-in-field beams were weighted 3%. The plan was completed with a total monitor unit (MU) of 297, maximum dose of 3571cGy, and a hot spot of 16% located within the bolus. After the plan was completed to the dosimetrists satisfaction, it was saved for the physician to evaluate. The physician approved the plan after reviewing and ensuring that the 100% isodose line sufficiently covered the GTV and the dose to the lenses was below 500 cGy (see Figure 5). Quality Assurance Checks The MU check was performed using the MuCheck 8.2.0. Software. At our clinical site, a 3% deviation in MU is the tolerance for any 3D-CRT plans. Anything outside this range needs to be recalculated and fixed by dosimetrists or physicists prior to treatment. This plan was approved with -2.2% for the primary right lateral field, -1.45% for the field-in-field right lateral field, -2.61 for the primary left lateral field, and -1.01% for the fieldin-field left lateral field. The treatment plan was then reviewed and evaluated by the medical physicist before the patient began his treatment. Conclusions: It was interesting working on this case since metastatic orbit cases are not seen more often. Planning this treatment with a lower maximum dose and adequate dose coverage of the PTV was challenging. This was the first real case I planned using a bolus. I was able to learn,
observe, and examine the use of bolus in modifying dose for superficial structures. I also learned the appropriate use of field-in-field techniques to improve dose distribution.
Figures
Figure 1: 0.5cm bolus taped to an aquaplast mask
Figure 2: right lateral and left lateral beam arrangement
Figure 3: the simulation isocenter and the calculation point on a transverse CT slice
Right lateral field in field BEV
Left lateral primary field BEV
Right lateral primary BEV
Left lateral field in field BEV
Figure 4: Beams eye view (BEV) of the lateral primary and field-in-field fields
Figure 5: Dose volume histogram (DVH)
References 1. Bentel GC. Radiation Therapy Planning. 2nd ed. New York: McGraw-Hill;1996: 490-526.
You might also like
- V 13 RtsummaryonsitetrainingworkshopfamanuelnegussieDocument1 pageV 13 Rtsummaryonsitetrainingworkshopfamanuelnegussieapi-174496267No ratings yet
- Ec 102 Eclipseinverseplanningimrtandrapidarcv 13 CamanuelnegussieDocument1 pageEc 102 Eclipseinverseplanningimrtandrapidarcv 13 Camanuelnegussieapi-174496267No ratings yet
- Amanuel Negussie: Certificate of AttendanceDocument1 pageAmanuel Negussie: Certificate of Attendanceapi-174496267No ratings yet
- ElectronDocument2 pagesElectronapi-174496267No ratings yet
- Amanuel Final 5 1 14Document19 pagesAmanuel Final 5 1 14api-174496267No ratings yet
- Fall EvalsDocument6 pagesFall Evalsapi-212894050No ratings yet
- PhotonDocument3 pagesPhotonapi-174496267No ratings yet
- ResumeDocument2 pagesResumeapi-174496267No ratings yet
- Fall EvalsDocument6 pagesFall Evalsapi-212894050No ratings yet
- Joe RTDocument1 pageJoe RTapi-174496267No ratings yet
- BrachytherapyDocument3 pagesBrachytherapyapi-174496267No ratings yet
- Comprehensive Case Study Final - AdjustedDocument17 pagesComprehensive Case Study Final - Adjustedapi-174496267No ratings yet
- Fall EvalsDocument6 pagesFall Evalsapi-212894050No ratings yet
- ImrtDocument3 pagesImrtapi-174496267No ratings yet
- For E-PortfolioDocument14 pagesFor E-Portfolioapi-174496267No ratings yet
- Monthly EvalDocument2 pagesMonthly Evalapi-174496267No ratings yet
- ConferenceDocument7 pagesConferenceapi-174496267No ratings yet
- Comprehensive Case Study - AnDocument31 pagesComprehensive Case Study - Anapi-174496267No ratings yet
- ComptotalsDocument3 pagesComptotalsapi-174496267No ratings yet
- Tally 1Document2 pagesTally 1api-174496267No ratings yet
- PT Case LogsDocument2 pagesPT Case Logsapi-174496267No ratings yet
- September Case StudyDocument20 pagesSeptember Case Studyapi-174496267No ratings yet
- ConferencesDocument4 pagesConferencesapi-174496267No ratings yet
- Case Log FallDocument2 pagesCase Log Fallapi-174496267No ratings yet
- October Case StudyDocument15 pagesOctober Case Studyapi-174496267No ratings yet
- August Citation AssignmentDocument2 pagesAugust Citation Assignmentapi-174496267No ratings yet
- 2nd Rotation PallDocument3 pages2nd Rotation Pallapi-174496267No ratings yet
- July Case StudyDocument18 pagesJuly Case Studyapi-174496267No ratings yet
- Conference LogsDocument1 pageConference Logsapi-174496267No ratings yet
- May EvalDocument6 pagesMay Evalapi-174496267No ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- EAU Guidelines On Male Sexual Dysfunction 2019Document96 pagesEAU Guidelines On Male Sexual Dysfunction 2019Muti IlmarifaNo ratings yet
- BHS InggrisDocument16 pagesBHS InggrisInri SusantiNo ratings yet
- CHHi PDocument13 pagesCHHi PBamo MuhammadNo ratings yet
- AlgorithmsDocument2 pagesAlgorithmsapi-237266632No ratings yet
- Oncologic NursingDocument132 pagesOncologic Nursingɹǝʍdןnos100% (10)
- Cancer: Causes, Symptoms and TreatmentDocument12 pagesCancer: Causes, Symptoms and TreatmentLeigh AnneNo ratings yet
- WK 9 Errors Failures RisksDocument29 pagesWK 9 Errors Failures RisksMd. Firoz HasanNo ratings yet
- IAEA Safety Standards 2010Document112 pagesIAEA Safety Standards 2010mariacheikhwafaNo ratings yet
- Wilms Tumour: Nitha K 2 Year MSC NursingDocument40 pagesWilms Tumour: Nitha K 2 Year MSC NursingNITHA K100% (1)
- ATRX LossDocument23 pagesATRX LossLeilane GlienkeNo ratings yet
- Tumors of The Middle Ear & Mastoid - Ear Surgery Information CenterDocument3 pagesTumors of The Middle Ear & Mastoid - Ear Surgery Information CenterDitha FadhilaNo ratings yet
- Options in The Treatment of Head and Neck CancerDocument137 pagesOptions in The Treatment of Head and Neck CancerDeniswara Axell100% (2)
- Retinoblastoma Case Report Latest With ReferenceDocument29 pagesRetinoblastoma Case Report Latest With ReferenceMasykur Ramadhan GaniNo ratings yet
- 09 Prostate Cancer LRDocument137 pages09 Prostate Cancer LRRaya LaelaNo ratings yet
- OSL Source BookDocument36 pagesOSL Source BookNawel MorjanNo ratings yet
- The Effectiveness of PersonalizedDocument6 pagesThe Effectiveness of PersonalizedDzenita Hamzic HalilagicNo ratings yet
- TG 119 IMRT Commissioning and QA PDFDocument15 pagesTG 119 IMRT Commissioning and QA PDFmarkNo ratings yet
- EdCaN Specialty Module 4Document23 pagesEdCaN Specialty Module 4cindy8127No ratings yet
- Exercises With Solutions in Radiation Physics) 4 Radiation DosimetryDocument53 pagesExercises With Solutions in Radiation Physics) 4 Radiation DosimetryDavitMartinezNo ratings yet
- Pet BrochureDocument20 pagesPet BrochureSheikh Hasnain AliNo ratings yet
- Stereotactic Treatment Definitions and LiteratureDocument66 pagesStereotactic Treatment Definitions and LiteratureOmkar KongariNo ratings yet
- PROSTATE CANCER PPT - OdpDocument20 pagesPROSTATE CANCER PPT - OdpCharissa Magistrado De LeonNo ratings yet
- MOSAIQ Radiation Oncology BrochureDocument8 pagesMOSAIQ Radiation Oncology Brochurealeksandar markovicNo ratings yet
- Article 1459955174Document9 pagesArticle 1459955174Nia LieantoNo ratings yet
- Larynx Cancer Case Study AndrewDocument13 pagesLarynx Cancer Case Study Andrewapi-273146320No ratings yet
- Shielding Calculation of RadiationDocument25 pagesShielding Calculation of RadiationHajarMalaghawaNo ratings yet
- S&TR October/November 2011Document8 pagesS&TR October/November 2011bernasekNo ratings yet
- Reishi Ganoderma - Gift of God: Testimonials Questions Answered Japan Doctor's Your CommentsDocument40 pagesReishi Ganoderma - Gift of God: Testimonials Questions Answered Japan Doctor's Your CommentsRediet DawitNo ratings yet
- A Deep Learning U-Net For Detecting and Segmenting Liver TumorsDocument48 pagesA Deep Learning U-Net For Detecting and Segmenting Liver TumorsSabir MuhammadNo ratings yet
- Terra Firma Medical Systems (SMU APEX 2010)Document29 pagesTerra Firma Medical Systems (SMU APEX 2010)Joe ChungNo ratings yet