Professional Documents
Culture Documents
Nursing Care Plan For Myocardial Infarction NCP
Uploaded by
dericOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nursing Care Plan For Myocardial Infarction NCP
Uploaded by
dericCopyright:
Available Formats
Student Nurses Community
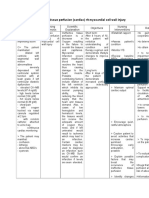
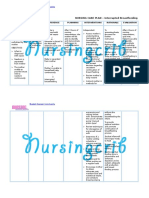
NURSING CARE PLAN Myocardial Infarction
ASSESSMENT
Subjective:
The client reports
of chest pain
radiating to the left
arm and neck and
back.
Objective:
Restlessness
Facial
grimacing
Fatigue
Peripheral
cyanosis
Weak pulse
Cold and
clammy skin
Palpitations
Shortness of
breath
Elevated
temperature
Pain scale of
8/10
DIAGNOSIS
PLANNING
INTERVENTION
RATIONALE
EVALUATION
Acute (Chest)
Pain r/t
myocardial
ischemia
resulting from
coronary artery
occlusion with
loss/restriction
of blood flow to
an area of the
myocardium
and necrosis of
the
myocardium.
STG:
Within 1 hour
of nursing
interventions,
the client will
have improved
comfort in
chest, as
evidenced by:
States a
decrease in
the rating of
the chest
pain.
Is able to
rest, displays
reduced
tension, and
sleeps
comfortably.
Requires
decrease
analgesia or
nitroglycerin.
INDEPENDENT:
1. Assess
characteristics of
chest pain, including
location, duration,
quality, intensity,
presence of
radiation,
precipitating and
alleviating factors,
and as associated
symptoms, have
client rate pain on a
scale of 1-10 and
document findings
in nurses notes.
1. Pain is indication
of MI. assisting the
client in quantifying
pain may
differentiate preexisting and current
pain patterns as
well as identify
complications.
STG:
Within 1 hour of
nursing
intervention, the
client had
improved comfort
in chest, as
evidenced by:
States a
decrease in the
rating of the
chest pain.
Is able to rest,
displays reduced
tension, and
sleeps
comfortably.
Requires
decrease
analgesia or
nitroglycerin.
Goal was met.
LTG:
The client
will have an
improved
feeling of
control as
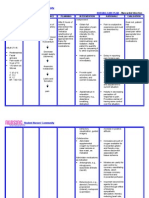
2. Obtain history of
previous cardiac
pain and familial
history of cardiac
problems.
3. Assess
respirations, BP and
heart rate with each
episodes of chest
pain.
4. Maintain bed rest
during pain, with
2. This provides
information that
may help to
differentiate current
pain from previous
problems and
complications.
3. Respirations may
be increased as a
result of pain and
associate anxiety.
4. To reduce oxygen
consumption and
demand, to reduce
competing stimuli
and reduces
anxiety.
5. Pain control is a
LTG:
The client had an
improved feeling
of control as
evidenced by
verbalizing a sense
of control over
present situation
Student Nurses Community
evidenced by
verbalizing a
sense of
control over
present
situation and
future
outcomes
within 2 days
of nursing
interventions.
position of comfort,
maintain relaxing
environment to
promote calmness.
5. Prepare for the
administration of
medications, and
monitor response to
drug therapy. Notify
physician if pain
does not abate.
6. istruct patient in
nitroglycerin SL
administration after
hospitalization.
Instruct patient in
activity alterations
and limitations.
7. Instruct
patient/family in
medication effects,
side-effects,
contraindications
and symptoms to
report.
DEPENDENT:
1. Obtain a 12-lead
ECG on admission,
then each time
chest pain recurs for
evidence of further
infarction as
prescribed.
priority, as it
indicates ischemia.
6. To decrease
myocardial oxygen
demand and
workload on the
heart.
7. To promote
knowledge and
compliance with
therapeutic regimen
and to alleviate fear
of unknown.
1. Serial ECG and
stat ECGs record
changes that can
give evidence of
further cardiac
damage and
location of MI.
2. Morphine is the
drug of choice to
control MI pain, but
other analgesics
may be used to
reduce pain and
reduce the
workload on the
heart.
3. To block
sympathetic
stimulation, reduce
and future
outcomes within 2
days of nursing
intervention.
Goal was met.
Student Nurses Community
2. Administer
analgesics as
ordered, such as
morphine sulfate,
meferidine of
Dilaudid N.
3. Administer betablockers as ordered.
4. Administer
calcium-channel
blockers as ordered.
heart rate and
lowers myocardial
demand.
4. To increase
coronary blood flow
and collateral
circulation which
can decrease pain
due to ischemia.
Student Nurses Community
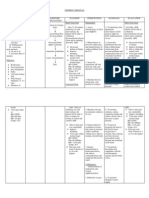
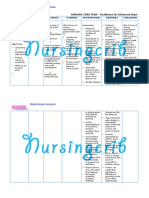
ASSESSMENT
DIAGNOSIS
PLANNING
INTERVENTION
RATIONALE
EVALUATION
Subjective:
The client
reports of
increased work
of breathing
associated with
feelings of
weakness and
tiredness.
Activity
Intolerance
r/t cardiac
dysfunction,
changes in
oxygen
supply and
consumption
as evidenced
by shortness
of breath.
STG:
Within 3 days of
nursing
interventions, the
client will be able
to tolerate activity
without excessive
dyspnea and will
be able to utilize
breathing
techniques and
energy
conservation
techniques
effectively.
INDEPENDENT:
1. Monitor heart rate,
rhythm, respirations
and blood pressure for
abnormalities. Notify
physician of
significant changes in
VS.
1. Changes in VS assist
with monitoring
physiologic responses
to increase in activity.
STG:
Within 3 days of
nursing
interventions, the
client tolerated
activity without
excessive dyspnea
and had been able
to utilize breathing
techniques and
energy conservation
techniques
effectively.
Goal was met.
Objective:
Increased
heart
rate
Increased
blood
pressure
Dyspnea
with
exertion
Pallor
Fatigue and
weakness
Decreased
oxygen
saturatio
n
Ischemic
ECG
changes
LTG:
Within 5 days of
nursing
interventions, the
client will be able
to increase and
achieve desired
activity level,
progressively,
with no
intolerance
symptoms noted,
such as
respiratory
compromise.
2. Identify causative
factors leading to
intolerance of activity.
3. Encourage patient
to assist with planning
activities, with rest
periods as necessary.
4. Instruct patient in
energy conservation
techniques.
5. Assist with active
or passive ROM
exercises at least QID.
6. Turn patient at
least every 2 hours,
and prn.
7. Instruct patient in
isometric and
breathing exercises.
2. Alleviation of factors
that are known to
create intolerance can
assist with
development of an
activity level program.
3. to help give the
patient a feeling of selfworth and well-being.
4. To decrease energy
expenditure and
fatigue.
5. To maintain joint
mobility and muscle
tone.
6. To improve
respiratory function and
prevent skin
breakdown.
7. To improve breathing
and to increase activity
level.
8. To promote self-
LTG:
Within 5 days of
nursing
interventions, the
client increased and
achieved desired
activity level,
progressively, with
no intolerance
symptoms noted,
such as respiratory
compromise.
Goal was met.
Student Nurses Community
8. Provide
patient/family with
exercise regimen,
with written
instructions.
DEPENDENT:
1. Assisst patient with
ambulation, as
ordered, with
progressive increases
as patients tolerance
permits.
worth and involves
patient and his family
with self-care.
1. To gradually increase
the body to
compensate for the
increase in overload.
Student Nurses Community
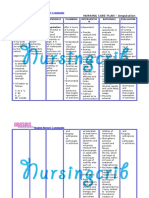
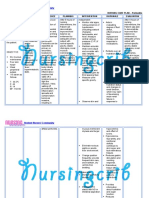
ASSESSMENT
DIAGNOSIS
PLANNING
INTERVENTION
RATIONALE
EVALUATION
Student Nurses Community
Subjective:
The client
verbalizes
questions
regarding
problems and
misconceptions
about his
condition.
Objective:
Lack of
improvement
of previous
regimen
Inadequate
follow-up on
instructions
given.
Anxiety
Lack of
understanding.
Deficient
Knowledge r/t
new diagnosis
and lack of
understanding
of medical
condition.
STG:
The client will be
able to verbalize
and demonstrate
understanding of
information given
regarding
condition,
medications, and
treatment
regimen within 3
days of nursing
interventions.
LTG:
The client will
able to correctly
perform all tasks
prior to discharge.
INDEPENDENT:
1. Monitor patients
readiness to learn and
determine best
methods to use for
teaching.
2. Provide time for
individual interaction
with patient.
3. Instruct patient on
procedures that may
be performed.
Instruct patient on
medications, dose,
effects, side effects,
contraindications, and
signs/symptoms to
report to physician.
4. Instruct in dietary
needs and restrictions,
such as limiting sodium
or increasing
potassium.
5. Provide printed
materials when
possible for
patient/family to
reviews.
6. Have patient
demonstrate all skills
that will be necessary
for post discharge.
7. Instruct exercises to
be performed, and to
avoid overtaxing
activities.
1. To promote optimal
learning environment
when patient show
willingness to learn.
2. To establish trust.
3. To provide
information to
manage medication
regimen and to ensure
compliance.
4. Client may need to
increase dietary
potassium if placed on
diuretics; sodium
should be limited
because of the
potential for fluid
retention.
5. To provide
reference for the
patient and family to
refer.
6. To provide
information that
patient has gained a
full understanding of
instruction.
7. These are helpful in
improving cardiac
function.
STG:
The client verbalized
and demonstrated
understanding of
information given
regarding condition,
medications, and
treatment regimen
within 3 days of
nursing interventions.
Goal was met.
LTG:
The client had been
able to correctly
perform all tasks prior
to discharge.
Goal was met.
Student Nurses Community
You might also like
- Nursing Care Plan For Pneumonia NCPDocument3 pagesNursing Care Plan For Pneumonia NCPderic79% (133)
- Nursing Care Plan For Ineffective Infant Feeding Pattern NCPDocument3 pagesNursing Care Plan For Ineffective Infant Feeding Pattern NCPderic71% (14)
- Nursing Care Plan For Myocardial InfarctionDocument7 pagesNursing Care Plan For Myocardial Infarctionmariejo95% (125)
- Nursing Care Plan For Risk For Aspiration NCPDocument5 pagesNursing Care Plan For Risk For Aspiration NCPderic100% (8)
- Nursing Care Plan For Readiness For Enhanced Spiritual Well Being NCPDocument4 pagesNursing Care Plan For Readiness For Enhanced Spiritual Well Being NCPderic83% (6)
- Nursing Care Plan For Post Trauma NCPDocument5 pagesNursing Care Plan For Post Trauma NCPderic82% (11)
- Nursing Care Plan For Peptic Ulcer NCPDocument2 pagesNursing Care Plan For Peptic Ulcer NCPderic85% (46)
- Nursing Care Plan For Liver Cirrhosis NCPDocument14 pagesNursing Care Plan For Liver Cirrhosis NCPderic92% (12)
- Nursing Care Plan For Seizure NCPDocument2 pagesNursing Care Plan For Seizure NCPderic88% (40)
- Nursing Care Plan For Rabies NCPDocument3 pagesNursing Care Plan For Rabies NCPderic100% (9)
- Nursing Care Plan For Insomnia NCPDocument2 pagesNursing Care Plan For Insomnia NCPderic83% (23)
- Acute Coronary Syndrome NCP 02Document6 pagesAcute Coronary Syndrome NCP 02AgronaSlaughterNo ratings yet
- Care Plan 5Document13 pagesCare Plan 5مالك مناصرة100% (2)
- Nursing Care Plan For Upper Gastrointestinal Bleeding NCPDocument3 pagesNursing Care Plan For Upper Gastrointestinal Bleeding NCPderic79% (14)
- Nursing Care Plan For Multiple Sclerosis NCPDocument2 pagesNursing Care Plan For Multiple Sclerosis NCPderic88% (17)
- Nursing Care Plan For Insufficient Breastmilk NCPDocument2 pagesNursing Care Plan For Insufficient Breastmilk NCPderic100% (17)
- NURSING CARE PLAN For Myocardial InfarctionDocument13 pagesNURSING CARE PLAN For Myocardial Infarctionbanyenye2593% (14)
- Nursing Care Plan For Coronary Artery DiseaseDocument3 pagesNursing Care Plan For Coronary Artery DiseaseLorraineAnneSantiagoCandelario91% (22)
- NCP Chest PainDocument2 pagesNCP Chest PainDOni Corleone87% (39)
- ACS Nursing Care PlanDocument21 pagesACS Nursing Care Planchris_arc90100% (6)
- Nursing Care Plan For AIDS/HIVDocument3 pagesNursing Care Plan For AIDS/HIVderic81% (16)
- Nursing Care Plan For AmputationDocument3 pagesNursing Care Plan For Amputationderic80% (25)
- Nursing Care Plan For Readiness For Enhanced Sleep NCPDocument4 pagesNursing Care Plan For Readiness For Enhanced Sleep NCPderic100% (2)
- "Acute Coronary Syndrome Non ST Elevation Myocardial Infarction, Hypertensive Cardiovascular Disease, Diabetes Mellitus Type 2, and Community Acquired Pneumonia" Nursing Care PlansDocument21 pages"Acute Coronary Syndrome Non ST Elevation Myocardial Infarction, Hypertensive Cardiovascular Disease, Diabetes Mellitus Type 2, and Community Acquired Pneumonia" Nursing Care PlansCarl Elexer Cuyugan Ano100% (1)
- Nursing Care Plan For Angina Pectoris NCPDocument2 pagesNursing Care Plan For Angina Pectoris NCPderic73% (15)
- Myocardial Infarction Case StudyDocument19 pagesMyocardial Infarction Case Studyapi-312992151No ratings yet
- Angina Pectoris Nursing Care PlanDocument1 pageAngina Pectoris Nursing Care PlanjamieboyRN86% (7)
- Nursing Care Plan For HemodialysisDocument2 pagesNursing Care Plan For Hemodialysisderic80% (20)
- Nursing Care Plan For Risk For Compromised Human Dignity NCPDocument3 pagesNursing Care Plan For Risk For Compromised Human Dignity NCPderic100% (2)
- NURSING CARE PLAN For Myocardial InfarctionDocument16 pagesNURSING CARE PLAN For Myocardial InfarctionFreisanChenMandumotan100% (1)
- Nursing Care Plan - Myocardial InfarctionDocument3 pagesNursing Care Plan - Myocardial Infarctionderic80% (10)
- NCP AnginaDocument3 pagesNCP AnginaShie LA100% (1)
- Care Plan Unstable AnginaDocument4 pagesCare Plan Unstable Anginaالغزال الذهبي50% (6)
- SAMPLE NCP For Angina PectorisDocument3 pagesSAMPLE NCP For Angina Pectorisseanne_may100% (4)
- Acute Myocardial Infarction - CSDocument49 pagesAcute Myocardial Infarction - CSMASII94% (17)
- Myocarditis NCP 2Document8 pagesMyocarditis NCP 2astro_aaron117375% (4)
- Nursing Care Plan For Hopelessness NCPDocument5 pagesNursing Care Plan For Hopelessness NCPderic100% (13)
- NCP Rheumatic Heart DiseaseDocument3 pagesNCP Rheumatic Heart DiseaseAdrian Mallar71% (28)
- NCP Ineffective Tissue Perfusion and Self Care DeficitDocument5 pagesNCP Ineffective Tissue Perfusion and Self Care DeficitFrances Anne Pasiliao100% (3)
- Nursing Care Plan For Smoke Poisoning NCPDocument2 pagesNursing Care Plan For Smoke Poisoning NCPderic100% (3)
- Nursing Care Plan For Rape Trauma Syndrome NCPDocument5 pagesNursing Care Plan For Rape Trauma Syndrome NCPderic100% (4)
- Nursing Care Plan For Disturbed Sleep Pattern NCPDocument3 pagesNursing Care Plan For Disturbed Sleep Pattern NCPderic67% (3)
- Nursing Care Plan For Neonatal Sepsis NCPDocument3 pagesNursing Care Plan For Neonatal Sepsis NCPderic67% (9)
- Nursing Care Plan For Interrupted Breastfeeding NCPDocument3 pagesNursing Care Plan For Interrupted Breastfeeding NCPderic88% (8)
- NCP Myocardial InfarctionDocument1 pageNCP Myocardial InfarctionjamieboyRN88% (8)
- Myocardial InfarctionDocument5 pagesMyocardial InfarctionDharline Abbygale Garvida AgullanaNo ratings yet
- NCP Heart BlockDocument3 pagesNCP Heart BlockEköw Santiago Javier33% (3)
- NCP For Mi PainDocument2 pagesNCP For Mi PainKahMallariNo ratings yet
- Nursing Care Plan For Myocardial InfarctionDocument7 pagesNursing Care Plan For Myocardial InfarctionjamieboyRN88% (8)
- NCP For Acute Coronary SyndromeDocument3 pagesNCP For Acute Coronary Syndromesarahtot75% (4)
- NURSING CARE PLAN - Myocardial Infarction Assessment Diagnosis Inference Planning Intervention Rationale EvaluationDocument4 pagesNURSING CARE PLAN - Myocardial Infarction Assessment Diagnosis Inference Planning Intervention Rationale Evaluationsweethoney220% (1)
- Myocardial Infarction NCPDocument3 pagesMyocardial Infarction NCPlapistolero33% (3)
- NCP - Acute Pain Related Myocardial IschemiaDocument2 pagesNCP - Acute Pain Related Myocardial IschemiaKian HerreraNo ratings yet
- Acute Coronary Syndrome NCP 03Document6 pagesAcute Coronary Syndrome NCP 03AgronaSlaughterNo ratings yet
- NCP For AnginaDocument5 pagesNCP For Anginacarizza_bernas100% (1)
- Nursing Care Plan: Assessment Diagnosis Planning Intervention Rationale EvaluationDocument3 pagesNursing Care Plan: Assessment Diagnosis Planning Intervention Rationale Evaluationandronicoc100% (5)
- Nursing Care PlanDocument13 pagesNursing Care PlanCris Solis33% (3)
- NCP (Pulmonary Embolism)Document3 pagesNCP (Pulmonary Embolism)Nica Respondo73% (11)
- Assessment Nursing Diagnosis Planning Interventions Rationale EvaluationsDocument3 pagesAssessment Nursing Diagnosis Planning Interventions Rationale EvaluationsAjay SupanNo ratings yet
- NCP IcuDocument12 pagesNCP IcuHazel Palomares50% (2)
- NCP MiDocument4 pagesNCP MiPitaca Madiam Annabehl PaulNo ratings yet
- NCP - Tissue Perfusion (Cerebral)Document2 pagesNCP - Tissue Perfusion (Cerebral)moodlayers50% (6)
- Ncp-Angina - Doc NCPDocument1 pageNcp-Angina - Doc NCPVanes SaRn67% (3)
- Unstable AnginaDocument32 pagesUnstable AnginaMary Ann Lumbay Paye100% (2)
- Care Plan Hip Replacement 11-13-14Document13 pagesCare Plan Hip Replacement 11-13-14api-25636238050% (2)
- Myocardial InfarctionDocument21 pagesMyocardial InfarctionasdnofalNo ratings yet
- NCP On CKDDocument15 pagesNCP On CKDDr-Sanjay Singhania100% (1)
- Nursing Care PlansDocument6 pagesNursing Care PlansMichelle Danica Vicente PaswickNo ratings yet
- NCPDocument3 pagesNCPKrizelle Abadesco Libo-on50% (2)
- NCP MiDocument8 pagesNCP MiPitaca Madiam Annabehl PaulNo ratings yet
- Nursing Care Plan About Pulmonary EdemaDocument3 pagesNursing Care Plan About Pulmonary EdemaKaren Joy DelayNo ratings yet
- NCPDocument8 pagesNCPJose Benit DelacruzNo ratings yet
- 1) Nursing Careplan For FeverDocument9 pages1) Nursing Careplan For FeverY. Beatrice AbigailNo ratings yet
- NCP Inffective Tissue PerfusionDocument3 pagesNCP Inffective Tissue PerfusionPaul Cubacub0% (1)
- NCPDocument7 pagesNCPBeverLyNo ratings yet
- What Symptoms Should Lead The Nurse To Suspect The Pain May Be Angina?Document5 pagesWhat Symptoms Should Lead The Nurse To Suspect The Pain May Be Angina?Dylan Angelo AndresNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term Goal: IndependentDocument4 pagesAssessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term Goal: IndependentNinaNo ratings yet
- NCP FinalDocument18 pagesNCP FinalJessica Medina100% (1)
- Patient With Acute Coronary Syndrome: N D P GDocument3 pagesPatient With Acute Coronary Syndrome: N D P Gkazelle100% (1)
- RNPIDEA-Coronary Artery Disease Nursing Care PlanDocument8 pagesRNPIDEA-Coronary Artery Disease Nursing Care PlanAngie MandeoyaNo ratings yet
- NCPDocument17 pagesNCPShayne Jessemae AlmarioNo ratings yet
- NCPDocument9 pagesNCPLeolene Grace BautistaNo ratings yet
- Case 3Document4 pagesCase 3Vien Marie Palaubsanon SilawanNo ratings yet
- Nursing Care Plan For Carbon Monoxide PoisoningDocument3 pagesNursing Care Plan For Carbon Monoxide Poisoningderic73% (11)
- Nursing Care Plan For GlaucomaDocument3 pagesNursing Care Plan For Glaucomaderic79% (28)
- Nursing Care Plan For Readiness For Enhanced Hope NCPDocument4 pagesNursing Care Plan For Readiness For Enhanced Hope NCPderic100% (6)
- Nursing Care Plan For Overflow Urinary Incontinence NCPDocument2 pagesNursing Care Plan For Overflow Urinary Incontinence NCPderic71% (7)
- Nursing Care Plan For Peritonitis NCPDocument2 pagesNursing Care Plan For Peritonitis NCPderic86% (7)
- Nursing Care Plan For Pedia TB Meningitis NCPDocument2 pagesNursing Care Plan For Pedia TB Meningitis NCPderic100% (1)
- Eddie Struble - Spring Valley Police Report Page 1Document1 pageEddie Struble - Spring Valley Police Report Page 1watchkeepNo ratings yet
- H.mohamed Ibrahim Hussain A Study On Technology Updatiing and Its Impact Towards Employee Performance in Orcade Health Care PVT LTD ErodeDocument108 pagesH.mohamed Ibrahim Hussain A Study On Technology Updatiing and Its Impact Towards Employee Performance in Orcade Health Care PVT LTD ErodeeswariNo ratings yet
- Teal Motor Co. Vs CFIDocument6 pagesTeal Motor Co. Vs CFIJL A H-DimaculanganNo ratings yet
- Review and Basic Principles of PreservationDocument43 pagesReview and Basic Principles of PreservationKarl Marlou Bantaculo100% (1)
- Under Suitable Conditions, Butane, C: © OCR 2022. You May Photocopy ThisDocument13 pagesUnder Suitable Conditions, Butane, C: © OCR 2022. You May Photocopy ThisMahmud RahmanNo ratings yet
- Patricio Gerpe ResumeDocument2 pagesPatricio Gerpe ResumeAnonymous 3ID4TBNo ratings yet
- Coc 1 ExamDocument7 pagesCoc 1 ExamJelo BioNo ratings yet
- Distance SortDocument6 pagesDistance SortAI Coordinator - CSC JournalsNo ratings yet
- Jordan CVDocument2 pagesJordan CVJordan Ryan SomnerNo ratings yet
- Oral Com Reviewer 1ST QuarterDocument10 pagesOral Com Reviewer 1ST QuarterRaian PaderesuNo ratings yet
- Family Factors: Its Effect On The Academic Performance of The Grade 6 Pupils of East Bayugan Central Elementary SchoolDocument11 pagesFamily Factors: Its Effect On The Academic Performance of The Grade 6 Pupils of East Bayugan Central Elementary SchoolGrace Joy AsorNo ratings yet
- Ace 2Document184 pagesAce 2Raju LaxmipathiNo ratings yet
- HC+ Shoring System ScaffoldDocument31 pagesHC+ Shoring System ScaffoldShafiqNo ratings yet
- Technical DescriptionDocument2 pagesTechnical Descriptioncocis_alexandru04995No ratings yet
- Java Edition Data Values - Official Minecraft WikiDocument140 pagesJava Edition Data Values - Official Minecraft WikiCristian Rene SuárezNo ratings yet
- Quiz 2 I - Prefix and Suffix TestDocument10 pagesQuiz 2 I - Prefix and Suffix Testguait9No ratings yet
- 3 AcmeCorporation Fullstrategicplan 06052015 PDFDocument11 pages3 AcmeCorporation Fullstrategicplan 06052015 PDFDina DawoodNo ratings yet
- Ep Docx Sca SMSC - V2Document45 pagesEp Docx Sca SMSC - V290007No ratings yet
- Case Study in Architectural Structures: A-7E Avionics System - ADocument36 pagesCase Study in Architectural Structures: A-7E Avionics System - Ajckz8No ratings yet
- Beng (Hons) Telecommunications: Cohort: Btel/10B/Ft & Btel/09/FtDocument9 pagesBeng (Hons) Telecommunications: Cohort: Btel/10B/Ft & Btel/09/FtMarcelo BaptistaNo ratings yet
- Coefficient of Restitution - Center of MassDocument3 pagesCoefficient of Restitution - Center of MassMannyCesNo ratings yet
- Introduction of ProtozoaDocument31 pagesIntroduction of ProtozoaEINSTEIN2D100% (2)
- Limestone Standards PDFDocument2 pagesLimestone Standards PDFJacqueline BerueteNo ratings yet
- Preliminary Examination The Contemporary WorldDocument2 pagesPreliminary Examination The Contemporary WorldJane M100% (1)
- 6 RVFS - SWBL Ojt Evaluation FormDocument3 pages6 RVFS - SWBL Ojt Evaluation FormRoy SumugatNo ratings yet
- Reflective Memo 1-PracticumDocument5 pagesReflective Memo 1-Practicumapi-400515862No ratings yet
- Category (7) - Installation and Maintenance of Instrumentation and Control SystemsDocument3 pagesCategory (7) - Installation and Maintenance of Instrumentation and Control Systemstafseerahmed86No ratings yet
- Diazonium Salts Azo DyesDocument8 pagesDiazonium Salts Azo DyesAnthony Basanta100% (1)
- Chapter 10 OutlineDocument3 pagesChapter 10 OutlineFerrari75% (4)
- State Farm Claims: PO Box 52250 Phoenix AZ 85072-2250Document2 pagesState Farm Claims: PO Box 52250 Phoenix AZ 85072-2250georgia ann polley-yatesNo ratings yet