Professional Documents
Culture Documents
Ijeb 51 (9) 702-708
Uploaded by
bnkjayaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ijeb 51 (9) 702-708
Uploaded by
bnkjayaCopyright:
Available Formats
Indian Journal of Experimental Biology
Vol. 51, September 2013, pp. 702-708
Anti-diabetic and antihyperlipidemic effect of allopolyherbal formulation in
OGTT and STZ-induced diabetic rat model
Swati Manik, Vinod Gauttam & A N Kalia*
Department of Pharmacognosy, ISF College of Pharmacy, Moga, 1420 01, India
Received 11 October 2012; revised 3 June 2013
The present study was undertaken to evaluate the antidiabetic and antihyperlipidemic activities of Allopolyherbal
formulation (APHF) consisting of combinations of three well known medicinal plants used in traditional medicines (Trigonella
foenum graceum, Momordica charantia, Aegle marmelos) and synthetic oral hypoglycaemic drug (Glipizide-GL). The
optimized combination of lyophilized hydro-alcoholic extracts of drugs was 2:2:1 using OGTT model. The optimized PHF was
simultaneously administered with GL and optimized using OGTT model in diabetic rats and further studied in STZ-induced
diabetic rats for 21 days. The results (serum glucose level, lipid profile, hepatic enzymes and body weight) were compared with
the standard drug GL (10 mg/kg body wt). The optimized APHF (500+5 mg/kg body wt) has shown significant
antihyperglycemic and antihyperlipidemic activities. The results were comparable with the standard; even better than the GL
(10 mg/kg body wt) alone. The proposed hypothesis has reduced the no. of drug components from eight to three and dose
almost 50 % of both PHF and GL which fulfil the FDA requirements for export. Thus the developed APHF will be an ideal
alternative for the existing hypoglycemic formulations in the market with an additional advantage of hypolipidemic effect and
minimizing the cardiovascular risk factors associated with diabetes.
Keywords: Allopolyherbal formulation, Diabetes mellitus, OGTT model, Polyherbal formulation, Streptozotocin
Diabetes mellitus (DM) is one of the most severe,
incurable metabolic disorders characterized by
hyperglycaemia as a result of a relative, or an absolute,
lack of insulin, or the action of insulin on its target
tissue or both1. Besides hyperglycaemia, several other
symptoms, including hyperlipidemia, are involved in
the development of microvascular complication of
diabetes, which are the major causes of morbidity and
death2. It is a global public health problem, now
emerging as a world over epidemic. The number of
people with diabetes in India is currently around 40.9
million which is expected to rise to 69.9 million by
2025 unless urgent preventive steps not taken3.
Recently there has been a shift in universal trend
from synthetic to herbal medicine which can Return to
Nature as modern oral hypoglycaemic agents produce
undesirable side effects and herbal drugs/formulations
being preferred because of their effectiveness, minimal
side effects and relatively low cost4.
Management of diabetes without dyslipidemia and
various other associated side effects is still a challenge
to the medical community. Combination of allopathic
and herbal drugs can assist to overcome the resistance
due to insulin and/or oral hypoglycaemic therapy in
case of uncontrolled diabetes by reducing the dose of
allopathic drugs and their associated side effects.
There are so many oral hypoglycaemic drugs and
polyherbal formulations (PHFs) available in the
market but still diabetes is an uncontrolled disease, so
there is a need for alternative therapy for the
management of diabetes. An attempt has been made
to counteract the risk factors associated with chronic
oral hypoglycaemic drug by the new concept of
allopolyherbal formulation (APHF).
The literature survey also reveals that more than 50%
of polyherbal antidiabetic formulations available in the
market contain Trigonella foenum-graceum (Fenugreek,
Methi in Hindi), Momordica charantia (Bitter gourd,
Karela in Hindi) and Aegle marmelos (Wood apple, Bael
in Hindi) as one of their major components. Moreover,
these plants have been proved scientifically for their
antihyperglycemic and antihyperlipidemic, spasmolytic,
and digestive activities. They have different mechanisms
of action, therefore selected for the proposed study5-7.
____________
*Correspondent author
Telephone: 016363-324200 (O); +919915939996 (M)
E-mail: ankalia_47@rediffmail.com
Glipizide (GL) is one of the newest oral
hypoglycemic, effective and safe compound with
unique properties8.
MANIK et al: ANTIDIABETIC AND ANTIHYPERLIPIDEMIC EFFECT OF ALLOPOLYHERBAL FORMULATION
Lyophilized extracts of Methi, Karela and Bael were
combined in different ratios to find out the best
antihyperglycemic combination and then the optimized
formulation based on preliminary screening using Oral
glucose tolerance test (OGTT) model, was combined
with GL as APHF in different doses and were used to
investigate their effect on blood glucose, body weight,
lipid profile, serum glutamic oxaloacetic transaminase
(SGOT) and serum glutamic pyruvate transaminase
(SGPT) in streptozotocin (STZ) induced diabetic rat
model.
Materials and Methods
ChemicalsSTZ was purchased from Sigma
Aldrich Co. (St Louis, MO, USA), GL was from USV
Limited (Mumbai, India) and the kits for glucose
determination; total cholesterol, triglycerides, high
density lipoprotein cholesterol (HDL-c), SGOT and
SGPT were purchased from Coral Company (Goa,
India). All other chemicals and reagents used were of
laboratory grade and were purchased from LDH,
Ranbaxy and MERCK etc.
Plant materialThe plant materials i.e. Methi
seeds, Karela fruits and Bael leaves were procured
locally, in the month of August and were
authenticated by Dr. Adarsh Pal, Head, Department of
Botanical and Enviornmental Sciences, Guru Nanak
Dev University, Amritsar (Punjab) and voucher
specimens were deposited in the department for future
reference.
Extraction and lyophilizationAll the drugs were
dried, coarsely powdered and stored in a closed
container. Dried powder of Methi was defatted with
petroleum ether and then extracted by triple
maceration with 70% ethanol whereas dried powder
of fruit and leaves of Karela and Bael were extracted
with 50 and 70% ethanol respectively using triple
maceration. These extracts were concentrated under
vacuum, deep freezed for overnight and were
lyophilized.
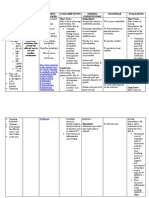
Development and optimization of polyherbal (PHF)
and allopolyherbal (APHF) formulationThe PHF
were developed by combining the lyophilized extracts
of selected plant materials in different experimental
ratios keeping Methi at constant ratio (Table 1) and
were optimized on the basis of OGTT study in normal
rats. The APHF were developed by mixing the
optimized PHF and GL in different experimental ratios
and optimized using OGTT studies in diabetic rats. The
optimized APHF was further evaluated by OGTT in
STZ-induced diabetic rat model.
703
AnimalsWistar rats (either sex) weighing
180-220 g were procured from the animal house of
I.S.F. College of Pharmacy, Moga (Reg. No.
816/PO/a/04/CPCSEA). The animals were kept in
polypropylene cages (3 in each cage) at an ambient
temperature of 252 C and 55-65% RH. A 12-12 h
light and dark schedule was maintained in the animal
house. The rats had free access to water and were fed
with commercially available feed. The protocol of the
experiment (IAEC/CPCSEA/2011/17) was approved
by Institutional Animal Ethics Committee and were
conducted in accordance with guidelines as per
Guide for the care and use of laboratory animal
and with permission from Committee for the Purpose
of Control and Supervision of Experiments on
Animals (CPCSEA).
Pharmacological screening
Optimization of PHF
Antihyperglycemic study in oral glucose tolerance
(OGTT) model in normal rats9Overnight fasted
normal rats were divided into 6 groups of 6 animals in
each. Gr. I Normal control (0.5% CMC solution); Gr. II
to IV were of different combination (PHF-A, PHF-B,
PHF-C)-1000 mg/kg b. wt; Gr. V PHF-B (500 mg/kg
body wt) and Gr. VI standard GL (10 mg/kg body wt).
The single dose of each prepared combination was
administered orally in the rats. All animals received
glucose (2 g/kg) orally after an hour of drug treatment.
The blood samples were withdrawn by retro-orbital
plexus under mild anaesthesia before administration of
the test drug-basal and at 0, 60 and 120 min after
glucose administration, the serum glucose was
estimated by glucose oxidase-peroxidase method10.
Induction of diabetesDiabetes was induced by a
single intra-peritoneal injection of freshly prepared
STZ (50 mg/kg body wt) in 0.1M citrate buffer (pH
4.5) to overnight fasted rats. STZ injected rats were
allowed to drink 20% glucose solution for 24 h to
prevent STZ-induced hypoglycaemic mortality11. The
development of diabetes was confirmed after 1 week
of STZ injection, the animals with fasting blood
Table 1Preparation of the polyherbal combination
Name of the formulation
Polyherbal formulation A
(PHF-A)-1000 mg/kg body wt.
Polyherbal formulation B
(PHF-B)-1000 mg/kg body wt.
Polyherbal formulation C
(PHF-C)-1000 mg/kg body wt.
Ratio of the plant material
Methi
Karela
Bael
2
1
2
2
INDIAN J EXP BIOL, SEPTEMBER 2013
704
glucose level more than 200 mg/dL were selected for
the present study12.
Optimization of the APHF
Antihyperglycemic study in oral glucose tolerance
test (OGTT) model in diabetic rats9Overnight
fasted diabetic rats were divided into 4 groups of 6
animals in each. Grouping of the animals was done as
mentioned below:
Gr. I Diabetic control (0.5% CMC solution); Gr. II
APHF A (500+5 mg/kg body wt); Gr. III APHF B
(750+5 mg/kg body wt) and Gr. IV GL (10 mg/kg
body wt).
Antihyperglycemic studies of optimized APHF in
STZ induced diabetic rat modelOn the basis of
OGTT studies in normal and diabetic rats dose was
selected for the STZ-induced diabetic rat model.
Experimental designAll diabetic rats were
randomly divided into following 5 groups of 6 each:
Gr. I
: Normal control (0.5% w/v CMC sol.)
: Diabetic control (0.5% w/v CMC sol.)
Gr. II
Gr. III : APHF A (500 mg/kg b. wt PHF-B+ 5 mg/kg
body wt GL)
Gr. IV : APHF B (750 mg/kg b. wt PHF-B+ 5 mg/kg
body wt GL)
Group V : GL 10 mg/kg body wt
All the test drugs were suspended in a vehicle
containing 0.5% (w/v) CMC in distilled water and
administered orally using an intra-gastric canula once
daily for 20 days.
The body weight of the animals was measured at
the onset of the study and at the regular intervals of
every week up to 21 days13.
The blood samples were collected on 0, 7, 14, 21
days of the study by puncturing the retro-orbital
plexus under mild anaesthesia. Serum was separated
by centrifugation at 3000 rpm for 15 min and used for
the estimation of glucose (GOD/POD method)10, total
cholesterol (CHOD/PAP method), total triglycerides
(TG) by GPO/PAP method, LDL-c, VLDL-c
(Freidewalds formula), and HDL-c levels (PEG
Precipitation method)14-17 Hepatic enzymes SGOT
and SGPT were determined using UV spectrometer18.
Postprandial studiesThe dose of APHF showing
the best antidiabetic activity in STZ-induced diabetic
rat model was selected for this study. Diabetic rats
fasted overnight were divided into four groups of six
rats each. Group I and III served as control (0.5% w/v
CMC sol.) and group II and IV received APHF B
(750 mg + 5 mg/ kg body wt).
In group I and III dose was given after meal and to
group II and IV it was given before meal. SGL was
taken initially and then food was given to the rats for
1 h and then dose was given after meal and before
meal to the respective groups and SGL was checked
at 2, 3 and 5 hrs after food administration.
Statistical analysisResults are presented as
meanSD. The statistical analysis involving two
groups was evaluated by means of two-way ANOVA
followed by Bonferroni post-test whereas one-way
ANOVA followed by Tukey post-test was used for
column analysis and P values (P<0.001 and P<0.05)
were considered to be significant.
Results and Discussion
Optimization of the formulation using OGTT normal
rat modelThe results showed 44.64 and 17.66% rise
in serum glucose level (SGL) after one hour of glucose
administration in vehicle control and GL (10 mg/kg b.
wt) pretreated groups, respectively. Whereas, group of
animals pretreated with the developed formulation
(PHF-A, PHF-B and PHF-C at the dose of 1000 mg/kg
b. wt, have shown rise in SGL by 28.26, 18.44 and
24.82%, respectively in comparison to 0 h (Table 2),
Table 2Effect of PHFs on serum glucose levels in OGTT model in normal rats
[Values are meanSD from 6 rate in each group. Figure in parentheses are % increase over O min values]
Groups
Normal control
PHF A (1000 mg/kg body wt)
PHF B (1000 mg/kg body wt)
PHF C (1000 mg/kg body wt)
PHF B (500 mg/kg body wt)
GL (10 mg/kg body wt)
a
Serum glucose levels (mg/dL
Basal
91.334.01
92.154.75
91.333.62
90.133.29
89.454.34
93.154.15
0 min
92.453.75
91.253.15
88.252.94
89.332.62
87.214.01
93.003.01
P< 0.001 vs normal vehicle control group. GL = Glipizide.
60 min
135.663.49 (44.64)
117.004.08 (28.26) a
105.003.01 (18.44) a
110.004.78 (24.82) a
110.004.15 (25.13) a
109.663.69 (17.66) a
120 min
99.253.16
96.663.85
93.753.75
94.002.16
94.373.75
95.002.63
MANIK et al: ANTIDIABETIC AND ANTIHYPERLIPIDEMIC EFFECT OF ALLOPOLYHERBAL FORMULATION
on the basis of results PHF-B was administered at the
dose of 500 mg/kg b. wt and have shown an increase
of 25.49% rise in SGL just at par with the 1000 mg/kg
b. wt dose of PHF-A & PHF-C, hence selected for
further study in STZ induced diabetic rat model.
However, all groups of animals almost normalize the
SGLs within two hours indicating that the pancreas of
animals was healthy to clear out the glucose load from
the body. The result of OGTT study had shown that
PHF-B consisting of Methi, Karela and Bael (2:2:1)
have maximum antihyperglycemic activity even at par
with the standard drug. This is because of Methi and
Karela in the higher ratio, possessing insulin
modulation action and extra-pancreatic effects such as
the regulation of glucose uptake from the intestinal
lumen by the inhibition of carbohydrate digestion by
Methi19; acting like insulin or promoting insulin
release by Karela20 as well as the synergistic effect of
the Bael for its extra-pancreatic effect7. Therefore,
PHF-B was selected for further study in combination
with GL in diabetic rats.
Optimization of the APHF using OGTT diabetic rat
modelVehicle treated group and GL (10 mg/kg
body wt) showed 62.02 and 33.6% increase,
respectively in SGL at 1 h after glucose
administration whereas, APHF A (500 mg+5 mg/kg
body wt) and APHF B (750 +5 mg/kg body wt)
showed 30.52 and 27.52% rise, respectively in SGLs
at 1 h compared to 0 h (Table 3). The results showed
that APHF combinations (A, B) have significantly
improved glucose tolerance in glucose induced
hyperglycaemia in comparison to PHF-B (500 and
1000 mg/kg body wt). This is because of the presence
of GL, as it has rapid absorption and onset of action, it
further have potentiated the insulin action. Its insulin
action is associated with an increase in plasma
membrane insulin receptor number, involves some
post receptor events, and is significantly greater on
peripheral uptake of glucose than suppression of
hepatic glucose production.21 However, when
compared with standard drug its activity was at par
with GL (10 mg/kg body weightt) Hence, our concept
of the development of the APHF has been achieved
and it was selected for further chronic study in STZ
induced diabetic rats.
Effect of APHF on serum glucose level and other
parameters of diabetic ratsDiabetic control rats
showed consistent and gradual rise in the fasting SGL
during the study. GL, (10 mg/kg body wt), APHF-A
(500+5 mg/kg body wt) and APHF-B (750+5 mg/kg
body wt) treated rats showed a reduction in SGL by
20.07, 34.49 and 47.08 %; 23.35, 39.39 and 49.20 %;
27.56, 42.15 and 54.40 % on 7th, 14th and 21st day of
the study, respectively as compared to onset of the
study and the results were found to be statistically
significant (P<0.001) as compared to diabetic control
group (Table 4).
The effect was found to be time dependent up to 21
day of the study. Decrease in SGL was more
significant (P<0.001) on 21st day in comparison to
14th and 7th days. The effect of developed APHF was
significant (P<0.001) when compared with standard
drug. This effect of APHF on SGL was due to the
synergistic effect of PHF and of GL. The PHF might
be due to the regeneration of cell in presence of
Methi22, Bael23 and preventing the death of cell by
Karela24. However, no significant difference was
observed when the results were compared between
high and low doses of APHF (Table 4). Hence, the
lower dose of APHF (500 + 5 mg/kg body wt) is
recommended for the management of SGL.
Body weightTable 5 shows the average body
weights of animals on 21st day. Reduction in body
weight was observed in diabetic animals. However,
animals treated with APHF A, APHF B and GL
registered the significant (P<0.001) check on the loss
of body weight on 21st day in comparison to onset day
of the study. This effect may be attributed to increased
Table 3Effect of APHF on serum glucose levels in OGTT in diabetic rats
[Values are meanSD from 6 rats in each group. Figures in parentheses are % increase of serum glucose lever
over O min values]
Groups
Diabetic control
APHF A (500 mg+5 mg/kg body wt)
APHF B (750 mg+5 mg/kg body wt)
GL (10 mg/kg body wt)
a
P< 0.001 vs diabetic control group.
Serum glucose levels (mg/dL)
Basal
237.662.05
249.333.09
214.504.50
245.373.15
705
0 min
240.663.01
204.663.39
165.853.15
206.122.17
60 min
391.003.81 (62.02) a
268.003.55 (30.52) a
212.503.01 (27.52) a
275.452.84 (33.60) a
120 min.
301.332.34
221.004.32
174.504.01
228.423.75
INDIAN J EXP BIOL, SEPTEMBER 2013
706
insulin secretion and food consumption25, 26; increased
GLUT-4 transporter protein of muscles and increased
glucose utilization in the liver and muscle by Karela20.
Lipid profile and hepatic enzymesAfter 21 days of
the study, animals of the diabetic control group showed
a significant (P<0.05) rise in serum cholesterol, TG,
LDL-c, VLDL-c, SGOT and SGPT levels, whereas,
significant reduction (P<0.05) was seen in serum HDLc in comparison to normal rats. The animals treated
with GL, APHF A and APHF B showed significant
(P<0.05) check on these abnormal levels of cholesterol,
TG, LDL-c, VLDL-c, SGOT and SGPT levels and
HDL-c levels in comparison to diabetic animals (Table
5). The developed APHF has proved to be more
effective in improving lipid metabolism as compared to
GL because Bael exerts its action by interfering with
the biosynthesis of cholesterol and utilization of
lipids27, hypo-cholesterolemic effect of Karela20 and
Methi seeds increase biliary cholesterol excretion in
liver due to sapogenins28 and the lipotropic effect of the
lecithin22. These results implied that developed
formulation can reduce the complications of lipid
metabolism and associated cardiovascular risk factors
during diabetes.
Table 4Effect of 20 days treatment of APHF on serum glucose levels of STZ-induced diabetic rats.
[Values are meanSD from rats in each group. Figures in parentheses are % increase of serum glucose level
over O day values]
Groups
Serum glucose levels (mg/dL)
0 day
Normal group
Diabetic control
APHF A (500 mg+5 mg/kg body wt)
7 day
14 day
21 day
85.165.98
262.135.01
250.835.53
85.006.05
84.664.85
86.166.07
271.536.13a
293.225.23a
310.106.53a
189.506.99
149.336.03
122.337.90
(23.35) abc
(39.39) abc
(49.20) abc
APHF B (750 mg+5 mg/kg body wt)
254.836.05
181.837.13
145.165.74
112.506.45
(27.56) abc
(42.15) abc
(54.40) abc
GL (10 mg/kg body wt)
267.005.29
211.336.30
169.668.71
138.006.08
(20.07) ab
(34.49) ab
(47.08) ab
a
b
c
Pvlaues: <0.001; Vs normal control group; diabetic control group; cGL treated group Figures in parentheses
are % decrease of serum glucose level over 0 day values.
Table 5Effect of APHF treatment on body weight, serum lipids and hepatic enzymes in STZ-induced diabetic rats on 21 day
[Values are meanSD from 6 rats in each group. Figures in parentheses are % increase/decrease]
Parameters
Groups
Normal
control
Diabetic
control
Body weight (g)
209.805.96
Cholesterol (mg/dL)
96.455.38
TG (mg/dL)
61.536.01
HDL-c (mg/dL)
42.354.01
VLDL-c (mg/dL)
12.454.15
LDL-c (mg/dL)
42.724.63
SGOT (U/L)
25.473.15
SGPT (U/L)
27.384.01
105.126.83
(45.12%)*
250.106.3
(151.79%)a
142.375.10
(118.34%)a
21.374.01
(45.25%)a
27.574.53
(93.37%)a
201.535.75
(337.76%)a
82.122.15
194.40%)a
79.373.78
164.89%)a
Pvalues: *<0.001, a<0.05 vs normal group
#<0.001, b<0.05 vs diabetic group
$ <0.001, c<0.05 vs Glipizide group
APHF-A
APHF-B
GL
(500 mg+5 mg/kg bdy wt) (750 mg+5 mg/kg body wt) (10 mg/kg body wt)
165.227.23
(17.54%)*#$
122.136.57
(49.80%)ab
92.476.75
(32.71%)ab
31.756.01
(48.77%)ab
19.733.15
(28.72%)ab
69.733.75
(64.55%)abc
23.153.23
68.69%)bc
24.494.17
65.53%)b
158.125.15
(15.18)*#$
112.475.20
(54.10%)abc
80.127.01
(40.91%)abc
40.533.15
(72.12%)bc
16.154.32
(36.23%)b
54.383.79
(71.93%)abc
15.474.15
(76.71%)abc
17.013.78
74.99%)abc
143.345.01
(19.87)*#
130.737.01
(46.27%)ab
95.347.34
(30.37%)ab
27.575.34
(29.66%)a
20.473.25
(26.10%)ab
79.134.10
(59.24%)ab
29.143.78
(59.84%)b
29.784.01
(59.36%)b
MANIK et al: ANTIDIABETIC AND ANTIHYPERLIPIDEMIC EFFECT OF ALLOPOLYHERBAL FORMULATION
707
Table 6Effect of APHF on serum glucose levels on postprandial studies in diabetic rats
[Values are meanSD from 6 rats in each group. Figures in parentheses are % increase of serum glucose level over O day values]
Groups
Dose administered after meal
Diabetic control group
APHF D
(750+5 mg/kg body wt.)
Serum glucose levels (mg/dL)
Basal
2h
3h
5h
204.002.94
302.332.05
(47.08)
257.453.01
(25.28)a
283.003.01
(38.20)
245.152.15
(18.95)a
268.662.86
(31.20)
230.753.15
(12.50)a
355.352.75
(40.34)
275.753.15
(14.29)a
311.753.45
(23.53)
252.272.75
(4.51)a
290.682.86
(15.04)
237.152.15
(1.93)a
205.152.75
Dose administered before meal
Diabetic control group
252.003.15
APHF D
(750+5 mg/kg body wt.)
240.004.01
P< 0.001 vs diabetic control group.
Hepatotoxicity is another risk factor associated
with oral hypoglycemics treatment on long term use.
This risk factor can be minimized by reducing the
dose of oral hypoglycemics in combination with
herbal drugs. Karela and Bael have been already
proved as hepatoprotective agents29,30. The APHFs (A,
B) exhibited better results than GL in the
improvement of hepatic enzymes SGOT and SGPT
levels (Table 5) indicating that the liver damage is to
a less extent in rats treated with APHFs than with GL
alone (10 mg/kg body wt).
Effect of APHF on postprandial studies in diabetic
ratsThe postprandial study in diabetic animals have
shown that the developed APHF is more effective if it
is given before food, which may be due to the
medication of enhanced insulin secretion by Bael and
the results were found to be significant (P<0.001) as
compared to respective diabetic control group
(Table 6). This effect may be due to the insulin
secretagogue effect by Bael; insulino-mimetic effect
of Karela and glucosidase enzyme inhibitory effect
of Methi. Moreover, blood glucose lowering effect of
the developed formulation is improved when it was
given before meal.
Toxicity studyThroughout the period of study,
animals treated with developed APHFs did not show
any behavioural changes and mortality as evident
from results showing normal hepatic functions,
therefore on this basis no separate toxicity studies
were carried out.
Conclusion
The postprandial study in diabetic animals have
shown that the developed APHF is more effective if it
is given before food, which may be due to the
mediation of enhanced insulin secretion by Bael,
inhibition of alpha amylase enzyme by Methi31 and
insulin like effect of Karela. Moreover, blood
glucose-lowering effect is improved when GL is
given before meal32 (Table 6).
The developed APHFs at lower dose of (500 mg/kg
body weight PHF + 5 mg/kg body wt GL) is
recommended for the management of diabetes and its
complications as it was found to be more effective
than standard drug GL (10 mg/kg body wt) alone and
the side effects associated with GL can be reduced as
its dose is reduced. There was no behavioural toxicity;
hepato-toxicity and mortality have been observed
during the complete duration of study. Hence,
developed APHF may be an ideal alternative for the
existing antihyperglycemic formulations with an
additional advantage of antihyperlipidemic effect and
minimizing the cardiovascular risk factors associated
with diabetes mellitus, hence, the concept has been
achieved.
It may be concluded that these findings will open a
new vista in the area of medical science for
the development of therapeutic approach for
the management of diabetes by simultaneous
administration of polyherbal formulation and synthetic
drug as this approach has reduced the dose, side effects
and adverse biological interaction of synthetic drug.
Acknowledgement
Thanks are due to Prof. P. L. Sharma, Head,
Department of Pharmacology for criticism and Shri
Parveen Garg (Chairman, ISFCP, Moga) for
infrastructure.
708
INDIAN J EXP BIOL, SEPTEMBER 2013
References
1 Ahmad F, Azevedo J L, Cortright R, Dohm G L & Goldstein
B J, Alterations in skeletal muscle protein-tyrosine
phosphatase activity and expression in insulin resistant human
obesity and diabetes, J Clin Invest, 100 (1997) 449.
2 Taskinen M R, Diabetic dyslipidemia, Atherosclerosis
Supplements, 3 (2002) 47.
3 Sandeep S, Ganesan A & Mohan V, Development and
updation of the diabetes atlas of India (Madras Diabetes
Research Foundation, Chennai) (2007) 1.
4 Venkatesh S, Reddy G D, Reddy B M, Ramesh M & Appa
Rao A V N, Antihyperglycemic activity of Caramulla
attenuate, Fitoterapia, 74 (2003) 274.
5 Mohammad I & Mohammad Y, Clinical evaluation of
antidiabetic activity of Trigonella seeds and Aegle marmelos
leaves, World Appl Sci J, 71 (2009) 231.
6 Waheed A, Miana G A, Sharafatullah T & Ahmad S I, Clinical
investigation of hypoglycemic effect of unripe fruit on
Momordica charantia in Type-2 (NIDDM) diabetes mellitus,
Pak J. Pharmacol, 25 (2008) 7.
7 Sachdewa A, Raina D, Srivastava A K & Khemani L D, Effect
of Aegle marmelos and Hibiscus rosa sinensis leaf extract on
glucose tolerance in glucose induced hyperglycemic rats
(Charles foster), J Environ Biol, 22 (2001) 53.
8 Charles R S, Glipizide: An overview, Am J Med, 75 (1983) 55.
9 Baron A D, Postprandial hyperglycemia and -glucosidase
inhibitors, Diabetes Res Clin Pr, 40 (1998) S51.
10 Trinder P, Determination of blood glucose using an oxidaseperoxidase system with a non carcinogenic chromogen, J Clin
Pathol, 22 (1969) 158.
11 Chandramohan G, Khalid S, Numair Al & Pugalendi K V,
Effect of 3-hydroxymethyl xylitol on hepatic and renal
functional markers and protein levels in streptozotocin diabetic
rats, Afr J Biochem Res, 3 (2009) 198.
12 Shanmugasundaram E R, Gopinath K L, Shanmugasundaram
K R & Rajendaran V M, Possible regeneration of the islets of
Langerhans in streptozotocin diabetic rats given Gymnema
sylvestre leaf extracts, J Ethnopharmacol, 30 (1990) 265.
13 Vijayalakshmi M, Noor A, Gunasekaran S & Manickam A S,
Antidiabetic activity of Aloe vera and histopathology of organs
in Streptozotocin induced diabetic rats, Curr Sci, 94 (2008)
1070.
14 Roeschlau P, Bernt E & Gruber W J, Estimation of serum
cholesterol by cholesterol oxidase and peroxidase method, J
Clin Chem Biochem, 12 (1974) 40.
15 Rifai N, Bachorik P S & Albers J J, Lipids, lipoproteins and
apolipoproteins, In Textbook of clinical chemistry, third edition
edited by CA Burtis & E R Ashwood, (W. B. Saunders
Company, Philadelphia) 1999, 809.
16 Friedewald W T, Levy R T & Frederickson D S, Estimation of
VLDL- and LDL- cholesterol, Clin Chem, 18 (1972) 499.
17 Warnick G R, Nguyen T & Albers A, A comparison of
improved precipitation methods for quantification of high
density lipoprotein cholesterol, Clin Chem, 26 (1985) 1775.
18 Expert Panel of the IFCC on Enzymes, Committee on
standards of IFCC provisional recommendations on IFCC
19
20
21
22
23
24
25
26
27
28
29
30
31
32
methods for measurement of catalytic concentration of
enzymes. Part 2. IFCC method for aspartate transferase, Clin
Chim Acta, 70 (1976) F19.
Hamza N, Berke B, Cheze C, Raphaele L G, Umar A, Agli A
N, Lassalle R, Jove J, Gin H & Moore N, Preventive and
curative effect of Trigonella foenum-graecum L. eeds in
C57BL/6J models of type 2 diabetes induced by high-fat diet, J
Ethnopharmacol, 142 (2) (2012) 516.
Grover J K & Yadav S P, Pharmacological actions and
potential uses of Momordica charantia: a review, J
Ethnopharmacol, 93 (2004) 123.
Harold E L & Mark N F, New Perspectives in NoninsulinDependent Diabetes Mellitus and the Role of Glipizide in Its
Treatment, Mechanism of action of the second-generation
sulfonylurea glipizide, Am J Med, 75 (1983) 46.
Enas A M K, Biochemical and histopathological studies on the
influence of aqueous extract of fenugreek seed (Trigonella
foenum graecum) on alloxan diabetic male rats, Egyp J Hosp
Med, 15 (2004) 83.
Das A V, Padayatti P S & Paulose C S, Effect of leaf extract of
Aegle marmelos (L) Correa ex Roxb. on histological and ultrastructural changes in tissues of streptozotocin induced diabetic
rats, Indian J Exp Biol, 34 (1996) 341.
Ahmed I, Adeghate E, Sharma A K, Pallot D J & Singh J,
Effects of Momordica charantia fruit juice on islet
morphology in the pancreas of the streptozotocin-diabetic rats,
Diabetes Res Clin Pract, 40 (1998) 145.
Fernstrom M H & Fernstrom J D, Large changes in serum free
tryptophan levels do not alter brain tryptophan levels: Studies
in streptozotocin-diabetic rats, Life Sci, 52 (1993) 907.
Farouque H M O & Meredith L T, Effects of inhibition of ATP
sensitive potassium channels on metabolic vasodilation in the
human forearm, Clin Sci, 104 (2003) 39.
Vijaya C, Ramanathan M & Suresh B, Lipid lowering activity
of ethanolic extract of leaves of Aegle marmelos (Linn.) in
hyperlipidaemic models of Wistar albino rats, Indian J Exp
Biol, 47 (2009) 182.
Baquer N Z, Kumar P, Taha A, Kale R K, Cowsik S M &
McLean P, Metabolic and molecular action of Trigonella
foenum-graecum (fenugreek) and trace metals in experimental
diabetic tissues, J Biosci, 36 (2011) 383.
Hossain M S, Ahmed M & Islam A, Hypolipidemic and
hepatoprotective effects of different fractions of methanolic
extract of Momordica charantia (Linn.) in alloxan induced
diabetic rats, Int J Pharma Sci Res, 2 (2011) 601.
Khan T H & Sultana S, Antioxidant and hepatoprotective
potential of Aegle marmelos Correa. against CCl4-induced
oxidative stress and early tumor events, J Enzyme Inhib Med
Chem, 24 (2009) 320.
Amin R, Abdul-Ghani A S & Suleiman M S, Effect of
Trigonella foenum graecum on intestinal absorption, Proc of
the 47th Annual Meeting of the American Diabetes
Association (Indianapolis USA), Diabetes, 36 (1987) 211a.
Melander A & Wahlin-Boll E, Clinical pharmacology
of glipizide, Am J Med, 75 (1983) 41.
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Testing Myths HP Network VirtualizationDocument12 pagesTesting Myths HP Network VirtualizationbnkjayaNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Sri Venkatachala Mahatmyam Part 1Document317 pagesSri Venkatachala Mahatmyam Part 1bnkjayaNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- ChallanDocument1 pageChallanapi-279452985No ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- P Block Elements Via Group Elements - UnlockedDocument26 pagesP Block Elements Via Group Elements - UnlockedbnkjayaNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- As A Man Thinketh Free EbookDocument14 pagesAs A Man Thinketh Free EbookSahil GuptaNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Lesson Plan - Jayasimha ChemDocument2 pagesLesson Plan - Jayasimha ChembnkjayaNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Quantum NumbersDocument30 pagesQuantum NumbersbnkjayaNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- UGC Notification Main Dec2015Document8 pagesUGC Notification Main Dec2015Aal Arif SarkarNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Ogtt in RatsDocument10 pagesOgtt in RatsbnkjayaNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Lipid Per Oxidation MechanismDocument18 pagesLipid Per Oxidation MechanismbnkjayaNo ratings yet
- Anti-Diabetic and Antioxidant Effects of Virgin Coconut Oil in Alloxan Induced Diabetic Male Sprague Dawley RatsDocument6 pagesAnti-Diabetic and Antioxidant Effects of Virgin Coconut Oil in Alloxan Induced Diabetic Male Sprague Dawley RatsbnkjayaNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Anti Oxidant EnymesDocument15 pagesAnti Oxidant EnymesbnkjayaNo ratings yet
- Anti Diabetic StudiDocument3 pagesAnti Diabetic StudibnkjayaNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Chemistry Scheme of Evaluation VIII STDDocument5 pagesChemistry Scheme of Evaluation VIII STDbnkjayaNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Mda 3Document7 pagesMda 3bnkjayaNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Ix MCQDocument6 pagesIx MCQbnkjayaNo ratings yet
- r1 r2 d2/d1 r1 r2 d1/d2 r2 r1 d2/d1 r1 r2 d2 d1Document2 pagesr1 r2 d2/d1 r1 r2 d1/d2 r2 r1 d2/d1 r1 r2 d2 d1bnkjayaNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Pre PHD Exam Question Paper PatternDocument1 pagePre PHD Exam Question Paper PatternbnkjayaNo ratings yet
- AtomsDocument12 pagesAtomsbnkjayaNo ratings yet
- Quantum NumbersDocument30 pagesQuantum NumbersbnkjayaNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Current ElectricityDocument10 pagesCurrent ElectricitybnkjayaNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- VIII STD CBS QBDocument5 pagesVIII STD CBS QBbnkjayaNo ratings yet
- Js MusclesDocument88 pagesJs MusclesbnkjayaNo ratings yet
- Astronomical ConstantsDocument1 pageAstronomical ConstantsbnkjayaNo ratings yet
- Magnetic Properties of Co Ordination CompoundsDocument14 pagesMagnetic Properties of Co Ordination CompoundsbnkjayaNo ratings yet
- Electron ConfDocument79 pagesElectron Confpk2varmaNo ratings yet
- Manual TestingDocument77 pagesManual TestingShaik Iliaz50% (2)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Current State of Diabetes Mellitus in IndiaDocument4 pagesThe Current State of Diabetes Mellitus in IndiaSanjay NavaleNo ratings yet
- Lawlor Et Al. (2017) Service User Satisfaction With CBTPDocument19 pagesLawlor Et Al. (2017) Service User Satisfaction With CBTPnuriasegarramarNo ratings yet
- Neuroscience and Biobehavioral Reviews: Janne C. Visser, Nanda N.J. Rommelse, Corina U. Greven, Jan K. BuitelaarDocument35 pagesNeuroscience and Biobehavioral Reviews: Janne C. Visser, Nanda N.J. Rommelse, Corina U. Greven, Jan K. BuitelaarCristinaNo ratings yet
- Milk Fever and Pregnancy Toxemia AssignmentDocument16 pagesMilk Fever and Pregnancy Toxemia AssignmentAmaru ErskineNo ratings yet
- Hipster Kedai Kopi Penjualan Lipat-Tiga Brosur 3Document3 pagesHipster Kedai Kopi Penjualan Lipat-Tiga Brosur 3Apung JoniNo ratings yet
- Benedict James Roldan BermasDocument4 pagesBenedict James Roldan BermasBenedict James BermasNo ratings yet
- Pembukaan Survei Pendampingan Akreditasi Rsu Permata Bunda - GroboganDocument14 pagesPembukaan Survei Pendampingan Akreditasi Rsu Permata Bunda - GroboganAli MuhsonNo ratings yet
- Full Download Health Safety and Nutrition For The Young Child 9th Edition Marotz Test BankDocument26 pagesFull Download Health Safety and Nutrition For The Young Child 9th Edition Marotz Test Bankretainalgrainascjy100% (37)
- Acute Pain Nursing Care PlanDocument3 pagesAcute Pain Nursing Care PlanSiafei RabeNo ratings yet
- LHV Diploma Course Prospectus 2023 Onward 1Document35 pagesLHV Diploma Course Prospectus 2023 Onward 1Rashid MehmoodNo ratings yet
- PR2 Chapter1 SleepqualityDocument9 pagesPR2 Chapter1 SleepqualityhoneypiecreamyteaNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Quick Guide Effective Record Keeping Ordering MedicinesDocument4 pagesQuick Guide Effective Record Keeping Ordering MedicinesnunikwahyuniNo ratings yet
- Trabajo de InglesDocument9 pagesTrabajo de InglesCoronado Ramirez, Jesús DavidNo ratings yet
- Senam Lanjut AerobikDocument14 pagesSenam Lanjut AerobikAziz CupinNo ratings yet
- The Concept of Value AdditionDocument5 pagesThe Concept of Value AdditionNura BasmerNo ratings yet
- Agron 3610 2016 SSR PDFDocument101 pagesAgron 3610 2016 SSR PDFkishore_bulli6666No ratings yet
- ZoxubitefubowDocument2 pagesZoxubitefubowGohil ManishNo ratings yet
- Nhóm 3 - For MergeDocument5 pagesNhóm 3 - For Mergetrongphap.0203No ratings yet
- Pocket-Book MCH Emergencies - English PDFDocument286 pagesPocket-Book MCH Emergencies - English PDFAbigail Kusi-Amponsah100% (1)
- EcardDocument2 pagesEcardBITI Education Pvt. Ltd.No ratings yet
- TCS NQT Solved Paper - 12th Sept 2021 (Morning Slot)Document98 pagesTCS NQT Solved Paper - 12th Sept 2021 (Morning Slot)Shailesh SumanNo ratings yet
- Acr On Modular Learning SimulationDocument4 pagesAcr On Modular Learning SimulationAbba JoyNo ratings yet
- Reynolds Child Depression Scale ArticleDocument9 pagesReynolds Child Depression Scale ArticleColette MeeNo ratings yet
- Review Related LiteratureDocument3 pagesReview Related LiteraturerdsamsonNo ratings yet
- Educational Video Intervention Effects On Periprocedural Anxiety Levels Among Cardiac Catheterization Patients A Randomized Clinical TrialDocument17 pagesEducational Video Intervention Effects On Periprocedural Anxiety Levels Among Cardiac Catheterization Patients A Randomized Clinical TrialFajar SaputraNo ratings yet
- BFR PicoDocument1 pageBFR PicoErLz Catubig AlmendralNo ratings yet
- Exam Questions For Students 1-350Document26 pagesExam Questions For Students 1-350Komal valve100% (2)
- GERIATRICE HEALTH CARE TEAM-FinalDocument6 pagesGERIATRICE HEALTH CARE TEAM-Finalcamile buhangin100% (2)
- Pnas 1609811114Document6 pagesPnas 1609811114CAMILLE HAMNo ratings yet
- Compounding in Hospital SettingDocument22 pagesCompounding in Hospital Settingkhangsiean89100% (1)
- IPE Interprofessional EducationDocument10 pagesIPE Interprofessional EducationdewaNo ratings yet
- Summary of Mary Claire Haver's The Galveston DietFrom EverandSummary of Mary Claire Haver's The Galveston DietRating: 5 out of 5 stars5/5 (1)
- The Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyFrom EverandThe Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyRating: 4.5 out of 5 stars4.5/5 (3)
- Instant Loss On a Budget: Super-Affordable Recipes for the Health-Conscious CookFrom EverandInstant Loss On a Budget: Super-Affordable Recipes for the Health-Conscious CookRating: 3.5 out of 5 stars3.5/5 (2)
- Gut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)From EverandGut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)Rating: 4 out of 5 stars4/5 (378)
- Forever Strong: A New, Science-Based Strategy for Aging WellFrom EverandForever Strong: A New, Science-Based Strategy for Aging WellNo ratings yet
- The Beck Diet Solution Weight Loss Workbook: The 6-Week Plan to Train Your Brain to Think Like a Thin PersonFrom EverandThe Beck Diet Solution Weight Loss Workbook: The 6-Week Plan to Train Your Brain to Think Like a Thin PersonRating: 3.5 out of 5 stars3.5/5 (33)