Professional Documents
Culture Documents
I-Iv Sections
Uploaded by
api-286042533Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
I-Iv Sections
Uploaded by
api-286042533Copyright:
Available Formats
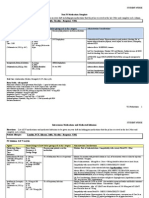
STUDENT NURSE
Preclinical Work-up
Student: STUDENT NUSE_
Unit: ICU
Day of Care: 5FEB2015
I. BASELINE INFORMATION
A. Demographics
Pt. Initials C.G Room #5 Gender/Age F/63 Code Status FULL A.D. YES
Ht 1.6 m (53)
Wt : 48 Kg (105 lb 13.1 oz)
ALLERGIES (and response to if known) Lanolin, PCN, Silicone, Sulfa, Vicodin (Unknown Response)
Admitting Diagnosis: RESPIRATORY FAILURE ACUTE/ HCC
Actual (Current) Diagnosis RESPIRATORY FAILURE ACUTE/ HCC
Date of Admission 02/01/2015
Current Surgery(s) flexible and rigid bronchoscopy for removal of airway foreign body (02/01/2015)
Isolation Precautions NONE
Fall Risk Precautions YES
Eriksons Developmental Level Generative vs. Stagnation
Culture/Ethnicity/Religious Preference: Caucasian/Jewish
II. INFORMATION FROM CHART
1. Chief Complaint (Reason for Hospitalization):
Acute Respiratory Arrest
2. History of Present Illness (HPI) Tell the patients story about this illness; provide a brief summary from the chart):
2/1/15 Pt. was having lunch when all of a sudden she started having difficulty breathing, chocking and coughing x10
min before collapsing. The paramedics were called and the pt. was brought to the ED intubated. She arrived with VS
T:95.8, HR:100, BP:101/77, RR:21. The EKG showed ST (124), cXray showed bilateral alveolar infiltrates, left greater
than right. A bronchoscopy revealed that the pt. was on acute respiratory failure secondary to foreign object (chicken) in
the left main bronchus. The pt. was on severe metabolic acidosis. The foreign object was Sx. removed.
2/2/15 Patient is stable. Foreign body removed. Right vocal cord appeared to have a lesion at DL. The plan is to wean
vent as tolerated. Consider outpatient or elective ENT consult. Trach to be considered and conversion of PEG (placed
2003) to be used for feedings. Pt. is on SR but converts to ST when agitated. There is moderate amount of blood tinged
pulmonary secretions. Feedings via PEG started and NGT clamped. Adequate UO via indwelling catheter. Intact skin.
PICC line inserted.
2/3/15 Lungs are diminished bilaterally. SR. BS WNL. No edema, no s/s of DVT. Tracheostomy
2/4/15 cXR continues to show significant L sided infiltrate and small on R. Rhonchi on L. SR. BS WNL.
3. Past Medical History (Bullet-points)
Migraine
Stroke (HCC)
Hypothyroidism
Aspiration pna
Sepsis
TB
Chronic back pain Baclofen pump
Pt. Deaf in both eats
Cerebral palsy
Anxiety disorder
Degenerative disc disease
Frozen should on the left side secondary to
fracture
Hx. of car accident resulting in neck surgery and
PEG placement
Hx. of dysphagia
I. Baseline Information II. Information from Chart III. Focus of Care IV. Considerations for Care
STUDENT NURSE
III. FOCUS CARE (Think like a nurse, bullet-points)
1. Based on your preclinical research, what do you expect this patient to look like in terms of their diagnosis and
condition when you walk into the room at the start of the shift?
Based on the Dx., I expect to find a pt. that continues to be sedated and restrained due to her need for a ventilator. During the
sedation vacation, the pt. becomes agitated and requires to be restrained to prevent her from pulling lines. Additionally, when the pt.
becomes agitated, she presents with ST. I predict that this pt. will not be ready to be weaned from the ventilator. The pt. continues to
show no s/s of pulmonary improvement, thus I expect to find that she is still on FiO2 40%. I expect the pt.s lungs will continue to
show s/s of L infiltrate and will continue to present with diminished bilateral breaths sounds.
2. What are the important assessment to make, including labs and diagnostics?
The focus of this pt.s assessment is RESPIRATORY
o Lung sounds
o RR
o ABGs
o O2 sat
o Monitor HR tachycardia can be an indication of respiratory failure
o Monitor cXR for s/s infiltrates
o Skin color and capillary refill
o Monitor CBC
It is important to assess VS for s/s of infection as the pt. is on a ventilator and at risk for VAP
3. What will tell you if the patient is improving?
cXR with decreased infiltrates
Clear lung sounds
ABGs pH WNL
No agitation during sedation vacation
Pt. shows signs of spontaneous effort
Pt. meets weaning criteria
Pt. tolerates ventilation weaning IMPORTANT FOR DISCHARGE FROM ICU!
4. What complications may occur & how would you recognize it; who would you notify if it did?
Inadvertent extubation pt. has a tracheostomy call for help (another nurse) if the pt. is agitated and requires
holding during reintubation - all the equipment the RN needs is at the beside. Document and let the charge nurse
know? Would you need to call the MD after or would it be something you shared when s/he came for rounds?
VAP contact MD and RT
DVT contact MD
Acid/Base imbalances contact MD
ARDS contact MD
5. What interventions will prevent the complications?
Use of restrains
ABCDE Bundle to promote early extubation
HOB at 30 to prevent aspiration
Monitor BS to determine motility, check residuals to prevent aspiration.
Intermittent sequential pneumatic compression
Suctioning
Oral care
I. Baseline Information II. Information from Chart III. Focus of Care IV. Considerations for Care
STUDENT NURSE
IV. CONSIDERATIONS FOR CARE
1. Diet and rationale (include reference):
Tube feeding tube feeding formulas contain vitamin k to meet the daily recommended intake of 80 mcg/day in 1000 to
1500 ml of formula. Consideration should be given when dosing anticoagulation medications for patient who have
recently and extremely limited their intake of dietary vitamin k.
Product: Replete (1 cal/ml, high protein, replaces promote). Rate: 40 ml. Increase 10 ml q6hr until goal rate (60 ml) is
met.
PEG
Additional water volume: 20 ml q2h
Rationale: Nutritional depletion can lead to loss of muscle mass, which can impair respiratory muscles and prolong
recovery. Enteral feedings provide the calories needed to meet the hypermetabolic state of the pt. and prevent nutritional
depletion. The pt. is on tube enteral feeding because during acute respiratory failure there is a risk for aspiration;
additionally the pt. is sedated and on a ventilator. (Lewis et al., 2011, p. 1755).
2. Activity order (per MD order (if no order, expected activity ability): BEDREST WITH HOB AT 30 AT ALL TIMES
3. Discharge (on MAP only, teaching, referrals, etc...):
4. Culture/Ethnicity (on MAP only, nursing considerations R/T )
I. Baseline Information II. Information from Chart III. Focus of Care IV. Considerations for Care
You might also like
- ComprehensiveDocument10 pagesComprehensiveapi-286042533No ratings yet
- VIII Advance Treatments and InterventionsDocument2 pagesVIII Advance Treatments and Interventionsapi-286042533No ratings yet
- VI MedicationsDocument6 pagesVI Medicationsapi-286042533No ratings yet
- V Labs and DiagnosticsDocument3 pagesV Labs and Diagnosticsapi-286042533No ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Undescended TestesDocument2 pagesUndescended TestesSamantha TarunNo ratings yet
- ImgDocument1 pageImgLIDIYA MOL P V100% (1)
- Asthma Broncial (Theophylline)Document41 pagesAsthma Broncial (Theophylline)Nadya Zahra Henni100% (1)
- "Bioterrorism": Delhi Pharmaceutical Sciences and Research UniversityDocument6 pages"Bioterrorism": Delhi Pharmaceutical Sciences and Research UniversityNeeru ChaudharyNo ratings yet
- Prasugrel and RosuvastatinDocument7 pagesPrasugrel and RosuvastatinMohammad Shahbaz AlamNo ratings yet
- Patient Care Assistant ResumeDocument8 pagesPatient Care Assistant Resumeafazakemb100% (2)
- NCM 103 Aliasas AtelectasisDocument3 pagesNCM 103 Aliasas AtelectasisDARREN EDMARKNo ratings yet
- Physical Changes With AgingDocument8 pagesPhysical Changes With Agingjanna mae patriarcaNo ratings yet
- Hipopresivos y Dolor Lumbar Cronico 2021Document9 pagesHipopresivos y Dolor Lumbar Cronico 2021klgarivasNo ratings yet
- Complications After CXLDocument3 pagesComplications After CXLDr. Jérôme C. VryghemNo ratings yet
- Nursing Care of a Patient with AppendicitisDocument3 pagesNursing Care of a Patient with AppendicitisKeisha BartolataNo ratings yet
- Care for a Client with LeptospirosisDocument4 pagesCare for a Client with LeptospirosisLyndon SayongNo ratings yet
- Strategi RS Dalam Pemenuhan Dan Pengaturan SDM CompressedDocument37 pagesStrategi RS Dalam Pemenuhan Dan Pengaturan SDM CompressedLilik SeptiyaNo ratings yet
- Recovery of Healthy Patient PACU HandoutDocument12 pagesRecovery of Healthy Patient PACU HandoutGe NavNo ratings yet
- How To Protect Yourself and OthersDocument2 pagesHow To Protect Yourself and OtherslistmyclinicNo ratings yet
- The Truth About The Flu ShotDocument5 pagesThe Truth About The Flu ShotPoorMexicanNo ratings yet
- Bitemporal HemianopiaDocument7 pagesBitemporal HemianopiasriNo ratings yet
- 155 Anaesthesia For Transurethral Resection of The Prostate (TURP)Document8 pages155 Anaesthesia For Transurethral Resection of The Prostate (TURP)Verico PratamaNo ratings yet
- Update On Importance of Diet in Gout: ReviewDocument6 pagesUpdate On Importance of Diet in Gout: ReviewIoana IonNo ratings yet
- Differences in Housemen Performance from CUCMS and Other Medical SchoolsDocument10 pagesDifferences in Housemen Performance from CUCMS and Other Medical SchoolsAfif AizatNo ratings yet
- SBI Insurance Violating PMJAY NormsDocument4 pagesSBI Insurance Violating PMJAY NormsAntar SinghNo ratings yet
- Electrical Burn PathophysiologyDocument1 pageElectrical Burn PathophysiologydanicaNo ratings yet
- Kuisioner Nutrisi Mini Nutritional AssessmentDocument1 pageKuisioner Nutrisi Mini Nutritional AssessmentNaufal AhmadNo ratings yet
- SA Psych MAY 2016 FIn Final WebDocument82 pagesSA Psych MAY 2016 FIn Final WebAKNTAI002No ratings yet
- Labor Pain ManagementDocument1 pageLabor Pain ManagementKenneth Sy100% (5)
- Diabetes TrackerDocument1 pageDiabetes Trackerwildlifewarrior_zrsNo ratings yet
- Cutaneous MelanomaDocument226 pagesCutaneous MelanomaGriskalia ChristineNo ratings yet
- Universitas Muhammadiyah Ponorogo Health Sciences JournalDocument10 pagesUniversitas Muhammadiyah Ponorogo Health Sciences JournalAjeng NingsihNo ratings yet
- NEET UG Biology Human Health and DiseasesDocument18 pagesNEET UG Biology Human Health and DiseasesMansoor MalikNo ratings yet