Professional Documents
Culture Documents
Appendix 1 Eliminating Rural-Disparities
Uploaded by
api-104972596Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Appendix 1 Eliminating Rural-Disparities
Uploaded by
api-104972596Copyright:
Available Formats
Eliminating Rural Disparities: Systematic Approach to Health Care Delivery Care
Luke Benko, Teresa Burks, Preston Fitzgerald, Jason Guichard, Ashley Mason, Laura Mills, Paul Packard, Jim Ryan, OStacia Schaffer, Karen Wager, Valerie West Medical University of South Carolina, Charleston, SC, USA INTRODUCTION
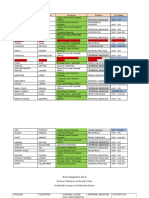
Objective: This study explores health care disparities in rural America, with particular emphasis on rural communities in South Carolina. We describe the demographics of rural communities, the degree to which rural citizens are at risk for health disparities, and some of the unique challenges facing rural health. Our study concludes with several health policy recommendations based upon our review of the literature, analysis of state-wide data, and interviews with key individuals. Definitions: According to the Office of Management and Budgets, a metropolitan area is a city with greater than 50,000 people. Anything non-metropolitan is considered rural, so according to this definition a city with less than 50,000 people is rural. In figure 1, showing the demographics of rural America and South Carolina, we see that a surprising high percentage of surface area in the US is indeed considered rural. Figure 1
METHODS
A literature review was performed to determine the definition of rural and identify rural health disparities and in addition, raw data was analyzed from the SC State Budget and Control Board. The remainder of the information for this poster was collected mainly through conducting interviews and focus groups with rural patients and healthcare providers and community leaders and advocates for rural health.
2. Education
Rural Citizens and their education (See Figure 6): less likely to receive preventative screening services minorities visit health care providers less often and receive less education because of limited access to high quality specialty care and specialists. limited high quality educational facilities public educational system is under funded, which diminishes recruitment for certified teachers, and the facilities are often outdated and poorly maintained. higher percentages of high school dropouts live below the national poverty level tend to be less likely to have attended/graduated from colleges/universities its important to remember that access is not everything. Education starts at childhood to change ingrained behaviors. (from a rural health policy maker at SCs Office of Rural Health)
4. Cost and Insurance (continued) The rising costs of healthcare are due to the following:
Advancements in technology Population characteristic changes (aging population, increased obesity, etc.) Increases in healthcare provider costs (mainly in-patient hospitalization, office-based visits and prescription costs) (www.ahrq.gov) Figure 8: Uninsured US Citizens Figure 9: US Citizens Living Below the Poverty Line
RESULTS
We discovered that the main barriers to healthcare for rural residents are transportation, lack of education, and low income/lack of health insurance, and access to specialists (Figure 5). Therefore, in an effort to work towards parity in rural healthcare, we have attempted not only to document the aforementioned causes of the problems, but also to offer solutions to help solve them. Figure 5 Rural Health Care Disparities
3. Access to Specialists
Patients in rural areas travel 2 to 3 times farther to see medical and surgical specialists than those living in urban areas. Chan, et al, The Journal of Rural Health; 2006; 22(140). (See also Figure 7) 39 SC counties have mental health professional shortage areas; all 46 SC counties have dental health professional shortage areas. (US Department of Health an d Human Services; HRSA) Figure 7
Primary care vs. specialty care physicians employed in 2003 in urban, rural, and very rural SC counties
% of physicians in county 80% 70% 60% 50% 40% 30% 20% 10% 0% urban county* rural county** rurality very rural county***
Transportation
Cost/Insurance
US Bureau of Census; Office of Management and Budget, 1998.
Education
Specialists
Disparities in healthcare between rural and urban residents are well documented. Not only do rural residents as a whole have less access to healthcare, but also have worse health outcomes due to a delay in getting appropriate care. Rural residents have higher rates of uncontrolled diabetes, higher death rates from acute MIs and higher rates of being uninsured than their urban counterparts, although differences by race and ethnicity exist (See Figures 2-4).
Figure 2. Adult Admissions for Uncontrolled Diabetes Without Complications per 100,000 Population, by Race Figure 3. Deaths per 1,000 Adult Admissions for Acute Myocardial Infarction, by Race/Ethnicity
HEALTH POLICY RECOMMENDATIONS
1. To Resolve Transportation Issues Incorporate the use of Healthcare Coaches:
Make transportation arrangements Provide referrals Make appointments for patients
1. Transportation
Factors Affecting Rural Residents:
67% lower socioeconomic class 43% less likely to own a vehicle 40% higher injury rates more chronic health conditions
primary care specialty care
American Public Health Association Fact sheet 2004
Transportation Issues:
80% rural areas have no public bus service 40% rural population lives in area without any type of public transportation system Federal government spends less than 10% of federal dollars for public transportation on rural areas
Rural Policy Research Institute www.rupri.org
* Charleston county ** Georgetown county ***Abbeville county Above counties were selected randomly to represent a cross-section of counties labeled as urban, rural, or very rural by the South Carolina Budget and State Control Board, Office of Research and Statistics; statistical data also obtained from the same source.
2. To Resolve Education Issues
Explore collaborative, university based specialty consults for rural community healthcare centers. Reform funding mechanism for public education
4. Cost and Insurance
Although 15.7% of the US population was without health insurance coverage in 2004, approximately 20% of rural residents were uninsured. (Figures 8 and 9)
3. To Resolve Specialist Issues
Extend scholarships and grants for healthcare providers willing to practice in rural areas Explore feasibility of using telemedicine to provide primary care practitioners in rural communities access to specialty care
Rural barriers to attending Diabetes Self Management Education Figure 6
Source: Agency for Healthcare Research and Quality, "Fact Sheet on Health Care Disparities in Rural Areas: Selected Findings From the 2004 National Healthcare Disparities Report." Key: Metropolitan=50,000 or more inhabitants, Micropolitan=10,000 to 50,000 inhabitants, Non-core= not metropolitan or micropolitan.
Health insurance and income level:
For the most part, rural = poorer. The most frustrating thing about caring for a poor, rural population is that they are poorly funded and a majority lack insurance or means to pay for the care they need. from a Family Medicine Doctor in Kingstree, SC There is a larger prevalence of uninsured citizens in rural communities than in urban communities. Each day in rural SC, 112 people receive medical services that they cannot pay for. Medicare and Medicaid accounted for 55% of rural inpatient hospitalization payments in 1999 Medicaid pays for a larger portion of emergency room visits and hospitalizations in rural SC than urban SC (www.ors2.state.sc.us)
4. To Resolve Cost/Insurance Issues
Rural communities tend to have a prominent number of small businesses therefore it would be beneficial to implement the program to help insure the employees of those small businesses The South Carolina Small Employer Health Plan provides a state-wide small employer coverage option that covers all employees in a group
(www.covertheuninsuredsc.org/policy.asp),
Figure 4. People Under Age 65 With Any Period of Uninsurance in Past Year, by Ethnicity
Graph from SC Rural Health Research Center 2004 http://rhr.sph.sc.edu/report/SCRHRC_KF_Diabetes.pdf
Subsidize the premium in this plan for covered individuals/families who are underinsured State or federal government health insurance reform
You might also like
- Rural UrbanDocument8 pagesRural UrbanSean McleanNo ratings yet
- Lake County2Document17 pagesLake County2api-528183036No ratings yet
- Rural Health ProjectDocument7 pagesRural Health ProjectSashaNo ratings yet
- ACCESS Transformed Full ReportDocument40 pagesACCESS Transformed Full ReportMark ReinhardtNo ratings yet
- Revitalizing the American Healthcare System: A Comprehensive Guide to Rebuilding, Reforming, and Reinventing Healthcare in the United States: Transforming the Future of Healthcare in America: A Practical and Inclusive ApproachFrom EverandRevitalizing the American Healthcare System: A Comprehensive Guide to Rebuilding, Reforming, and Reinventing Healthcare in the United States: Transforming the Future of Healthcare in America: A Practical and Inclusive ApproachNo ratings yet
- Program PlanningDocument9 pagesProgram PlanningRomnick Pascua TuboNo ratings yet
- Executive Summary 2006Document5 pagesExecutive Summary 2006Pin Siwatra SubhapholsiriNo ratings yet
- Insourced: How Importing Jobs Impacts the Healthcare Crisis Here and AbroadFrom EverandInsourced: How Importing Jobs Impacts the Healthcare Crisis Here and AbroadNo ratings yet
- Ali Med Soc PresentationDocument15 pagesAli Med Soc Presentationhali9000No ratings yet
- The Importance of Community Health CentersDocument15 pagesThe Importance of Community Health CentersJosh Queyquep100% (1)
- Yu 2020Document9 pagesYu 2020Epigmenio Díaz CruzNo ratings yet
- Additionals For The Research PaperDocument9 pagesAdditionals For The Research PaperSenouiiNo ratings yet
- Rural Fact Sheet-CardDocument2 pagesRural Fact Sheet-CardProgressOhio251No ratings yet
- NACHC 2022 Workforce Survey Full Report 1Document8 pagesNACHC 2022 Workforce Survey Full Report 1Bai Monisa GampongNo ratings yet
- 2021 Rural Health ChartbookDocument184 pages2021 Rural Health Chartbookjoseph.arkoNo ratings yet
- Health: Status and Access: Ashita AllamrajuDocument31 pagesHealth: Status and Access: Ashita AllamrajuAadhityaNo ratings yet
- Leveraging Census Data and Cathoic Charities Annual SurveyDocument25 pagesLeveraging Census Data and Cathoic Charities Annual SurveyCCUSA_PSMNo ratings yet
- The City and the Hospital: The Paradox of Medically Overserved CommunitiesFrom EverandThe City and the Hospital: The Paradox of Medically Overserved CommunitiesNo ratings yet
- Nur 340 Community Change Group Project Final VersionDocument23 pagesNur 340 Community Change Group Project Final Versionapi-239588178No ratings yet
- The Health of The African American Community in D.C.Document16 pagesThe Health of The African American Community in D.C.Christina Sturdivant100% (1)
- Healthcare Leadership and Rural Communities: Challenges, Strategies, and SolutionsFrom EverandHealthcare Leadership and Rural Communities: Challenges, Strategies, and SolutionsNo ratings yet
- Running Head: Policy Action Plan: Health Care Disparities 1Document9 pagesRunning Head: Policy Action Plan: Health Care Disparities 1api-509672908No ratings yet
- Literature ReviewDocument6 pagesLiterature Reviewapi-625929470No ratings yet
- Health Inequities by Rama Baru PDFDocument6 pagesHealth Inequities by Rama Baru PDFwrit majumdarNo ratings yet
- Behavioral Health: The Gap in California's Dual Eligible DemonstrationDocument34 pagesBehavioral Health: The Gap in California's Dual Eligible Demonstrationapi-79044486No ratings yet
- Community Assessment 26 Ebi Template WordDocument9 pagesCommunity Assessment 26 Ebi Template Wordapi-641501601No ratings yet
- In Search of Hippocrates: A Solution to the Health Care Crisis Facing AmericaFrom EverandIn Search of Hippocrates: A Solution to the Health Care Crisis Facing AmericaNo ratings yet
- Summarizing - Kharisma Okta AlfiyantiDocument3 pagesSummarizing - Kharisma Okta AlfiyantilaipiyajodohguanlinNo ratings yet
- Healthcare Delivery SystemDocument2 pagesHealthcare Delivery SystemMark Teofilo Dela PeñaNo ratings yet
- 7 Rural-RemoteTribal 508Document22 pages7 Rural-RemoteTribal 508Esayase AsnakeNo ratings yet
- Medication A.R.E.A.S. Bundle: A Prescription for Value-Based Healthcare to Optimize Patient Health Outcomes, Reduce Total Costs, and Improve Quality and Organization PerformanceFrom EverandMedication A.R.E.A.S. Bundle: A Prescription for Value-Based Healthcare to Optimize Patient Health Outcomes, Reduce Total Costs, and Improve Quality and Organization PerformanceNo ratings yet
- A Needs-Based Method For Estimating The Behavioral Health PDFDocument13 pagesA Needs-Based Method For Estimating The Behavioral Health PDFaprilNo ratings yet
- Restoring Quality Health Care: A Six-Point Plan for Comprehensive Reform at Lower CostFrom EverandRestoring Quality Health Care: A Six-Point Plan for Comprehensive Reform at Lower CostNo ratings yet
- Availability of Health ServicesDocument1 pageAvailability of Health Serviceswps.resengNo ratings yet
- Health Care's Blind Side PDFDocument12 pagesHealth Care's Blind Side PDFiggybauNo ratings yet
- RWJF Issue BriefDocument4 pagesRWJF Issue BriefiggybauNo ratings yet
- Swot Analysis of Rural Health HospitalDocument4 pagesSwot Analysis of Rural Health HospitalRainWalkerNo ratings yet
- Definition: What Is Resource Allocation?Document4 pagesDefinition: What Is Resource Allocation?tkas4uNo ratings yet
- Community Needs AssessmentDocument12 pagesCommunity Needs Assessmentrachael costello100% (1)
- Public Health NursesDocument4 pagesPublic Health NursesYang MolosNo ratings yet
- The Middleboro Casebook: Healthcare Strategy and Operations, Second EditionFrom EverandThe Middleboro Casebook: Healthcare Strategy and Operations, Second EditionNo ratings yet
- Community Assessment and Analysis: Name Institution Course DateDocument24 pagesCommunity Assessment and Analysis: Name Institution Course DateSamwel KangyNo ratings yet
- CH 01Document12 pagesCH 01eman abu koushNo ratings yet
- RWJFPhysicians Survey Executive SummaryDocument12 pagesRWJFPhysicians Survey Executive SummaryhousingworksNo ratings yet
- Tillman, Matt Rural Health Care HC Systems Paper (Final)Document17 pagesTillman, Matt Rural Health Care HC Systems Paper (Final)api-282411018No ratings yet
- BÁO CÁO QUẢN LÝ Y TẾDocument7 pagesBÁO CÁO QUẢN LÝ Y TẾLê MaiNo ratings yet
- WUC102TMA1Document4 pagesWUC102TMA1Choong LeongNo ratings yet
- Midwest Edition: Midwest Has High Quality ScoresDocument5 pagesMidwest Edition: Midwest Has High Quality ScoresPayersandProvidersNo ratings yet
- C4a Presentation Ss LM 9-27-12 FinalDocument53 pagesC4a Presentation Ss LM 9-27-12 Finalapi-79044486No ratings yet
- NutritionDocument44 pagesNutritionapi-240122097No ratings yet
- Minnesota Hospital Association's Lown Institute ResponseDocument3 pagesMinnesota Hospital Association's Lown Institute ResponseinforumdocsNo ratings yet
- Over View For The Health SystemDocument27 pagesOver View For The Health SystemWissam AlnaemahNo ratings yet
- LasellmDocument9 pagesLasellmapi-296534570No ratings yet
- VHC Annual Report 2011Document12 pagesVHC Annual Report 2011Orhan Mc MillanNo ratings yet
- Cost Trends Nov-2009Document27 pagesCost Trends Nov-2009mikebotta70No ratings yet
- Registered Nurse Shortage in Rural Healthcare SettingsDocument9 pagesRegistered Nurse Shortage in Rural Healthcare SettingsShelley KrumwiedeNo ratings yet
- Executive Summaryfinaldec42012Document4 pagesExecutive Summaryfinaldec42012api-104972596No ratings yet
- Capstone Paper 11-27-2011 Version 11-1lbkDocument55 pagesCapstone Paper 11-27-2011 Version 11-1lbkapi-104972596No ratings yet
- Appendix 16c Capstone Telemed Device Data Flow WithDocument1 pageAppendix 16c Capstone Telemed Device Data Flow Withapi-104972596No ratings yet
- Telehealth Annotated References Nov 27 FinalDocument108 pagesTelehealth Annotated References Nov 27 Finalapi-104972596No ratings yet
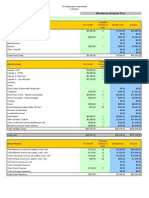
- Appendix 3 Financial AnalysisDocument4 pagesAppendix 3 Financial Analysisapi-104972596No ratings yet
- Mmi Capstone Presentation Nov 29Document31 pagesMmi Capstone Presentation Nov 29api-104972596No ratings yet
- Appendix 16b Tumc Telemedicine Device DeploymentDocument1 pageAppendix 16b Tumc Telemedicine Device Deploymentapi-104972596No ratings yet
- Appendix 16aDocument1 pageAppendix 16aapi-104972596No ratings yet
- Appendix 15 IbndianaDocument3 pagesAppendix 15 Ibndianaapi-104972596No ratings yet
- Appendix14 - Glucose Smart TrackingDocument52 pagesAppendix14 - Glucose Smart Trackingapi-104972596No ratings yet
- Teahm Study Action Final061511comp-2Document59 pagesTeahm Study Action Final061511comp-2api-104972596No ratings yet
- Appendix 15 MichiganDocument5 pagesAppendix 15 Michiganapi-104972596No ratings yet
- Appendix11 Example RFPDocument24 pagesAppendix11 Example RFPapi-104972596No ratings yet
- Appendix 13 Video StandardsDocument2 pagesAppendix 13 Video Standardsapi-104972596No ratings yet
- Appendix 7 Lewinf Model of ChangeDocument2 pagesAppendix 7 Lewinf Model of Changeapi-104972596No ratings yet
- Appendix 9 GlossaryDocument7 pagesAppendix 9 Glossaryapi-104972596No ratings yet
- Appendix 2 Telehealth Service Delivery ModelsDocument3 pagesAppendix 2 Telehealth Service Delivery Modelsapi-104972596No ratings yet
- Appendix 8 Home Telehealth Policy Ver3 5Document6 pagesAppendix 8 Home Telehealth Policy Ver3 5api-104972596No ratings yet
- Bimetricdataflow 406Document1 pageBimetricdataflow 406api-104972596No ratings yet
- Appendix 4 Reimbursement Issues WordDocument2 pagesAppendix 4 Reimbursement Issues Wordapi-104972596No ratings yet
- Appendix 6 Literature Telemedicine SupportDocument4 pagesAppendix 6 Literature Telemedicine Supportapi-104972596No ratings yet
- Appendix 5 WorkflowDocument3 pagesAppendix 5 Workflowapi-104972596No ratings yet
- Unofficial TranscriptsDocument2 pagesUnofficial Transcriptsapi-104972596No ratings yet
- Medical Informatics (Graduation December 2011) Through Northwestern University. This Program Focuses On The Technical, Organizational, andDocument3 pagesMedical Informatics (Graduation December 2011) Through Northwestern University. This Program Focuses On The Technical, Organizational, andapi-104972596No ratings yet
- RHCmanual 1Document164 pagesRHCmanual 1Disha SolankiNo ratings yet
- Geriatric Nursing - Roles and Responsibilities by Cyndi HojasDocument1 pageGeriatric Nursing - Roles and Responsibilities by Cyndi HojasKim Rose Sabuclalao100% (3)
- Collet Gps DNP FNP Copy With Grades Blacked OutDocument4 pagesCollet Gps DNP FNP Copy With Grades Blacked Outapi-251653314No ratings yet
- The Role of Social Work in Integrated Health: Judith Anne Debonis PHDDocument66 pagesThe Role of Social Work in Integrated Health: Judith Anne Debonis PHDGouri BhosaleNo ratings yet
- Role of RN in The Primary Health CareDocument7 pagesRole of RN in The Primary Health CareNandia SeptiyoriniNo ratings yet
- Test Bank For Medical Terminology A Living Language 7th Edition by FremgenDocument46 pagesTest Bank For Medical Terminology A Living Language 7th Edition by FremgenCarlos Derringer100% (28)
- Region Name of LaboratoryDocument7 pagesRegion Name of LaboratorySabling DritzcNo ratings yet
- National Suicide Prevention Strategy For EnglandDocument44 pagesNational Suicide Prevention Strategy For EnglandSara SimãoNo ratings yet
- Megatrends Kpmg-Healthcare-2030Document24 pagesMegatrends Kpmg-Healthcare-2030Cassiopeia ValenciaNo ratings yet
- LTO Accredited Clinics Region 7Document5 pagesLTO Accredited Clinics Region 7Ssa ZabalaNo ratings yet
- LF - Rural Health Clinic Start Up Business PlanDocument20 pagesLF - Rural Health Clinic Start Up Business PlanLauren Favela100% (4)
- BATHE TechniqueDocument3 pagesBATHE TechniqueYan Sheng HoNo ratings yet
- TMSDocument2 pagesTMSrapgabrielNo ratings yet
- Key - Tape Giáo Trình TOEIC CDocument127 pagesKey - Tape Giáo Trình TOEIC Cvu longNo ratings yet
- List of Clinic Chains in UsDocument90 pagesList of Clinic Chains in Usarpit.mNo ratings yet
- Impact of Continuing Medical Education For PrimaryDocument12 pagesImpact of Continuing Medical Education For Primaryxp7jmnh5rpNo ratings yet
- List of HDocument20 pagesList of HHari Dahal0% (1)
- Dubai Health Strategy 2016-2021 enDocument22 pagesDubai Health Strategy 2016-2021 enHasnain ShakirNo ratings yet
- Unit 1 PPT FinalDocument9 pagesUnit 1 PPT FinalRochelle Anne Abad Banda100% (1)
- Personal Health Record - Template For AdultsDocument16 pagesPersonal Health Record - Template For AdultsGeorgiana BlagociNo ratings yet
- TDJSept2021 Low Res 9.27.21Document44 pagesTDJSept2021 Low Res 9.27.21Nicole ScottNo ratings yet
- 2014-Updated Accredited DoctorsDocument17 pages2014-Updated Accredited DoctorsLizanne GauranaNo ratings yet
- Healthy LivingDocument16 pagesHealthy LivingThe Myanmar TimesNo ratings yet
- DR Martins Office - FNDocument4 pagesDR Martins Office - FNCJ Chan0% (1)
- National & Sttae Health Care Policy, National Population Policy, AyushDocument52 pagesNational & Sttae Health Care Policy, National Population Policy, Ayushkrishnasree100% (2)
- Texas COVID-19 Initial Pediatric Vaccine Allocation List (11-02-21)Document21 pagesTexas COVID-19 Initial Pediatric Vaccine Allocation List (11-02-21)CBS Austin WebteamNo ratings yet
- Health Care USA Chapter 13Document34 pagesHealth Care USA Chapter 13David Turner100% (1)
- 2022 UHP Provider Pharmacy Directory Central Florida and Treasure CoastDocument253 pages2022 UHP Provider Pharmacy Directory Central Florida and Treasure CoastArturo esparsaNo ratings yet
- Pain - SpringerDocument1,175 pagesPain - SpringerGrossl Schorr Fernando100% (1)
- Updated CHMF Providers ListDocument65 pagesUpdated CHMF Providers ListRaj BautistaNo ratings yet