Professional Documents
Culture Documents
NCPs For Infant
Uploaded by
Ray Carlo Ybiosa AntonioOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NCPs For Infant
Uploaded by
Ray Carlo Ybiosa AntonioCopyright:
Available Formats
SILLIMAN UNIVERSITY
DUMAGUETE CITY
NURSING CARE PLAN
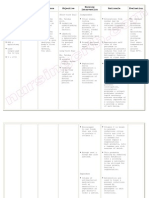
CUES/EVIDENCES NURSING DIAGNOSIS OBJECTIVES INTERVENTIONS RATIONALE EVALUATION
Subjective:
• Mother verbalized Risk for infection r/t Within my care, the infant • Monitor vital signs • To keep track of At the end of our care all
“wala pa man na presence of newly clamped will remain free of baseline data objectives were met as
gilimpyohan iya cord stump infection as evidenced by: • Observe Principles • To help prevent evidenced by:
pusod” of asepsis spread of
•Cord Stump is free pathogenic • Mother verbalized
Objective: from bleeding substances “wala naman
• Date and time of •Umbilical cord is • Inspect the infant’s • If the clamp gadugo iya pusod”
delivery: Sept 14, healing and free of cord to be certain it loosens before • Absent of blood on
2006, 5:35 pm infection is clamped securely thrombosis, binder
• Delivered via •Area around the hemorrhage will • Umbilical stump
NSVD cord stump is dry result appeared dry and is
• Apgar’s score is 9 and is without • Assess cord for • The cut surface of healing well
at the 1st minute purulent discharges number of vessels the umbilical cord • Absence of foul
and 9, after 4 •Absence of foul without touching presents a site for odor
minutes odor the cut surface. proliferation of • Gauze remained
• Assessed cord •Gauze remains dry microorganisms dry and free from
stump and noticed •Vital signs remain • Perform Cord Care, • To promote healing secretions
blood on binder within normal range fold diapers down of the cord stump • Vital signs within
present T = 36.5 – 37.2 °C to expose the cord and prevent normal range
• Cord care hasn’t P = 120 – 140 bpm infection, Keeping T = 37 °C
been performed R = 30 – 60 cpm the cord exposed P = 125 bpm
• No foul odor noted facilitates drying R = 35 cpm
• Gauze soaked with and inhibits
secretions bacterial growth
• Skin is pinkish in • Observe neonate • Early detection of
color for signs and signs of infection
• Vital signs symptoms of can provide prompt
T = 37 °C infection. Assess intervention
P = 120 bpm, cord for erythema,
R = 40 cpm, bleeding, foul odor
regular, rapid and purulent
respirations discharge
• Perform Infant • To cleanse the
Sponge Bath body of
microorganisms
this would provide
comfort to the baby
and prevent
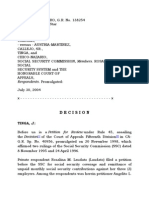
SILLIMAN UNIVERSITY
DUMAGUETE CITY
NURSING CARE PLAN
CUES/EVIDENCES OBJECTIVES INTERVENTIONS RATIONALE EVALUATION
CUES/EVIDENCES NURSING DIAGNOSIS
NURSING DX OBJECTIVES
SILLIMANINTERVENTIONS
UNIVERSITY RATIONALE EVALUATION
Objective: DUMAGUETE CITY
Subjective:
• Mother
Date and Altered
Risk forNutrition:
ineffective
Less Within my care, NURSING
the baby
infant •CARE PLAN
Monitor Vital signs • To keep track of At the end of my
our care, a;;
all
verbalized
time of delivery: thanthermoregulation
body requirements will maintain
increase its
a stable
bodilybody baseline data objectives were met as
“Maglisod
Sept 14, 2006, ko og5:35 Related
related to mother’s
immature requirementsasasevidenced
temperature evidenced • Mummifying
Educate mother theon evidenced by:
patutoy niya,
pm inability
thermoregulation
to producecenter
milk by: the importance
baby properly of • To keep the
Mother’s gained
baby
•gamay ra gyud
Delivered and sudden changes in breastfeeding knowledge
warm and provide
on • Vital signs
Mother verbalized
within
sukad
via NSVD gabi-i” environmental • •Vital
MotherSigns
expresses
within breastfeeding will
comfort “naa naman
normal rangegatas
• “Murag
Apgar’s temperature. normal
understanding
range of • Encourage the • motivate
To form aher to
good mugawas
T = 36.5 °Cnya
iyang is
score iluwa
9 at akong
the 1st Tbreastfeeding
= 36.5 – 37.2 °C mother to be with continue
bonding makatotoy
P = 120 bpm na sya
totoy” and 9, after
minute Ptechniques
= 120 – 140 and
bpm • the
teach
child
the as
mother
often in
as breastfeedingwhile
relationship og=tarong
R 45 cpmog
4• minutes “Maluoy Rpractices
= 30 – 60 cpm proper
possible • To ensure
keeping theproper
baby nakalibang na pod
•
man gud ko sa ako
Mother and • Newborn will be breastfeeding nutrition of neonate
warm • sya”
Newborn appeared
bata…”
infant are staying •Mother
calm andexhibits
rested • Make
techniques
sure • Bathing quickly in • Mother
relax andappeared
rested
in the alley not • continued
Baby being • environment
Monitor neonate is a warm • relax andisatnegative
Neonate ease
Objective:
therapeutic for the breastfeeding
properly draped for signs
warm enough
of for • To establish need
environment avoids while breastfeeding
for chilling or
• careDate of andantime
infantof during when dehydration
bathing. Wash andand for immediate
heat loss from • Infant displayed
excessive sweating
•delivery: Sept 14,
Sudden •Assume
performing dry head
mucous firs, then medical
evaporation and • good
Newborn is reflex
sucking
2006,
shift from pm
5:35 responsibility
procedures (ex.
for membranes
expose and wash intervention
convection while breastfeeding
properly draped
• intrauterine
Delivered via effective
infant sponge bath) one area of the • Infant doing
when voided twice
NSVD
environment to the • breastfeeding
Newborn is • body at a time
Encourage and
mother and defecated with
procedures
• environment
Apgar’s score is 9 properly clothed dry thoroughly
to breastfeed baby • Stimulation for • soft greenish
Newborn is stool
outside
at the 1stofminutethe •Neonate
and kept will
warm void
and before
every 2° moving to production of milk • Mucous clothed
properly
mother’s
and 9, after womb4 ordry
defecate within another area membranes
and kept warm and
•minutesEnvironmen normal output appeared wet
dry
t• is hot and
Verbalnot well • Avoid unnecessary • Exposure of body
ventilated
reports of exposure of body parts may cause the
•unsatisfactory
Presence of parts when baby to chill
breast – feeding
sweating in the performing
knowledge
head procedures
• Mother
shows difficulty
wrapping the infantin • Avoid placing • Placing the infant
latching-on
in thick blanketsthe infant on cool on a cool surface or
baby if it is too hot
even surfaces or using using a cool
• Vital• signs Neonate cold instruments in instrument
shows
T = 37 inability
°C to assessment (ex. increases heat loss
nurse
P = 120well,
bpm, doespulse stethoscope) by conduction
notirregular
is demonstrate
effective
R = 40 cpm,suck and • Place infant away • Heat may be lost
swallowrapid
regular, reflex from windows, directly from the
avoid drafts infant’s body to
You might also like
- Nursing Care Plan Risk For Uterine InfectionDocument4 pagesNursing Care Plan Risk For Uterine Infectionderic97% (30)
- Nursing Care Plan of The NewbornDocument5 pagesNursing Care Plan of The Newbornappleliciouz0860% (10)
- NCP Preterm NeonateDocument3 pagesNCP Preterm NeonateLilia Priscilla Tuibuen Aureus100% (2)
- NB Nursing DiagnosisDocument2 pagesNB Nursing Diagnosisnursingmvd92% (13)
- NCP NewbornDocument8 pagesNCP Newbornsupacalifragirlistic67% (9)
- Newborn Nursing CareplanDocument7 pagesNewborn Nursing CareplanSamantha MillerNo ratings yet
- NSVD Patient Sleep IssuesDocument3 pagesNSVD Patient Sleep IssuesAlma Gobaleza100% (1)
- Biographical Data - InfantDocument3 pagesBiographical Data - Infantmitsuki_sylphNo ratings yet
- NCP NewbornDocument2 pagesNCP Newbornsonylynne94% (17)
- NCP InfectionDocument2 pagesNCP InfectionAngie Dino100% (2)
- Preterm Infant Nursing Care PlanDocument19 pagesPreterm Infant Nursing Care Planysamariano100% (1)
- Care Plan Redo For NeonateDocument2 pagesCare Plan Redo For NeonateIris Lopez100% (6)
- Neonatal Jaundice and Ineffective Breundiceeding Nursing Care PlanDocument3 pagesNeonatal Jaundice and Ineffective Breundiceeding Nursing Care Planpapadaad100% (1)
- Nursing Care Plan. LyksDocument3 pagesNursing Care Plan. LyksKiyla92No ratings yet
- Neonatal Sepsis NCPDocument9 pagesNeonatal Sepsis NCPHollan Galicia100% (1)
- Maintaining Normal Body Temperature in NewbornsDocument2 pagesMaintaining Normal Body Temperature in NewbornsErica Veluz LuyunNo ratings yet
- Newborn Careplan 9-15-2011Document17 pagesNewborn Careplan 9-15-2011Brittany Wood100% (1)
- NCP Ineffective ThermoregulationDocument4 pagesNCP Ineffective ThermoregulationCharmae Navea100% (1)
- NCPDocument3 pagesNCPJefferson ManasanNo ratings yet
- Care Plan PostpartumDocument2 pagesCare Plan Postpartumteokie082483% (6)
- Risk For Hypothermia of New BornDocument2 pagesRisk For Hypothermia of New BornjenspryNo ratings yet
- HyperthermiaDocument2 pagesHyperthermiapamgee100% (11)
- Neonatal Sepsis (NCP)Document10 pagesNeonatal Sepsis (NCP)Lucero Hyacinth100% (1)
- Proper Cord CareDocument1 pageProper Cord CareMelanie Bagasol SisonNo ratings yet
- Head-To-Toe AssessmentDocument10 pagesHead-To-Toe AssessmentJenny Rose Colico RNNo ratings yet
- Patty NCP HyperthermiaDocument4 pagesPatty NCP HyperthermiaPatricia Jean FaeldoneaNo ratings yet
- NCPDocument4 pagesNCPMarielle SorianoNo ratings yet
- Nursing Care Plan Ineffective Infant Feeding PatternDocument3 pagesNursing Care Plan Ineffective Infant Feeding PatternMarife Lipana Reyes100% (1)
- NCP SepsisDocument6 pagesNCP SepsisgopscharanNo ratings yet
- Nursing Care Plan Ineffective ThermoregulationDocument2 pagesNursing Care Plan Ineffective ThermoregulationLoraNo ratings yet
- NEONATAL SEPSIS ASSESSMENT AND MANAGEMENTDocument12 pagesNEONATAL SEPSIS ASSESSMENT AND MANAGEMENTPamela laquindanumNo ratings yet
- NCP-Effective Breast FeedingDocument3 pagesNCP-Effective Breast Feedingjava_biscocho12290% (1)
- Nursing Care PlanDocument7 pagesNursing Care Planrockerespi1283No ratings yet
- NCP Less Than Body Req.Document2 pagesNCP Less Than Body Req.Mary Ann Contreras100% (1)
- SDL1 NCP Case2Document3 pagesSDL1 NCP Case2Alec AnonNo ratings yet
- Definition of The Case + Hyperthermia NCPDocument2 pagesDefinition of The Case + Hyperthermia NCPCindy MariscotesNo ratings yet
- NCP - Hyperbilirubinemia - Staff NursingDocument3 pagesNCP - Hyperbilirubinemia - Staff NursingnurseM67% (3)
- Nursing Care PlanDocument6 pagesNursing Care PlanAnthea ValinoNo ratings yet
- Newborn Nursing Care Plan With ReferncesDocument6 pagesNewborn Nursing Care Plan With Referncesneuronurse92% (63)
- Student Nurses' Community: NURSING CARE PLAN Neonatal SepsisDocument2 pagesStudent Nurses' Community: NURSING CARE PLAN Neonatal SepsisChristian Remetio100% (1)
- Nutrition Knowledge GainDocument4 pagesNutrition Knowledge GainTrisha CayabyabNo ratings yet
- Dysfunctional Uterine Bleeding (DUB)Document1 pageDysfunctional Uterine Bleeding (DUB)Bheru LalNo ratings yet
- Nursing Diagnosis Rationale Goals/ Objectives Nursing Interventions Rationale EvaluationDocument20 pagesNursing Diagnosis Rationale Goals/ Objectives Nursing Interventions Rationale EvaluationElaine Grace Timbol-Babasa100% (1)
- Nursing Care Plan JaundiceDocument2 pagesNursing Care Plan Jaundicepapadaad86% (35)
- Family Nursing Care PlansDocument4 pagesFamily Nursing Care PlanssenyorakathNo ratings yet
- Discharge PlanningDocument3 pagesDischarge PlanningAlex Marie100% (2)
- Nursing ResponsibilityDocument9 pagesNursing Responsibilityايام اول الشحيNo ratings yet
- Assessment Nursing Diagnosis Outcome Nursing Interventions Evaluation Standard Criteria Subjective: Short Term GoalDocument6 pagesAssessment Nursing Diagnosis Outcome Nursing Interventions Evaluation Standard Criteria Subjective: Short Term GoalmitchNo ratings yet
- NCP For Delivery RoomDocument4 pagesNCP For Delivery RoomGiselle EstoquiaNo ratings yet
- Nursing Care for 2nd Degree Perineal LacerationDocument2 pagesNursing Care for 2nd Degree Perineal LacerationDickson,Emilia Jade100% (1)
- Peach and Green Organic Shapes Meditation Workshop Webinar Keynote PresentationDocument7 pagesPeach and Green Organic Shapes Meditation Workshop Webinar Keynote PresentationNicole Ivy GorimoNo ratings yet
- NCP1 IntrapartalDocument1 pageNCP1 IntrapartalYvone Zoe OrdistaNo ratings yet
- Understanding Normal Spontaneous Vaginal Delivery PathophysiologyDocument7 pagesUnderstanding Normal Spontaneous Vaginal Delivery PathophysiologyMa Christina RabayaNo ratings yet
- Case AnalysisDocument6 pagesCase AnalysisAngela CancinoNo ratings yet
- Communicable Disease Sir FedsDocument19 pagesCommunicable Disease Sir FedsHarold LinNo ratings yet
- Lesson: Plan ON Topic - Umbilical Cord CareDocument6 pagesLesson: Plan ON Topic - Umbilical Cord CareBhawna PandhuNo ratings yet
- Lesson Plan On Umbilical Cord CareDocument9 pagesLesson Plan On Umbilical Cord CareJasmine PraveenNo ratings yet
- 2.01 Gynecology Infections of The Genital TractDocument16 pages2.01 Gynecology Infections of The Genital TractAsela MirandaNo ratings yet
- 2A-Sarigumba - 10 MEDICALLY IMPORTANT BACTERIA PDFDocument18 pages2A-Sarigumba - 10 MEDICALLY IMPORTANT BACTERIA PDFSean SarigumbaNo ratings yet
- Week 7 Ha - MachDocument9 pagesWeek 7 Ha - MachAC MartinNo ratings yet
- Affidavit of CohabitationDocument1 pageAffidavit of CohabitationRay Carlo Ybiosa Antonio74% (23)
- Letter To MayorDocument3 pagesLetter To MayorRay Carlo Ybiosa AntonioNo ratings yet
- SPADocument1 pageSPARay Carlo Ybiosa AntonioNo ratings yet
- SFC ProvCon 2017Document2 pagesSFC ProvCon 2017Ray Carlo Ybiosa AntonioNo ratings yet
- Liga ng mga Barangay Meeting Minutes San JoseDocument2 pagesLiga ng mga Barangay Meeting Minutes San JoseRay Carlo Ybiosa AntonioNo ratings yet
- AGW 2016 Program ScriptDocument8 pagesAGW 2016 Program ScriptRay Carlo Ybiosa AntonioNo ratings yet
- Barangay Certification Ybiosa, JessaDocument1 pageBarangay Certification Ybiosa, JessaRay Carlo Ybiosa Antonio100% (1)
- Register now for the 2016 SFC Negros Oriental Provincial ConferenceDocument1 pageRegister now for the 2016 SFC Negros Oriental Provincial ConferenceRay Carlo Ybiosa AntonioNo ratings yet
- PROVCON 2017 General Program FlowDocument1 pagePROVCON 2017 General Program FlowRay Carlo Ybiosa AntonioNo ratings yet
- 1 People Vs de La CruzDocument9 pages1 People Vs de La CruzRay Carlo Ybiosa AntonioNo ratings yet
- Corpo NotesDocument4 pagesCorpo NotesRay Carlo Ybiosa AntonioNo ratings yet
- Hotel List 2Document20 pagesHotel List 2Ray Carlo Ybiosa AntonioNo ratings yet
- 77 Producer's Bank Vs NLRCDocument12 pages77 Producer's Bank Vs NLRCRay Carlo Ybiosa AntonioNo ratings yet
- 70 Apex Mining Corp Vs NLRCDocument6 pages70 Apex Mining Corp Vs NLRCRay Carlo Ybiosa AntonioNo ratings yet
- 71 Kamaya Point Hotel Vs NLRCDocument3 pages71 Kamaya Point Hotel Vs NLRCRay Carlo Ybiosa AntonioNo ratings yet
- 75 Honda Phils Vs Samahan NG Malalayang Mangagawa Sa HondaDocument7 pages75 Honda Phils Vs Samahan NG Malalayang Mangagawa Sa HondaRay Carlo Ybiosa AntonioNo ratings yet
- Agabon CaseDocument14 pagesAgabon CasealiahNo ratings yet
- 74 Manila Electric Co Vs Secretary of LaborDocument27 pages74 Manila Electric Co Vs Secretary of LaborRay Carlo Ybiosa AntonioNo ratings yet
- Davao Fruits Corp Vs ALUDocument4 pagesDavao Fruits Corp Vs ALUtengloyNo ratings yet
- 73 Manila Banking Corp Vs NLRCDocument14 pages73 Manila Banking Corp Vs NLRCRay Carlo Ybiosa AntonioNo ratings yet
- 76 Philippine Veterans Bank Vs NLRCDocument7 pages76 Philippine Veterans Bank Vs NLRCRay Carlo Ybiosa AntonioNo ratings yet
- D Accommodation LetterDocument1 pageD Accommodation LetterRay Carlo Ybiosa AntonioNo ratings yet
- A 1 Samples Marketing LetterDocument1 pageA 1 Samples Marketing LetterRay Carlo Ybiosa AntonioNo ratings yet
- Experiencing Christ at CFC-Singles ConferenceDocument1 pageExperiencing Christ at CFC-Singles ConferenceRay Carlo Ybiosa AntonioNo ratings yet
- Lazaro Vs SSSDocument8 pagesLazaro Vs SSSRay Carlo Ybiosa AntonioNo ratings yet
- Dispute over talent contract between broadcaster and TV hostDocument17 pagesDispute over talent contract between broadcaster and TV hostRay Carlo Ybiosa AntonioNo ratings yet
- Ramos Vs CADocument13 pagesRamos Vs CARay Carlo Ybiosa AntonioNo ratings yet
- Bezold AbscessDocument5 pagesBezold AbscessCarimaGhalieNo ratings yet
- Sir James Young Simpson CollectionDocument77 pagesSir James Young Simpson CollectionSuresh KumarNo ratings yet
- Mual Dan Muntah Pada KehamilanDocument16 pagesMual Dan Muntah Pada KehamilanJuwita Valen RamadhanniaNo ratings yet
- Married Women of Reproductive AgeDocument26 pagesMarried Women of Reproductive Agelibagon rhuNo ratings yet
- Arnica The Miracle RemedyDocument10 pagesArnica The Miracle RemedyAnand GuptaNo ratings yet
- PICU Handbook - University of Iowa Stead Family Children's HospitalDocument10 pagesPICU Handbook - University of Iowa Stead Family Children's HospitalAhmed MohammedNo ratings yet
- Maternity Record Keeping 4.0Document24 pagesMaternity Record Keeping 4.0ItaNo ratings yet
- Local Anesthetic Nerve Block ReviewDocument8 pagesLocal Anesthetic Nerve Block Reviewvelo100% (1)
- Graduation ExercisesDocument3 pagesGraduation ExercisesRenesiy NovillaNo ratings yet
- Diarrhea - Toddlers PDFDocument1 pageDiarrhea - Toddlers PDFNida AwaisNo ratings yet
- FHSIS Report SummaryDocument30 pagesFHSIS Report SummaryReuben Jr UmallaNo ratings yet
- UntitledDocument205 pagesUntitledAdil PatelNo ratings yet
- Distal Radius FracturesDocument68 pagesDistal Radius Fracturescalvin_c_wangNo ratings yet
- M - C - Q. R. & Answer & Answer & ANSWER SHEETDocument70 pagesM - C - Q. R. & Answer & Answer & ANSWER SHEETnmyhrtNo ratings yet
- Caffeine Breast Pain: Revisiting The ConnectionDocument9 pagesCaffeine Breast Pain: Revisiting The ConnectionGrace PelicioniNo ratings yet
- Health Report 1997-99-Solomon IslandsDocument122 pagesHealth Report 1997-99-Solomon IslandsMalefoasi100% (1)
- The Effect of Aloe Vera Compress On The Plebitis DDocument4 pagesThe Effect of Aloe Vera Compress On The Plebitis DAyu FahrinaNo ratings yet
- 4 History of MassageDocument3 pages4 History of MassageJoanna AaronNo ratings yet
- Primary Amenorrhea NotesDocument2 pagesPrimary Amenorrhea NotesRomulo Vincent PerezNo ratings yet
- International Clinical Fellowship Programme Brochure - September - 2023Document29 pagesInternational Clinical Fellowship Programme Brochure - September - 2023Anam QadeerNo ratings yet
- MENSTRUAL DISORDERS AND TREATMENTDocument8 pagesMENSTRUAL DISORDERS AND TREATMENTpranaji100% (7)
- NCLEX Pregnancy NotesDocument3 pagesNCLEX Pregnancy NotesrustiejadeNo ratings yet
- Dr. Pedro Dennis Cereno, and Dr. Santos Zafe, Petitioners, vs. Court of Appeals, Spouses Diogenes S. Olavere and Fe R. Serrano, RespondentsDocument11 pagesDr. Pedro Dennis Cereno, and Dr. Santos Zafe, Petitioners, vs. Court of Appeals, Spouses Diogenes S. Olavere and Fe R. Serrano, Respondentssophia100% (1)
- pv0615 CelluliteDocument12 pagespv0615 Celluliteapi-287373625No ratings yet
- Prenatal Development (Child Psychology)Document37 pagesPrenatal Development (Child Psychology)Yel BaldemorNo ratings yet
- 1-Mini-implant-miniscrews in Orthodontics-oussama Sandid- Mohamad Aboualnaser-Awatef Shaar-maria Doughan-miniscrews Mini-implant en Orthodontie- Beirut- Lebanon- France- Usa -Dentist - Orthodontist-dentistry school beirut arab university zaarourieh zaarourieDocument129 pages1-Mini-implant-miniscrews in Orthodontics-oussama Sandid- Mohamad Aboualnaser-Awatef Shaar-maria Doughan-miniscrews Mini-implant en Orthodontie- Beirut- Lebanon- France- Usa -Dentist - Orthodontist-dentistry school beirut arab university zaarourieh zaarourieAnonymous oD9H6T8p100% (2)
- Case Study Neonatal SepsisDocument22 pagesCase Study Neonatal Sepsisaishah shamsudinNo ratings yet
- Breastfeeding BibliographyDocument6 pagesBreastfeeding BibliographyPiyush DuttaNo ratings yet
- Accreditation Form for Postgraduate Training in Oral & Maxillofacial SurgeryDocument17 pagesAccreditation Form for Postgraduate Training in Oral & Maxillofacial SurgerywjeelaniNo ratings yet
- PRC OR Circulating Scrub Major FormDocument2 pagesPRC OR Circulating Scrub Major FormLIEZEL GONo ratings yet