Professional Documents
Culture Documents
Thickness Obtained by Software Image Normative Data of Outer Photoreceptor Layer
Uploaded by
AzuleslindoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Thickness Obtained by Software Image Normative Data of Outer Photoreceptor Layer
Uploaded by
AzuleslindoCopyright:
Available Formats
Downloaded from bjo.bmj.com on October 20, 2010 - Published by group.bmj.
com
Normative data of outer photoreceptor layer thickness obtained by software image enhancing based on Stratus optical coherence tomography images
U C Christensen, K Kroyer, J Thomadsen, et al. Br J Ophthalmol 2008 92: 800-805
doi: 10.1136/bjo.2007.130500
Updated information and services can be found at:
http://bjo.bmj.com/content/92/6/800.full.html
These include:
References
This article cites 19 articles, 5 of which can be accessed free at:
http://bjo.bmj.com/content/92/6/800.full.html#ref-list-1
Article cited in:
http://bjo.bmj.com/content/92/6/800.full.html#related-urls
Email alerting service
Receive free email alerts when new articles cite this article. Sign up in the box at the top right corner of the online article.
Topic collections
Articles on similar topics can be found in the following collections Retina (1082 articles)
Notes
To request permissions go to:
http://group.bmj.com/group/rights-licensing/permissions
To order reprints go to:
http://journals.bmj.com/cgi/reprintform
To subscribe to BMJ go to:
http://journals.bmj.com/cgi/ep
Downloaded from bjo.bmj.com on October 20, 2010 - Published by group.bmj.com
Clinical science
Normative data of outer photoreceptor layer thickness obtained by software image enhancing based on Stratus optical coherence tomography images
U C Christensen,1 K Kroyer,1 J Thomadsen,2 T M Jorgensen,2 M la Cour,1 B Sander1
1
Department of Ophthalmology, Glostrup Hospital, University of Copenhagen, Denmark; 2 Department of Optics and Plasma Research, Ris National Laboratory, Roskilde, Denmark Correspondence to: Dr U C Christensen, Department of Ophthalmology, Glostrup Hospital, Nordre Ringvej 57, DK-2600 Glostrup, Denmark; ulrikchristensen@dadlnet.dk Accepted 24 January 2008
ABSTRACT Aim: To present normative data of outer photoreceptor layer thickness obtained by a new semiautomatic image analysis algorithm operating on contrast-enhanced optical coherence tomography (OCT) images. Methods: Eight Stratus OCT3 scans from identical retinal locations from 25 normal eyes were registered and combined to form a contrast-enhanced average image. Utilising the vertical intensity gradients of the enhanced OCT images to demarcate retinal layers, thickness measurements of the outer photoreceptor- and retinal pigment epithelium layer (RPE-OScomplex) were obtained. Additionally backscattered light within the outer nuclear layer (ONL) in the fovea was registered and compared with backscattered light within the ONL in the peripheral part of the macula (Iratio-ONL). Results: The mean RPE-OScomplex thickness in the foveal centre was 77.2 mm (SD = 3.95). The RPE-OScomplex thickness in the superior macula 0.53 mm of the centre was significantly increased as compared with the corresponding inferior retina. In healthy subjects, the IratioONL was 1.06. Conclusions: Contrast-enhanced OCT images enable quantification of outer photoreceptor layer thickness, and normative values may help understanding better the relationship between functional outcome and photoreceptor morphology in retinal diseases.
averaging of a series of repetitive B-scans from identical fundus locations.4 5 By using this software to contrast-enhance OCT images, it is possible to improve the visualisation of smaller intraretinal structures, such as the reflection arising from the photoreceptor inner- and outer segment junction, as compared with standard OCT imaging.4 5 The primary aim of this study is to present normative data of outer photoreceptor layer thickness, obtained by a newly developed semiautomatic quantitative image analysis algorithm operating on contrast-enhanced OCT images. Thus, image data are obtained by the Stratus OCT system which is available in most ophthalmological departments. Besides providing thickness measurements of the photoreceptor layer, the new image-analysis algorithm also provides a measure of the backscattered light arsing from the outer nuclear layer in the foveal centre. This measurement may be relevant in the clinical evaluation of visual function in retinal diseases with induced gliosis. The alignment- and measuring software used in this study is available as shareware upon request to the corresponding author.
METHODS Participants
This methodological study included 25 normal eyes. All subjects had a negative history of previous eye disease and were examined clinically with indirect ophthalmoscopy and documented by fundus images before entering the study. Visual acuity testing was performed using Early Treatment of Diabetic Retinopathy Study (ETDRS) charts with a standard protocol at a distance of 4 m. The ETDRS chart is a logMAR chart where 8488 ETDRS letters correspond to a logMAR value of 0.0 and a Snellen ratio of 20/20.6
Optical coherence tomography (OCT) is currently the gold-standard imaging technique for diagnosing and evaluation of retinal diseases. Until recently, it has not been possible to visualise the subtle intraretinal morphological changes responsible for poor functional results in unfortunate cases, that is after surgery for macula-off retinal detachments or macular hole. Using the widely distributed time-domain Stratus OCT system, it is possible in a non-invasive manner to produce crosssectional images of the retina with 610 mm axialand 15 mm transverse resolutions. Stratus OCT thus enables visualisation of most major intraretinal layers.1 With the introduction of ultrahighresolution OCT scanners (UHR-OCT), which uses a light source with a broader bandwidth than conventional OCT, an axial image resolution of ,3 mm can be obtained.2 Thus, these scanners improve the visualisation of especially outer retinal features to a level where quantitative analyses of the photoreceptor layer are possible.3 Previous studies from our group have shown that improved OCT imaging can be achieved by alignment and
800
OCT imaging
All healthy subjects were examined using the OCT3 instrument (Stratus model 3000; Carl Zeiss Meditec, Humphrey Division, Dublin, CA). The subjects underwent scanning after pupil dilation fixating on the internal fixation light during scanning. Using the Line scan acquisition protocol, 20 vertically directed (90u) B-scans from the same location were collected. Each OCT scan was 1024 pixels (2 mm) in depth and 512 pixels (6 mm) in length.
Br J Ophthalmol 2008;92:800805. doi:10.1136/bjo.2007.130500
Downloaded from bjo.bmj.com on October 20, 2010 - Published by group.bmj.com
Clinical science
As previously described in detail, it is possible to reduce speckle noise in OCT images by alignment and averaging of multiple OCT scans from identical retinal locations.5 7 Using this method of enhanced OCT, it is possible to improve the signal-to-noise ratio of the resulting average image by the square root of the number of images used.5 7 In this way, image quality can be increased to the level where the outer retinal layers are clearly discernible (fig 1).4 Because recorded speckle patterns will vary only in cases when the imaging geometry or setup is slightly modified, small movements of the head and saccadic eye movements leading to small axial movements of the retina relative to the image geometry are the basis for suppression of scatter. The selection of images used for software enhancing was based on a visual inspection of qualitatively identicallooking raw scans with a good demarcation of the vitreoretinaland chorioretinal interface and absence of artefacts due to eye movements and pupillary shadowing. Out of the 20 obtained raw scans, eight scans were selected manually for software enhancing.
The central thickness measurement in these cases reflects the thickness of the remaining RPE-OScomplex peripheral to the defect. In cases with larger (.100 mm) central IS/OS defects the algorithm measures the thickness of the remaining central RPEOScomplex layer.
Retinal thickness
The retinal thickness is defined like in standard Stratus OCT software, as the distance from the vitreoretinal interface to the top of the inner hyperreflective IS/OS layer.
Ratio of intensity of backscattered light from the outer nuclear layer (Iratio-ONL)
The ratio of light intensity of the outer nuclear layer (IratioONL) is defined as the pixel light intensity in the central part of retina at the location of the Muller cell cone as compared with a reference pixel light intensity from the ONL in the peripheral part of the macula. This ratio may be of clinical relevance when studying retinal degenerative diseases, where you might find increased backscattered light, indicating high levels of glia tissue. The ratio is calculated based on two 15615 pixel boxes; the first automatically placed by the algorithm 10 pixels above the hyperreflective external limiting membrane in the centre of the scan; the second box placed within the ONL at a location 1500 mm superiorly of the centre. However, the observer is able of modifying the box positions according to the clinical situation.
Quantitative analyses
Windows-based image-processing software was developed in C++ Builder to operate on the contrast-enhanced images in order to trace retinal layers and to quantify descriptive distance measures.8 A shortest cost-path algorithm implemented using so-called dynamic programming was used to extract smooth contours of the desired retinal layers. Specifically, the software provides measurements of the retinal pigment epithelium- and photoreceptor outer segment complex thickness (I), retinal thickness (II) and the intensity of the backscattered light from the outer nuclear layer in the central part of the retina (III) (fig 2).
RESULTS
Normative data were obtained from 25 eyes of 17 subjects, nine women and eight men. The mean age of the normal volunteers was 56.8 years (4568 years). The mean visual acuity was 86 ETDRS letters (7991 letters) corresponding to a Snellen ratio of 20/20. The mean spherical refraction was plano (23.75 sph. to +2.25 sph.). In healthy subjects, the mean thickness of the RPE-OScomplex in the foveal centre was 77.2 mm (SD 3.95). The RPE-OScomplex thickness in corresponding locations 1 mm inferior and 1 mm superior of the centre was 63.76 mm and 67.84 mm, respectively (p,0.001). The RPE-OScomplex thickness in corresponding locations 2 mm inferior and 2 mm superior of the centre was 62.16 mm and 65.36 mm respectively (p = 0.002). Accordingly, the RPE-OScomplex thickness in the superior macula from 0.5 mm to 3 mm of the centre was significantly increased as compared with the corresponding inferior retina (Mann
Thickness of the RPE-OScomplex
The three hyper-reflective layers seen in the outer part of OCT scans of the human retina are thought to arise from the retinal pigment epithelium (RPE), the RPE and photoreceptor outer segment junction (RPE/OS), and the junction between the photoreceptor inner- and outer segments (IS/OS).9 The hyporeflective band between the IS/OS- and RPE/OS layers corresponds to the photoreceptor outer segments (OS) which are longer and thus easier to visualise in the fovea (fig 1). We define the RPE-OScomplex thickness as the distance from the IS/OS line to the outer border of the RPE. In pathological cases with small breaks (,100 mm) in the IS/OS line, the algorithm will ignore the central break by generating a straight line across the defect. Figure 1 Contrast-enhanced optical coherence tomography image of a normal macula. All retinal layers are distinguishable. Enhanced optical coherence tomography imaging especially improves visualisation of the outer retinal structures. GCL, ganglion cell layer; ELM, external limiting membrane; INL, inner nuclear layer; IPL, inner plexiform layer; IS/ OS, photoreceptor inner and outer segment junction; NFL, nerve fibre layer; ONL, outer nuclear layer; OPL, outer plexiform layer; OS, photoreceptor outer segments; RPE, retinal pigment epithelium; RPE/OS, retinal pigment epithelium and photoreceptor outer segment junction. Patient consent has been obtained for publication of this figure.
Br J Ophthalmol 2008;92:800805. doi:10.1136/bjo.2007.130500
801
Downloaded from bjo.bmj.com on October 20, 2010 - Published by group.bmj.com
Clinical science
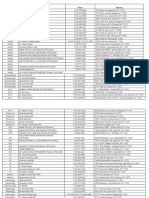
Figure 2 (Left) Vertical intensity profile from the central a-scan (no. 256) of a normal macula. The algorithm uses the vertical intensity profile of the contrastenhanced optical coherence tomography image for finding the shortest path between two sets of pixels in the image. (Right) Contrast-enhanced optical coherence tomography image of a normal macula with the lines of the measuring software superimposed. The outer photoreceptor- and retinal pigment epithelium layer (RPE-OScomplex) thickness is measured between the two lines in the outer retina. The retinal thickness (RT) at any point along the 6 mm long scan is calculated between the lines at the vitreoretinal interface and the photoreceptor inner and outer segment junction. The mean pixel light intensity of the outer nuclear layer at the apex of the Muller cell cone in the foveal centre (central box) is compared with reference pixel intensity from the peripheral part of the outer nuclear layer (peripheral box). Patient consent has been obtained for publication of this figure. Whitney rank sum test: p,0.001). Based on the RPE-OScomplex thickness measurements of normal eyes, a thickness profile of the 6 mm long vertically oriented scan was generated. This graphical presentation of the mean RPE-OScomplex thickness profile showed a rise in the central ,1000 mm of the scan, corresponding to the long cone photoreceptor outer segments in this region (fig 3). In healthy subjects, the ratio of intensity of backscattered light from the outer nuclear layer was identical in the central part of the macula as compared with the peripheral part (IratioONL = 1.06). The mean central retinal thickness was 161.5 mm (SD = 15.2). The normative values of the 25 healthy eyes, as obtained by the semiautomatic algorithm on the contrast-enhanced OCT images, are listed in table 1. The validity of the algorithm was tested by assessing the degree of agreement between the algorithm generated foveolar RPE-OScomplex thickness measurements versus caliper assisted thickness measurement on single Stratus OCT images. Additionally, we tested the degree of agreement between foveal retinal thickness measurements obtained from Stratus OCT software and the new algorithm. The caliper measurements were performed on the eight single Stratus OCT raw scans used in the contrast-enhanced image, utilising the built-in software of the OCT machine. The mean of the eight thickness measurements was compared with the measurement obtained Table 1 Characteristics and normative data of 25 healthy eyes obtained by the new algorithm operating on contrast-enhanced stratus OCT images
Normals (n = 25) Mean visual acuity in ETDRS letters (range) Mean spherical refraction in dioptres (range) Algorithm measurements I RPE-OScomplex in the foveola (mm) (SD) RPE-OScomplex 2 mm inferior of foveola (mm) (SD) RPE-OScomplex 1 mm inferior of foveola (mm) (SD) RPE-OScomplex 2 mm superior of foveola (mm) (SD) RPE-OScomplex 1 mm superior of foveola (mm) (SD) II Retinal thickness in the foveola (mm) (SD) III Iratio-ONL Stratus caliper measurements RPE-OScomplex in the foveola (mm) (SD) Retinal thickness in the foveola (mm) (SD) 86 (7991) Plano (23.75 to 2.25)
77.2 (3.95) 62.16 (3.05) 63.76 (3.38) 65.36 (3.77) 67.84 (3.74) 161.5 (15.2) 1.06 (0.11) 75.3 (4.00) 166.3 (15.8)
Figure 3 Mean thickness profile (black line) of the outer photoreceptor layer (outer photoreceptor- and retinal pigment epithelium layer (RPEOScomplex)) of 25 normal eyes as obtained vertically on a 6 mm long contrast-enhanced optical coherence tomography image. Black punctuated lines: 2SD of the mean.
802
For comparison reasons, values of foveolar RPE-OScomplex thickness and central retinal thickness, as obtained manually by the Stratus OCT caliper measuring tool, are also provided. ETDRS letters, number of letters seen on the Early Treatment of Diabetic Retinopathy Study Chart (8488 letters corresponds to 20/20); Iratio-ONL, central- versus peripheral pixel light intensity of the outer nuclear layer; RPE-OScomplex, retinal pigment epithelium and photoreceptor outer segment thickness.
Br J Ophthalmol 2008;92:800805. doi:10.1136/bjo.2007.130500
Downloaded from bjo.bmj.com on October 20, 2010 - Published by group.bmj.com
Clinical science
from the enhanced OCT image. All caliper measurements were performed in a masked set-up, that is without any knowledge of the corresponding algorithm generated values. Specifically, measurements of outer photoreceptor layer thickness were obtained by positioning the centre of the caliper-crosses directly at the inner- and outer borders of the hyperreflective layer in the outer retina. Figure 4A,B shows the two scatter diagrams where all data points are near the line of equality. Figure 4C,D shows a plot of the difference between the methods against their mean. We find discrepancies between the Stratus algorithm and the new algorithm of up to 11 mm in foveal retinal thickness measurements, and between the manual caliper method and the automatic algorithm of up to 9 mm in RPE-OScomplex thickness measurements. value when assessing retinal reactions to degenerative diseases or surgical trauma. Thus, increased levels of backscattered light might indicate high levels of glia tissue. Validation analyses compared thickness measurements obtained manually using Stratus OCT software with thickness measurements from our new semiautomatic algorithm. We found discrepancies between the two methods of up to 11 mm in retinal thickness measurements and up to 9 mm in RPE-OScomplex thickness measurements. These small differences are acceptable in daily clinical evaluations; however, the new algorithm has one major advantage over the Stratus caliper measurements in being automatic and independent of observer variations. The method used in this study for suppressing image noise and speckle has previously been presented by Sander and Jrgensen.4 5 By optimising the backscatter of the OCT scans the photoreceptor- and retinal pigment epithelium layers will be clearly visible thus enabling quantitative measurements. Also, the integrity of the IS/OS junction which is an important indicator for restoration of visual function1016 can easily be assessed in the contrast-enhanced OCT images. The methodology of this study of course is limited by possible sampling errors introduced by the alignment- and averaging procedure when sampling the enhanced OCT images. Aligning raw scans which are slightly decentred will lead to misinterpretations of subtle intraretinal changesfor example
DISCUSSION
Contrast-enhanced OCT imaging was capable of quantifying the outer photoreceptor layer in healthy subjects. We have presented normative values of outer photoreceptor layer thickness and demonstrated a difference in outer photoreceptor layer thickness between corresponding areas of inferior and superior macula. Additionally, we have introduced the ratio of intensity of backscattered light from the outer nuclear layer in the central part of the retina as compared with the peripheral part. This ratio is close to 1 in healthy subjects but may have
Figure 4 (A, B) Scatter plots of foveal retinal thickness and foveolar outer photoreceptor- and retinal pigment epithelium layer (RPE-OScomplex) thickness measured with standard Stratus optical coherence tomography (OCT) software and with the new semiautomatic algorithm. (C, D) Difference against the mean for foveal retinal thickness data and foveolar RPE-OScomplex thickness measured using Stratus OCT software and with the new semiautomatic algorithm. The RPE-OScomplex thickness was measured using Stratus OCT software by manually positioning the centre of the calipercrosses directly at the inner- and outer borders of the hyper-reflective layer in the outer retina.
Br J Ophthalmol 2008;92:800805. doi:10.1136/bjo.2007.130500 803
Downloaded from bjo.bmj.com on October 20, 2010 - Published by group.bmj.com
Clinical science
underestimation of central RPE-OScomplex thickness. Therefore, it is important that each scan used in the image enhancing is selected manually after inspection for qualitative identical images. Scans which are obviously decentred should be rejected. Because the Stratus OCT used in this study does not contain an eye-tracking system, we have no possibility to test for 100% identical retinal scan location, except than to visually inspect and compare the 20 (presumed) identical scans before running the software alignment procedure. However, the basis for noise reduction is that the recorded speckle patterns will wary only in cases when the image geometry is slightly modified; therefore small movements of the retina relative to the imaging geometry during image recording is necessary for increasing the signal-tonoise ratio of the enhanced image. This means that the loci of the A-scans scatter around the ideal scan path and some transverse resolution will be lost in the combined image as compared with that of a singe B-scan. However, due to the increase in signal to noise ratio by 34 times, segmentation and characterisation of the retinal layers is facilitated. Regarding axial measurements multiple scattering events in especially outer retinal layers theoretically may overestimate thickness measurements slightly. We have previously shown that the lateral resolution of the average image is close to 25 mm and the axial resolution below 10 mm, indicating a high-quality image.5 Although ultrahigh-resolution OCT systems give a better resolution,9 these systems will not be available for most ophthalmological departments in the near future. Thus, one important strength of image enhancing as described by Sander and Jrgensen4 5 is that image data are provided by the Stratus OCT, which is found in most ophthalmological departments and large clinics. New spectral-domain OCT (SD-OCT) systems are now available with simultaneous capture of the OCT image and the fundus image (Cirrus HD-OCT, Carl Zeiss Meditec; Spectralis HRA+OCT, Heidelberg Engineering). These systems ensure precise registration between the OCT scan and the fundus image, and are potentially capable of performing these measurements in a more satisfying way by shortening the time over which images are acquired. With such a system, one needs only to perform the axial registration when combining a series of recordings to form an enhanced image. The first report using SD-OCT with multiple B-scan averaging has just recently been published,17 but unfortunately this study is only qualitative and does not provide quantitative measurements of the intraretinal layers. Additionally the caliper tools of the software in these scanners are subject to potentially considerable interobserver variations due to the very small screens allocated when placing the calipers. After considering these possible confounders, it is our experience that quantification of contrast-enhanced images is useful in research and clinical decision-making of retinal diseases where the integrity of the photoreceptor layer and thus central vision may be compromised. The normative values of outer photoreceptor layer thickness (RPE-OScomplex), as presented in this study, therefore may be valuable. Additionally, the normative value of backscattered light the central part of retina (Iratio-ONL) may be valuable when studying retinal reactions to surgical intervention, that is after macula-off retinal detachment or full-thickness macular hole. Besides presenting normative values of the outer photoreceptor layer, we found a significantly thicker outer photoreceptor layer in the superior macula as compared with the inferior macula. To our knowledge, there is no evidence of a difference in retinal morphology between the superior and inferior macula in humans. However,
804
our observation supports recent observations of significantly better reading performance in 6u (<1444 mm) of eccentric viewing when using the superior retina as compared with the inferior retina.18 During the conduction of this study, we found that the Stratus OCT algorithm had difficulties in detecting the retinal boundaries used for retinal thickness measurements in some cases. Especially in cases with irregular macular surface configuration or defects/breaks in the normally homogenous IS/OS-line, the Stratus OCT algorithm often showed errorbased patterns. Previous reports have addressed this erroneous retinal thickness measurements in eyes with macular pathology.1922 We found that contrast-enhanced OCT imaging and automated delineation were superior to the Stratus OCT algorithm in detecting the retinal boundaries in these cases. Thus, we expect the new algorithm will find good applicability in cases with retinal pathology, where relatively small errors of the Stratus algorithm may have extensive affects on thickness measurements. In conclusion, the present study for the first time has introduced normative values of outer photoreceptor layer thickness and demonstrated a difference in outer photoreceptor layer thickness between corresponding areas of inferior and superior macula. Our hope is that the objective thickness measurements on contrast-enhanced OCT images can aid assessing and understanding better the relationship between functional outcome and photoreceptor morphology after resolution of retinal diseases involving the macula.
Funding: The Danish Eye Health Society; The Danish Medical Research Council; The John and Birthe Meyer Foundation. Competing interests: None. Ethics approval: Approval was obtained from the local Committee on Biomedical Research Ethics. Patient consent: Informed consent according to the tenets of the Declaration of Helsinki was obtained from all subjects before entering the study
REFERENCES
1. 2. Puliafito CA, Hee MR, Lin CP, et al. Imaging of macular diseases with optical coherence tomography. Ophthalmology 1995;102:21729. Ko TH, Fujimoto JG, Duker JS, et al. Comparison of ultrahigh- and standard-resolution optical coherence tomography for imaging macular hole pathology and repair. Ophthalmology 2004;111:203343. Chan A, Duker JS, Ishikawa H, et al. Quantification of photoreceptor layer thickness in normal eyes using optical coherence tomography. Retina 2006;26:65560. Sander B, Larsen M, Thrane L, et al. Enhanced optical coherence tomography imaging by multiple scan averaging. Br J Ophthalmol 2005;89:20712. Jrgensen TM, Thomadsen J, Christensen U, et al. Enhancing the signal-to-noise ratio in ophthalmic optical coherence tomography by image registrationmethod and clinical examples. Biomed Opt 2007;12:041208. Early Treatment Diabetic Retinopathy Study Research Group. Treatment techniques and clinical guidelines for photocoagulation of diabetic macular edema. Early Treatment Diabetic Retinopathy Study Report Number 2. Ophthalmology 1987;94:76174. Jrgensen TM, Thomadsen J, Thrane, et al. Dynamic contour model for aligning and segmenting OCT B-scans. Proceedings, Coherence domain optical methods and optical coherence tomography in biomedicine 9, San Jose, CA, 2326 January 2005. Tuchin VV, Izatt JA, Fujimoto JG, eds. (The International Society for Optical Engineering, Bellingham, WA, 2005) (SPIE Proceedings Series, 5690; Progress in Biomedical Optics and Imaging, vol. 6, no. 5), 2006:4805. Thomadsen J, Jrgensen TM, Christensen U, et al. Characterization of pre- and postoperative macular holes from retinal OCT images. Biophotonics imaging for diagnostics and treatment 2006;9. MICCAI conference, MICCAI workshop on biophotonics imaging, Lyngby (DK), 6 Oct 2006. Ersbll BK, Jorgensen TM, eds. (Technical University of Denmark, Informatics and Mathematical Modelling, Lyngby) (IMM-Technical report-2006-17), 2006:618. Drexler W, Sattmann H, Hermann B, et al. Enhanced visualization of macular pathology with the use of ultrahigh-resolution optical coherence tomography. Arch Ophthalmol 2003;121:695706. Villate N, Lee JE, Venkatraman A, et al. Photoreceptor layer features in eyes with closed macular holes: optical coherence tomography findings and correlation with visual outcomes. Am J Ophthalmol 2005;139:2809.
3. 4. 5.
6.
7.
8.
9.
10.
Br J Ophthalmol 2008;92:800805. doi:10.1136/bjo.2007.130500
Downloaded from bjo.bmj.com on October 20, 2010 - Published by group.bmj.com
Clinical science
11. 12. 13. 14. 15. 16. Kitaya N, Hikichi T, Kagokawa H, et al. Irregularity of photoreceptor layer after successful macular hole surgery prevents visual acuity improvement. Am J Ophthalmol 2004;138:30810. Uemoto R, Yamamoto S, Aoki T, et al. Macular configuraion determined by optical coherence tomography after idiopathic macular hole surgery with or without internal limiting membrane peeling. Br J Ophthalmol 2002;86:12402. Haritoglou C, Neubauer AS, Reiniger IW, et al. Long-term functional outcome of macular hole surgery correlated to optical coherence tomography measurements. Clin Experiment Ophthalmol 2007;35:20813. Ota M, Tsujikawa A, Murakami T, et al. Association between integrity of foveal photoreceptor layer and visual acuity in branch retinal vein occlusion. Br J Ophthalmol 2007;91:16449. Eandi CM, Chung JE, Cardillo-Piccolino F, et al. Optical coherence tomography in unilateral resolved central serous chorioretinopathy. Retina 2005;25:41721. Piccolino FC, de la Longrais RR, Ravera G, et al. The foveal photoreceptor layer and visual acuity loss in central serous chorioretinopathy. Am J Ophthalmol 2005;139: 8799. 17. 18. 19. 20. 21. 22. Sakamoto A, Hangai M, Yoshimura N. Spectral-domain optical coherence tomography with multiple B-scan averaging for enhanced imaging of retinal diseases. Ophthalmology. In press. Frennesson C, Nilsson SE. The superior retina performs better than the inferior retina when reading with eccentric viewing: a comparison in normal volunteers. Acta Ophthalmol Scand 2007;85:86870. Costa RA, Calucci D, Skaf M, et al. Optical coherence tomography 3: Automatic delineation of the outer neural retinal boundary and its influence on retinal thickness measurements. Invest Ophthalmol Vis Sci 2004;45:2399406. Sadda SR, Wu Z, Walsh AC, et al. Errors in retinal thickness measurements obtained by optical coherence tomography. Ophthalmology 2006;113:28593. Sadda SR, Tan O, Walsh AC, et al. Automated detection of clinically significant macular edema by grid scanning optical coherence tomography. Ophthalmology 2006;113:1187.e112. Ray R, Stinnett SS, Jaffe GJ. Evaluation of image artifact produced by optical coherence tomography of retinal pathology. Am J Ophthalmol 2005;139: 1829.
Submit an eLetter, and join the debate
eLetters are a fast and convenient way to register your opinion on topical and contentious medical issues. You can find the submit a response link alongside the abstract, full text and PDF versions of all our articles. We aim to publish swiftly, and your comments will be emailed directly to the author of the original article to allow them to respond. eLetters are a great way of participating in important clinical debates, so make sure your voice is heard.
Br J Ophthalmol 2008;92:800805. doi:10.1136/bjo.2007.130500
805
You might also like
- Feng Et Al 2023 Epithelial Thickness Mapping in Keratoconic Corneas Repeatability and Agreement Between Cso Ms 39Document14 pagesFeng Et Al 2023 Epithelial Thickness Mapping in Keratoconic Corneas Repeatability and Agreement Between Cso Ms 39vahidsmpNo ratings yet
- OPtical Biometry Module Study With IOL Master 700Document11 pagesOPtical Biometry Module Study With IOL Master 700Chee Yuan LokNo ratings yet
- Kjo 32 172Document10 pagesKjo 32 172Nurul Dwi LestariNo ratings yet
- Artículo 5Document6 pagesArtículo 5María Oña MartosNo ratings yet
- OCT Guide To Interpreting PDFDocument98 pagesOCT Guide To Interpreting PDFBrit Lee100% (2)
- I1552 5783 57 9 Oct51Document18 pagesI1552 5783 57 9 Oct51Vladimir KobelevNo ratings yet
- Chalam 2010Document6 pagesChalam 2010Sonya MabroukNo ratings yet
- s12886 017 0419 1Document8 pagess12886 017 0419 1Madhu C KNo ratings yet
- Optical Coherence TomographyDocument82 pagesOptical Coherence TomographyPutri kartiniNo ratings yet
- 2015 Acta Endocrinologica - Optochiasmatic Syndrome Assessing Optic Nerve Changes by OCTDocument8 pages2015 Acta Endocrinologica - Optochiasmatic Syndrome Assessing Optic Nerve Changes by OCTHoratiuSilaghiNo ratings yet
- Diagnostic Ability of Retinal Ganglion Cell Complex, RetinalDocument7 pagesDiagnostic Ability of Retinal Ganglion Cell Complex, RetinalYoselin Herrera GuzmánNo ratings yet
- Age-related macular degeneration: Diagnosis, symptoms and treatment, an overviewFrom EverandAge-related macular degeneration: Diagnosis, symptoms and treatment, an overviewNo ratings yet
- Focal Structure-Function Relationships in Primary Open-Angle Glaucoma Using OCT and OCT-A MeasurementsDocument10 pagesFocal Structure-Function Relationships in Primary Open-Angle Glaucoma Using OCT and OCT-A MeasurementsAlejandro LondoñoNo ratings yet
- Automated 3-D Region-Based Volumetric Estimation of Optic Disc Swelling in Papilledema Using Spectral-Domain Optical Coherence TomographyDocument8 pagesAutomated 3-D Region-Based Volumetric Estimation of Optic Disc Swelling in Papilledema Using Spectral-Domain Optical Coherence TomographyKalo RafinNo ratings yet
- Optical Coherence Tomography 2Document82 pagesOptical Coherence Tomography 2Putri kartiniNo ratings yet
- 2012 MotaghiannezamDocument12 pages2012 MotaghiannezamTim WeberNo ratings yet
- Comparing CVA Defects To Local RNFLDocument9 pagesComparing CVA Defects To Local RNFLkagone walidNo ratings yet
- Combination of Snapshot Hyperspectral Retinal Imaging and Optical Coherence Tomography To Identify Alzheimer 'S Disease PatientsDocument13 pagesCombination of Snapshot Hyperspectral Retinal Imaging and Optical Coherence Tomography To Identify Alzheimer 'S Disease PatientsMadhu CkNo ratings yet
- Iras GTDocument8 pagesIras GTijudoptoNo ratings yet
- S R E D B O C T H E: Ignal and Esolution Nhancements in UAL EAM Ptical Oherence Omography of The Uman YEDocument10 pagesS R E D B O C T H E: Ignal and Esolution Nhancements in UAL EAM Ptical Oherence Omography of The Uman YEcanadianman989No ratings yet
- CET OCT in GlaucomaDocument6 pagesCET OCT in GlaucomaQuyen HuynhNo ratings yet
- Clinical Study: The Effects of Uncomplicated Cataract Surgery On Retinal Layer ThicknessDocument7 pagesClinical Study: The Effects of Uncomplicated Cataract Surgery On Retinal Layer ThicknessJohn ElfranNo ratings yet
- Deep Learning Is Effective For Classifying Normal Versus Age-Related MacularDocument6 pagesDeep Learning Is Effective For Classifying Normal Versus Age-Related MacularNicolòNo ratings yet
- Single Photon Emission Computed TomographyDocument15 pagesSingle Photon Emission Computed TomographyChris HartoyoNo ratings yet
- First Slit Lamp Integrated OCT Sept 2009Document1 pageFirst Slit Lamp Integrated OCT Sept 2009valbayerosNo ratings yet
- Thmoid Inus Ancer: ASE TudyDocument5 pagesThmoid Inus Ancer: ASE TudyOmkar KongariNo ratings yet
- 0006 10jmihi03-2980Document6 pages0006 10jmihi03-2980VenkatramanNo ratings yet
- Clinical Utility of Optical Coherence Tomography in GlaucomaDocument12 pagesClinical Utility of Optical Coherence Tomography in GlaucomaOkta Kurniawan SaputraNo ratings yet
- Optical Coherence TomographyDocument8 pagesOptical Coherence Tomographymotoy asaph musanNo ratings yet
- Avancés Technologique en SpectDocument43 pagesAvancés Technologique en Spectzahira zyatiNo ratings yet
- Weiland EMBS 2005Document3 pagesWeiland EMBS 2005Kumar PrabhatNo ratings yet
- Corneal Parameters Measurement in Healthy Subjects Using Scheimpflug and Anterior Segment Optical Coherence TomographyDocument6 pagesCorneal Parameters Measurement in Healthy Subjects Using Scheimpflug and Anterior Segment Optical Coherence TomographyvahidsmpNo ratings yet
- Temporal Bone Imaging: Comparison of Flat Panel Volume CT and Multisection CTDocument6 pagesTemporal Bone Imaging: Comparison of Flat Panel Volume CT and Multisection CTNovi DwiyantiNo ratings yet
- A Fresh Take On Optical Coherence TomographyDocument4 pagesA Fresh Take On Optical Coherence TomographysightbdNo ratings yet
- Imaging Techniques in Glaucoma: Presenter: Dr. Rujuta Moderator: Dr. Rita DhamankarDocument54 pagesImaging Techniques in Glaucoma: Presenter: Dr. Rujuta Moderator: Dr. Rita Dhamankardrvishalkulkarni2007No ratings yet
- Boe 13 1 65Document17 pagesBoe 13 1 65Rajesh KrishananNo ratings yet
- As OctDocument7 pagesAs OctRasha Mounir Abdel-Kader El-TanamlyNo ratings yet
- TAC PeñascoDocument10 pagesTAC PeñascoJose ManuelNo ratings yet
- The Start Button: As Simple As PressingDocument12 pagesThe Start Button: As Simple As Pressingevans DNo ratings yet
- Segmentation Errors in Macular Ganglion Cell Analysis As Determined by Optical Coherence Tomography in Eyes With Macular PathologyDocument8 pagesSegmentation Errors in Macular Ganglion Cell Analysis As Determined by Optical Coherence Tomography in Eyes With Macular PathologyMadhu C KNo ratings yet
- Inroduction: Brachyodanio) .For Applications in Developmental Biology, OCT Is of Interest Because It AllowsDocument16 pagesInroduction: Brachyodanio) .For Applications in Developmental Biology, OCT Is of Interest Because It AllowsvargheseNo ratings yet
- Texture AnalysisDocument6 pagesTexture AnalysisSumit ChakravartyNo ratings yet
- Automatic Method of Analysis of OCT Images in Assessing The Severity Degree of Glaucoma and The Visual Field LossDocument18 pagesAutomatic Method of Analysis of OCT Images in Assessing The Severity Degree of Glaucoma and The Visual Field LossGirija BalajiNo ratings yet
- 2010 Jbo Multispectral in Vivo Three-Dimensional Optical Coherence Tomography of Human SkinDocument15 pages2010 Jbo Multispectral in Vivo Three-Dimensional Optical Coherence Tomography of Human Skinapi-299727615No ratings yet
- Master Thesis Optical Coherence TomographyDocument6 pagesMaster Thesis Optical Coherence Tomographydebbirchrochester100% (2)
- Body Mass Index and Interocular Asymmetry of Retinal and Choroidal Thickness in Emmetropic and Ametropic SubjectsDocument13 pagesBody Mass Index and Interocular Asymmetry of Retinal and Choroidal Thickness in Emmetropic and Ametropic SubjectsAthenaeum Scientific PublishersNo ratings yet
- Optical Coherence Tomography: An Emerging Technology For Biomedical Imaging and Optical BiopsyDocument17 pagesOptical Coherence Tomography: An Emerging Technology For Biomedical Imaging and Optical BiopsyoverkindNo ratings yet
- Determonacion Del Segmento Anterio Por OctDocument10 pagesDetermonacion Del Segmento Anterio Por OctFelipe AlarcónNo ratings yet
- 1 s2.0 S2212440312000442 MainDocument6 pages1 s2.0 S2212440312000442 MainMarinaNo ratings yet
- Imaging of Glaucoma DiagnosisDocument74 pagesImaging of Glaucoma Diagnosisabiraham zigaleNo ratings yet
- 2010-02-17-1109CRSTEuro Ambrosio Rs Reprint PDFDocument4 pages2010-02-17-1109CRSTEuro Ambrosio Rs Reprint PDFYunisNo ratings yet
- Wakabayashi 2010Document10 pagesWakabayashi 2010Sonya MabroukNo ratings yet
- A 3D Deep Learning System For Detecting Referable Glaucoma Using Full OCT Macular Cube ScansDocument14 pagesA 3D Deep Learning System For Detecting Referable Glaucoma Using Full OCT Macular Cube ScansAna-Maria ȘtefanNo ratings yet
- Computed TomographyDocument31 pagesComputed TomographyAvik Mukherjee100% (3)
- Ophthalmology Femtosecond LaserDocument5 pagesOphthalmology Femtosecond LaserChandrika MaluftiNo ratings yet
- PIIS0002939422003841Document6 pagesPIIS0002939422003841Anca Florina GaceaNo ratings yet
- Https:opg Optica Org:directpdfaccess: - 417296:boe-10-9-4896 Pdf?da 1&id 417296&seq 0&mobile NoDocument11 pagesHttps:opg Optica Org:directpdfaccess: - 417296:boe-10-9-4896 Pdf?da 1&id 417296&seq 0&mobile NoHarsh PanchalNo ratings yet
- Fmed 09 864879Document11 pagesFmed 09 864879804390887No ratings yet
- Radio Digital 1Document6 pagesRadio Digital 1Lucy Esther Calvo PerniaNo ratings yet
- Ijphrd VenkatDocument5 pagesIjphrd VenkatVenkatramanNo ratings yet
- Middle Ear CleftDocument17 pagesMiddle Ear CleftDrsreeram ValluriNo ratings yet
- (2001) Ultrasonographic Evaluation of The Eye Parameters in Dogs of Different AgeDocument4 pages(2001) Ultrasonographic Evaluation of The Eye Parameters in Dogs of Different Ageludiegues752No ratings yet
- Community Eye Health Journal How To Test For The Red Reflex in A Child 2014Document2 pagesCommunity Eye Health Journal How To Test For The Red Reflex in A Child 2014Kamilla GarciaNo ratings yet
- A+P CHP 15 QuizDocument8 pagesA+P CHP 15 QuizGennaroNo ratings yet
- Field of SpecialistDocument4 pagesField of Specialistapi-598083311No ratings yet
- Waves Aranoco Ppt-Anatomy of The EyeDocument40 pagesWaves Aranoco Ppt-Anatomy of The EyeARNOLD ARANOCONo ratings yet
- Optical Correction of Aphakia in Children: Review ArticleDocument12 pagesOptical Correction of Aphakia in Children: Review Articleaisa mutiaraNo ratings yet
- C S A A y I: N L S SDocument21 pagesC S A A y I: N L S SMiguel JaènNo ratings yet
- Reasons For Extraction of Primary Teeth in Jordan-A Study.: August 2013Document5 pagesReasons For Extraction of Primary Teeth in Jordan-A Study.: August 2013Mutia KumalasariNo ratings yet
- Classification of Partially Edentulous ArchesDocument27 pagesClassification of Partially Edentulous ArchesBharti DuaNo ratings yet
- Embryology of The EyeDocument29 pagesEmbryology of The EyeBimo Juliansyah100% (1)
- Management of Anterior Cross Bite in Mixed Dentition Using Catlan's ApplianceDocument4 pagesManagement of Anterior Cross Bite in Mixed Dentition Using Catlan's ApplianceRati Ramayani AbidinNo ratings yet
- Round No 2Document8 pagesRound No 2Taleb AliNo ratings yet
- Bates Method - Wikipedia, The Free EncyclopediaDocument14 pagesBates Method - Wikipedia, The Free EncyclopediaVd Vivek SharmaNo ratings yet
- Nerve Supply of FaceDocument1 pageNerve Supply of FaceYusri Arif100% (2)
- U2 Describing People Tiger 4Document9 pagesU2 Describing People Tiger 4marisa.yuste08No ratings yet
- Contact Lenses in Pediatrics CLIPStudyDocument7 pagesContact Lenses in Pediatrics CLIPStudyLorena MendozaNo ratings yet
- Long-Term Spontaneous Changes Following Removal of All First Premolars in Class I Cases With CrowdingDocument12 pagesLong-Term Spontaneous Changes Following Removal of All First Premolars in Class I Cases With CrowdingElizabeth MesaNo ratings yet
- Maxicare List of Dental Provider As of January 31, 2021Document68 pagesMaxicare List of Dental Provider As of January 31, 2021Cherry Lou38% (13)
- Daftar PustakaDocument5 pagesDaftar PustakaNISANo ratings yet
- Pseudo ExfoliationDocument6 pagesPseudo ExfoliationvannyanoyNo ratings yet
- IOL Power CalculationDocument27 pagesIOL Power CalculationAisha TahirNo ratings yet
- Part 1. Assessing Eyes: Unit 4 Patient Assessment 3 (Eyes and Ears)Document4 pagesPart 1. Assessing Eyes: Unit 4 Patient Assessment 3 (Eyes and Ears)rinaNo ratings yet
- A To Z Orthodontics Vol 25 Orthodontic MCQDocument113 pagesA To Z Orthodontics Vol 25 Orthodontic MCQghassanNo ratings yet
- Su PlayerDocument6 pagesSu Playernetra costumerNo ratings yet
- JKCD 6Document5 pagesJKCD 6sulistyowati_rnNo ratings yet
- DentalAnatomy ManualDocument285 pagesDentalAnatomy ManualMayleen Lee100% (1)
- Zhu2012 - Eye AnatomyDocument9 pagesZhu2012 - Eye Anatomytobing704No ratings yet
- Phacoemulsification Versus Small Incision Cataract Surgery For Treatment ofDocument7 pagesPhacoemulsification Versus Small Incision Cataract Surgery For Treatment ofRagni MishraNo ratings yet
- Final - Short & Long Question PhysiologyDocument2 pagesFinal - Short & Long Question Physiologykikukiku728No ratings yet