Professional Documents
Culture Documents
Cerebral Palsy
Uploaded by
TracyCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cerebral Palsy
Uploaded by
TracyCopyright:
Available Formats
Cerebral Palsy
About: The term cerebral palsy refers to any one of a number of neurological disorders that appear in
infancy or early childhood and permanently affect body movement and muscle coordination but don’t
worsen over time. Even though cerebral palsy affects muscle movement, it isn’t caused by problems in the
muscles or nerves. It is caused by abnormalities in parts of the brain that control muscle movements. The
majority of children with cerebral palsy are born with it, although it may not be detected until months or
years later. The early signs of cerebral palsy usually appear before a child reaches 3 years of age. The most
common are a lack of muscle coordination when performing voluntary movements (ataxia); stiff or tight
muscles and exaggerated reflexes (spasticity); walking with one foot or leg dragging; walking on the toes, a
crouched gait, or a “scissored” gait; and muscle tone that is either too stiff or too floppy. A small number of
children have cerebral palsy as the result of brain damage in the first few months or years of life, brain
infections such as bacterial meningitis or viral encephalitis, or head injury from a motor vehicle accident, a
fall, or child abuse.
Cerebral palsy may be classified by the type of movement problem (such as spastic or athetoid cerebral
palsy) or by the body parts involved (hemiplegia, diplegia, and quadriplegia). Spasticity refers to the inability
of a muscle to relax, while athetosis refers to an inability to control the movement of a muscle. Infants who
at first are hypotonic wherein they are very floppy may later develop spasticity. Hemiplegia is cerebral palsy
that involves one arm and one leg on the same side of the body, whereas with diplegia the primary
involvement is both legs. Quadriplegia refers to a pattern involving all four extremities as well as trunk and
neck muscles. Another frequently used classification is ataxia, which refers to balance and coordination
problems. The motor disability of a child with CP varies greatly from one child to another; thus
generalizations about children with cerebral palsy can only have meaning within the context of the subgroups
described above. For this reason, subgroups will be used in this book whenever treatment and outcome
expectations are discussed. Most professionals who care for children with cerebral palsy understand these
diagnoses and use them to communicate about a child's condition.
Spastic Cerebral Palsy
Spastic Cerebral Palsy is the most common diagnosis. If your child’s CP is “spastic,” her muscles are rigid
and jerky, and she has difficulty getting around. There are three types of spastic Cerebral Palsy:
• Spastic diplegia — Your child’s leg and hip muscles are tight, and his legs cross at the knees, making
it difficult to walk. This kind of movement is frequently referred to as “scissoring.”
• Spastic hemiplegia — Only one side of your child’s body is stiff. Her arms or hands might be more
affected than her legs. On the affected side, her arm and leg may not develop normally. She may also
require leg braces.
• Spastic quadriplegia — The severest of the three, spastic quadriplegia means that your child is more
likely to have mental retardation if diagnosed as quadriplegia. His legs, arms, and body are affected.
It will be difficult for him to walk and talk, and he may also experience seizures.
Athetoid Dyskinetic Cerebral Palsy
Athetoid dyskinetic is the second most frequently diagnosed type of Cerebral Palsy. Your child will have
normal intelligence, but her body will be totally affected by muscle problems. Her muscle tone can be weak
or tight, and she might have trouble walking, sitting, or speaking clearly. She may also have trouble
controlling her facial muscles and therefore drool.
Ataxic Cerebral Palsy
This is the least diagnosed type of Cerebral Palsy. Your child will have trouble tying his shoes, buttoning his
shirt, cutting with scissors, and doing other tasks that require fine motor skills. He might walk with his feet
farther apart than normal and have trouble with his balance and coordination. Your child may also suffer
from “intention tremors,” a shaking that begins with a voluntary movement. For example, your child may
reach for a toy, and then his hand and arm will start to shake. As he gets closer to the toy, the tremor worsens.
Hypotonic Cerebral Palsy
Unlike with other types of CP, you will notice that your baby has muscle control problems early in life. Her
head seems floppy, and she will not be able to control it when sitting up. Her motor skills will be
developmentally delayed.
It is suspected that this type of Cerebral Palsy is caused by brain damage or malformations that occur while a
baby’s brain is still developing.
Mixed Cerebral Palsy
If your child does not “fit” into one of the above diagnoses, your doctor will consider him “mixed.” This is
quite common.
Congenital Cerebral Palsy
If your child is diagnosed with congenital Cerebral Palsy, be aware that this is not a “type” of palsy, but
rather it is a term meaning “birth defect.” In other words, your child’s doctor is saying that he developed
Cerebral Palsy during development. It is not a condition that your child inherited from you or your husband
or partner. And it is not caused by a medical error.
Erb’s Palsy
If any type of Cerebral Palsy can be attributed to a birthing accident, it is Erb’s palsy (brachial plexus palsy).
According to the National Institute of Neurological Disorders and Stroke:
Although injuries can occur at any time, many brachial plexus injuries happen when a baby’s
shoulders become impacted during delivery and the brachial plexus nerves stretch or tear.
If your baby has Erb’s palsy, he will have no muscle control in his arm; the arm will be limp and have no
feeling.
Based on the nerve area that is affected, there are four types of Erb’s Palsy:
• Avulsion — the nerve completely separates from the spine.
• Rupture — the nerve is torn throughout but not from the spine.
• Praxis/stretch — the nerve is damaged but not torn and could heal on its own.
• Neuroma — scar tissue from an injury puts pressure on the nerve.
Causes: The common cerebral palsy causes are premature delivery, malnutrition, bacterial or viral infection
at the time of birth, low birth weight, injury caused to head or brain due to a fall or accident and
hemorrhages.
Pathophysiology: Cerebral palsy is caused by an insult to the immature brain; the period during which the
insult can occur ranges from any time before birth up to the postnatal period. (Some classify cerebral palsy as
an insult to the brain before age 3 years.) After the immediate postnatal period, cerebral palsy often has an
identifiable cause (eg, hypoxic-ischemic encephalopathy), which should be noted. The cerebral insult alters
muscle tone, muscle stretch reflexes, primitive reflexes, and postural reactions. Other associated symptoms
may be involved secondary to the neurologic insult (eg, mental retardation, vision and hearing problems,
seizures), but they are not part of the definition of cerebral palsy.
The etiology of the cerebral insults includes vascular, hypoxic-ischemic, metabolic, infectious, toxic,
teratogenic, traumatic, and genetic causes. The pathogenesis of cerebral palsy involves multifactorial causes,
but much is still unknown. Different pathogenetic mechanisms of cerebral palsy have been associated with
preterm and term births. In many cases, a cause cannot be accurately determined. Some believe that a pre-
existing condition in some fetuses causes early birth and neurologic problems, as opposed to the prematurity
itself causing cerebral palsy.
Treatment: Treatment may include physical and occupational therapy, speech therapy, drugs to control
seizures, relax muscle spasms, and alleviate pain; surgery to correct anatomical abnormalities or release tight
muscles; braces and other orthotic devices; wheelchairs and rolling walkers; and communication aids such as
computers with attached voice synthesizers.
You might also like
- Understanding Cerebral PalsyDocument4 pagesUnderstanding Cerebral Palsyfaye kim100% (1)
- Cerebral Palsy Guide: Causes, Symptoms & TypesDocument97 pagesCerebral Palsy Guide: Causes, Symptoms & TypesPrernaSharma100% (3)
- ClubfootDocument5 pagesClubfootCherry AlmarezNo ratings yet
- ClubfootDocument21 pagesClubfootRoss Carolino Fernandez100% (1)
- ClubfootDocument9 pagesClubfootLorebell100% (5)
- Case StudyDocument11 pagesCase StudyAnj TadxNo ratings yet
- What Is Spina BifidaDocument18 pagesWhat Is Spina BifidaAnonymous dI1hgIJfjzNo ratings yet
- Nursing Care for a Pregnant Woman with Severe AnemiaDocument22 pagesNursing Care for a Pregnant Woman with Severe AnemiaRAKHI PAUL100% (1)
- What is Paget's Disease: Causes, Symptoms, Diagnosis and TreatmentDocument17 pagesWhat is Paget's Disease: Causes, Symptoms, Diagnosis and Treatmentraghunandhakumar100% (1)
- Congenital hip dysplasia diagnosis in under 40Document6 pagesCongenital hip dysplasia diagnosis in under 40Bek DiazNo ratings yet
- Down Syndrome (Case Presentation Output)Document6 pagesDown Syndrome (Case Presentation Output)Jommel Ryan Corpus LumibaoNo ratings yet
- Surgical Management of Cerebral PalsyDocument72 pagesSurgical Management of Cerebral PalsySamNo ratings yet
- Congenital Hip DislocationDocument13 pagesCongenital Hip DislocationKei CruzNo ratings yet
- Types, Causes and Treatments of ComasDocument3 pagesTypes, Causes and Treatments of ComasgcsNo ratings yet
- Case Study - CharleinDocument13 pagesCase Study - Charleinmacky_lumberaNo ratings yet
- Club FootDocument5 pagesClub FootNika Joy Cabrera AlarconNo ratings yet
- Threatened AbortionDocument2 pagesThreatened AbortionMark Rey50% (2)
- CASE-STUDY-DM AmputationDocument32 pagesCASE-STUDY-DM AmputationJerushamae Castillo0% (1)
- Herniated Nucleus Pulposus: by Limytch DiazDocument23 pagesHerniated Nucleus Pulposus: by Limytch DiazCob CornNo ratings yet
- ANENCEPHALYDocument10 pagesANENCEPHALYSharmaine SimonNo ratings yet
- Cva Case StudyDocument31 pagesCva Case StudyZoe AnnaNo ratings yet
- Benign Febrile Convulsions Nursing Care PlansDocument10 pagesBenign Febrile Convulsions Nursing Care PlansMurugesan100% (1)
- DwarfismDocument2 pagesDwarfismKatrina PonceNo ratings yet
- Hirschsprung-Disease Case StudyDocument20 pagesHirschsprung-Disease Case StudyFaith TorralbaNo ratings yet
- Spina Bifida Anatomy, Causes, and Nursing CareDocument5 pagesSpina Bifida Anatomy, Causes, and Nursing Careroseavy100% (1)
- Neurological AssessmentDocument18 pagesNeurological AssessmentMackenzie GaranNo ratings yet
- Tracheo-Oesophageal FistulaDocument19 pagesTracheo-Oesophageal Fistularajan kumar100% (3)
- BRITTLE BONE DISEASE: OSTEOPOROSIS AND FRACTURESDocument25 pagesBRITTLE BONE DISEASE: OSTEOPOROSIS AND FRACTURESNavya Sruthi MandapatiNo ratings yet
- Case Study of Cesarean SectionDocument9 pagesCase Study of Cesarean SectionErika Joy Imperio0% (1)
- Case Study of "Subtrochanteric Femur": Prepared By: John Ress A. Escobal Group 1Document11 pagesCase Study of "Subtrochanteric Femur": Prepared By: John Ress A. Escobal Group 1J.r. MercadoNo ratings yet
- Parkinsons PresentationDocument7 pagesParkinsons PresentationrinninNo ratings yet
- PREECLAMPSIA Case ScenarioDocument2 pagesPREECLAMPSIA Case Scenariosabao kizuiteNo ratings yet
- Velez College Nursing Students Present Case Study on HydrocephalusDocument37 pagesVelez College Nursing Students Present Case Study on HydrocephalusMarlon Glorioso IINo ratings yet
- Osteoporosis Case ReportDocument21 pagesOsteoporosis Case ReportJewenson SalvadorNo ratings yet
- Cerebral Palsy AssessmentDocument6 pagesCerebral Palsy AssessmentdrprasantNo ratings yet
- Migraine Case StudyDocument15 pagesMigraine Case StudyJean LaiNo ratings yet
- Mechanisms Case StudyDocument13 pagesMechanisms Case Studyshane_tin143No ratings yet
- Anatomy and Physiology of Breech PresentationDocument2 pagesAnatomy and Physiology of Breech Presentationeskempertus0% (2)
- Pathophysiology of mesenchymal chondrosarcomaDocument7 pagesPathophysiology of mesenchymal chondrosarcomaMaria Grace Raquel Ormeneta100% (1)
- Case PresentationDocument10 pagesCase PresentationWina Hanriyani0% (1)
- Case Study: Carpal Tunnel SyndromeDocument30 pagesCase Study: Carpal Tunnel SyndromeMuslihah Mohd Razali0% (1)
- Brittle Bone Disease Causes Fragile BonesDocument30 pagesBrittle Bone Disease Causes Fragile BonesKhim GoyenaNo ratings yet
- Obesity Prevention and Education For School Nurses Community Health NursingDocument66 pagesObesity Prevention and Education For School Nurses Community Health NursingGabrielaNo ratings yet
- Physiological Changes During Pregnancy: Presented By: Ms. Vruti PatelDocument44 pagesPhysiological Changes During Pregnancy: Presented By: Ms. Vruti PatelSANJEEV KUMARNo ratings yet
- Hip Fracture Case Study: 39-Year-Old Male with EpilepsyDocument9 pagesHip Fracture Case Study: 39-Year-Old Male with EpilepsyufuNo ratings yet
- Mature CataractDocument24 pagesMature CataractmethadamayNo ratings yet
- Pediatric Assessment 1 12 PDFDocument11 pagesPediatric Assessment 1 12 PDFJackieNate Ortiz100% (1)
- Incomplete AbortionDocument37 pagesIncomplete AbortionGerarld Immanuel Kairupan100% (1)
- OsteoporosisDocument12 pagesOsteoporosisAzharul Islam ArjuNo ratings yet
- Down SyndromeDocument18 pagesDown Syndromepreciouslacdan86% (7)
- Guiilan Barre SyndromeDocument19 pagesGuiilan Barre SyndromeDhayaneeDruAinsleyIINo ratings yet
- Case Study AnemiaDocument5 pagesCase Study AnemiaMeriam Estepa MartinezNo ratings yet
- A Case Study In:: Hirschsprung DiseaseDocument18 pagesA Case Study In:: Hirschsprung DiseaseJaimie La PenaNo ratings yet
- ReflexesDocument1 pageReflexesBinal Joshi100% (1)
- Case Scenerio HydrocephalusDocument9 pagesCase Scenerio HydrocephalusEllen AngelNo ratings yet
- CORD PROLAPSE GUIDEDocument2 pagesCORD PROLAPSE GUIDEUsman Ali AkbarNo ratings yet
- Site Accessibility Contact Mychild Sitemap Select Language Create AccountDocument42 pagesSite Accessibility Contact Mychild Sitemap Select Language Create Accountretno widyastutiNo ratings yet
- Introduction To LocomotorDocument148 pagesIntroduction To LocomotorsherinprinceNo ratings yet
- Cerebral Palsy Overview: Posture Brain Paralysis Abnormal Muscle MotorDocument11 pagesCerebral Palsy Overview: Posture Brain Paralysis Abnormal Muscle Motorrena_psNo ratings yet
- Intravenous Fluid SelectionDocument12 pagesIntravenous Fluid SelectionTracy100% (4)
- Late Onset PTSTDocument7 pagesLate Onset PTSTTracy100% (1)
- Common List of Cardiac DrugsDocument3 pagesCommon List of Cardiac DrugsTracy100% (2)
- Acid Base DisturbancesDocument34 pagesAcid Base DisturbancesTracy100% (1)
- Appendix B: Clinical Institute Withdrawal Assessment For Alcohol (CIWA-A)Document2 pagesAppendix B: Clinical Institute Withdrawal Assessment For Alcohol (CIWA-A)Tracy100% (1)
- Cardiovascular DrugsDocument22 pagesCardiovascular DrugsTracy100% (1)
- Patient Procedures SurgeriesDocument4 pagesPatient Procedures SurgeriesTracyNo ratings yet
- ABG Interpretation: Julie Perkins RRT-NPS LPCH Respiratory CareDocument14 pagesABG Interpretation: Julie Perkins RRT-NPS LPCH Respiratory CareTracy100% (4)
- Abg InterpretationDocument14 pagesAbg Interpretationmara5140100% (7)
- Mania-Nursing Care PlanDocument2 pagesMania-Nursing Care PlanTracy74% (34)
- Cardiac Meds To MemorizeDocument4 pagesCardiac Meds To MemorizekellyaeNo ratings yet
- Schizophrenia Booket 2009Document22 pagesSchizophrenia Booket 2009Tracy100% (1)
- Patient Implantable Medical DevicesDocument1 pagePatient Implantable Medical DevicesTracy100% (1)
- Common Cardiac Related MedicationsDocument18 pagesCommon Cardiac Related MedicationsTracy100% (2)
- Bipolar Mood ChartDocument2 pagesBipolar Mood ChartTracyNo ratings yet
- Alcohol Withdrawal Assessment SheetsDocument2 pagesAlcohol Withdrawal Assessment SheetsTracy100% (1)
- Notes To Slideshow: How Does The Chronic Care Model Work?Document18 pagesNotes To Slideshow: How Does The Chronic Care Model Work?TracyNo ratings yet
- Drug Calculation TutorialDocument13 pagesDrug Calculation TutorialTracyNo ratings yet
- Documenting A Transfusion Reaction: Chart SmartDocument2 pagesDocumenting A Transfusion Reaction: Chart SmartTracyNo ratings yet
- Soap NoteDocument2 pagesSoap Notetopopirate100% (4)
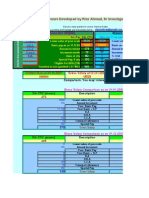
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- WhenTPN Is IndicatedDocument3 pagesWhenTPN Is IndicatedTracyNo ratings yet
- PAS Quick GuideDocument1 pagePAS Quick GuideTracyNo ratings yet
- Psychiatry OverviewDocument2 pagesPsychiatry OverviewTracyNo ratings yet
- Nursing Care Plan GuideDocument1 pageNursing Care Plan GuideTracy100% (1)
- Useful AbbreviationsDocument2 pagesUseful AbbreviationsTracyNo ratings yet
- Types of PainDocument1 pageTypes of PainTracy100% (3)
- Spina BifidaDocument2 pagesSpina BifidaTracy100% (2)
- Cleft Lip and PalateDocument2 pagesCleft Lip and PalateTracy100% (1)
- Gage JR 2001 An Update On The Treatment of Gait Problems in CPDocument10 pagesGage JR 2001 An Update On The Treatment of Gait Problems in CPMarco Tulio FigueroaNo ratings yet
- An Update On The Treatment of Gait Problems in Cerebral PalsyDocument10 pagesAn Update On The Treatment of Gait Problems in Cerebral Palsyyarianna2No ratings yet
- Assessment of Gait Disorders in ChildrenDocument3 pagesAssessment of Gait Disorders in ChildrenMadalina RarincaNo ratings yet
- IjpotDocument209 pagesIjpotmahenderNo ratings yet
- Comparison Between Task Oriented Training and Proprioceptiveneuromuscular Facilitation Exercises On Lower Extremity Function Ince 2165 7025 1000291Document9 pagesComparison Between Task Oriented Training and Proprioceptiveneuromuscular Facilitation Exercises On Lower Extremity Function Ince 2165 7025 1000291Gopi KrishnanNo ratings yet
- Conditioning Effects of Backward Treadmill TraininDocument8 pagesConditioning Effects of Backward Treadmill Traininmaham YousufNo ratings yet
- One More Step: My Story of Living With Cerebral Palsy, Climbing Kilimanjaro, and Surviving The Hardest Race On Earth by Bonner Paddock (Excerpt)Document22 pagesOne More Step: My Story of Living With Cerebral Palsy, Climbing Kilimanjaro, and Surviving The Hardest Race On Earth by Bonner Paddock (Excerpt)HarperOne (an imprint of HarperCollins)No ratings yet
- Neural Plasticity: Effects of and Perspectives for Therapy in Cerebral PalsyDocument20 pagesNeural Plasticity: Effects of and Perspectives for Therapy in Cerebral PalsyΒασίλης ΒασιλείουNo ratings yet
- Al Gabbani PDFDocument107 pagesAl Gabbani PDFArkar SoeNo ratings yet
- Cerebral Palsy by DR - Jaya ShankerDocument38 pagesCerebral Palsy by DR - Jaya ShankerJaya Shankar TedlaNo ratings yet
- Paediatric Neurology Handbook (13 Sept)Document81 pagesPaediatric Neurology Handbook (13 Sept)Moses MutsikwiNo ratings yet
- Cerebral PalsyDocument2 pagesCerebral PalsyTracy100% (1)
- Braddom 6th CH 47 Cerebral PalsyDocument34 pagesBraddom 6th CH 47 Cerebral Palsy李宗旻No ratings yet
- Effectiveness of Neurodevelopmental Technique andDocument4 pagesEffectiveness of Neurodevelopmental Technique andAna paula CamargoNo ratings yet
- Clinical Examination of Children With Cerebral PalsyDocument10 pagesClinical Examination of Children With Cerebral PalsyYogin PatelNo ratings yet
- AOPA Handout NewParadigms Sciences IMPDocument34 pagesAOPA Handout NewParadigms Sciences IMPAnup PednekarNo ratings yet
- Neuromuscular Taping For The Upper LimbDocument4 pagesNeuromuscular Taping For The Upper LimbFayza RihastaraNo ratings yet
- Pennsylvania Grand Jury Report of The Life and Death of Danieal KellyDocument263 pagesPennsylvania Grand Jury Report of The Life and Death of Danieal KellyBeverly TranNo ratings yet
- Comparing The Effects of Aquatic and Land-Based Exercises On Balance and Walking in Spastic Diplegic Cerebral Palsy ChildrenDocument8 pagesComparing The Effects of Aquatic and Land-Based Exercises On Balance and Walking in Spastic Diplegic Cerebral Palsy ChildrenJorgeAdalbertoCabralPerezNo ratings yet
- Bouchard HallbergDocument67 pagesBouchard HallbergVioletteNo ratings yet
- (129 136) V9N5PTDocument8 pages(129 136) V9N5PTAqila NurNo ratings yet
- Pediatric Rehabilitation: Cerebral PalsyDocument133 pagesPediatric Rehabilitation: Cerebral PalsyAlfredson Busto Ramirez100% (1)
- 1000-Article Text-2416-1-10-20190906Document14 pages1000-Article Text-2416-1-10-20190906AzisNo ratings yet
- Hip Displacement in Cerebral PalsyDocument9 pagesHip Displacement in Cerebral PalsyJohannesSchoppmannNo ratings yet
- Pediatric Endurance and Limb Strengthening For Children With Cerebral PalsyDocument10 pagesPediatric Endurance and Limb Strengthening For Children With Cerebral PalsysudersonNo ratings yet
- Comorbidities and Their RelatiDocument5 pagesComorbidities and Their RelatiDwi juliana DewiNo ratings yet
- Ways To Improve Balance in Cerebral Palsy PatientsDocument3 pagesWays To Improve Balance in Cerebral Palsy PatientsSakthiVel Ramu100% (1)
- Effectiveness of Sensory Integration Therapy (Vestibular & Proprioception Input) On Gross Motor Functioning in Developmental Delayed and Spastic Diplegic CP ChildrenDocument6 pagesEffectiveness of Sensory Integration Therapy (Vestibular & Proprioception Input) On Gross Motor Functioning in Developmental Delayed and Spastic Diplegic CP ChildrenYanuar Adi SanjayaNo ratings yet