Professional Documents
Culture Documents
Nursing Care Plan For Ineffective Tissue Perfusion
Uploaded by
brenhoodOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nursing Care Plan For Ineffective Tissue Perfusion
Uploaded by
brenhoodCopyright:
Available Formats
STUDENT NAME CLINICAL DATE
Section 1: Physical Assessment
DATE/TIME INITIAL ASSESSMENT 11/09/09 Date/Time* Possible Related Nursing
Explanation of Diagnoses
CHIEF COMPLAINT: Peripheral Vascular Disease Abnormal
PAST MEDICAL HISTORY: CHF, Peripheral Vascular disease, IDDM, Seizure disorder, Assessment Factors
anxiety disorder, Osteoarthritis, Malignant Neoplasm Prostate, Depressive disorder,
hyperlipidema, hypothyroidism, Hypokalemia
ALLERGIES:NKA
PAST SURGICAL HISTORY: Total Knee Replacement (rt knee)
Thin Obese Emaciated Well-developed Well-nourished No Acute Distress 11/09/09 1330 Latex Allergy Response
Height 5'8" Weight 271.3 BMI 41.2 Systolic BP was Latex Allergy Response,
Admitting Vital Signs BP: 154/71, PULSE: 84, PAIN: 0, RESP.: 18 , TEMP: 95.9 elevated. Risk for
Today’s Vital Signs BP: 128/60, PULSE: 80, PAIN: 0, RESP: 20, TEMP: 97 11/10/09 Stated that
BP was usually low in
the morning.
I. PHYSIOLOGIC ASSESSMENT
A. OXYGENATION
1. BREATHING Gordon’s Pattern of Activity and Exercise Airway Clearance, Ineffective
Respiratory Rate 20 Rhythm: Regular Irregular 11/10/09 0730 Aspiration, Risk for
Depth: Deep Shallow Stated had pneumonia Breathing Pattern, Ineffective
No distress Dyspneic Apneic sec. Gas Exchange, Impaired
a few weeks ago. No
Labored Accessory muscle use Tachypneic information found in the Infection, Risk for
Sudden Infant Death Syndrome,
medical record.
BREATH SOUNDS/LOCATION of FINDINGS Risk for
Cl -Clear Pleural Rub Suffocation, Risk for
Cr -Crackles Rh- Rhonci Ventilation, Impaired,
Wh –Wheezing R- Rales Spontaneous
D -Decreased Ventilatory Weaning
A -Absent Response, Dysfunctional
Oxygen Therapy:
RA FiO2 L / or % NC Mask Trach Other
O2 Saturation: N/A q hr Continuous pulse oximeter
Pulse Oximetry Readings (Identify on R.A. or O2): _; _;
Chest Config: Symmetrical Asymmetrical Flail
Cough: No cough Weak Strong Frequent Infrequent
Nonproductive Productive Description:
Color Odor Viscosity Incentive Spirometer
Shape of Chest: AP diameter 1:2, barrel, pectus excavatum,
(highlight or document) kyphotic; other
Drainage: Chest Tube/Pleuravac: R L Water seal only
Suction cm of water N/A
Medications R/T Breathing: Yes No Type
2. CIRCULATION Gordon’s Pattern of Activity and Exercise Cardiac Output, Decreased
Heart Rate (Radial Pulse) 80 Rhythm Irregular 11/09/09 1330 Fluid Balance, Readiness for
Heart Sounds: Describe chest area:barely audible/ No murmurs detected. At brachial Enhanced
2+Pitting edema RLE,
artery: Lub dub, pause, lub pause dub, lub dub Fluid Volume Deficit
and R/L ankles.
Neck Veins (45o angle): Flat Distended Fluid Volume Excess
11/10/09 0715
BP: R128/60 L 130/62 Apical Pulse:UTA D – Doppler Fluid Volume, Risk for Deficit
A – Absent Upon auscultation of
Arterial 1+ - Barely Palpable Fluid Volume, Risk for
DP 2+ - Weak the brachial artery, the Imbalanced
Pulses C B R F PT 3+ - Normal
4+ - Full Bounding heart sounds were Tissue Perfusion, Ineffective
irregular. (specify: renal, cerebral,
Right/
2+ Pitting edema cardiopulmonary,
Left 3+ 3+ 3+ 3+ A A
R/L LE 3+ pitting gastrointestinal, peripheral)
Capillary Refill: Brisk <3 sec. Prolonged >3 sec. sec.
edema both ankles.
Nail bed Color: Pink Pale Cyanotic
Chest Pain: No Yes Describe
Edema: None Generalized Non-pitting Pitting 1 + 2+ 3+ 4+
Other
Location L/R LE, (R/L ankles 3+) (R/L LE: 2+ )
WOSC Freshman Clinical Assessment Form -1-
Pacemaker: N/A Permanent Type Has a history of
External Rate Ischemic heart
Location: disease, CHF,
Peripheral Vascular
Disease, and
hypertension. Bilateral
pedal pulses were
absent
2. CIRCULATION (Continued) Date/Time Related Nursing Diagnoses
Explanation of
Abnormal
Assessment Factors
Homan’s sign: Left: pos. neg. Right: pos. neg.
Calf redness/tenderness: Left: yes no Right: yes no
Anti-embolism stockings: N/A Remove/Replaced q shift
Sequential compression device: N/A Remove/Replaced q shift
Other
IV’s / INVASIVE LINE MONITORING
Type/Port ID** Solution Rate Dosage Location Site Code*
NONE
*SITE CODE: **ID INFUSION DEVICE:
C - Clear p - pump
S - Swelling pca+ - PCA
R - Redness g - gravity
I - Inflamed
DI - Dsg Dry & Intact
Medications R/T Circulation: Yes No Type Asprin 325mg QD, Lopressor
50mg PO q12h, Zaroxolyn 10mg po QD, Lasix 40mg po QD, ,Nitroglycerin 0.4mg
subling, Q 5minx3 PRN Chest pain
3. NEUROLOGICAL 11/10/09 0715 Confusion, Acute
Has a history of Confusion, Chronic
Level Of Consciousness:
Awake Alert Oriented x 4 (time, place, person, event) seizures. Environmental Interpretation
Syndrome, Impaired
Restless Drowsy Sedated Confused
Infant Behavior, Disorganized
Glasgow Coma Scale: Infant Behavior, Readiness for
a) Best eye opening: 4 Spontaneously 3 To Speech 2 To Pain 1 None Enhanced Organized
b) Best verbal response: 5 Oriented 4 Confused Infant Behavior, Risk for
3 Inappropriate words 2 Incomprehensible sounds 1 None Disorganized
Intracranial, Decreased Adaptive
c) Best motor response: 6 Obeys commands 5 Localizes to pain
Capacity
4 Withdraws 3 Flexion (decorticate)
Memory, Impaired
2 Extension (decerebrate) 1 None
Thought Processes, Disturbed
Total Glasgow Coma Scale 15 / 15 (Add a, b, c above)
PERRL Pinpoint Fixed
Dilated, but reactive to light Dilated, nonreactive
Unequal: R>L L>R Dolls eyes Other
Brain Stem Signs:N/A (+/-) cough gag corneal Babinski
Communication: Verbal Writes notes Mouths words
Nods head appropriately to yes/no questions
Medications R/T Neurological Condition: Yes No Type Topamax 100mg po QD ,
Lamictal 50mg po bid ,
4. NEUROVASCULAR 11/10/09 0715
WOSC Freshman Clinical Assessment Form -2-
Extremities Examined: U/LE CSM q hr Partial loss of voluntary Dysreflexia, Autonomic
Traction/Cast: N/A Type movement of Dysreflexia, Risk for
Color: Pink Reddened Blue Blanched upper/lower extremities Autonomic
Temperature: Cool Warm Hot Rt side weakness Peripheral Neurovascular
Movement: Active Passive Limited LE cool to touch, shiny, Dysfunction, Risk for
Sensation: Numbness Tingling Pain waxy appearance; UE
Restraints: N/A Type CSM q hr warm. Venous Stasis
Restraint Protocol Instituted Remove/Replaced q shift noted. States feet and
legs are numb and
tingly.
B. NUTRITION Gordon’s Nutritional-Metabolic Pattern Date/Time Related Nursing Diagnoses
Explanation of
Abnormal
Assessment Factors
Abdomen: Soft Firm Hard Tender Distended cm. 11/10/09 0730 Breastfeeding, Effective
Breastfeeding, Ineffective
Bowel Sounds: Active Hyper Hypo Absent Abdomen is Breastfeeding, Interrupted
Flatus: Yes No distended. Dentition, Impaired
Diet: Type ADA/ LOW SODIUM NPO TPN Tube feeding ADA diet r/t IDDM, Failure to Thrive, Adult
Meal: Breakfast Lunch Dinner % taken 100% taken Fluid Volume, Deficit
and low sodium diet
Fluid Volume, Deficit, Risk for
Type gastric tube N/A Placement Verified r/t hypretension/ heart Infant Feeding Pattern,
Purpose: Feeding Decompression Other failure Ineffective
Formula: Type Rate cc’s q hrs N/A Pt is Obese, stated Nausea
Suction: N/A Intermittent Low continuous that he has gained Nutrition: Imbalanced, Risk for
Drainage: Describe More Than Body
alot of weight in the
Requirements
Mucous Membranes: Moist Dry Cracked Sores Patches past few months. Nutrition: Imbalanced, Less
Pink Dusky Other Than Body Requirements
Dentures: Full Upper Lower N/A Stated that he Nutrition: Imbalanced, More
Than Body Requirements
Diet toleration: Anorexia Nausea Vomiting sometimes sneaks
Nutrition, Readiness for Enhanced
Weight Loss: Amount Time Period N/A food that he is not Oral Mucous Membranes,
24o Intake UTA 24o Output UTA Balance: Positive Negative supposed to eat. Impaired
Blood Glucose Monitoring q 4 hrs Time/Result 1130 227 N/A Self-Care Deficit, Feeding
Self-feed Assist-feed Swallowing precautions Swallowing, Impaired
FSBS 227
Medications R/T Nutrition: Yes No Type Magnesium chloride 128mg po QD,
Potassium bicarbonate 120mEq liq po QID,Sitagliptin 50mg po QD, glyBuride 10mg QAM
0800, Novolog (sliding scale)
C. ELIMINATION Gordon’s Pattern of Elimination 11/10/09 0800 Constipation
Constipation, Perceived
1. BOWEL Prescribed several
Constipation, Risk for
Stool: Formed Loose Impacted Last BM 11/10/09 medications that have Diarrhea
Color: brown Regular Irregular constipation as a Incontinence, Bowel
possible side effect. Nausea
Outlet: Rectum Colostomy Ileostomy Rectal Tube Fistula Takes several
Output: Tube Drainage cc’s Describe: N/A medications to
Stoma: N/A Pink Edema Dusky prevent constipation.
Surrounding Skin: D/I Excoriated Other
Toileting: Self Assist History Laxative Use: No Yes
Medications R/T Bowel: Yes No Type Milk of Mag suspension 30 cc liq po QD
PRN, Dulcolax 1 suppository rectally QD PRN, Colace 200mg po bid, miralax 17gm po
bid,
2. URINARY 11/10/09 0700 Fluid Volume, Risk for
Imbalanced
GU Drainage: Voiding Straight Catheter q hrs Incontinent most of Infection, Risk for
Indwelling Foley 3-way cath (irrigation) the time, but tries to Incontinence, Functional
External cath Other use a urinal. States Incontinence, Reflex
Other: Bladder Training Catheter Care Hourly Urine Output that he has to “pee a Incontinence, Risk for Urge
Bladder Irrigation: Continuous Manual Solution: Incontinence, Stress
lot” at night. (nocturia)
Incontinence, Total
Urine: Clear Cloudy Sediment Odor: Faint Offensive Has a history of Incontinence, Urge
Color: Light Yellow Dark Yellow Orange Clots Hematuria malignant neoplasm Tissue Perfusion, Ineffective
Patterns: Incontinent Polyuria Nocturia Oliguria Urgency prostate. Urinary Elimination, Impaired
Dysuria Retention Anuria Other Urinary Elimination, Readiness
for Enhanced
Genitalia: No Anomalies Discharge Excoriation Other Urinary Retention
Medications R/T Bladder: Yes No Type Detrol LA 4mg po QD
D. ACTIVITY/REST Gordon’s Pattern of Activity and Rest/ Pattern of Sleep & Rest
WOSC Freshman Clinical Assessment Form -3-
Range of Motion: Active Passive Limitations Activity Intolerance
11/10/09 0730
Activity Intolerance, Risk for
Bed Mobility: Self Assist: Partial Total Unable to perform Disuse Syndrome, Risk for
Assistive Devices: Type Wheel chair N/A active ROM. Diversional Activity Deficient
CPM: Right Left N/A Fatigue
Stated that he Mobility, Impaired Bed
Joints: Tenderness Pain Swelling No abnormalities sometimes has pain, Mobility, Impaired Physical
Ordered Activity level: swelling, and Mobility, Impaired Wheelchair
Sleep Patterns: Usual # Hours 3 to 4 hrs # Last 24 hours 4hrs tenderness in joints, Perioperative Positioning
Injury, Risk for
Special Needs: but that he was not in
Sedentary Lifestyle
Medications R/T Activity/Rest: Yes No Type Ambien 5mg po qhs x’s 60days pain at the moment. Sleep Deprivation
Diagnosed with Sleep Pattern, Disturbed
insomnia. States Sleep, Readiness for Enhanced
Transfer Ability, Impaired
sometimes has a hard Walking, Impaired
time sleeping.
WOSC Freshman Clinical Assessment Form -4-
E. Comfort Date/Time Related Nursing Diagnosis
Explanation of
Abnormal
Assessment
Factors
11/10/09 0745 Comfort
Pain/Discomfort: No Yes Describe:
States that he Pain, Acute
Pain Scale: (0-10) 0 Last Medicated:
sometimes has Pain, Chronic
Location:
pain in his LE.
Quality: Sexual
PRN Analgesic/Narcotic PCA Epidural Sexuality Patter, Ineffective
Other Modalities: Sexual Dysfunction
Safety and Security
Medications R/T Comfort: Yes No Type Robaxin 500mg po q8h PRN
spasms ,Lortab 5mg q4h PRN pain, Tylenol 325mg q4h PRN pain Temperature
Hyperthermia
F. SEXUAL Gordon’s sexuality-Reproductive Pattern Hypothermia
Reproductive: LMP______ Premenopausal Postmenopausal Male Temperature, Risk for
Hysterectomy: Ovaries Removed Ovary/Ovaries Remain Imbalanced body
Breast: Symmetrical Asymmetrical Describe: Thermoregulation, Ineffective
Self Breast/Testicle Exams: Yes No Freq: Skin
Cancer Screen: Date 5/09 Test prostate cancer Result malignant Infection, Risk for
Date Test Result (Breast, Pap, Prostate)
Sexual/Fertility Concerns None
Injury, Risk for
Hormone Replacement None for sexuality Latex Allergy Response
Latex Allergy Response, Risk for
Medications Related to Sexuality: Yes No Type: Protection, Ineffective
II. SAFETY AND SECURITY 11/10/09 0700 Skin Integrity, Impaired
Needs assistance Skin Integrity, impaired, Risk for
Temperature: 97 w/dressing, total Tissue Integrity, Impaired
Route Taken: Oral Tympanic Ax. Rectal Temporal assistance w/ Physical
toileting, personal Falls, Risk for
hygiene, and
Skin: Turgor: Location:sternum Elastic Tented Taut Shiny Growth, Risk for disproportional
bathing.
Temp: Hot Warm Cool Dry Clammy Diaphoretic Mobility, Impaired Physical
Color: Location: face Pink Pale Cyanotic Perioperative Positioning Injury,
Flushed Jaundiced Mottled Other Brown Risk for
Bony Prominences: Skin Intact Reddened Gray Trauma, Risk for
Pressure Sore Stage: Location: Self-Care Deficit,
Bathing/Hygiene
Wound Location : NONE Self-Care Deficit,
Wound: N/A Sutures Staples Drain Dehiscence Dressing/Grooming
Evisceration Healing by secondary intention Other Self-care Deficit, Toileting
Dressing: N/A Dry/Intact Open to Air Stained Saturated Surgical Recovery, Delayed
Changed: q______hrs wet to dry Other Describe: Wandering
Perception
Isolation/Precautions: Standard Precautions Additional fd Energy Field, Disturbed
Protocols: Braden Scale Restraints Special Bed Other Environmental Interpretation
Physical: Syndrome, Impaired
General Unassisted Supervised Assisted Unable Infant Behavior, Disorganized
Movement: Hemiparesis/plegia Paraparesis/plegia Infant Behavior, Disorganized,
Quadriparesis/plegia Risk for
Infant Behavior, Readiness for
Bathing/Hygiene: Self Assist Total Partial PM Care
Oral Care: Self Assist
Enhanced organized
Poisoning, Risk for
Assistive Devices: N/A Type: Wheelchair Self-Mutilation
Weight Bearing Status: FWB L PWB R PWB NWB Self-Mutilation, Risk for
Sensory/Perception,
Precautions: Swallowing Seizure Spinal Fall Subarachnoid Disturbed (specify):
Visual, Kinesthetic, Auditory,
Perception: Gordon’s Cognitive-Perceptual Pattern
Vision Deficits: Blind (legally) Glasses Contacts Wears glasses Gustatory, Tactile, Olfactory
Hearing Deficits: Deaf HOH Hearing Aid(s): L R Bilat. Suicide, Risk for
Other: Unilateral Neglect
Violence, Risk for Other-
Precautions: none Danger to Self Danger to Others
Self Mutilation
Directed
Suicide Alcohol and Drug Withdrawal Violence, Risk for Self-Directed
Medications R/T Safety and Security: Yes No Type:
Pt.’s Highest Level of Education: High school
WOSC Freshman Clinical Assessment Form -5-
III. LOVE AND BELONGING Gordon’s Pattern of Coping & Stress Tolerance Related Nursing Diagnoses
1. Emotional State Adjustment, Impaired
Caregiver Role Strain
a. What seems to be the client’s mood? Normal for Age/Culture Caregiver Role Strain, Risk for
Withdrawn Depressed Anxious Fearful Uncooperative Communication, Impaired Verbal
Flat Affect Elevated Euphoric Expressive Other Communication, Readiness for
Enhanced
Community Coping, Ineffective
2. Client’s Life Experience Gordon’s Pattern of Values & Beliefs Community Coping, Readiness for
a. How have previous life experiences affected the client’s perception of the current health Enhanced
Delayed Development, Risk for
problems? Pt stated that he smoked until he was 54 years old, ate whatever he wanted, and that he Family Coping: Disabled
used to drink alcohol frequently. He stated that he thought that was the reason he had “heart problems, high Family Coping: Readiness for
Enhanced
blood pressure, and diabetes. Family Processes, Dysfunctional:
b. How has life changed as a result of the current health problem? Stated that now his family has Alcoholism
to visit him at the nursing home instead of his “own house”. Stated that he is no longer able to get around like Family Process, Interrupted
he used to. Stated that he was unhappy that he was gaining weight and couldn’t be as active as he used to be. Family Processed, Readiness for
Enhanced
c. Describe any signs or symptoms that may indicate actual/potential physical/emotional Growth and Development, Delayed
abuse. NONE Loneliness, Risk for
Parental Role Conflict
Parent/Infant/Child Attachment,
3. Family Gordon’s Role-Relationship Pattern
Impaired, Risk for
a. What is the client and family’s perception of the illness/admission? Pt stated that his family was Parenting, Impaired
Parenting, Impaired, Risk for
sad that he wasn’t at home.
Parenting, Readiness for Enhanced
What evidence indicates that family life has changed? Pt is living at the English Manor instead of at Role Performance, Ineffective
home with his wife. Social Interaction, Impaired
Social Isolation
b. How do family members seem to be coping? UTA directly from the family. Pt. stated that his Violence, Risk for
family was “coping with it just fine”.
c. What supportive behaviors from family/significant others are evident? According to pt and
staff the pt’s family members visit every day or every other day.
4. Erikson Developmental Stage Integrity vs. Despair
a. What tasks are appropriate for this stage of development? Looks back on good times with
gladness, on hard times with self-respect, and on mistakes and regrets with forgiveness, will find a
new sense of integrity and a readiness for perceived wrongs, and dissatisfied with the life they've
led.
b. How has this health problem interfered with accomplishing the development tasks for this
client? Pt’s developmental stage doesn’t seem to be affected.
c. What evidence indicates negative or positive developmental resolution? Pt has a sense of
fulfillment about life and a sense of unity within himself and with others.
IV. SELF-ESTEEM: Gordon’s Pattern of Self perception & Self Concept Related Nursing Diagnoses
1. Self-Esteem and Body Image Self-Esteem
a. How is the client’s self-esteem threatened by this illness/admission? Pt stated that he was Adjustment, Impaired
Anxiety
unhappy being overweight. Body Image Disturbed
b. What is the client’s perception of body image and how has it changed? Stated that he had Doping, Defensive
Coping, Ineffective
never been so physically unfit and over weight until he was diagnosed with DM and unable to walk Coping, Readiness for Enhanced
due to a “bad knee”. He stated that he was unhappy about being over weight, the fact that he was Death Anxiety
Decisional Conflict (Specify)
unable to walk and be an active person, but that he had a wonderful life. Stated that he was not Denial, Ineffective
happy about what happened to him but that he “accepted how things were”, and was thankful for Fear
Grieving, Anticipatory
what he did have, and the things he was able to do. . Grieving, Dysfunctional
Grieving, Dysfunctional, Risk for
Hopelessness
WOSC Freshman Clinical Assessment Form -6-
Personal Identify, Disturbed
c. What fears/concerns were expressed by the client that relate to client’s present illness? Post-Trauma Syndrome
Post-Trauma Syndrome, Risk for
2. Culture: Gordon’s Pattern of Values & Beliefs Powerlessness
a. What is the client’s ethnic background? African American
b. How does culture/language influence communication between client/family and healthcare
workers? Pt wants to be informed regarding his health status.
c. Which communication factors are relevant and why do you think so? (Touch, personal
space, eye contact, facial expressions, body language) Eye contact, facial expressions,
therapeutic touch, active listening, and body language are all relevant communication factors.
Effective communication skills help establish a good nurse-patient relationship, allows for the
exchange of information, and permits the pt to feel comfortable, relevant, and respected.
WOSC Freshman Clinical Assessment Form -7-
d. Who seems to be making the healthcare decisions in the family? The patient Powerlessness
Powerlessness, Risk for
e. Based on your observations, what role does each family member play? The wife and Rape-Trauma Syndrome
Rape-Trauma Syndrome, Compound
children have become caregivers secondary to the staff at the nursing home.
Reaction
Religiosity, Impaired
f. Who is responsible for care of a sick family member at home? The patient’s family Religiosity, Readiness for Enhanced
members. Religiosity, Risk for Impaired
Relocation Stress Syndrome
g. What cultural practices related to hospitalization need to be considered? None Relocation Stress Syndrome, Risk for
Self-Mutilation
3. Spirituality Self-Mutilations, Risk for
Sorrow, Chronic
a. What spiritual/religious beliefs does the client express? Baptist
Spiritual Distress
Spiritual Distress, Risk for
b. What spiritual practices related to hospitalization need to be considered? Allow patient Spiritual Well-Being, Readiness for
time for personal prayer, access to church services, and likes to watch religious T.V. Enhanced
programs. Self-Actualization
Health Maintenance, Ineffective
Health Seeking Behaviors (Specify)
Home Maintenance, Impaired
V. SELF-ACTUALIZATION Gordon’s Pattern of Health Perception & Health Management Knowledge, Deficient (Specify)
Knowledge, Readiness for Enhanced
1. What is the client’s/family’s current level of understanding of their health/illness problem? Pt (Specify)
understands that he is elderly and that it is very unlikely that he will ever fully recover. Noncompliance
Therapeutic Regimen: Community,
2. What type of relationship exists with healthcare providers? Pt is very respectful and trusts Ineffective Management of
Therapeutic Regimen: Families,
healthcare providers to take care of him.
Ineffective Management of
Therapeutic Regimen: Management,
VI. Education/discharge planning: (M.E.T.H.O.D.) Effective
Therapeutic Regimen: Management,
MEDICATIONS: Lamictal 50mg po bid, Mobic 15mg po qd, Januvia 50mg po qd, Ineffective
Synthroid 0.1mg po qd, Reglan 5mg po bid, Lopressor 50mg po q12h. (hold if Therapeutic Regimen: Management,
Readiness for Enhanced
systolic b/p <90 or pulse <60), Asprin 325mg po qd, Slow-Mag 128mg po qd,
Topamax 100mg po qd @1800, Ambien 5mg po qhs x60days, Lasix 40mg po qd,
Potassium 120mEq liq po qid, Metolazone 10mg po qd, Nexium 40mg po qd,
Cardura 2mg po qhs, Detrol LA 4mg po qd, Colace 200mg po bid, Miralax 17g po
bid 1 scoop in 8oz water, Glyburide 10mg qam0800 w/meal, Refresh tears 1gtt ou
qhs, Nitroglycerin 0.4mg po sublingual q 5min x 3 PRN CP, Robaxin 500mg po q8h
prn spasms, Robitussin DM 2tsp liq po q6h prn cough, Lortab 5mg q4h prn pain,
Tylenol 325 mg po q4h prn pain/temp, Milk of Magnesia susp 30mL liq po QD prn
constipation, Dulcolax 1 supp rectally QD prn constipation. Advise client to
monitor: blood glucose q4h, blood pressure, pulse and daily weight. Instruct
client on s/s of hypoglycemia (abdominal pain, sweating, hunger, weakness,
dizziness, headache, tremor, tachycardia, anxiety). Inform client to adhere to all
follow up appointments w/ physician to monitor his fluid and electrolyte balance,
thyroid function, CBC, renal and hepatic function. Instruct the client to take B/P
and pulse,prior to taking Lopressor. Hold if systolic B/P is <90 or pulse <60.
ENVIRONMENT: Teach client and family about the importance of implementing fall
precautions, keeping the home free from clutter, installing handicap safety
accessories (shower seat, hand grab bars, grip mat, raised toilet seat, ect.)
THERAPIES: Educate on DVT’s s/s (pain, swelling, tenderness, discoloration or
redness of the affected area, and skin that is warm to the touch) and prevention.
(ROM exercises passive and active w/in limits). Refer to Physical Therapy.
HOME CARE: Pt and family will be encouraged to monitor FSBS, pulse, blood
pressure, daily weight, check for any peripheral edema. (teach how to use scale:
1+ 2+ 3+ 4+) Contact case manager for a Home health care referral. (pt. will need
extensive assistance w/ ADL’s) Teach patient the importance of meticulous foot
care. (Wash feet with warm water and mild soap, and dry them well, particularly
between the toes. Inspect feet and apply moisturizing cream every day but not
between toes.)
WOSC Freshman Clinical Assessment Form -8-
OUTPATIENT THERAPIES: Educate the pt regarding the importance of physical
therapy sessions and following up with a nutritionist. (Refer to physical therapist
and nutritionist.)
DIET: Reeducate the pt about the importance of an approved ADA diet. (print out
pamphlet from ADA website www.diabetes.org) Reiterate how important it is to
adhere to low sodium diet and an approved ADA diet to help maintain health
status. (Refer client and family to a nutritionist for more extensive
education.)
****NOTE: You must be specific in your discharge education.
WOSC Freshman Clinical Assessment Form -9-
Western Oklahoma State College Student Name:
Nursing 1119, 1129, 1123, 2219 & 2229 Patient Initials/Age/Sex PB/83/M
ADMISSION DATE Date Date
NORMAL
TEST 7/10/09 8/07/09 10/06/09 Identify WNL Significance/Trends
RANGE LAB VALUES
WBC UTA UTA UTA UTA
4.5 -13.5
RBCs UTA UTA UTA UTA
4 - 5.2
High Could be due to the patient having poor heart
function (CHF). If the pt had pneumonia at the time
Hgb of the test, that could’ve been the cause. (pt stated he
12-16% 8.2 8.8
had pneumonia a few weeks ago) The pt is also on
Nexium which alters Hgb levels. Could also be due
to prostate cancer.
Hct UTA UTA UTA UTA
37% - 47%
MCV UTA UTA UTA UTA
78 - 102
MCH UTA UTA UTA UTA
25 -35
MCHC UTA UTA UTA UTA
31 - 37
RDW 11.5% - UTA UTA UTA UTA
14.5%
Retic. UTA UTA UTA UTA
0.5 - 2.3%
Platelet UTA UTA UTA UTA
130 - 140
Neutrophils UTA UTA
1.9 -8 UTA UTA
Lymphocytes UTA
19% - 48% UTA UTA UTA
Monocytes UTA
3% - 9% UTA UTA UTA
Eosinophils UTA
0 - 7% UTA UTA UTA
Basophils UTA
0-2% UTA UTa UTA
Sodium WNL
137 -145 UTA 138 UTA
HIGH Could be mean the pt has anemia, pt is on a
med (Topamax) that frequently causes anemia.
Chloride
98 -107 UTA 110 UTA Could be dehydration, or from the pt eating too much
salt. W/O a total lab report it is hard to pin point the
cause.
Potassium WNL
3.5 -5.1 UTA 4.6 UTA
CO2 WNL
22 - 30 UTA 23 UTA
Magnesium UTA
1.5 - 2.4 UTA UTA UTA
LOW Could be due to bone problems or age, the pts
use of laxatives and diuretics, or could be due to
Calcium kidney problems since the creatinine level is high.
8.4 -10.2 UTA 8.2 UTA
Could also be a problem with the pituitary gland since
the T4 is low and TSH is WNL. W/O a total lab report
it is hard to pin point the cause.
INR UTA
UTA UTA UTA
PT UTA
6.0 -8.5 UTA UTA UTA
PTT UTA
20 - 36 sec UTA UTA UTA
BUN WNL
10-20 UTA 15 UTA
Creatinine 0.6-1.2 UTA 1.5 UTA HIGH May mean that the kidneys are not functioning
WOSC Freshman Clinical Assessment Form -10-
properly, or could be due to the pt taking Nexium
which can raise creatinine levels.
Glucose HIGH Has IDDM Could be due to non-adherence to
74-106 UTA 239 UTA
diet regiment.
AST UTA
14 -36 UTA UTA UTA
ALT UTA
9 -52 UTA UTA UTA
Acid UTA
0.0-4.3 UTA UTA UTA
Phosphate
LDH UTA
140-280 UTA UTA UTA
ADMISSION DATE Date Date
NORMAL
TEST Identify WNL Significance/Trends
RANGE LAB VALUES
Amylase
12-52 UTA UTA UTA UTA
Lipase UTA
3.1-34.6 UTA UTA UTA
Phosphorus UTA
2.5 - 4.5 UTA UTA UTA
Alk. Phos. UTA
38 -126 UTA UTA UTA
Total UTA
Bilirubin 0.1 -1.3 UTA UTA UTA
Cholesterol UTA
<100 UTA UTA UTA
Uric acid UTA
250 - 750 UTA UTA UTA
Total Protein UTA
6.3 - 8.2 UTA UTA UTA
Albumin UTA
3.5 - 5 UTA UTA UTA
Globulin UTA
2.3 - 3.5 UTA UTA UTA
Digoxin level N/A
0.5 to 1.9 N /A N /A N /A
Theophylline N/A
10 to 20
level N /A N /A N /A
mcg/mL
Dilantin level N/A
10-20µg/ml N /A N /A N /A
ADMISSION DATE Date Date
NORMAL
TEST UTA 8/07/09 10/06/09 Identify WNL Significance/Trends
RANGE LAB VALUES
Low Pt has been diagnosed with hypothyroidism,
but since his TSH level is not high and the
T4 Calcium level is also low, it could mean that the
5.53-11 UTA UTA 4.88
pituitary gland is responisble for the
hypothyroidism. Further test would need to done
to determine exact cause.
TSH WNL
0.485-4.68 UTA UTA 1.68
ANION GAP WNL
5-15 UTA 5 UTA
PSA WNL
0-4 0.08 UTA UTA
WOSC Freshman Clinical Assessment Form -11-
ADULT LABORATORY/ DIAGNOSTIC TOOL
URINALYSIS (UTA) #1 ABGS (UTA) #2 ABGS (UTA)
Date Date Date
Color pH pH
Appearance pCO2 pCO2
Spec. gravity pO2 PO2
Protein B.E B.E.
Glucose O2 sat O2 sat
Ketones Bicarb Bicarb
Bacteria
Blood 1. ABG ANALYSIS (UTA)
2. ABG ANALYSIS(UTA)
WOSC Freshman Clinical Assessment Form -12-
Western Oklahoma State College Student Name
Nursing 1119, 1129, 1123, 2219 & 2229 Patient Initials/Age/Sex PB/83/M
Clinical Date11/10/09
OTHER DIAGNOSTIC TESTS AND RADIOLOGIC TESTS
DIAGNOSTIC/RADIOLOGIC TEST DATE RESULTS SIGNIFICANCE OF TEST RESULTS/NURSING
and DESCRIPTION OF TEST INTERVENTIONS (i.e client preparation for test/during
test/after test)
(UTA) (UTA) (UTA) (UTA)
(UTA) (UTA) (UTA) (UTA)
(UTA) (UTA) (UTA) (UTA)
(UTA) (UTA) (UTA) (UTA)
(UTA) (UTA) (UTA) (UTA)
(UTA) (UTA) (UTA) (UTA)
WOSC Freshman Clinical Assessment Form -13-
Student Name
Nursing 1119, 1129, 1123, 2219 & 2229 Patient Initials/Age/Sex PB/83/M
Clinical Date11/10/09
Developmental Stage Integrity vs. Despire
Psychosocial Crisis Conflict between sense of personal integrity & despair over regretted life events.
Health-Illness Continuum: Maximum Health Health Illness Death
DIRECTIONS:According to Maslow, identify needs based on Maslow’s hierarchy. Star or
highlight the most outstanding need(s). Justify identified need(s) with specific
objective and subjective findings from the physical assessment, medications, lab,
and other diagnositic test results
I.) Biological and Physiological Needs (Oxygen needs, elimination, nutrition, hydration,sex, rest, activity, shelter, Basic Life
Needs)
1. History of Ischemic heart disease
2. History of CHF
3. History of Peripheral Vascular disease
4. Diagnosed with Malignant Neoplasm prostate
5. Venous Stasis
6. History of seizures
7. Diagnosed withHypertension
8. 2+ and 3+ pitting edema on lower extremities
9. IDDM
10. States that he doesn’t adhere to ADA diet
11. Obese
12. Incontinent
13. FSBS 227
14. Requires total assistance for hygiene and bathing
15. Needs assistance with bed mobility
16. Requires total assistance with toileting needs
17. Requires Total assistance with transfers
18. Pt was soiled with urine
19. Stated Pain in legs and feet at times
20. Skin on LE shiny, waxy, and discolored
21. States has a hard time sleeping
22. States feet and legs are numb and tingly sometimes
23. absent bilateral pedal pulses
24. Brachial artery (irregular heart beat)
II.) Safety Needs (protection, security, order, law, limits, stability, etc)
1. Fall precautions
2. Wears glasses
3. Immobility
4. Rt sided weakness
III.) Belongingness and Love Needs (family, affection, relationships, work group, etc)
1. Father of three
2. Grandfather of 5
3. Pt stated that his family comes to visit every day or every other day
4.
IV.) Esteem Needs (achievement, status, responsibility, reputation)
1. Pt stated that is a proud retiree from the US Air force
2. Pt stated that he was in law enforcement before he “got sick”
3. Staff stated that the pt was a very nice man, who was a joy to work with and be around.
4.
V.) Self actualization (personal growth and fulfillment)
1.
2.
3.
4.
WOSC Freshman Clinical Assessment Form -14-
INDIVIDUALIZED CLIENT NURSING DIAGNOSIS BASED ON MASLOW’S HIERARCHY
Prioritize in accordance to Maslow’s Hierarchy
1. Ineffective Tissue Perfusion: Peripheral
2. Impaired Urinary elimination
3. Impaired physical mobility
4. Imbalanced nutrition: More than body requirements
5. Self-care deficient: hygiene and bathing
WOSC Freshman Clinical Assessment Form -15-
Western Oklahoma State College Student Name Brenda Hood
Nursing 1119 Patient Initials/Age/Sex PB/83/M
Clinical Date11/10/09
Medical Diagnosis (Top priority): Peripheral Vascular Disease
Brief Pathophysiology of Medical Diagnosis with signs and symptoms my patient is/has
exhibited starred *or highlighted : Peripheral artery disease is due to atherosclerosis. This is a
gradual process in which a fatty material builds up inside the arteries. The fatty material mixes with
calcium, scar tissues, and other substances and hardens slightly, forming plaques of arteriosclerosis.
These plaques block, narrow, or weaken the vessel walls. Blood flow through the arteries can be
restricted or blocked totally. Atherosclerosis is known for affecting the arteries of the heart (coronary
arteries) and the brain (carotid arteries). Over the long term, the high blood sugar level of persons
with diabetes can damage blood vessels. This makes the blood vessels more likely to become
narrowed or weakened. Plus, people with diabetes frequently also have high blood pressure and high
fats in the blood, which accelerates the development of atherosclerosis. Of the peripheral arteries,
those of the legs are most often affected. Other arteries frequently affected by atherosclerosis include
those supplying blood to the kidneys or arms. When an artery is blocked or narrowed, the part of the
body supplied by that artery does not get enough blood or oxygen. Decreased blood flow/oxygen, can
injure nerves and other tissues. Some people with peripheral artery disease may need to have the
limb amputated. Rates of amputation are particularly high among African Americans and Hispanics
with diabetes. If arteriosclerosis is in both limbs, the intensity is usually different in each. Symptoms
include: change of color of the legs, cold legs or feet, leg pain at rest or exercise, loss of hair on legs,
muscle pain in thighs calves or feet, numbness of legs or feet, cyanosis, gait abnormalities, weak or
absent pulse in limb
Labs and Diagnostic tests that confirm or are related to the medical diagnosis) :
Ankle-brachial index (ABI) is one of the most common tests used to diagnose PAD. It compares the
blood pressure in your ankle with the blood pressure in your arm. To get a blood pressure reading,
the physician uses a blood pressure cuff and a special ultrasound device to evaluate blood pressure
and flow. Doppler ultrasound or duplex scanning can evaluate blood flow through blood vessels and
identify blocked or narrowed arteries. An angiography can be done by injecting a dye into blood
vessels; this test allows the physician to view blood flow through your arteries as it happens. The
physician is able to trace the flow of the contrast material using imaging techniques such as X-ray
imaging or procedures called magnetic resonance angiography (MRA) or computerized tomography
angiography (CTA). Catheter angiography is a more invasive procedure that involves guiding a
catheter through an artery in your groin to the affected area and injecting the dye that way. Although
invasive, this type of angiography allows for simultaneous diagnosis and treatment - finding the
narrowed area of a blood vessel and then widening it with an angioplasty procedure or administering
medication to improve blood flow. A sample of your blood can be used to measure your cholesterol
and check levels of homocysteine and C-reactive protein.
Primary Nursing Interventions for Disease Processes Listed: The primary nursing intervention
for patients with diabetes and peripheral vascular disease is to help reduce the risk of foot and leg
amputations. Provide patient with meticulous foot care. Wash feet with warm water and mild soap,
and dry them well, particularly between the toes. Inspect feet and apply moisturizing cream every day
but not between toes. To prevent pressure on legs and feet, make sure the pt changes position every
2 hours and performs range-of-motion exercises, if possible. Use protective padding, foot cradles, or
an alternating-pressure mattress to reduce the risk of pressure injuries. Teach pt. how to promote
circulation. Help him devise a ROM exercise program to develop circulation and enhance venous
return. Instruct him to stop exercising if he feels pain. Stress the importance of following a weight
loss program, controlling diabetes, controlling hyperlipidemia and hypertension. Elevate edematous
legs as ordered.
WOSC Freshman Clinical Assessment Form -16-
Western Oklahoma State College Student Name
Nursing 1119, 1129, 1123, 2219 & 2229 Patient Initials/Age/SexPB/83/M
Clinical Date11/10/09
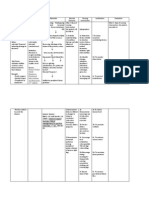
#1 Pt Problem: Edema of the
lower extremities.
Nursing Diagnosis: Ineffective
Tissue Perfusion: Peripheral r/t
interruption of vascular flow #2 Pt Problem:
aeb: cool temp. LE, shiny, Incontinence
waxy, discolored legs; absent
pedal pulses, R/LLE 2+ and 3+ Nursing Diagnosis:
#5 Pt Problem: Unable pitting edema, venous Impaired urinary
to bathe self or perform Medical Diagnosis:
insufficiency elimination r/t a swollen
basic hygiene 1. Peripheral Vascular Disease
prostate
Nursing Diagnosis: Self-
2. IDDM
care deficit: hygiene
and bathing r/t 3. Malignant Neoplasm
weakness in upper and Prostate
lower extremities 4. CHF
#4 Pt Problem: Obesity #3 Pt Problem:
Nursing Diagnosis: Nursing Diagnosis:
Imbalanced nutrition: More Impaired physical mobility
than body requirements r/t r/t partial loss of voluntary
excessive intake in relation to movement of upper and
metabolic need. lower extremities.
RATIONALE FOR CHOOSING NURSING DIAGNOSIS TO COMPLETE CONCEPT MAPS FOR: (i.e. Airway
a basic need according to Maslow’s )
I chose Ineffective tissue perfusion first because the pt has peripheral vascular disease.
With the edema and venous stasis, it makes him more susceptible to DVT’s which can
cause death or amputation. I chose impaired urinary elimination next because the pt was
diagnosed with prostate cancer. As a nurse, I can’t do anything about the cancer, but
maybe I can help relieve some of the symptoms, one being urinary incontinence. I chose
impaired physical mobility next because if my pt was able to be more active, then he might
be more able to loose weight; in turn that could help with his diabetes and heart disease. I
chose self care deficit because the pt is totally dependent on nursing for ADL’s.
WOSC Freshman Clinical Assessment Form -17-
Western Oklahoma State College Nursing Department Student Name:
# 1 Nursing Diagnosis Concept Map
Subjective Data Objective Data
Pt. stated that he sometimes has pain in his leg Lower extremities: shiny, waxy, discoloration of
and ankles. Pt states that his feet and legs are the skin; cool skin temp; absent pedal pulses; 2+
numb and tingly sometimes. Stated that the and 3+ pitting edema. Loss of hair on the legs;
doctor said he had a “bad heart”, high BP 154/71; FSBS 227
cholesterol, and that his arteries were getting
“clogged up”.
Nursing Diagnosis
Ineffective tissue perfusion: peripheral r/t interruption of vascular
flow aeb shiny, waxy, discolored skin, cool skin temperature,
absent pedal pulses, 2+ and 3+ pitting edema
Short Term and Long Term Outcome (must be measurable)
Pt will identify changes in life style needed to increase tissue perfusion by the end of my
shift.
Pt will verbalize knowledge of treatment regimen, including appropriate ROM exercises
and medications and their actions and possible side effects by discharge from hospital.
WOSC Freshman Clinical Assessment Form -18-
Nursing Interventions Scientific Nursing Rationale
1. Check the dorsal pedis pulses bilaterally. 1. Diminished or absent peripheral pulses indicate
arterial insufficiency with resultant ischemia NDHB
2. Elevate edematous legs as ordered. 845
3. Stress the importance of following a weight 2. Elevation increases venous return and helps
loss program, controlling diabetes, controlling decrease edema. NDHB 846
hyperlipidemia and hypertension.
3. All of these risk factors for atherosclerosis can
4. Note skin color and feel the temperature of the be modified. NDHB 847
skin.
4. Skin pallor or mottling, cool or cold skin
5. Observe for signs of deep vein thrombosis temperature, or an absent pulse can signal arterial
including pain, tenderness, swelling in the calf obstruction, which is an emergency that requires
and thigh and redness. immediate intervention. NDHB pg845
6. Provide patient with meticulous foot care. 5. Thrombosis with clot formation is usually first
Wash feet with warm water and mild soap, and detected as swelling of the involved leg and then as
dry them well, particularly between the toes. pain. NDHB 846
Inspect feet and apply moisturizing cream every
day but not between toes. 6. Ischemic feet are vulnerable to injury; meticulous
foot care can prevent further injury NDHB 846
7. Use protective padding, foot cradles, or an
alternating-pressure mattress to reduce the risk 7. Ischemic feet are vulnerable to injury; meticulous
of pressure injuries. foot care can prevent further injury NDHB 846
Evaluation of Short Term and Long Term Outcomes (met or not met and why)
Goal met pt was able to identify changes in lifestyle needed to increase tissue perfusion.
Goal met pt was able to verbalize knowledge of treatment regimen.
WOSC Freshman Clinical Assessment Form -19-
You might also like
- Nursing Diagnosis & Careplan SamplesDocument5 pagesNursing Diagnosis & Careplan SamplesE94% (18)
- Nursing DiagnosisDocument58 pagesNursing DiagnosisPrecious Santayana100% (3)
- Nursing Care Plan 6 Impaired Gas ExchangeDocument9 pagesNursing Care Plan 6 Impaired Gas Exchangedbryant0101100% (12)
- Activity Intolerance Care PlanDocument4 pagesActivity Intolerance Care Planapi-315890029No ratings yet
- Nursing Care Plan Ineffective Peripheral Tissue PerfusionDocument3 pagesNursing Care Plan Ineffective Peripheral Tissue PerfusionRosalie Delfin90% (10)
- Concept Map of DepressionDocument2 pagesConcept Map of DepressionJu Lie AnnNo ratings yet
- Congestive Heart Failure and Pulmonary Edema Concept MapDocument1 pageCongestive Heart Failure and Pulmonary Edema Concept MapAndrew Godwin100% (5)
- Cavite State University College of Nursing Nursing Care PlanDocument1 pageCavite State University College of Nursing Nursing Care PlanMariko BarbaNo ratings yet
- Ineffective Renal Tissue PerfusionDocument2 pagesIneffective Renal Tissue PerfusionHendra Tanjung100% (4)
- Concept Map StrokeDocument1 pageConcept Map StrokeMary GiuntiniNo ratings yet
- Impaired Gas ExchangeDocument3 pagesImpaired Gas ExchangeBenedicto RosalNo ratings yet
- Nursing Care PlanDocument2 pagesNursing Care Planmjoie_baby6568470100% (6)
- Decreased Cardiac OutputDocument3 pagesDecreased Cardiac OutputTiffany Mathis100% (1)
- NCP - Ineffective Tissue Perfusion ECLAMPTIC SEIZUREDocument2 pagesNCP - Ineffective Tissue Perfusion ECLAMPTIC SEIZUREkhanepot100% (2)
- Activity IntoleranceDocument2 pagesActivity Intolerancejunex123No ratings yet
- Nursing Care Plans For UTIDocument2 pagesNursing Care Plans For UTIHannah Pin50% (2)
- Ineffective Breathing PatternDocument2 pagesIneffective Breathing PatternJoy Arizala CarasiNo ratings yet
- BSNURSE: NCP - HypertensionDocument3 pagesBSNURSE: NCP - Hypertensionmickey_beeNo ratings yet
- Nursing Care Plans For Decreased Cardiac OutputDocument4 pagesNursing Care Plans For Decreased Cardiac OutputCarmela Balderas Romantco80% (5)
- Activity IntoleranceDocument6 pagesActivity IntoleranceDenvEr CabaniLlasNo ratings yet
- Acute Pain NURSING CARE PLANDocument2 pagesAcute Pain NURSING CARE PLANMatthew Emmanuel M. Martinez100% (4)
- Nursing Care Plans for Neurological PatientDocument9 pagesNursing Care Plans for Neurological PatientJam AbantaoNo ratings yet
- Nursing Care Plan 2Document6 pagesNursing Care Plan 2ayanori_boyNo ratings yet
- Impaired Tissue Integrity - CellulitisDocument3 pagesImpaired Tissue Integrity - CellulitisKelvin Kurt B. AgwilangNo ratings yet
- Nursing Care PlanDocument7 pagesNursing Care PlanGem Ma100% (7)
- Nursing Care Plan Risk For Urinary RetentionDocument4 pagesNursing Care Plan Risk For Urinary RetentionReginald Julia100% (2)
- NCP GbsDocument2 pagesNCP GbsJaylord VerazonNo ratings yet
- Nursing Care Plan Acute PainDocument3 pagesNursing Care Plan Acute Paindbryant010199% (69)
- Risk For Infection NCP Ortho JadDocument1 pageRisk For Infection NCP Ortho JadjadpauloNo ratings yet
- Acute Confusion Nursing DiagnosisDocument4 pagesAcute Confusion Nursing Diagnosisasmika danaNo ratings yet
- Urinary Tract Infection, (UTI) Is An Infection of One orDocument4 pagesUrinary Tract Infection, (UTI) Is An Infection of One orLorebellNo ratings yet
- Nursing Care PlanDocument4 pagesNursing Care PlanJoy Callo100% (2)
- ABC: Sickle-Cell Anemia, Shock, PoisoningDocument46 pagesABC: Sickle-Cell Anemia, Shock, Poisoningroneln100% (1)
- Risk For Decreased Cardiac OutputDocument3 pagesRisk For Decreased Cardiac OutputSid Artemis FriasNo ratings yet
- NCP & Prio!!!Document45 pagesNCP & Prio!!!Sj 斗力上100% (1)
- NCP HypokalemiaDocument2 pagesNCP HypokalemiaJoyVee Pillagara-De Leon40% (5)
- Risk For Ineffective Tissue PerfusionDocument5 pagesRisk For Ineffective Tissue PerfusionElle Oranza100% (1)
- Nursing Diagnosis Care Plan HyponitremiaDocument2 pagesNursing Diagnosis Care Plan HyponitremiaAbdallah AlasalNo ratings yet
- Urinary Tract Infection - NCPDocument2 pagesUrinary Tract Infection - NCPIssa Farne0% (1)
- NCP Blood Glucose Imbalance 4thDocument2 pagesNCP Blood Glucose Imbalance 4thRainier IbarretaNo ratings yet
- Post-op Nursing Care Plan for Skin IntegrityDocument2 pagesPost-op Nursing Care Plan for Skin IntegritySharewin PulidoNo ratings yet
- Decrease Cardiac OutputDocument6 pagesDecrease Cardiac OutputGerardeanne ReposarNo ratings yet
- Nursing Care PlanDocument22 pagesNursing Care PlanjamNo ratings yet
- NURSING CARE PLAN On Impaired Skin IntegrityDocument2 pagesNURSING CARE PLAN On Impaired Skin Integrityapi-371817493% (30)
- Concept Map Pleural EffusionDocument1 pageConcept Map Pleural Effusionapi-341263362No ratings yet
- Managing Impaired Gas Exchange in an Elderly COPD PatientDocument23 pagesManaging Impaired Gas Exchange in an Elderly COPD PatientKaren Joyce Costales Magtanong100% (3)
- Everyone Would Be Better Off Without Me" As Verbalized by The PatientDocument4 pagesEveryone Would Be Better Off Without Me" As Verbalized by The PatientDanica Kate GalleonNo ratings yet
- Ineffective Tissue PerfusionDocument3 pagesIneffective Tissue PerfusionStephanie Louisse Gallega Hisole100% (2)
- NCP Inffective Tissue PerfusionDocument3 pagesNCP Inffective Tissue PerfusionPaul Cubacub0% (1)
- NCP - Excess Fluid Volume (Aortic Stenosis)Document3 pagesNCP - Excess Fluid Volume (Aortic Stenosis)Daniel Vergara Arce100% (3)
- Diarrhea NCP 1Document1 pageDiarrhea NCP 1Rhence Efner Saylon50% (2)
- Jantung - Acute Heart FailureDocument32 pagesJantung - Acute Heart FailurefaradibaNo ratings yet
- Assessment and Concept Map Care Plan Critical Care PatientDocument8 pagesAssessment and Concept Map Care Plan Critical Care Patientapi-508051902No ratings yet
- PREM AlgorithmsDocument20 pagesPREM AlgorithmsalexNo ratings yet
- Sterling Roberts Concept Map Complex CareDocument6 pagesSterling Roberts Concept Map Complex Careapi-662884360No ratings yet
- Warning: Learners, Please Complete The Learner Survey (Ucalgary - Ca/Codeblue/Surveys) Before Viewing This PowerpointDocument27 pagesWarning: Learners, Please Complete The Learner Survey (Ucalgary - Ca/Codeblue/Surveys) Before Viewing This PowerpointHandrian RahmanNo ratings yet
- Code Blue Simulation TrainingDocument26 pagesCode Blue Simulation TrainingJenny CandraNo ratings yet
- Paediatric Respiratory Assessment Cheat SheetDocument1 pagePaediatric Respiratory Assessment Cheat SheetReihann N. EdresNo ratings yet
- Ocne 8 SupportDocument9 pagesOcne 8 Supportapi-349380871No ratings yet
- Case Study On Children With Cardiac DisordersDocument3 pagesCase Study On Children With Cardiac DisordersAlyNo ratings yet
- FHP and NCPDocument12 pagesFHP and NCPMa. Ferimi Gleam BajadoNo ratings yet
- Manual Dinamap Critikon 8100Document48 pagesManual Dinamap Critikon 8100Andrea Nathaly Medina SanchezNo ratings yet
- Week 13 CD COURSE TASK 7. Dengue Fever, Filariasis, Malaria and EncephalitisDocument5 pagesWeek 13 CD COURSE TASK 7. Dengue Fever, Filariasis, Malaria and EncephalitisRogelyn PatriarcaNo ratings yet
- Nueva Ecija University of Science And: O V A ADocument8 pagesNueva Ecija University of Science And: O V A ALeslie PaguioNo ratings yet
- 3-BSE B - Activity 1 - Section 1 and 2 - Module 1Document6 pages3-BSE B - Activity 1 - Section 1 and 2 - Module 1Karmela CosmianoNo ratings yet
- English Assignments About Case Study Name: Indriyani Eka Lani Oematan NIM: 01.2.17.00609Document4 pagesEnglish Assignments About Case Study Name: Indriyani Eka Lani Oematan NIM: 01.2.17.00609Eka OematanNo ratings yet
- Vital SignsDocument7 pagesVital SignsEmeroot RootNo ratings yet
- Sample Family Care Study (N107)Document51 pagesSample Family Care Study (N107)Dan Dan Soi T97% (31)
- Malaria Case Studies Only - EnglishDocument11 pagesMalaria Case Studies Only - EnglishFeik Emelje100% (1)
- Physical Assessment Vitals and FindingsDocument16 pagesPhysical Assessment Vitals and FindingsDaryl Jake FornollesNo ratings yet
- English M8102-9441ADocument40 pagesEnglish M8102-9441ABong Kek ChiewNo ratings yet
- Ems Pic Data Entry Logic For Public ViewDocument20 pagesEms Pic Data Entry Logic For Public Viewmedic9341No ratings yet
- Admision and DischargeDocument29 pagesAdmision and DischargeJAMES TONNY OKINYINo ratings yet
- Pediatrics History and Physical ExamDocument16 pagesPediatrics History and Physical ExamstarrnewmanpaNo ratings yet
- Medical Surgical Nursing QuestionsDocument7 pagesMedical Surgical Nursing Questionseloisa mae gementizaNo ratings yet
- Activity # Title Shampoo Product "Blowsom"Document33 pagesActivity # Title Shampoo Product "Blowsom"Kathleen B BaldadoNo ratings yet
- Patient Discharge SummaryDocument1 pagePatient Discharge SummaryampalNo ratings yet
- NMC Ape Guidelines DraftDocument5 pagesNMC Ape Guidelines DraftJordan Michael De VeraNo ratings yet
- Diagnostic Tests for Diabetes CaseDocument5 pagesDiagnostic Tests for Diabetes Caseangelica dizonNo ratings yet
- Dr. P. Ocampo Colleges, Inc. de Mazenod Avenue Extension Cotabato CityDocument3 pagesDr. P. Ocampo Colleges, Inc. de Mazenod Avenue Extension Cotabato Cityrasul kanakan ganiNo ratings yet
- PONR - Comprehensive Nursing Health History and Physical ExaminationDocument21 pagesPONR - Comprehensive Nursing Health History and Physical ExaminationDRJC100% (1)
- HerniaDocument6 pagesHerniahani alzo3bi100% (7)
- OMNI 3 BrochureDocument6 pagesOMNI 3 BrochureRichard CeballosNo ratings yet
- Critikon Dinamap Compact - Service Manual 2Document78 pagesCritikon Dinamap Compact - Service Manual 2Ayaovi JorlauNo ratings yet
- ELICIAE MV20 - Clinical Study - VL - 26AUG2020Document29 pagesELICIAE MV20 - Clinical Study - VL - 26AUG2020ngocbienk56No ratings yet
- Day 1: FDAR/ NCP (Pain) : Form No.: Revision No.: Effectivity DateDocument3 pagesDay 1: FDAR/ NCP (Pain) : Form No.: Revision No.: Effectivity DateLiza M. PurocNo ratings yet
- Nursing care for post-tonsillitis surgery painDocument2 pagesNursing care for post-tonsillitis surgery painDwi PratiwiNo ratings yet
- ER Triage ScenariosDocument3 pagesER Triage Scenariosamal abdulrahmanNo ratings yet
- Problem StatementsDocument7 pagesProblem StatementsSunilSahaniNo ratings yet
- NCP and Focus Charting For PainDocument3 pagesNCP and Focus Charting For PainArian May MarcosNo ratings yet