Professional Documents
Culture Documents
NFSC 471-Case Study
Uploaded by
api-242439244Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NFSC 471-Case Study
Uploaded by
api-242439244Copyright:
Available Formats
10/16/2013
Chronic Obstructive Pulmonary Disease (COPD) with Respiratory Failure
Prevalence of COPD
3rd leading cause of death in the United States About 13.5 million people have been diagnosed with COPD in the United States It is estimated an equal number are undiagnosed (1) Kills more women than breast cancer or diabetes (1) COPD is responsible for more than 120,000 deaths per year
By: Amrita Samra & Brittany Fellows
That equals 1 death every four minutes (2)
(1) (2) http://www.healthinaging.org/aging-and-health-a-to-z/topic:copd/ http://www.legislature.mi.gov/%28S%2854i4nn45wqtv1jmc3yhsi13h%29%29/documents/20112012/Journal/House/pdf/2012-HJ-11-28-075.pdf
Incidence COPD in the United States
millions)
(In
Incidences of COPD vary depending on Geographic's
13.1
The incidence 8.9of COPD is on the rise
7.1
10.5
Can you guess why?
Source: U.S Centers for Disease Control and Prevention
Because of the prevalence of smokers
Regions which have the lowest population of smokers also have a lower incidence of COPD
What is COPD?
COPD is an umbrella term used to characterize a group of abnormal inflammatory response in the lungs and partially obstruct airflow
COPD develops over time and continually worsens, lifestyle and medication can slow the progression but the damage is not reversible
Key Signs of COPD - Chronic cough - Increased mucous - Short of breath during physical activities
Key Point Airflow obstruction
10/16/2013
Airflow: Oxygen & Carbon Dioxide
Inspiration: Lung Expands & Diaphragm Contracts Expiration: Lung Relaxes & Diaphragm relaxes
Chronic Bronchitis
Definition: Inflammation of the bronchial mucous membrane, characterized by cough, hypersecretion of mucus, and expectoration of sputum over a long period of time and associated with increased vulnerability to bronchial infection.
Inflammation of the bronchial results in the production of mucus Mucus clogs the airway making it difficult to breath This results in chronic coughing which causes more damage to the bronchial tubes
http://medical-dictionary.thefreedictionary.com/chronic+bronchitis
Oxygen is inhaled through the mouth and nose
Carbon dioxide goes through the capillary membrane and into the alveolar membrane Carbon dioxide continues on through the alveoli to the bronchioles
Goes down pass the trachea into the bronchi
Travels through the bronchioles to the alveoli
Up through the trachea
Through the alveolar membrane to the capillary membrane and into the blood
And exhaled through the mouth and nose
Emphysema
Definition: Emphysema is a chronic respiratory disease where there is overinflation of the air sacs (alveoli) in the lungs, causing a decrease in lung function, and often, breathlessness.
The walls of the alveoli become damaged and lose there elasticity, pockets of air called bullae are formed in damaged areas The damaged areas cause narrowing of the airways, making breathing difficult
COPD is caused by.
Inflammation and damage to lung tissue caused by: Smoking (or 2nd hand) Pollution Genetics Stress
1. J. of Nutritional Biochemistry, Vol23, Issue7
Affecting the ability to exhale first and progressively the ability to inhale
http://medical-dictionary.thefreedictionary.com/emphysema
Symptoms
Cough Wheezing Hemoptysis Chest pain Anorexia Early satiety Weight loss Dyspnea Tachypnea
Anemia Altered taste Fatigue Malaise Depression
Assessing COPD
Preparing Meals Quality of life should be looked into as it pertains to the inability to cook and prepare meals (EAL).
Assessing Body Composition Can be done with BMI as a starting point, should not be the only indicator used for a patients status (EAL).
Assessing Calorie Needs Inflammation increases REE so more calories are needed for the patient (EAL).
http://andevidencelibrary.com/topic.cfm?cat=3708
10/16/2013
Testing for COPD
Spirometry
Mild = >80% Moderate= 50-80% Severe = 30-50% Very Severe =<30%
Medications & Surgery
X-ray ABG
http://www.nlm.nih.gov/medlineplus/ency/article/000091.htm http://copdcanada.ca/understanding_your_numbers.htm
Surgery to remove a damaged part of the lung can be done to help the non-damaged part function normally.
Lung transplant (most severe)
http://www.nlm.nih.gov/medlineplus/ency/article/000091.htm
Management & Prevention
http://www.nlm.nih.gov/medlineplus/ency/article/000091.htm
Respiratory Quotient
Amount of CO2 produced/ amount of O2 consumed For glucose 1.0 For fat 0.7 For protein 0.8 RQ for conversion of glucose to fat >1.0
MNT for COPD
Calories: Increased calorie needs with labored breathing/ malnutrition Overfeeding results in increased difficulty breathing for the patient, requires a balance
Vitamin C Supplementation
Micronutrients: Vitamin C
Grade A Study: Randomized double-blind study done with COPD patients. Experiment: One control group given placebo, One experimental group given ascorbic acid for 14 days; Patients required to write daily symptoms of COPD in diaries Results: Severity of symptoms decreased as experiment went on; Vitamin C supplementation may work to decrease symptoms of COPD
http://web.ebscohost.com.mantis.csuchico.edu/ehost/detail?sid=5a1d0df0-0935-42ef-802d8f2c32193ce6%40sessionmgr113&vid=1&hid=122&bdata=JnNpdGU9ZWhvc3QtbGl2ZQ%3d%3d#db=aph&AN=65430245
Protein: 1.2-1.7 g/kg/ per day
Diet recommendation to balance RQ:
15-20% Protein 30-45% Fat 40-55% CHO
10/16/2013
Vitamin D Supplementation
Micronutrients:Vitamin D Grade C Study: Randomized case-control study done with COPD patients and patients w/out COPD Experiment: COPD patients and non-COPD patients were split into two groups and Vitamin D levels were measured in both Results: COPD patients had severely lower levels of Vitamin D compared to patients w/out COPD
Micronutrients
Smoker: Vitamin C Prevent Osteoporosis: Mg & Ca Mg & Phos (Monitor & supplement if low) Malnutrition & Meds: Vitamin D & K If Cor Pulmonale is present: Fluid restriction
http://web.ebscohost.com.mantis.csuchico.edu/ehost/pdfviewer/pdfviewer?sid=6e2b4b7b-fcde-49cd-afe3a4477db40541%40sessionmgr115&vid=2&hid=122
Patient Information
Patient: Daishi Hayato Age: 65 Sex: Male
Meet Mr. & Mrs. Hayato
Ethnic background: Asian American Household Members: Wife Occupation: Retired manager of local grocery store
Chief Complaint
Patient was working in the yard and became very short of breath. Patients wife then called the doctor and was told to take him to the emergency room immediately.
Medical Diagnosis
Peripheral Vascular Disease with Intermittent Claudication
Acute Respiratory Distress
COPD
10/16/2013
Nutrition Care Process
Assessment Monitoring & Evaluation
Step 1: Assessment
Medical History: COPD secondary to chronic tobacco use, 2 packs per day for 50 years Limited exercise capacity due to dyspnea on exertion Intermittent claudication
Diagnosis
Total dental extraction 5 years ago Emphysema >10 years ago Cholecystectomy 20 years ago
Intervention
Step 1: Assessment
Medication Prior to Hospitalization: Combivent: 2 inhalations 4 times/day Lasix: daily Oxygen: L/hour via nasal cannula at night Risk Screening: Current Smoker: 2 packs per day for 50 years Allergies: Penicillin
Step 1: Assessment
Patient Report: General appetite is only fair Breakfast is normally his largest meal Appetite has decreased for past several weeks
Usual Dietary Intake: AM: Egg, hot cereal or muffin, and hot tea with milk and sugar Lunch: Soup, sandwich, and hot tea with milk and sugar Dinner: Small amount of meat, rice, 2-3 kinds of vegetables, and hot tea with milk and sugar
24-Hour Recall: 2 scrambled eggs, few bites of Cream of Wheat, sips of hot tea, bite of toast Ate nothing rest of day- sips of hot tea
Step 1: Physical Examination
General Appearance: Acutely dyspneic in acute respiratory distress Heart Rate: 118bpm (slightly elevated) Throat: trachea is shifted to the right Extremities: Cyanosis, with 1 + Edema Skin: Warm, dry to touch Chest/Lungs: harsh breath sounds over right chest w/absent sound on left side, use of accessory muscles at rest
Anthropometric Data
Weight: 122lbs 55kg Height: 54 64in. 163cm Usual Body Weight: 135lbs Ideal Body Weight: 130lbs 59kg Body Mass Index: 21 (Normal) Percent Ideal Body Weight: 90%(Adequate E stores) Percent Usual Body Weight: 94% (Normal)
Calories: 66.5+(13.8x59kg)+(5x163cm) (6.8x65)= 1253.5 1253.5 X 1.3 X 1.4= 2281 kcals/day Based on Body Weight 1,475 2065 Kcals
Protein: 59kg x 1.6g/kg /protein per day= 94.4g of Protein/day
10/16/2013
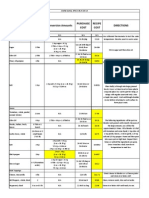
Laboratory Analysis
Acidosis Anemia Hemoglobin = 13.2(L) Anemia Hematocrit= 39(L) Anemia Transferrin 173(L) Result of low pH Anemia
Hospital Course Story
Chest tube was inserted into the left thorax with drainage under suction. The oropharynx was cleared. The patient was placed on ventilator with high flow oxygen, 15 breaths/min with an FiO2 of 100%. Day 2: Enteral feedings initiated, however due to high residuals the patient was started on ProcalAmine. Day 4: Enteral feedings restarted Day 5: ProcalAmine discontinued Day 8: Enteral feedings discontinued and patient was weaned from ventilator Day 11: Discharged home Day 12: Patient meets with his new RDs
Serum Protein Albumin= 3.5 (Low end) PEM Prealbumin= 17 (Low end) PEM
ph = 7.22(L) Acidosis pCO2 = 66(H) Hypoventilation Acidosis pO2 = 57(L) Respiratory Failure HCO3(bicarbonate) = 37(H)
Step 2: Diagnosis
Step 3: Intervention
Nutrition Education: Recommended modifications (E-1.4) - Increase fat and protein, decrease carbohydrate - Small frequent meals
Inadequate energy intake (NI-1.4) related to shortness of breath and early satiety as evidenced by unintended weight loss, 24-hour recall, and patient report.
Nutrition Education: Nutrition relationship to health/ disease (E-1.4) - Education on smoking, exercise, & nutrition
Coordination of Nutrition Care: Referral to community agencies (RC-1.4) -COPD support group/ Smoking support group
Nutrition Counseling: Social support (C-2.4) - Educate & Counsel patients wife on important modifications
Implementing Intervention
Recommended Modifications
We educated the patient on the importance of small frequent meals throughout the day to increase oral intake. Also educating the patient on the importance of high fat & protein and low carbohydrate to help manage oxygen levels.
Patients Goals
After educating the patient and his wife on the importance of nutrition and lifestyle modifications the patient set personal goals to achieve such modifications. Goal 1: The patient and his wife agreed that every two hours she would offer a calorie dense meal, using the handout of high calorie recipes. Goal 2: The patient also decided to attend COPD & smoking support groups every other week for one month. Barriers: The patients primary barrier was giving up smoking and does not wish to modify behavior at this time, but will supplement vitamin C as long as he continues to smoke. The patient was also concerned with tolerance of additional feedings, and agreed to trying oxygen support during meals if needed.
Nutrition Relationship to Disease
Educated the patient on the relationship between smoking and the progression of COPD. Educated the patient on the benefits of exercise on dyspnea
Referral to Community Agencies
Refer patient to community support groups for COPD & smoking.
Social Support
Educated the wife about the importance of nutrition and calorie dense food choice Answering any questions or concerns she had
10/16/2013
Action goals
Small frequent meals High fat & protein Low carbohydrate COPD/Smoking support group If trouble tolerating increased meals add oxygen during meal If continues smoking supplement vitamin C
Short Term Goals: Outcome goals
Increase fat & protein
Increase overall kcals consumed orally Stabilize RQ value Decrease dyspnea at meal time
Long Term Outcome Goals
Education Materials
Prevent malnutrition Prevent PEM Minimize progression of COPD
Simple recipes for increasing fat & protein Tips for decreasing dyspnea
Scope ofIs Practice Tree This In Our Scope Requested Act or Service Of Practice?
1. Is it permitted? No or Not Sure Yes
Monitoring & Evaluating
Anthropometric: Dry weight: biweekly Laboratory Analysis: Albumin & Prealbumin: biweekly pH, pCO2, pO2, HCO3-: biweekly Vitamin & Mineral Status: C, D, K, Mg, Ca++, Phos: Once a month Evaluate patients understanding and adherence through biweekly appointments. Using motivational interviewing to understand our patients ability and confidence to maintain changes. Assess barriers and patient concerns
2. Is it covered by any national or organizational explicit guidance? No
Yes 3. Would it be reasonable for a dietetics practitioner to do? No 5. Can I demonstrate the knowledge, skill, and competence? Yes No
Yes
4. Do I personally have the education needed? Yes
No
STOP Until additiona l educatio n acquired Proceed if authorization documented
STOP Performance of activity or service may place dietetics practitioner and client at risk!
STOP Until current knowledge, skill, and competence demonstrated
STOP The accountability is not assumed! Notify appropriate person(s)
No
6. Do I accept responsibility and accountability for my Yes actions?
10/16/2013
Follow up Recommendations
Follow up biweekly with outpatient RD Support groups available weekly for COPD Support & Smoking sensation support
Approximately every four minutes someone dies from COPD
Approximately seven people died of COPD during this presentation
References
http://pats.atsjournals.org/content/8/4/363.full http://www.sciencedirect.com/science/article/pii/S095528631100132X
http://andevidencelibrary.com/topic.cfm?cat=3708
http://web.ebscohost.com.mantis.csuchico.edu/ehost/pdfviewer/pdfviewer?sid=6e2b4b7b-fcde-49cd-afe3a4477db40541%40sessionmgr115&vid=2&hid=122
http://web.ebscohost.com.mantis.csuchico.edu/ehost/detail?sid=5a1d0df0-0935-42ef-802d8f2c32193ce6%40sessionmgr113&vid=1&hid=122&bdata=JnNpdGU9ZWhvc3QtbGl2ZQ%3d%3d#db=aph&AN=65430245 http://www.nlm.nih.gov/medlineplus/ency/article/000091.htm http://copdcanada.ca/understanding_your_numbers.htm http://medical-dictionary.thefreedictionary.com/emphysema
You might also like
- PT Case: Copd Exacerbation: DedicationDocument10 pagesPT Case: Copd Exacerbation: DedicationDianaLopezBorjaNo ratings yet
- Copd PDFDocument28 pagesCopd PDFDarawan MirzaNo ratings yet
- Case 3 - Copd With Respiratory FailureDocument13 pagesCase 3 - Copd With Respiratory FailureFatima SadiqNo ratings yet
- COPD Nursing Care GuideDocument16 pagesCOPD Nursing Care GuideJay-ar Zars0% (1)
- Hide 1 Description 2 Classification 2.1 Chronic Bronchitis 2.2 Emphysema 3 Pathophysiology 4 EpidemiologyDocument29 pagesHide 1 Description 2 Classification 2.1 Chronic Bronchitis 2.2 Emphysema 3 Pathophysiology 4 EpidemiologyAngie Mandeoya100% (1)
- Multidisciplinary Case-Based Teaching: Prof. S. O 'Neill Dr. D. Royston Dr. S. ShaikhDocument90 pagesMultidisciplinary Case-Based Teaching: Prof. S. O 'Neill Dr. D. Royston Dr. S. Shaikhmynoidanh19No ratings yet
- Plenary Discussion Scenario 3Document8 pagesPlenary Discussion Scenario 3RifaiNo ratings yet
- COPD Case PresentationDocument78 pagesCOPD Case PresentationMaria Rogine ElopreNo ratings yet
- What Is A LobectomyDocument6 pagesWhat Is A LobectomyMaria Carmela TormesNo ratings yet
- COPD Nursing Questions: Key Teaching Points for PatientsDocument9 pagesCOPD Nursing Questions: Key Teaching Points for PatientsJay-ar ZarsNo ratings yet
- Cystic Fibrosis Nursing Care PlanDocument27 pagesCystic Fibrosis Nursing Care PlanAbdelrahman AlshatnawiNo ratings yet
- COPD Case Pres2Document29 pagesCOPD Case Pres2Kelly Queenie Andres100% (1)
- COPDDocument52 pagesCOPDswapnil3250No ratings yet
- Cognitive Concept Map - Case of The Week - USMLE Genetics - All About Cystic Fibrosis (CF) - DR Kumar Ponnusamy & DR Jegathambigai RNDocument2 pagesCognitive Concept Map - Case of The Week - USMLE Genetics - All About Cystic Fibrosis (CF) - DR Kumar Ponnusamy & DR Jegathambigai RNPonnusamy KumarNo ratings yet
- D5W Uses and Side EffectsDocument4 pagesD5W Uses and Side EffectsHanilyn ArdinaNo ratings yet
- COPD and Diverticulitis QuestionsDocument57 pagesCOPD and Diverticulitis Questionsjabunn7487No ratings yet
- Copd Case StudyDocument6 pagesCopd Case StudyChrischia Yvonne GualbertoNo ratings yet
- Nutrition and COPD - Dietary Considerations For Better BreathingDocument3 pagesNutrition and COPD - Dietary Considerations For Better BreathingReina NoviaNo ratings yet
- Patient Prep: Follow Guidelines On P. 65 of Clinical PacketDocument4 pagesPatient Prep: Follow Guidelines On P. 65 of Clinical PacketKatherine AmbrosiaNo ratings yet
- Pneumonia Diagnosis GuideDocument6 pagesPneumonia Diagnosis GuideMa Clara MolinaNo ratings yet
- A Case Presentation On Chronic Obstructive Disease (COPD)Document18 pagesA Case Presentation On Chronic Obstructive Disease (COPD)Harvey T. Dato-onNo ratings yet
- Chronic Illness Module OutcomesDocument12 pagesChronic Illness Module OutcomesOmar IzzoNo ratings yet
- Case Study: Chronic Obstructive Pulmonary DiseaseDocument13 pagesCase Study: Chronic Obstructive Pulmonary DiseaseJohn Vincent Canillas PedregozaNo ratings yet
- Final Case UutDocument31 pagesFinal Case Uutkelakar unandNo ratings yet
- Our Lady of Fatima University - ValenzuelaDocument3 pagesOur Lady of Fatima University - ValenzuelaMeriam Estepa MartinezNo ratings yet
- COPD Notes DownloadDocument5 pagesCOPD Notes DownloadJubitta JobyNo ratings yet
- CASE PRESENTATIONDocument34 pagesCASE PRESENTATIONPhilbert Russell Del ValleNo ratings yet
- North South UniversityDocument11 pagesNorth South UniversityChaudhuri Misavvir Asif 2122170630No ratings yet
- Jcom Nov99 BronchDocument10 pagesJcom Nov99 BronchheartbcglNo ratings yet
- Copd HandoutDocument6 pagesCopd Handoutapi-272951876No ratings yet
- Pneumonia Case Study: Toddler Diagnosis and TreatmentDocument5 pagesPneumonia Case Study: Toddler Diagnosis and TreatmentcrisolandNo ratings yet
- Chronic Obstructive Pulmonary Disease (COPD) Is A Condition ofDocument12 pagesChronic Obstructive Pulmonary Disease (COPD) Is A Condition ofDiana Jalaynie S. SambolawanNo ratings yet
- Chronic Obstructive Pulmonary Disease (COPD) Is A Condition ofDocument12 pagesChronic Obstructive Pulmonary Disease (COPD) Is A Condition ofDiana Jalaynie S. SambolawanNo ratings yet
- DearDocument21 pagesDearLouresa Mae TNo ratings yet
- 100 Item Quiz 401Document21 pages100 Item Quiz 401Sheryl Anne GonzagaNo ratings yet
- COPD: Chronic Obstructive Pulmonary Disease ExplainedDocument15 pagesCOPD: Chronic Obstructive Pulmonary Disease Explainedrmarty_35No ratings yet
- Chronic Obstructive Pulmonary DiseaseDocument8 pagesChronic Obstructive Pulmonary DiseaseYessamin Paith RoderosNo ratings yet
- Case Study PneumoniaDocument8 pagesCase Study PneumoniaThesa FedericoNo ratings yet
- COPDDocument49 pagesCOPDArmoured SpartanNo ratings yet
- COPD Case StudyDocument22 pagesCOPD Case StudyAnonymous HNTNhspNo ratings yet
- SepsisDocument11 pagesSepsisesha.k35No ratings yet
- ASN 11 Handout Case Study PDFDocument4 pagesASN 11 Handout Case Study PDFania ojedaNo ratings yet
- COPD ExacerbationDocument12 pagesCOPD ExacerbationJeffrey ShermanNo ratings yet
- Practice EamDocument35 pagesPractice EamMYKRISTIE JHO MENDEZNo ratings yet
- Young Child with Acute Respiratory DistressDocument25 pagesYoung Child with Acute Respiratory Distresspriyarajan007100% (2)
- Pediatric Community Acquired Pneumonia Case StudyDocument17 pagesPediatric Community Acquired Pneumonia Case StudyMary Ann Credo Manlangit100% (2)
- Myeloperoxidase and Protein Oxidation in The Airways of Young Children With Cystic FibrosisDocument7 pagesMyeloperoxidase and Protein Oxidation in The Airways of Young Children With Cystic FibrosisMichael StudiofourteenohnineNo ratings yet
- Study Guide Example PDFDocument18 pagesStudy Guide Example PDFmrmr92No ratings yet
- Nutrition and Respiratory Diseases PDFDocument53 pagesNutrition and Respiratory Diseases PDFliggiedy100% (1)
- COPD - Salmorin & SatairapanDocument13 pagesCOPD - Salmorin & SatairapanMichelle SatairapanNo ratings yet
- Competencymr McdougalcopdDocument17 pagesCompetencymr Mcdougalcopdmac_rymrt7569No ratings yet
- Dr-Sang Internal Med Presentatn (Autosaved)Document27 pagesDr-Sang Internal Med Presentatn (Autosaved)Shitanjni WatiNo ratings yet
- Written Case Presentation 2Document21 pagesWritten Case Presentation 2api-283248618No ratings yet
- Pneumonia Case StudyDocument8 pagesPneumonia Case StudyChristopher John AgueloNo ratings yet
- Pathophysiology and Management of COPDDocument6 pagesPathophysiology and Management of COPDNeil Andro Marcelo100% (1)
- Management of COPD in Primary and Secondary Care, TheFrom EverandManagement of COPD in Primary and Secondary Care, TheRating: 5 out of 5 stars5/5 (1)
- Pulmonary Fibrosis, (Lung Scarring) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandPulmonary Fibrosis, (Lung Scarring) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- 440 ReflectionDocument1 page440 Reflectionapi-242439244No ratings yet
- 365 Reflection 2Document1 page365 Reflection 2api-242439244No ratings yet
- 465 ReflectionDocument1 page465 Reflectionapi-242439244No ratings yet
- 431 ReflectionDocument1 page431 Reflectionapi-242439244No ratings yet
- 365 Reflection 2Document1 page365 Reflection 2api-242439244No ratings yet
- 431 Reflection 2Document1 page431 Reflection 2api-242439244No ratings yet
- 430 ReflectionDocument1 page430 Reflectionapi-242439244No ratings yet
- 470 ReflectionDocument1 page470 Reflectionapi-242439244No ratings yet
- NFSC 403-Finalcase StudyDocument5 pagesNFSC 403-Finalcase Studyapi-242439244No ratings yet
- 457 ResumeDocument1 page457 Resumeapi-242439244No ratings yet
- 471 ReflectionDocument1 page471 Reflectionapi-242439244No ratings yet
- NFSC 431-Logic ModelDocument3 pagesNFSC 431-Logic Modelapi-242439244No ratings yet
- Nfsc440-And Evidence Analysis WorksheetDocument5 pagesNfsc440-And Evidence Analysis Worksheetapi-242439244No ratings yet
- NFSC 430-Recipe Costing 2Document2 pagesNFSC 430-Recipe Costing 2api-242439244No ratings yet
- Nfsc470-Case StudyDocument11 pagesNfsc470-Case Studyapi-242439244No ratings yet
- Ariston Oven ManualDocument16 pagesAriston Oven ManualJoanne JoanneNo ratings yet
- David Emmett & Graeme Nice - What You Need To Know About Cannabis - Understanding The FactsDocument120 pagesDavid Emmett & Graeme Nice - What You Need To Know About Cannabis - Understanding The FactsJovana StojkovićNo ratings yet
- VET PREVENTIVE MEDICINE EXAMDocument8 pagesVET PREVENTIVE MEDICINE EXAMashish kumarNo ratings yet
- 2 Obligations General Provisions 1156 1162Document15 pages2 Obligations General Provisions 1156 1162Emanuel CenidozaNo ratings yet
- c350 Troubleshooting Guide PDFDocument94 pagesc350 Troubleshooting Guide PDFPaula Rosal SittlerNo ratings yet
- Baldwin 1e Ch14 PPT FINAL AccessibleDocument29 pagesBaldwin 1e Ch14 PPT FINAL AccessibleA BlessNo ratings yet
- Amgen Inc. v. F. Hoffmann-LaRoche LTD Et Al - Document No. 423Document19 pagesAmgen Inc. v. F. Hoffmann-LaRoche LTD Et Al - Document No. 423Justia.comNo ratings yet
- Lawson v. Mabrie Lawsuit About Botched Funeral Service - October 2014Document9 pagesLawson v. Mabrie Lawsuit About Botched Funeral Service - October 2014cindy_georgeNo ratings yet
- Pengayaan Inisiasi 6-SynonymyDocument35 pagesPengayaan Inisiasi 6-SynonymyAriNo ratings yet
- City of Manila vs. Hon CaridadDocument2 pagesCity of Manila vs. Hon CaridadkelbingeNo ratings yet
- UCO Reporter 2021, December Edition, November 26, 2021Document40 pagesUCO Reporter 2021, December Edition, November 26, 2021ucopresident100% (2)
- NGOs Affiliated To SWCDocument2,555 pagesNGOs Affiliated To SWCMandip marasiniNo ratings yet
- MATHS UNDERSTANDINGDocument15 pagesMATHS UNDERSTANDINGNurul IzzaNo ratings yet
- Einstein Quotes On SpiritualityDocument2 pagesEinstein Quotes On Spiritualitybob jamesNo ratings yet
- Additional Practice Questions on Bonding and Mechanical Properties of MaterialsDocument26 pagesAdditional Practice Questions on Bonding and Mechanical Properties of MaterialsYeo JosephNo ratings yet
- Facebook Use Case Diagram Activity Diagram Sequence DiagramDocument21 pagesFacebook Use Case Diagram Activity Diagram Sequence DiagramSaiNo ratings yet
- FedSupport Codebook FY2020Document259 pagesFedSupport Codebook FY2020Aaron BlackmonNo ratings yet
- Yoga For The Primary Prevention of Cardiovascular Disease (Hartley 2014)Document52 pagesYoga For The Primary Prevention of Cardiovascular Disease (Hartley 2014)Marcelo NorisNo ratings yet
- Test Initial Engleza A 8a Cu Matrice Si BaremDocument4 pagesTest Initial Engleza A 8a Cu Matrice Si BaremTatiana BeileșenNo ratings yet
- ICE Professional Review GuidanceDocument23 pagesICE Professional Review Guidancerahulgehlot2008No ratings yet
- Marketing Case Study - MM1 (EPGPX02, GROUP-06)Document5 pagesMarketing Case Study - MM1 (EPGPX02, GROUP-06)kaushal dhapareNo ratings yet
- Council Of Architecture Scale Of ChargesDocument4 pagesCouncil Of Architecture Scale Of ChargesAshwin RajendranNo ratings yet
- Munslow, A. What History IsDocument2 pagesMunslow, A. What History IsGoshai DaianNo ratings yet
- Best Practices in Implementing A Secure Microservices ArchitectureDocument85 pagesBest Practices in Implementing A Secure Microservices Architecturewenapo100% (1)
- Rational design of Nile bargesDocument8 pagesRational design of Nile bargesjhairNo ratings yet
- Java Thread Priority in MultithreadingDocument3 pagesJava Thread Priority in MultithreadingMITALI SHARMANo ratings yet
- Shell Rimula R7 AD 5W-30: Performance, Features & Benefits Main ApplicationsDocument2 pagesShell Rimula R7 AD 5W-30: Performance, Features & Benefits Main ApplicationsAji WibowoNo ratings yet
- Igbo Traditional Security System: A Panacea To Nigeria Security QuagmireDocument17 pagesIgbo Traditional Security System: A Panacea To Nigeria Security QuagmireChukwukadibia E. Nwafor100% (1)
- MICROHARDNESS TESTER HMV-2 - SeriesDocument9 pagesMICROHARDNESS TESTER HMV-2 - SeriesRicoNo ratings yet
- Ganuelas v. CawedDocument4 pagesGanuelas v. CawedHanna AlfantaNo ratings yet