Professional Documents
Culture Documents
Maternal Age - and Gestation-Specific Risk For Trisomy 21
Uploaded by
temmyOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Maternal Age - and Gestation-Specific Risk For Trisomy 21
Uploaded by
temmyCopyright:
Available Formats
Ultrasound Obstet Gynecol 1999;13:167170
Maternal age- and gestation-specific risk for
trisomy 21
R. J. M. Snijders, K. Sundberg*, W. Holzgreve, G. Henry and K. H. Nicolaides
Harris Birthright Research Centre for Fetal Medicine, Kings College Hospital Medical School, London, UK;
*Department of Obstetrics and Gynecology, Rigshospitalet, Copenhagen, Denmark; Department of Obstetrics and
Gynecology, Universitt Frauenklinik, Basel, Switzerland; Reproductive Genetics Center, Denver, USA
Key words:
TRISOMY 21, CHROMOSOMAL DEFECTS, MATERNAL AGE, RISK COUNSELLING, NUCHAL TRANSLUCENCY
ABSTRACT
INTRODUCTION
Objective To provide estimates of maternal age- and
gestational age-related risks for trisomy 21.
Estimates of the maternal age-related risk for trisomy 21 at
birth are based on two surveys with almost complete ascertainment; in a survey in South Belgium, every neonate was
examined for features of trisomy 21, and, in a survey in
Sweden, information was verified using several sources
such as hospital notes, cytogenetic laboratories, genetic
clinics and schools for the mentally handicapped13.
During the past decade, with the introduction of maternal serum biochemistry and ultrasound screening for
chromosomal defects at different stages of pregnancy, it has
become necessary to establish maternal age- and gestational age-specific risks for chromosomal defects. Previous
studies derived such estimates by comparing the birth
prevalence of trisomy 211 to the prevalence reported in two
multicenter studies on amniocentesis at 1620 weeks of
gestation4,5 and the prevalence in small series on chorionic
villus sampling at 914 weeks of gestation6,7. In this study,
we revised our previous estimates by examining 57 614
pregnancies that were karyotyped at 916 weeks of gestation. Furthermore, we examined the accuracy of these estimates in a group of 96 127 singleton pregnancies with
complete follow-up that were recruited at 1014 weeks of
gestation8.
Methods The prevalence of trisomy 21 was examined in
57 614 women who had fetal karyotyping at 916 weeks
of gestation for the sole indication of maternal age of 35
years or more. On the basis of the maternal age distribution and the reported maternal age-related risk for trisomy
21 at birth, the expected number of trisomy 21 cases was
calculated for each gestational age subgroup (910 weeks,
1114 weeks and 1516 weeks). The ratio of the observed
to expected number of cases of trisomy 21 was then calculated and regression analysis was applied to derive a
smoothened curve. The formula for maternal age- and gestational age-related risk was then applied to a population
of 96 127 pregnancies that were examined at 1014 weeks
to calculate the expected number of trisomy 21 pregnancies, and this number was compared to the observed
number of 326.
Results In the 57 614 pregnancies there were 538 cases
of trisomy 21. The relative prevalences of trisomy 21,
compared to a prevalence of 1.0 at 40 weeks, was
10 exp(0.2718 log10(gestation)2 1.023 log10(gestation) + 0.9425). On the basis of the estimated maternal
age- and gestational age-related risks, the expected number
of trisomy 21 cases at 1014 weeks of gestation in the 96
127 pregnancies was 329 (95% confidence interval
291361), which was not significantly different from the
observed number of 326 cases (2 = 0.02).
SUBJECTS AND METHODS
Estimate of risk
To calculate estimates of risk for trisomy 21 at different
gestations, we used data from 57 614 women who had
fetal karyotyping at 916 weeks of gestation for the sole
indication of maternal age of 35 years or more. On
the basis of the maternal age distribution and maternal
age-related risk for trisomy 21 at birth1, the expected
Conclusion The risk for trisomy 21 increases with maternal age and decreases with gestation. The prevalence of
trisomy 21 at 12 and 16 weeks of gestation is higher than
the prevalence at 40 weeks by 30% and 21%, respectively.
Correspondence: Professor K. H. Nicolaides, Harris Birthright Research Centre for Fetal Medicine, Kings College Hospital Medical School,
Denmark Hill, London SE5 8RX, UK
167
O R I GI N A L PAP E R
98/133
AMA: First Proof
Received 18698
Revised 111298
Accepted 5199
Maternal age and gestation in trisomy 21 risk
Snijders et al.
number of trisomy 21 cases was calculated for each gestational age subgroup (910 weeks, 1114 weeks and 1516
weeks) and for each maternal age. In these calculations, the
appropriate corrections were made for those women whose
age in years would increase between the time of antenatal
assessment at 916 weeks and the time of delivery. Gestational age was available in completed weeks. Pearson
correlation analysis was applied to examine whether the
ratio changed significantly with maternal age and/or gestation. Regression analysis was applied to ratios at 910
weeks, 1114 weeks, 1516 weeks and 40 weeks (where
the ratio was set at one) to derive a smoothened curve for
the decrease in ratio with gestational age.
Validation of the model
In a multicenter study of screening for trisomy 21 by combination of maternal age and fetal nuchal translucency
thickness at 1014 weeks of gestation, we obtained details
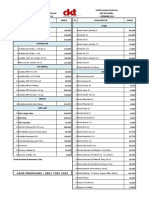
Table 1
RESULTS
The maternal age and gestational age distributions of the
57 614 pregnancies are shown in Table 1. Trisomy 21 was
diagnosed in 538 cases (Table 2). The relative prevalence of
trisomy 21 (observed to expected ratio), compared to a
prevalence of 1.0 at 40 weeks, was not significantly associated with maternal age (r = 0.178; p = 0.31) but
decreased with gestational age (r = 0.812; p < 0.01).
Data were grouped to derive the relative prevalence at different gestations (Table 3) and regression
analysis was applied to derive a smoothened curve
Maternal age and gestational age distribution of the 57 614 women who had fetal karyotyping
Maternal
age (years)
35
36
37
38
39
40
41
42
43
44
45
Total
Table 2
on the outcome of 96 127 pregnancies8. This group included 326 pregnancies with trisomy 21. The new formula
for maternal age- and gestational age-related risk was
applied to this population, to calculate the expected
number of trisomy 21 pregnancies, and this number was
compared to the observed number of 326.
Gestational age (weeks)
9
10
11
12
13
14
15
16
Total
916
891
744
661
413
278
168
97
45
23
4
1832
1736
1486
1139
905
597
408
219
108
75
17
823
805
774
629
479
339
231
128
84
29
16
233
258
241
170
164
115
85
59
32
18
2
192
185
120
109
104
60
48
29
13
1
8
1139
971
779
567
364
274
172
96
46
30
9
3 676
3 101
2 363
1 789
1 211
749
459
283
135
64
24
5 252
4 484
3 388
2 614
1 740
1 147
689
357
184
86
27
14 063
12 431
9 895
7 678
5 380
3 559
2 260
1 268
647
326
107
4240
8522
4337
1377
869
4447
13 854
19 968
57 614
Maternal age and gestational age distribution of the 538 pregnancies with trisomy 21
Maternal
age
(years)
Gestational age (weeks)
9
10
11
12
13
14
15
16
Total
35
36
37
38
39
40
41
42
43
44
45
5
6
7
8
7
3
4
4
2
1
0
9
9
10
11
16
14
11
8
5
5
2
5
4
7
5
8
8
4
3
4
1
2
1
2
2
2
1
2
2
2
1
0
0
0
1
0
1
1
1
1
1
1
0
1
4
5
5
5
5
4
3
2
2
1
1
14
16
15
14
14
14
10
7
5
3
1
18
31
18
25
23
10
16
12
7
5
2
56
74
64
71
75
56
51
39
27
16
9
47
100
51
15
37
113
167
538
Total
Table 3
Observed number of cases with trisomy 21 compared to the number expected in live births in relation to gestational age
Gestational age
(weeks)
9 + 010 + 6
11 + 014 + 6
15 + 016 + 6
Observed
Expected
Ratio
95% confidence
interval
Regressed ratio
12 762
11 030
33 822
147
111
280
93.6
82.4
217.8
1.57
1.35
1.29
1.321.82
1.101.60
1.141.44
1.55
1.38
1.27
168 Ultrasound in Obstetrics and Gynecology
AMA: First Proof
98/133
Maternal age and gestation in trisomy 21 risk
Snijders et al.
[log10(relative prevalence) = 0.2718 log10(gestation)2
1.023 log10(gestation) + 0.9425]. The estimated maternal
age- and gestational age-related risks for trisomy 21 are
given in Table 4. The estimated rates of spontaneous fetal
death between different gestations and delivery at 40 weeks
were derived on the basis of the relative prevalences
between these gestations and 40 weeks (Table 5).
of gestation. The expected number of cases with trisomy 21
was estimated to be 329 (95% confidence interval
291361). This number is not significantly different from
the observed number of 326 cases (2 = 0.02). There was
no significant difference between the observed and expected numbers for different gestational age and maternal
age subgroups (Table 6).
Validation of the model
DISCUSSION
The accuracy of the model was examined on the basis of
findings in 96 127 pregnancies examined at 1014 weeks
This study provides revised estimates of maternal age- and
gestational age-related risk for trisomy 21. Compared to
our previous report7, in this study the number of cases with
fetal karyotyping was much higher (57 614 compared to
15 793). Additionally, in this study the appropriate corrections were made for the increase in maternal age with
advancing gestation.
The estimates for the rate of spontaneous fetal death for
trisomy 21 are lower than in our previous report (30%
compared to 41% for the loss rate between 12 and 40
weeks of gestation and 21% compared to 31% for the loss
rate between 16 and 40 weeks)7. The main reason for this
apparent discrepancy is that in the previous analysis there
was no correction for the increase in maternal age with
advancing gestation. This led to an underestimate for the
expected number of trisomy 21 live births and thus to an
overestimate of the loss rate. The new estimates of loss
rates are similar to the 31% from 12 weeks and 18% from
16 weeks reported by Halliday and colleagues9; they compared the prevalence of trisomy 21 in 10 545 women
having chorionic villus sampling or amniocentesis for the
sole indication of maternal age of 36 years or more, to the
prevalence in live births from 12 921 women of similar age
who did not have fetal karyotyping9.
Assessment of the model on the basis of findings in
96 127 pregnancies indicates that the estimated prevalences
are accurate at least for the gestational range of 1014
weeks; the estimates at 16 weeks and 20 weeks of gestation
require validation with an independent data set.
The model makes it possible to counsel patients presenting at different stages of pregnancy concerning the risk that
their fetus has trisomy 21 and the chances that the pregnancy will result in a live birth with this condition. Furthermore, the data can be used to calculate the expected
Table 4 Prevalence of trisomy 21 by maternal age and gestational age
Maternal
age
(years)
20
25
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
Gestational age (weeks)
10
12
14
16
20
40
1/983
1/870
1/576
1/500
1/424
1/352
1/287
1/229
1/180
1/140
1/108
1/82
1/62
1/47
1/35
1/26
1/20
1/15
1/1068
1/946
1/626
1/543
1/461
1/383
1/312
1/249
1/196
1/152
1/117
1/89
1/68
1/51
1/38
1/29
1/21
1/16
1/1140
1/1009
1/668
1/580
1/492
1/409
1/333
1/266
1/209
1/163
1/125
1/95
1/72
1/54
1/41
1/30
1/23
1/17
1/1200
1/1062
1/703
1/610
1/518
1/430
1/350
1/280
1/220
1/171
1/131
1/100
1/76
1/57
1/43
1/32
1/24
1/18
1/1295
1/1147
1/759
1/658
1/559
1/464
1/378
1/302
1/238
1/185
1/142
1/108
1/82
1/62
1/46
1/35
1/26
1/19
1/1527
1/1352
1/895
1/776
1/659
1/547
1/446
1/356
1/280
1/218
1/167
1/128
1/97
1/73
1/55
1/41
1/30
1/23
Table 5 Estimates for spontaneous loss rates for
fetuses with trisomy 21 between various gestations
and delivery at 40 weeks
Gestational age (weeks)
Estimated loss rate (%)
36
30
25
21
10
12
14
16
Table 6
Expected and observed number of pregnancies with trisomy 21 for different gestations and maternal age subgroups
n
Expected
Observed number
Observed 95% CI
Gestational age (weeks)
10
11
12
13
4 889
34 046
42 884
14 308
15.8
119.1
146.2
48.0
11
137
141
37
518
114160
118164
2549
0.86
1.26
0.09
1.43
Maternal age (years)
< 30
3034
3539
40
39 834
32 489
20 263
3 541
46.2
73.9
128.2
80.8
36
67
125
98
2448
5183
103147
79117
1.03
0.25
0.02
1.51
Total
96 127
329.1
326
291361
0.02
Ultrasound in Obstetrics and Gynecology 169
98/133
AMA: First Proof
Maternal age and gestation in trisomy 21 risk
prevalence of trisomy 21 in any study group when new
ultrasonographic or biochemical methods of screening are
being evaluated.
ACKNOWLEDGEMENT
This study was supported by the Fetal Medicine
Foundation (UK registered charity 1037116).
REFERENCES
1. Hecht CA, Hook EB. The imprecision in rates of Down syndrome by 1-year maternal age intervals: a critical analysis of
rates used in biochemical screening. Prenat Diagn 1994;14:
72938
2. Koulisher L, Gillerot Y. Downs syndrome in Wallonia (South
Belgium), 19711978: cytogenetics and incidence. Hum Genet
1980;54:24350
3. Hook EB, Lindjo A. Down syndrome in live births by single
year maternal age interval in a Swedish study: comparison with
results from a New York State study. Am J Hum Genet 1978;
30:1927
Snijders et al.
4. Hook EB, Cross PK, Regal RR. The frequency of 47,+21,
47,+18, and 47,+13 at the uppermost extremes of maternal
ages: results on 56,094 fetuses studied prenatally and comparisons with data on livebirths. Hum Genet 1984;68:21120
5. Ferguson-Smith MA, Yates JRW. Maternal age specific rates
for chromosomal aberrations and factors influencing them:
report of a collaborative European study on 52,965 amniocenteses. Prenat Diagn 1984;4:544
6. Snijders RJM, Holzgreve W, Cuckle H, Nicolaides KH. Maternal age-specific risks for trisomies at 914 weeks gestation.
Prenat Diagn 1994;14:54352
7. Snijders RJM, Sebire NJ, Nicolaides KH. Maternal age and
gestational age-specific risk for chromosomal defects. Fetal
Diagn Ther 1995;10:35667
8. Snijders RJM, Noble P, Sebire N, Souka A, Nicolaides KH. UK
multicentre project on assessment of risk of trisomy 21 by
maternal age and fetal nuchal translucency thickness at 1014
weeks of gestation. Lancet 1998;352:3436
9. Halliday JL, Watson LF, Lumley J, Danks DM, Sheffield LJ.
New estimates of Down syndrome risks at chorionic villus
sampling, amniocentesis, and livebirth in women of advanced
maternal age from a uniquely defined population. Prenat Diagn
1995;15:45565
170 Ultrasound in Obstetrics and Gynecology
AMA: First Proof
98/133
You might also like
- Absolute Obstetric Anesthesia Review: The Complete Study Guide for Certification and RecertificationFrom EverandAbsolute Obstetric Anesthesia Review: The Complete Study Guide for Certification and RecertificationNo ratings yet
- Fast Facts: Complex Perianal Fistulas in Crohn's Disease: A multidisciplinary approach to a clinical challengeFrom EverandFast Facts: Complex Perianal Fistulas in Crohn's Disease: A multidisciplinary approach to a clinical challengeNo ratings yet
- Cavadino 2017Document6 pagesCavadino 2017christian roblesNo ratings yet
- 1 s2.0 S0002937897802177 MainDocument1 page1 s2.0 S0002937897802177 MainPutri AgriNo ratings yet
- Screening For Fetal Growth Restriction Using Ultrasound and The Sflt1/Plgf Ratio in Nulliparous Women: A Prospective Cohort StudyDocument13 pagesScreening For Fetal Growth Restriction Using Ultrasound and The Sflt1/Plgf Ratio in Nulliparous Women: A Prospective Cohort StudynicolasdlcaNo ratings yet
- The NeoUpdates - DecDocument7 pagesThe NeoUpdates - DecDr Satish MishraNo ratings yet
- 1 s2.0 S0002937804009159 MainDocument6 pages1 s2.0 S0002937804009159 MainNi Wayan Ana PsNo ratings yet
- Association Between Gestational Diabetes Mellitus.46Document7 pagesAssociation Between Gestational Diabetes Mellitus.46Frank MacíasNo ratings yet
- Postdates Induction With An Unfavorable Cervix and Risk of CesareanDocument6 pagesPostdates Induction With An Unfavorable Cervix and Risk of CesareanrobertNo ratings yet
- Good18.Prenatally Diagnosed Vasa Previa A.30Document9 pagesGood18.Prenatally Diagnosed Vasa Previa A.30wije0% (1)
- Risk of Respiratory Morbidity in Term Infants Delivered by Elective Caesarean Section: Cohort StudyDocument9 pagesRisk of Respiratory Morbidity in Term Infants Delivered by Elective Caesarean Section: Cohort StudyAlagendran Thanabalan PillayNo ratings yet
- Chorioamnionitis and Prognosis For Term Infants-13Document5 pagesChorioamnionitis and Prognosis For Term Infants-13ronny29No ratings yet
- Prediction of Preterm Delivery in Twins by Cervical Assessment at 23 WeeksDocument4 pagesPrediction of Preterm Delivery in Twins by Cervical Assessment at 23 WeeksBudi Darmawan DiswanNo ratings yet
- Twins PecepDocument8 pagesTwins Pecepjj_cani91No ratings yet
- Genitmed00026-0016Document4 pagesGenitmed00026-0016Momon ManiezNo ratings yet
- JurnalDocument9 pagesJurnaleeeeeeNo ratings yet
- Singleton Term Breech Deliveries in Nulliparous and Multiparous Women: A 5-Year Experience at The University of Miami/Jackson Memorial HospitalDocument6 pagesSingleton Term Breech Deliveries in Nulliparous and Multiparous Women: A 5-Year Experience at The University of Miami/Jackson Memorial HospitalSarah SilaenNo ratings yet
- 1471-0528 16519Document12 pages1471-0528 16519Leydi PaolaNo ratings yet
- A first trimester trisomy 13/trisomy 18 risk algorithm combining fetal nuchal translucency thickness, maternal serum free β-hCG and PAPP-ADocument3 pagesA first trimester trisomy 13/trisomy 18 risk algorithm combining fetal nuchal translucency thickness, maternal serum free β-hCG and PAPP-AManoj DekaNo ratings yet
- Cervical FunnelingDocument3 pagesCervical FunnelingRatnakar KamathNo ratings yet
- Cerclage Twins EJOGRB 2024Document6 pagesCerclage Twins EJOGRB 2024Willans Eduardo Rosha HumerezNo ratings yet
- Original ArticleDocument4 pagesOriginal ArticlefeyzarezarNo ratings yet
- Faktor Kejadian Preeklampsi Ringan Di Wilayah Kerja Puskesmas Rawat Inap Gedong Tataan Kabupaten PesawaranDocument11 pagesFaktor Kejadian Preeklampsi Ringan Di Wilayah Kerja Puskesmas Rawat Inap Gedong Tataan Kabupaten PesawaranBellachristy BellachristyNo ratings yet
- Grabovac 2017Document12 pagesGrabovac 2017Karindha Handayani HelisusantoNo ratings yet
- Twin Pregnancy - Labor and DeliveryDocument19 pagesTwin Pregnancy - Labor and Deliveryrugasa291100% (2)
- Risk Factors and Outcomes of Umbilical Cord Prolapse: Evaluation of 94 CasesDocument3 pagesRisk Factors and Outcomes of Umbilical Cord Prolapse: Evaluation of 94 CasesElva Diany SyamsudinNo ratings yet
- Bjo0117 0830 PDFDocument7 pagesBjo0117 0830 PDFkhairun nisaNo ratings yet
- Articles: BackgroundDocument13 pagesArticles: BackgroundHartanto LieNo ratings yet
- $116 SMFM AbstractsDocument1 page$116 SMFM AbstractsSheila Regina TizaNo ratings yet
- Hipertensi Pada Ibu Hamil Trimester 3Document8 pagesHipertensi Pada Ibu Hamil Trimester 3deskha putriNo ratings yet
- Frederiksen 2018Document7 pagesFrederiksen 2018WinniaTanelyNo ratings yet
- Changes in The Utilization of Prenatal Diagnosis.19Document6 pagesChanges in The Utilization of Prenatal Diagnosis.19Filipa DiasNo ratings yet
- Aust NZ J Obst Gynaeco - 2022 - Silveira - Placenta Accreta Spectrum We Can Do BetterDocument7 pagesAust NZ J Obst Gynaeco - 2022 - Silveira - Placenta Accreta Spectrum We Can Do BetterDrFeelgood WolfslandNo ratings yet
- First-Trimester Determination of Fetal Gender PDFDocument3 pagesFirst-Trimester Determination of Fetal Gender PDFkukadiyaNo ratings yet
- The Cesarean Section Rate in Cases With Premature Rupture of Membrane (Prom) at 36Th Week of Pregnancy or LaterDocument5 pagesThe Cesarean Section Rate in Cases With Premature Rupture of Membrane (Prom) at 36Th Week of Pregnancy or LaterBob IrsanNo ratings yet
- 3151 12154 1 PB PDFDocument5 pages3151 12154 1 PB PDFmohamad safiiNo ratings yet
- A Re-Look at The Duration of Human Pregnancy: Bhat R A, Kushtagi PDocument5 pagesA Re-Look at The Duration of Human Pregnancy: Bhat R A, Kushtagi PjackofmanytradesNo ratings yet
- Quadrivalent HPV Vaccination and The Risk of Adverse Pregnancy OutcomesDocument11 pagesQuadrivalent HPV Vaccination and The Risk of Adverse Pregnancy OutcomesRastia AlimmattabrinaNo ratings yet
- Fracture of The Clavicle in The Newborn Following Normal Labor and DeliveryDocument6 pagesFracture of The Clavicle in The Newborn Following Normal Labor and DeliveryAlberto OrtizNo ratings yet
- Association of Vaginal Infections in Preterm Labour: Srilakshmi Yarlagadda, Sajana G., Prasuna J. L. NarraDocument6 pagesAssociation of Vaginal Infections in Preterm Labour: Srilakshmi Yarlagadda, Sajana G., Prasuna J. L. NarraNurRahMatNo ratings yet
- Medip, IJRCOG-5630 O PDFDocument5 pagesMedip, IJRCOG-5630 O PDFSuraj NagarajNo ratings yet
- Poster Session II: ObjectiveDocument1 pagePoster Session II: ObjectivefujimeisterNo ratings yet
- Screening For Fetal Aneuploidies at 11 To 13 Weeks: ReviewDocument9 pagesScreening For Fetal Aneuploidies at 11 To 13 Weeks: Reviewarturm21No ratings yet
- Grob Man 2018Document11 pagesGrob Man 2018Ervan SuryaNo ratings yet
- Prediction and Prevention of Small For Gestational Age Neonates Evidence FromDocument8 pagesPrediction and Prevention of Small For Gestational Age Neonates Evidence FromOscar AncheitaNo ratings yet
- Evidence FGDocument14 pagesEvidence FGpeter_mrNo ratings yet
- Health of Children Born To Mothers Who Had Preeclampsia: A Population-Based Cohort StudyDocument10 pagesHealth of Children Born To Mothers Who Had Preeclampsia: A Population-Based Cohort StudyAdhitya Pratama SutisnaNo ratings yet
- Is Breech Presentation A Risk Factor For Cerebral Palsy? A Norwegian Birth Cohort StudyDocument6 pagesIs Breech Presentation A Risk Factor For Cerebral Palsy? A Norwegian Birth Cohort StudyPutriNo ratings yet
- Placental Abruption in Term and Preterm.8 PDFDocument8 pagesPlacental Abruption in Term and Preterm.8 PDFMuhammad Riza FahlawiNo ratings yet
- Relation Between Increased Fetal Nuchal.4Document5 pagesRelation Between Increased Fetal Nuchal.4dachimescuNo ratings yet
- Am J Perinatol. 2007 Jun24 (6) 373-6Document4 pagesAm J Perinatol. 2007 Jun24 (6) 373-6Ivan Osorio RuizNo ratings yet
- Medip, IJRCOG-12438 ODocument4 pagesMedip, IJRCOG-12438 On2763288No ratings yet
- Ijss Jan Oa25 - 2017Document4 pagesIjss Jan Oa25 - 2017Esther Ellise AbundoNo ratings yet
- Grobman Et Al. 2018Document12 pagesGrobman Et Al. 2018EmmanuelRajapandianNo ratings yet
- The Diagnostic Performance of The Ductus Venosus For The DetectionDocument17 pagesThe Diagnostic Performance of The Ductus Venosus For The DetectionEdwin BravoNo ratings yet
- Hematoma SubcorionicoDocument6 pagesHematoma SubcorionicoMagic_OverNo ratings yet
- The in Uence of Parity and Gravidity On ®RST Trimester Markers of Chromosomal AbnormalityDocument3 pagesThe in Uence of Parity and Gravidity On ®RST Trimester Markers of Chromosomal AbnormalityANJANEYULUNo ratings yet
- Roos 2010Document8 pagesRoos 2010msc plmNo ratings yet
- Del 153Document6 pagesDel 153Fan AccountNo ratings yet
- Jurnal KedokteranDocument6 pagesJurnal Kedokteranusk.ppdsobgynganjil2022No ratings yet
- Surrogacy LawsDocument122 pagesSurrogacy LawsMonica Saini100% (1)
- Evidence-Based Approach To Unexplained Infertility: A Systematic ReviewDocument10 pagesEvidence-Based Approach To Unexplained Infertility: A Systematic ReviewEni Maria SiscaNo ratings yet
- NEW PRICE LIST - BATAM September 2018Document4 pagesNEW PRICE LIST - BATAM September 2018YuliantiNo ratings yet
- Intrebari Capitolul 6 - ColorDocument8 pagesIntrebari Capitolul 6 - ColorMonica EnescuNo ratings yet
- Ivm Protocol Medicult 1Document2 pagesIvm Protocol Medicult 1nilesh suvagiyaNo ratings yet
- GNRH Agonist Trigger For The Induction of Oocyte Maturation in GNRH Antagonist IVF Cycles: A SWOT AnalysisDocument12 pagesGNRH Agonist Trigger For The Induction of Oocyte Maturation in GNRH Antagonist IVF Cycles: A SWOT Analysisgardener10No ratings yet
- 08.04.20-AF, Unit-12, Family Wefare Programme, - Methods of contraception-8.04.20-ANDocument65 pages08.04.20-AF, Unit-12, Family Wefare Programme, - Methods of contraception-8.04.20-ANElakkiyaanu64 Elakkiyaanu64No ratings yet
- ACOG Postpartum Discharge FormDocument2 pagesACOG Postpartum Discharge Formnandipati ramnadh100% (1)
- Yes No MaybeDocument6 pagesYes No MaybeBobbyVNo ratings yet
- Preventol InfoDocument2 pagesPreventol InfoInderpreetKaurMaanNo ratings yet
- 107 Family PlanningDocument69 pages107 Family PlanningRiegne Chiara Fay AcuzarNo ratings yet
- Human Reproduction WorksheetDocument3 pagesHuman Reproduction WorksheetDEEBAN0% (1)
- Post Term PregnancyDocument22 pagesPost Term PregnancyDarianne HernandezNo ratings yet
- Ra Hu !!9910339635 ! iRLs in DeLhi EsCoRt ! @GurGaOn CaLL Irls in GuRgaOnDocument13 pagesRa Hu !!9910339635 ! iRLs in DeLhi EsCoRt ! @GurGaOn CaLL Irls in GuRgaOnDikshaSethiNo ratings yet
- Female Reproductive System Anatomy and PhysiologyDocument5 pagesFemale Reproductive System Anatomy and PhysiologyGeevee Naganag VentulaNo ratings yet
- DLL - Science 5 - Q2 - W5Document9 pagesDLL - Science 5 - Q2 - W5karlo echave100% (1)
- S5LT IIe 5Document4 pagesS5LT IIe 5Junalyn Elmedorial EspiñaNo ratings yet
- Nursing Management During PregnancyDocument46 pagesNursing Management During PregnancyHmp KepmaNo ratings yet
- Right To Life Movement PowerpointDocument8 pagesRight To Life Movement Powerpointapi-452788589No ratings yet
- 6worksheet ReproductionDocument2 pages6worksheet ReproductionivyNo ratings yet
- Sex EdDocument8 pagesSex EdRaj Sharma100% (1)
- Blocked Fallopian TubesDocument6 pagesBlocked Fallopian TubesJuliet AmondiNo ratings yet
- Male Sterilization: VasectomyDocument1 pageMale Sterilization: VasectomyKarl Kiw-isNo ratings yet
- Academic Writing Answers 1Document31 pagesAcademic Writing Answers 1mihaela_calin_24100% (2)
- Faktor Yang Berhubungan Dengan Kesiapan Persalinan Ibu Primigravida Di Wilayah Kerja Puskesmas Batulappa Kabupaten PinrangDocument5 pagesFaktor Yang Berhubungan Dengan Kesiapan Persalinan Ibu Primigravida Di Wilayah Kerja Puskesmas Batulappa Kabupaten PinrangPapy AleshaNo ratings yet
- 12 Population PDFDocument12 pages12 Population PDFMahroof YounasNo ratings yet
- Assisted Reproductive TechnologyDocument8 pagesAssisted Reproductive Technologymaria kousalya0% (1)
- Ichroma II Test Panels 210331 104829Document2 pagesIchroma II Test Panels 210331 104829Sinergy DiagnosticNo ratings yet
- Topic: Mechanisms of Fertilization:: Presented byDocument16 pagesTopic: Mechanisms of Fertilization:: Presented byMajani RajbonshiNo ratings yet
- Family Planning and ContraceptionDocument11 pagesFamily Planning and ContraceptionJose Emmanuel Ribaya RuivivarNo ratings yet