Professional Documents
Culture Documents
Family Nursing Process
Uploaded by
Rocel DevillesOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Family Nursing Process
Uploaded by
Rocel DevillesCopyright:
Available Formats
OUR LADY OF FATIMA UNIVERSITY COLLEGE OF NURSING NCM 101 FAMILY HEALTH NURSING Family Health Nursing
Involves a set of actions by which the nurse measure the status of the family as a client, their ability to maintain wellness, prevent and control or resolve problems in order to achieve health and well-being among its members.
Is a special field in nursing in which the family is the unit of care, health as its goal and nursing as its medium or channel of care.
Steps in Nursing Assessment 1. Data Collection The process of identifying the types or kinds of data needed. Specify the methods necessary to collect such data. Methods of Data Collection
Family Nursing Process It is a means by which the health care provider addresses the health needs and problems of the client. It is a logical and systematic, way of processing information gathered from different source and translating into meaningful actions or interventions. Steps: 1. Relating Establishing a working relationship. Results in positive outcomes such as good quality of data, partnership in addressing identified health need and problems, and satisfaction of the nurse and the client.
a.
Observation is use of all sensory capacities. The familys status can be inferred from the manifestations of problem areas reflected in the following: 1. communication & interaction pattern expected, used & tolerated by family members 2. role perceptions/ tasks assumptions by each member including decisionmaking patterns 3. conditions in the home & environment Physical Examination is done through inspection, palpation, percussion & auscultation Interview by completing health history for each member. Health history determines current health status. Record Review is the review existing records & reports pertinent to the client/ family such as diagnostic reports and immunization records. Laboratory/ Diagnostic tests
b. c. d.
e.
2.
Assessment Data Collection, data analysis and data interpretation and problem definition or nursing diagnosis.
Two types of assessment:
1. 2.
3.
First Level Assessment - Data on status/ conditions of family household members. Second Level Assessment - Data on family assumption of health tasks on each health problem identified in the First Level Assessment.
Planning Determination of how to assist client in resolving concerns related to restoration, maintenance or promotion of health. Establishment of priorities, set goals / objectives, selects strategies, describe rationale. Implementation The carrying out of plan of care by client and nurse, make ongoing assessment, update / revise plan, document responses. Evaluation A systematic, continuous process of comparing the clients response with written goal and objective. Determines progress and evaluate the implemented intervention as to: 1. Effectiveness 2. Efficiency 3. Adequacy 4. Acceptability 5. Appropriateness
5 Types of Date in Family Nursing Assessment (Initial Data Base) A. Family Structure, Characteristics and Dynamics 1. Members of the household and relationship to the head of the family 2. Demographic data - age, sex, civil status, position in the family 3. Place of residence of each member - whether living with the family or elsewhere. 4. Type of family structure - e.g. matriarchal or patriarchal, nuclear or extended 5. Dominant family members in terms of decision-making, especially in matters of health care. 6. General family relationship / dynamics - presence of any obvious / readily observable conflict between members; characteristic, communication / interaction pattern among members B. Socio-economic and Cultural Characteristics 1. Income and expenses a. Occupation, place of work and income of each working member b. Adequacy to meet basic necessities (food, clothing, shelter) c. Who makes decisions about money and how it is spent 2. Educational attainment of each member 3. Ethnic background and religious affiliation 4. Significant Others - role(s) they play in family's life 5. Relationship of the family to larger community - Nature and extent of participation of the family in community activities. Home and Environment 1. Housing a. Adequacy of living space b. Sleeping arrangement c. Presence of breeding or resting sites of vectors of disease (e.g. mosquitoes, roaches, flies, rodents, etc)
4.
5.
C.
I. Nursing Assessment
2. 3. 4. D.
d. Presence of accident hazards e. Food storage and cooking facilities f. Water supply - source, ownership, sanitary condition g. Garbage/ refuse disposal - type, sanitary condition h. Drainage system - type, sanitary condition Kind of neighborhood, e.g. congested, slum Social and health facilities available Communication and transportation facilities available
6. 7. 3.
Interpreting results of comparisons to determine signs and symptoms or cues of specific wellness state/s, health deficit/s, health threat/s, foreseeable crises/stress point/s and their underlying causes or associated factors. Making conclusions about the reasons for the existence of the health condition or problem, or risk for non-maintenance of wellness state/s which can be attributed to non-performance of family tasks.
Health Status of each Family Member 1. Medical and nursing history indicating current or past significant illnesses or beliefs and practices conducive to health and illness. 2. Nutritional assessment ( specially for vulnerable or risk at-risk members) a. Anthropometric data : Measures of nutritional status of children- weight, height, mid-upper arm circumference. b. Dietary history specifying quality and quantity of food/ nutrient intake per day c. Eating/feeding habits /practices 3. Developmental assessment of infants, toddlers, and preschoolers - e.g., Metro Manila Developmental Screening Test (MMDST) 4. Risk factor assessment indicating presence of major and contributing modifiable risk factors for - e.g. hypertension physical inactivity, sedentary lifestyle, cigarette/ tobacco smoking, elevated blood lipids/ cholesterol, obesity, diabetes mellitus, inadequate fiber intake, stress, alcohol drinking and other substance abuse. 5. Physical assessment indicating presence of illness state/s (diagnosed or undiagnosed by medical practitioners. Results of laboratory / diagnostic and other screening procedures supportive of assessment findings
Problem Definition/Nursing Diagnosis End result of 2 major types of assessment.
Family Nursing Problem - Stated as an inability to perform specific health task and the reasons / etiology) why the family cannot perform such task. Consists of 2 parts: main category of problem (coming from unattained health task) and specific problems (statement of factors contributory for the existence of the main problem. Example: (general): Inability to utilize resources for health care due to lack of adequate family resources, specifically: (specific) a. financial resources b. manpower resources c. time The more specific the problem definition, the more useful is the nursing diagnosis in determining the nursing intervention. Therefore, as many as three or four levels of problem definition can be stated.
6.
Typology of Nursing Problems in Family Nursing Practice 1. First Level of Assessment process whereby conditions/problems of the family are determined. existing potential health
E.
Values, Habits, Practices on Health Promotion, Maintenance and Disease Prevention Such as: 1. Immunization status of family members. 2. Healthy lifestyle practices. 3. Adequacy of : a. rest and sleep b. exercise / activities c. Use of protective measures - e.g. adequate footwear in parasite- infested areas; use of bednets and protective clothing in malaria and filariasis endemic areas. d. Use of relaxation and other stress management activities 4. Use of promotive-preventive health services. 2. Data Analysis Steps:
a. b.
Presence of Wellness Condition states as potential or readiness a clinical or nursing judgement about a client in transition from a specific level of wellness or capability to a higher level.
Presence of Health Deficits - Instances of failure in health maintenance. A. Illness States, regardless of whether it is diagnosed or undiagnosed by medical practitioner B. Failure to thrive/ develop according to normal rate C. Disability - whether (1) congenital or (2) arising from illness Presence of Health Threats - Conditions that are conducive to disease, accident or failure to realize one's health potential. A. Family history of hereditary condition / disease B. Threat of cross infection from a communicable disease case C. Family size beyond what family resources can adequately provide D. Accident hazards . 1. broken stairs 2. pointed /sharp objects, poisons, & medicines improperly kept 3. fire hazards 4. fall hazards 5. others (specify):________ E. Faulty / unhealthy nutritional / eating habits or feeding techniques / practices. 1. inadequate food intake both in quality and quantity
c.
1.
2.
Sorting of data for broad categories (such as those related with health status or practices about home and environment). Clustering of related cues to determine relationship among data. Distinguishing relevant form irrelevant data. This will help in deciding what information is pertinent to the situation at hand and what information is immaterial. Identifying patterns such as physiologic function, developmental, nutritional/dietary, coping/adaptation or communication patterns. Compare patterns with norms or standards of health, family functioning and assumption of health tasks.
3. 4. 5.
2. excessive intake of certain nutrients 3. faulty eating habits 4. ineffective breastfeeding 5. faulty feeding techniques F. Stress-provoking factors 1. strained marital relationship 2. strained parent-sibling relationship 3. interpersonal conflicts between family members 4. care-giving burden G. Poor home / environmental condition/ sanitation 1. inadequate living space 2. lack of food storage facilities 3. polluted water supply 4. presence of breeding or resting sites of vectors of diseases 5. improper garbage / refuse disposal 6. unsanitary waste disposal 7. poor lightning and ventilation 8. noise pollution 9. air pollution H. Unsanitary food handling and preparation I. Unhealthy lifestyle and personal habits /practices 1. alcohol drinking 2. cigarette / tobacco smoking 3. walking barefooted or inadequate footwear 4. eating raw meat or fish 5. poor personal hygiene 6. self-medication/ substance abuse 7. sexual promiscuity 8. engaging in dangerous sports 9. inadequate rest or sleep 10. lack of / inadequate exercise / physical activity 11. lack of / inadequate activities 12. non-use of self-protection measures (e.g. non-use of bednets in Malaria and Filariasis endemic areas) J. inherent personal characteristics - such as poor impulses control K. Health history which may precipitate / induce the occurrence of a health deficit, e.g. previous history of difficult labor. L. Inappropriate role assumption - e.g. child assuming mother's role, father not assuming his role M. Lack of immunization / inadequate immunization status specially of children N. Family disunity - e.g. self-oriented behavior of members (s), unresolved conflicts of members(s), intolerable disagreement O. Others, specify : _____________
L. M. N. O.
Death of a Member Resettlement in a new community Illegitimacy Other, Specify ______________
2.
Second Level of Assessment defines the nature or type of nursing problems that the family encounters in performing health. I. Inability to recognize the presence of the condition or problem due to: A. Lack of or inadequate knowledge B. Denial about its existence or severity as a result of fear of consequences of diagnosis of problem, specifically : 1. social-stigma, loss of respect of peers / significant others 2. economic / cost implications 3. physical consequences 4. emotional / psychological issues / concerns C. Attitude / philosophy in life which hinders recognition / acceptance of a problem D. Others, specify ____________ II. Inability to make decisions with respect to taking appropriate health action due to : A. Failure to comprehend the nature/ magnitude of the problem / condition B. Low salience of the problem / condition C. Feeling of confusion, helplessness and / or resignation brought by perceived magnitudes / severity of the situation or problem, i.e., failure to break down problems into manageable units of attacks D. Lack of / or inadequate knowledge / insight as to alternative courses of action to take E. Inability to decide which action to take among the list of alternatives F. Conflicting opinions among family members / significant others regarding action to take G. Lack of / or inadequate knowledge of community resources for care H. Fear of consequence of action, specially: social consequences economic consequences physical / psychological consequences I. Negative attitude towards the health problem By negative attitude is meant one that interferes with rational decision making J. Inaccessibility of appropriate resources for care, specifically: 1. physical inaccessibility 2. cost constraints or economic / financial inaccessibility K. L. Lack of trust / confidence in the health personnel / agency Others, specify______________
d.
Presence of Stress Points / Foreseeable Crisis - Anticipated periods of unusual demand on the individual or family in terms of adjustment / family resources. A. Marriage B. Pregnancy, labor, puerperium C. Parenthood D. Additional member - e.g. newborn, lodger E. Abortion F. Entrance at school G. Adolescence H. Divorce or separation I. Menopause J. Loss of Job K. Hospitalization of a family member
III. Inability to provide adequate nursing care to sick, disabled, dependent or vulnerable / at-risk member of the family due to: A. Lack of / inadequate knowledge about the disease / health condition (nature, severity, complications, prognosis and management ); B. Lack of / inadequate knowledge about the child development and care; Lack of / inadequate knowledge of the nature and extent of nursing care needed; C. Lack of the necessary facilities, equipment and supplies for care; D. Lack of or inadequate knowledge and skill in carrying out the necessary interventions / treatment / procedure / care (e.g., complex therapeutic regimen or healthy lifestyle program); E. Inadequate family resources for care, specifically: Absence of responsible member
F. G. H. I. J.
K.
Financial constraints Limitations / lack of physical resources e.g. isolation room Significant persons unexpressed feelings (e.g. hostility / anger, guilt, fear / anxiety, despair, rejection) which disable his / her capacities to provide care. Philosophy in life which negates / hinder caring the sick, disabled, dependent, vulnerable / At risk member Members preoccupation with own concerns / interests Prolonged disease or disability progression which exhausts supportive capacity of family members Altered role performance specify : a. role denial or ambivalence b. role strain c. role dissatisfaction d. role conflict e. role confusion f. role overload Others, specify _________________
J. K.
Negative attitude / philosophy in life which hinders effective / maximum utilization of community resources for health care Others, specify----------------
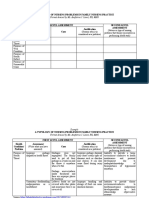
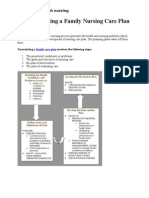
II. Planning The step in the process w/c answers the following questions: What is to be done? How is it to be done? When it is to be done? It is actually the phase wherein the health care provider formulates a care plan. Steps in developing a Family Nursing Care Plan 1. Prioritized problems 2. Goals and objectives of the nursing care 3. Plan of intervention 4. Plan for evaluating care Prioritizing Health Problems
IV. Inability to provide a home environment conducive to health maintenance and personal development due to : A. Inadequate family resources, specifically: a. financial constraints / limited financial resources b. limited physical resources e.g. lack of space to construct facility B. Failure to see benefits (specifically long-term ones) of investment in home environment improvement C. Lack of / inadequate knowledge of importance of hygiene and sanitation D. Lack of / inadequate knowledge of preventive measures E. Lack of skill in carrying out measures to improve home environment F. Ineffective communication patterns within the family G. Lack of supportive relationship among family members H. Negative attitude / philosophy in life which is not conducive to health maintenance and personal development I. Lack of / inadequate competencies in relating to each other for mutual growth and maturation (e.g. reduced ability to meet the physical and psychological needs of other members as a result of J. familys preoccupation with current problem or condition) K. Others, specify -------------------------V. Failure A. B. C. D. E. to utilize community resources for health care due to : Lack of / inadequate knowledge of community resources for health care Failure to perceive the benefits of health care / services Lack of trust / confidence in the agency / personnel Previous unpleasant experience with health worker Fear of consequences of action (preventive, diagnostic, therapeutic. Rehabilitative ), specifically : a. physical / psychological consequences b. financial consequences b. social consequences e.g. , loss of esteem of peer / significant others Unavailability of required care / service Inaccessibility of required care / service due to: cost constraints physical inaccessibility, i.e. location of facility Lack of or inadequate family resources, specifically ; a. manpower resources e.g. baby sitter b. financial resources e.g., cost of medicine prescribed Feeling of alienation to / lack of support from the community, e.g., stigma due to mental illness, AIDS, etc.
1. 2.
Nature of the Problem Presented - Categorized into wellness state, health threat, health deficit and foreseeable crisis. Modifiability of the Problem/Condition - Refers to the probability of success in enhancing, improving, minimizing, alleviating or totally eradicating the problem through intervention.
3. 4.
Scoring 1. 2.
Preventive Potentials - Refers to the nature and magnitude of future problems that can be minimized or totally prevented if intervention is done on the problem under consideration. Salience - Refers to the family's perception and evaluation of the problem in terms of seriousness and urgency of attention needed or family readiness.
Decide a score for each of the criteria divide the score by the highest possible & multiply by the weight
3.
Score Highest score
weight
Sum up the score of all criteria. The highest score is 5 equivalent to the total weight.
F. G. a. b. H. I.
CRITERIA 1. Nature of the problems Presented Scale: -Health deficit / Wellness 3 Health threat 2 - Foreseeable crisis 1 2. Modifiability of the problem Scale: 2 easily modifiable 1 Partially modifiable 0 Not modifiable 3. Preventive potential Scale: 3 High 2 Moderate 1 Low 4. Salience Scale: -A condition / problem 2 needing Immediate attention 1 A condition / problem not needing Immediate 0 attention Not perceived as a problem or condition needing change It revolves around identified health problems. It is a mean to an end and not a end to itself. It is a continuous process, not one shot deal.
Weight 1
Factors affecting priority setting: The nurse considers the availability of the following factors in determining the modifiability of a health condition or problem. 1. Current Knowledge, technology and interventions 2. Resources of the family - physical, financial & manpower 3. Resources of the nurse - knowledge, skills and time 4. Resources of the community - facilities and community organization or support Factors in Deciding Appropriate Score for Preventive Potential 1. Gravity or severity of the problem - Refers to the progress of the disease/ problem indicating extent of damage on the patient / family. Also indicates the prognosis, reversibility of the problem 2. Duration of the problem - refers to the length of time the problem has been existing 3. Current Management - refers to the presence and appropriateness of intervention 4. Exposure of any high risk group Family Nursing Care Plan It is the blueprint of care that the nurse designs to systematically minimize or eliminate the identified family health problem through explicitly formulated outcomes of care (goal and objectives) and deliberately chosen set of interventions/resources and evaluation criteria, standards, methods and tools. Characteristics of Family Nursing Care Plan 1. It focuses on actions w/c are designed to solve or alleviate & existing problem. 2. It is a product of deliberate systematic process. 3. The FNCP as with other plans relates to the future.
4. 5. 6.
Desirable Qualities of Family Nursing Care Plan 1. It should be based on a clear definition of the problem. 2. A good plan is realistic, meaning it can be implemented w/ reasonable chance of success 3. It should be consistent w/ the goals & philosophy of the health agency. 4. Its drawn w/ the family. 5. Its best kept in written form. Setting/ Formulating Goals & Objectives This will set direction of the plan. This should be stated in terms of client outcomes whether at the individual, family or community level. The mutual setting of goals w/c is the cornerstone of effective planning consists of: 1. Identifying possible resources. 2. Delineating alternative approaches to meet goals. 3. Selecting specific interventions. 4. Operationalizing the plan - setting of priorities. Goal It is a general statement of the condition or state to be brought about by specific courses of action.
Cardinal Principle in Goal setting
It must be set jointly with the family. This ensures family commitment to their realization. Basic to the establishment of mutually acceptable goal in the familys recognition and acceptance of existing health needs and problems.
IV. Evaluation
Barriers to Joint Goal Setting 1. Failure in the part of the family to perceive the existence of the problem. 2. Sometimes the family perceives the existence of the problem but does not see it as serious enough to warrant attention. Characteristics of Goals/ Objectives
Determination whether goals / objectives are met. Determination whether nursing care rendered to the family are effective. Determines the resolution of the problem or the need to reassess, and re-plan and re-implement nursing interventions.
According to Alfaro-LeFevre: Evaluation is being applied through the steps of the nursing process:
1. 2. 3. 4. 5.
Specific Measurable Attainable Realistic Time bound
Assessment changes in health status. Diagnosis if identified family nursing problems were resolved, improved or controlled. Planning are the interventions appropriate & adequate enough to resolve identified problems. Implementation determine how the plan was implemented, what factors aid in the success and determine barriers to the care.
Objective Refers to a more specific statement of desired outcome of care. They specify the criteria by which the degree of effectiveness of care is to be measured. Types of Objective 1. Short term or Immediate Objective Formulated for problem situation w/c require immediate attention & results can be observed in a relatively short period of time. They are accomplished w/ few HCP-family contacts & relatively less resources.
Types of Evaluation: Ongoing Evaluation analysis during the implementation of the activity, its relevance, efficiency and effectiveness. Terminal Evaluation undertaken 6-12 months after the care was completed. Ex-post Evaluation undertaken years after the care was provided
2.
3.
Medium or Intermediate objective Objectives w/c is not immediately achieved & is required to attain the long ones. Long Term or Ultimate Objective This requires several HCP-family contacts & an investment of more resources.
Plan of Actions/ Interventions Its aim is to minimize all the possible reasons for causes of the familys inability to do certain tasks. It is highly dependent on 2 Major Variables: 1. nature of the problem 2. the resources available to solve the problem Typology of Interventions
Steps in Evaluation: 1. Decide what to Evaluate. Determine relevance, progress, effectiveness, impact and efficiency 2. Design the Evaluation Plan Quantitative a quantifiable means of evaluation which can be done through numerical counting of the evaluation source. Qualitative descriptive transcription of the outcome conducted through interview to acquire an in-depth understanding of the outcome. 3. Collect Relevant Data that will support the outcome 4. Analyze Data - What does the data mean? 5. Make Decisions If interventions are effective, interventions done can be applied to other client / group with the similar circumstances If ineffective, give recommendations 6. Report / Give Feedbacks Dimensions of Evaluation
1. 2. 3.
Supplemental - the HCP is the direct provider of care. Facilitative - HCP removes barriers to needed services. Developmental - improves clients capacity.
III. Implementation Actual doing of interventions to solve health problems.
1. 2. 3. 4.
Effectiveness focused on the attainment of the objectives. Efficiency related to cost whether in terms on money, effort or materials. Appropriateness refer its ability to solve or correct the existing problem, a question which involves professional judgment. Adequacy pertains to its comprehensiveness.
Tools Being used during Evaluation Instruments are tools are being used to evaluate the outcome of the nursing interventions: Thermometer Tape measure Ruler BP apparatus Weighing scale Checklist Key Guide Questionnaires Return Demonstrations
Methods of Evaluation 1. Direct observation 2. Records review 3. Review of questionnaire 4. Simulation exercises
You might also like
- The Seasons of Life by Jim RohnDocument111 pagesThe Seasons of Life by Jim RohnChristine Mwaura97% (29)
- Cave Rescue ActivityDocument6 pagesCave Rescue Activityshweta bambuwalaNo ratings yet
- ScreenwritingDocument432 pagesScreenwritingkunalt09100% (4)
- CHN Skills Lab Module 2020Document138 pagesCHN Skills Lab Module 2020mysterioushumane100% (4)
- Public Speaking Skills for Career SuccessDocument7 pagesPublic Speaking Skills for Career SuccessAnish John100% (1)
- Nursing AssessmentDocument34 pagesNursing Assessmentjikkapoot0% (1)
- First Level of AssessmentDocument7 pagesFirst Level of AssessmentJai - Ho100% (1)
- Sample FNCPDocument90 pagesSample FNCPmuddVayne89% (19)
- A Typology of Nursing Problems in Family Nursing PracticeDocument10 pagesA Typology of Nursing Problems in Family Nursing PracticeAnika Ajihil100% (2)
- Nursing Assessment in Family Nursing PracticeDocument33 pagesNursing Assessment in Family Nursing PracticeLuis WashingtonNo ratings yet
- Family Health Tasks GuideDocument58 pagesFamily Health Tasks GuideJmarie Brillantes PopiocoNo ratings yet
- French Revolution ChoiceDocument3 pagesFrench Revolution Choiceapi-483679267No ratings yet
- Peptan - All About Collagen Booklet-1Document10 pagesPeptan - All About Collagen Booklet-1Danu AhmadNo ratings yet
- Records in Family Health Nursing PracticeDocument6 pagesRecords in Family Health Nursing PracticeA.j. Caraca88% (8)
- Maternal Child NursingDocument31 pagesMaternal Child Nursingmatrixtrinity88% (24)
- Community Health NursingDocument7 pagesCommunity Health NursingFreeNursingNotes87% (47)
- Community Health NursingDocument237 pagesCommunity Health Nursingjhing_apdan100% (2)
- Family Nursing Typology (COPAR)Document33 pagesFamily Nursing Typology (COPAR)Rhon Narciso100% (1)
- A guide to community health nursing and occupational healthDocument2 pagesA guide to community health nursing and occupational healthMaria Bernadette Manumbas60% (5)
- Module 6 CHN Family Nursing Process (Formulating and ImplementingDocument22 pagesModule 6 CHN Family Nursing Process (Formulating and ImplementingAirah Fajardo100% (5)
- Family Nursing Care Plan for Barefoot LifestyleDocument2 pagesFamily Nursing Care Plan for Barefoot LifestyleLawrence Espinosa50% (2)
- Family Nursing ProcessDocument7 pagesFamily Nursing Processaibuty75% (4)
- RANK HEALTH CONDITIONS ACCORDING CRITERIADocument1 pageRANK HEALTH CONDITIONS ACCORDING CRITERIAJm Bernardo50% (2)
- Community Health Nursing Review (Edited)Document407 pagesCommunity Health Nursing Review (Edited)api-2658787991% (35)
- Community Health Nursing LectureDocument5 pagesCommunity Health Nursing LectureEzraManzano33% (3)
- Related Learning Experience (RLE) Activity in NCM 104: Community Health Nursing 1 (Individual and Family) 1 Semester (A.Y. 2020-2021)Document5 pagesRelated Learning Experience (RLE) Activity in NCM 104: Community Health Nursing 1 (Individual and Family) 1 Semester (A.Y. 2020-2021)Borromeo, Kriztian Ralph O.No ratings yet
- Douglas Frayne Sargonic and Gutian Periods, 2334-2113 BCDocument182 pagesDouglas Frayne Sargonic and Gutian Periods, 2334-2113 BClibrary364100% (3)
- Aklan State University Community Health NursingDocument34 pagesAklan State University Community Health Nursingmysterioushumane100% (2)
- Nursing Care Plans for Diarrhea, Dehydration & Acute PainDocument13 pagesNursing Care Plans for Diarrhea, Dehydration & Acute PainRocel DevillesNo ratings yet
- Ethico-Legal Relevant To Health AssessmentDocument13 pagesEthico-Legal Relevant To Health AssessmentLorelie Asis79% (14)
- Typology of Nursing Problems in Family Nursing PracticeDocument2 pagesTypology of Nursing Problems in Family Nursing PracticeHarlene Joyce Rey100% (3)
- Hypertension FNCPDocument1 pageHypertension FNCPGerome T. Manantan100% (1)
- Family Nursing ProcessDocument25 pagesFamily Nursing ProcessJAMES ROD MARINDUQUE100% (1)
- Community Health NursingDocument8 pagesCommunity Health NursingFirenze Fil93% (30)
- Family Nursing Care PlanDocument19 pagesFamily Nursing Care Planɹǝʍdןnos95% (43)
- Making a Family Nursing Care Plan (FNCPDocument4 pagesMaking a Family Nursing Care Plan (FNCPMary LouNo ratings yet
- Community Health Nursing 1 Chapter 1Document42 pagesCommunity Health Nursing 1 Chapter 1Lawrence Ryan Daug100% (2)
- Ethical Considerations in Community Health NursingDocument19 pagesEthical Considerations in Community Health Nursingedgar malupengNo ratings yet
- Avanto Magnet System Error MessagesDocument21 pagesAvanto Magnet System Error MessagesMuhammad Ahmad75% (4)
- Family Nursing Care PlanDocument11 pagesFamily Nursing Care PlanFirenze Fil100% (34)
- Family Health Nursing ProcessDocument37 pagesFamily Health Nursing ProcessNeethu Vincent100% (2)
- Family Health Nursing 3Document60 pagesFamily Health Nursing 3mark Orpilla0% (1)
- Family Health Assessment FormDocument3 pagesFamily Health Assessment FormMitchTalledo100% (2)
- Community Health Nursing Philippines PDFDocument2 pagesCommunity Health Nursing Philippines PDFHeidi13% (8)
- Mafia Bride by CD Reiss (Reiss, CD)Document200 pagesMafia Bride by CD Reiss (Reiss, CD)Aurniaa InaraaNo ratings yet
- Family Health Nursing Practice 1Document42 pagesFamily Health Nursing Practice 1Pam LalaNo ratings yet
- Community Organizing Participatory Action Research (COPAR)Document22 pagesCommunity Organizing Participatory Action Research (COPAR)Evelyn F. Tadena100% (1)
- MATH 8 QUARTER 3 WEEK 1 & 2 MODULEDocument10 pagesMATH 8 QUARTER 3 WEEK 1 & 2 MODULECandy CastroNo ratings yet
- COMMUNITY HEALTH NURSING (Continuation)Document18 pagesCOMMUNITY HEALTH NURSING (Continuation)Angel Joy Catalan100% (2)
- Acute Coronary Syndrome - A Case StudyDocument11 pagesAcute Coronary Syndrome - A Case StudyRocel Devilles100% (2)
- FNCP ProperDocument4 pagesFNCP ProperLiezel Ann EstebanNo ratings yet
- Community Health Nursing ProcessDocument69 pagesCommunity Health Nursing ProcessDharylle CariñoNo ratings yet
- Family Health Nursing Exam GuideDocument2 pagesFamily Health Nursing Exam GuideJonaPhieDomingoMonteroIINo ratings yet
- FNCP Maglaya FormatDocument1 pageFNCP Maglaya Formatjovanie01100% (6)
- Family Nursing PracticeDocument34 pagesFamily Nursing PracticeAisa Castro Arguelles100% (3)
- FNCPDocument1 pageFNCPapi-383235850% (2)
- Scales For Ranking Family Health ProblemsDocument7 pagesScales For Ranking Family Health ProblemsJai - Ho0% (1)
- Lack of VentilationDocument1 pageLack of Ventilationsleep whatNo ratings yet
- FNCPDocument31 pagesFNCPmanilyn100% (1)
- Measures The Status of The FamilyDocument7 pagesMeasures The Status of The FamilyKitkat Aquino Cabugwas100% (1)
- Family Nursing ProcessDocument43 pagesFamily Nursing ProcessJenny Rose AnieteNo ratings yet
- Family Health Care: 1. Nuclear/nuclear Dyad 2. Multigenerational/extended 3. Single-Parent/incompleteDocument4 pagesFamily Health Care: 1. Nuclear/nuclear Dyad 2. Multigenerational/extended 3. Single-Parent/incompleteMatt SinnungNo ratings yet
- Nursing Assessment in Family Nursing PracticeDocument7 pagesNursing Assessment in Family Nursing PracticeJoshua MendozaNo ratings yet
- Topics Week 1 CHN 104Document80 pagesTopics Week 1 CHN 104Krizia Claire Marie RedondoNo ratings yet
- CHN ReportDocument14 pagesCHN ReportEldonVinceIsidroNo ratings yet
- CHN 1 (Module 3)Document13 pagesCHN 1 (Module 3)HazelNo ratings yet
- Family Nursing Process - 1Document14 pagesFamily Nursing Process - 1Reese TañedoNo ratings yet
- Family Nursing ProcessDocument12 pagesFamily Nursing ProcessChristine CornagoNo ratings yet
- Nursing Assessement in Family Nursing Practice AutosavedDocument92 pagesNursing Assessement in Family Nursing Practice AutosavedricciNo ratings yet
- Family Health Nursing Problems and SolutionsDocument41 pagesFamily Health Nursing Problems and SolutionsCathleen Nasis ForrosueloNo ratings yet
- Family Health NursingDocument40 pagesFamily Health NursingKATE LAWRENCE BITANTOSNo ratings yet
- 2023 - CHN - Topic 4Document99 pages2023 - CHN - Topic 4Mariah Angela PonceNo ratings yet
- Case Study - AGEDocument12 pagesCase Study - AGERocel DevillesNo ratings yet
- Budgetary InsufficiencyDocument2 pagesBudgetary InsufficiencyRocel DevillesNo ratings yet
- Panhypopituitarism: Causes, Signs, and TreatmentDocument22 pagesPanhypopituitarism: Causes, Signs, and TreatmentRocel Devilles100% (1)
- Case PresentationDocument28 pagesCase PresentationRocel DevillesNo ratings yet
- Distance LearningDocument24 pagesDistance LearningRocel DevillesNo ratings yet
- Week 2 LectureDocument41 pagesWeek 2 LectureRocel DevillesNo ratings yet
- Psyclone: Rigging & Tuning GuideDocument2 pagesPsyclone: Rigging & Tuning GuidelmagasNo ratings yet
- 1st ClassDocument18 pages1st Classchitl.23bi14075No ratings yet
- CFC KIDS FOR CHRIST 2020 FINAL EXAMDocument13 pagesCFC KIDS FOR CHRIST 2020 FINAL EXAMKaisser John Pura AcuñaNo ratings yet
- Law of The Limiting FactorsDocument4 pagesLaw of The Limiting FactorsBiswajit DarbarNo ratings yet
- Goldenberg and Reddy (2017)Document10 pagesGoldenberg and Reddy (2017)Mariana ToniniNo ratings yet
- College Physics Reasoning and Relationships 2nd Edition Nicholas Giordano Solutions ManualDocument36 pagesCollege Physics Reasoning and Relationships 2nd Edition Nicholas Giordano Solutions Manualshippo.mackerels072100% (22)
- Master of Advanced Nursing Practice degreeDocument2 pagesMaster of Advanced Nursing Practice degreeAgusfian Trima PutraNo ratings yet
- Plant Processes: Lesson 3Document3 pagesPlant Processes: Lesson 3Kayla Ta’jaeNo ratings yet
- Nodelman 1992Document8 pagesNodelman 1992Ana Luiza RochaNo ratings yet
- (Salim Ross) PUA 524 - Introduction To Law and The Legal System (Mid Term)Document4 pages(Salim Ross) PUA 524 - Introduction To Law and The Legal System (Mid Term)Salim RossNo ratings yet
- Land Equivalent Ratio, Growth, Yield and Yield Components Response of Mono-Cropped vs. Inter-Cropped Common Bean and Maize With and Without Compost ApplicationDocument10 pagesLand Equivalent Ratio, Growth, Yield and Yield Components Response of Mono-Cropped vs. Inter-Cropped Common Bean and Maize With and Without Compost ApplicationsardinetaNo ratings yet
- The Leaders of The NationDocument3 pagesThe Leaders of The NationMark Dave RodriguezNo ratings yet
- CVR College of Engineering: UGC Autonomous InstitutionDocument2 pagesCVR College of Engineering: UGC Autonomous Institutionshankar1577No ratings yet
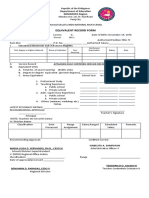
- Equivalent Record Form: Department of Education MIMAROPA RegionDocument1 pageEquivalent Record Form: Department of Education MIMAROPA RegionEnerita AllegoNo ratings yet
- Iso 696 1975Document8 pagesIso 696 1975Ganciarov MihaelaNo ratings yet
- Demo TeachingDocument22 pagesDemo TeachingCrissy Alison NonNo ratings yet
- Oposa vs. Factoran 224 Scra 792Document28 pagesOposa vs. Factoran 224 Scra 792albemartNo ratings yet
- Provisional List of Institutes1652433727Document27 pagesProvisional List of Institutes1652433727qwerty qwertyNo ratings yet
- Class 9 - Half Yearly Examination - 2023 - Portions and BlueprintDocument16 pagesClass 9 - Half Yearly Examination - 2023 - Portions and BlueprintSUBRAMANI MANOHARANNo ratings yet
- School readiness assessmentDocument10 pagesSchool readiness assessmentJave Gene De AquinoNo ratings yet