Professional Documents
Culture Documents
Anti Tubercular Drugs
Uploaded by
Radowan AhmadCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Anti Tubercular Drugs
Uploaded by
Radowan AhmadCopyright:
Available Formats
Anti-tubercular 1
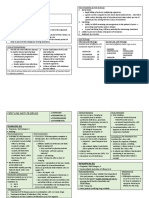
Anti Tubercular Drugs Tuberculosis is a common, and in many cases lethal, infectious disease caused by various strains of mycobacteria. Mycobacterium tuberculosis, one of a number of mycobacterium that causes tuberculosis infection and disease. Tuberculosis typically attacks the lungs and then infection will spread into genitourinary tract, skeleton and meninges. It is spread through the air when people who have an active tuberculosis infection cough, sneeze, or otherwise transmit their saliva through the air. Most infections are asymptomatic and latent, but about one in ten latent infections eventually progresses to active disease which, if left untreated, kills more than 50% of those so infected. The organism grows slowly; thus the disease may have to be treated for 6 months to 24 months. Resistant organisms readily emerge, particularly in patients who have had prior therapy or who fail to adhere to the treatment protocol. It is currently estimated that about one third of the worlds population is infected with Mycobacterium tuberculosis, with 30 million people having active disease. Worldwide 8 million new cases occur and approximately 2million people die of the disease each year.
Figure 01: Mycobacterium tuberculosis Tuberculosis occurs disproportionately among disadvantaged population such as the malnourished, homeless and those living in overcrowded and substandard housing. India had the highest total number of TB cases worldwide in 2010, in part due to poor disease management within the private health care sector. Programs such as the Revised National Tuberculosis Control Program are helping to reduce TB levels amongst people receiving public health care.
Anti-tubercular 2
Signs and Symptoms: 1. Malaise 2. Anorexia 3. Weight loss 4. Fever 5. Night sweats 6. Chronic cough, blood with sputum 7. Rarely, dyspnea
Figure 02: The main symptoms of variants and stages of tuberculosis are given Types: Anti-tubercular drugs are the antibiotics used in prevention and treatment of tuberculosis. There are three classes of anti-tubercular drugs. First-line Drugs for treatment of Tuberculosis: These are common anti-tubercular drugs. They are
1. Isoniazid (INH)
Anti-tubercular 3
2. Rifampicin (RMP) 3. Ethambutol (EMB) 4. Pyrizanamide (PZA) 5. Streptomycin (SM)
But Streptomycin is no longer considered as a first line drug by ATS/IDSA/CDC because of high rates of resistance.
Figure 03: Cumulative percentage of strains of Mycobacterium tuberculosis showing resistance to streptomycin. In short course treatment of tuberculosis the Isoniazid, Rifampicin, pyrazinamide and ethambutol is given for 2 months followed by Isoniazid and Rifampicin alone for 4 months. Second line Drugs for Treatment of Tuberculosis: There are six classes of second-line drugs (SLDs) used for the treatment of TB. These drugs have toxic side-effects (e.g., cycloserine) and some drugs are unavailable in many developing countries (e.g., fluoroquinolones): 1. Polypeptides like capreomycin.
2. Aminoglycosides like Amikacin, kanamycin. 3. Fluoroquinolones like ciprofloxacin, levofloxacin, moxifloxacin
4. Thioamides like ethionamide, prothionamide 5. Cycloserine 6. Para aminosalicylic acid
Anti-tubercular 4
Third line drugs for Treatment of tuberculosis: These drugs may be considered "third-line drugs" and are listed here either because they are not very effective (e.g., clarithromycin) or because their efficacy has not been proven (e.g., linezolid, R207910). Rifabutin is effective, but is not included on the WHO list because for most developing countries, it is impractically expensive. 1. Rifabutin 2. Macrolides like clarythromycin 3. Linezolid 4. Thioacetazone 5. Vitamin D 6. Thioridazine The standard regimen Tuberculosis has been treated with combination therapy for over fifty years. Drugs are not used singly (except in latent tuberculosis or chemoprophylaxis), and regimens that use only single drugs result in the rapid development of resistance and treatment failure. The rationales for using multiple drugs to treat tuberculosis are based on simple probability. The frequencies of spontaneous mutations that confer resistance to an individual drug are well known: 1 in 107 for EMB, 1 in 108 for STM and INH, and 1 in 1010 for RMP. A patient with extensive pulmonary tuberculosis has approximately 1012 bacteria in his body, and therefore will probably be harboring approximately 105 EMB-resistant bacteria, 104 STMresistant bacteria, 104 INH-resistant bacteria and 10 RMP-resistant bacteria. Resistance mutations appear spontaneously and independently, so the chances of him harboring a bacterium that is spontaneously resistant to both INH and RMP is 1 in 108 x 1 in 1010 = 1 in 1018, and the chances of him harboring a bacterium that is spontaneously resistant to all four drugs is 1 in 1033. This is, of course, an oversimplification, but it is a useful way of explaining combination therapy. There are other theoretical reasons for supporting combination therapy. The different drugs in the regimen have different modes of action. INH is bactericidal against replicating bacteria. EMB is bacteriostatic at low doses, but is used in TB treatment at higher, bactericidal doses.
Anti-tubercular 5
RMP is bactericidal and has a sterilizing effect. PZA is only weakly bactericidal, but is very effective against bacteria located in acidic environments, inside macrophages, or in areas of acute inflammation. All tuberculosis regimens in use were 18 months or longer until the appearance of rifampicin. Pharmacokinetic properties: The pharmacokinetic properties of the different anti-tubercular drugs are illustrated here. A. Isoniazid Isoniazid is the hydrazide of isonicotinic acid, is a synthetic analog of pyridoxine. It is the most potent of the antitubercular drugs but is never given as a single agent in the treatment of active tuberculosis. Its introduction revolutionized the treatment of tuberculosis.
Figure 04: Structure of Isoniazid Pharmacokinetics: Orally administered isoniazid is readily absorbed. Absorption is impaired if isoniazid is taken with food, particularly carbohydrates, or with aluminum-containing antacids. The drug diffuses into all body fluids, cells, and caseous material (necrotic tissue resembling cheese that is produced in tubercles). Drug levels in the cerebrospinal fluid (CSF) are about the same as those in the serum. The drug readily penetrates host cells and is effective against bacilli growing intracellularly. Infected tissue tends to retain the drug longer. Isoniazid undergoes Nacetylation and hydrolysis, resulting in inactive products. Chronic liver disease decreases metabolism, and doses must be reduced. Excretion is through glomerular filtration, predominantly as metabolites. Slow acetylators excrete more of the parent compound. Severely depressed renal function results in accumulation of the drug, primarily in slow acetylators. Adverse effects: The incidence of adverse effects is fairly low. Except for hypersensitivity, adverse effects are related to the dosage and duration of administration.
Anti-tubercular 6
Peripheral neuritis: Peripheral neuritis, which is the most common adverse
effect, appears to be due to a relative pyridoxine deficiency. Most of the toxic reactions are corrected by supplementation of 25 to 50 mg per day of pyridoxine (vitamin B6).
o
Hepatitis and idiosyncratic hepatotoxicity: Potentially fatal hepatitis is the most
severe side effect associated with isoniazid. It has been suggested that this is caused by a toxic metabolite of monoacetylhydrazine, formed during the metabolism of isoniazid. Its incidence increases among patients with increasing age, among patients who also take rifampin, or among those who drink alcohol daily.
o
Drug interactions: Because isoniazid inhibits metabolism of phenytoin (Figure
05), isoniazid can potentiate the adverse effects of that drug (for example, nystagmus and ataxia). Slow acetylators are particularly at risk.
Figure 05: Isoniazid potentiates the adverse effects of phenytoin
o
Other adverse effects: Mental abnormalities, convulsions in patients prone to
seizures, and optic neuritis have been observed. Hypersensitivity reactions include rashes and fever. B. Rifampin Rifampin, which is derived from the soil mold Streptomyces, has a broader antimicrobial activity than isoniazid and has found application in the treatment of a number of different bacterial infections. Because resistant strains rapidly emerge during therapy, it is never given as a single agent in the treatment of active tuberculosis.
Anti-tubercular 7
Figure 06: Structure of Rifampin Pharmacokinetics: Absorption is adequate after oral administration. Distribution of rifampin occurs to all body fluids and organs. Adequate levels are attained in the CSF even in the absence of inflammation. The drug is taken up by the liver and undergoes enterohepatic cycling. Rifampin itself can induce the hepatic mixed-function oxidases, leading to a shortened half-life. Elimination of metabolites and the parent drug is via the bile into the feces or via the urine. Adverse effects: Rifampin is generally well tolerated. The most common adverse reactions include nausea, vomiting, and rash. Hepatitis and death due to liver failure is rare; however, the drug should be used judiciously in patients who are alcoholic, elderly, or have chronic liver disease due to the increased incidence of severe hepatic dysfunction when rifampin is administered alone or concomitantly with isoniazid. Often, when rifampin is dosed intermittently, or in daily doses of 1.2 grams or greater, a flu-like syndrome is associated with fever, chills, and myalgias and sometimes is associated with acute renal failure, hemolytic anemia, and shock. Drug interactions: Because rifampin can induce a number of cytochrome P450 enzymes, it can decrease the half-lives of other drugs that are coadministered and metabolized by this system. This may lead to higher dosage requirements for these agents.
C. Pyrazinamide
Pyrazinamide is a synthetic, orally effective, bactericidal, antitubercular agent used in combination with isoniazid, rifampin, and ethambutol. It is bactericidal to actively dividing organisms, but the mechanism of its action is unknown. Pyrazinamide must be enzymatically hydrolyzed to pyrazinoic acid, which is the active form of the drug. Some resistant strains lack
Anti-tubercular 8
the pyrazinamidase. Pyrazinamide is active against tubercle bacilli in the acidic environment of lysosomes as well as in macrophages.
Figure 07: Structure of Pyrazinamide Pharmacokinetics: Pyrazinamide distributes throughout the body, penetrating the CSF. It undergoes extensive metabolism. Side effects: About one to five percent of patients taking isoniazid, rifampin, and pyrazinamide may experience liver dysfunction. Urate retention can also occur and may precipitate a gouty attack D. Ethambutol Ethambutol is bacteriostatic and specific for most strains of M. tuberculosis and M. kansasii. Ethambutol inhibits arabinosyl transferase, an enzyme that is important for the synthesis of the mycobacterial arabinogalactan cell wall. Resistance is not a serious problem if the drug is employed with other antitubercular agents.
Figure 08: Structure of Ethambutol Pharmacokinetics: Ethambutol can be used in combination with pyrazinamide, isoniazid, and rifampin to treat tuberculosis. Absorbed on oral administration, ethambutol is well distributed throughout the body. Penetration into the central nervous system (CNS) is therapeutically adequate in tuberculous meningitis. Both parent drug and metabolites are excreted by glomerular filtration and tubular secretion.
Anti-tubercular 9
Adverse effects: The most important adverse effect is optic neuritis, which results in diminished visual acuity and loss of ability to discriminate between red and green. Visual acuity should be periodically examined. Discontinuation of the drug results in reversal of the optic symptoms. In addition, urate excretion is decreased by the drug; thus, gout may be exacerbated. E. Streptomycin Streptomycin is the first antibiotic effective in the treatment of tuberculosis and is discussed with the aminoglycosides. Its action is directed against extracellular organisms. Infections due to streptomycin-resistant organisms may be treated with kanamycin or amikacin, to which these bacilli remain sensitive.
Figure 09: Structure of Streptomycin Pharmacokinetics: Administration: The highly polar, polycationic structure of the aminoglycosides prevents adequate absorption after oral administration. Therefore, Streptomycin must be given parenterally to achieve adequate serum levels. The bactericidal effect of Streptomycin is concentration and time dependent; that is, the greater the concentration of drug, the greater the rate at which the organisms die. They also have a postantibiotic effect. Because of these properties, once-daily dosing with the Streptomycin can be employed. This results in less toxicity and is less expensive to administer. The exceptions are pregnancy, neonatal infections, and bacterial endocarditis, in which these agents are administered in divided doses every 8 hours. Distribution: Streptomycin levels achieved in most tissues are low, and penetration into most body fluids is variable. Concentrations in CSF are inadequate, even when the meninges are inflamed. Streptomycin may be administered intrathecally or intraventricularly. High
Anti-tubercular 10
concentrations accumulate in the renal cortex and in the endolymph and perilymph of the inner ear, which may account for their nephrotoxic and ototoxic potential. Streptomycin cross the placental barrier and may accumulate in fetal plasma and amniotic fluid. Fate: Metabolism of the Streptomycin does not occur in the host. All are rapidly excreted into the urine, predominantly by glomerular filtration. Accumulation occurs in patients with renal failure and requires dose modification. Adverse effects: It is important to monitor plasma levels of gentamicin, tobramycin, and amikacin to avoid concentrations that cause dose-related toxicities. Patient factors, such as old age, previous exposure to aminoglycosides, and liver disease, tend to predispose patients to adverse reactions. The elderly are particularly susceptible to nephrotoxicity and ototoxicity.
F. Capreomycin
Capreomycin is a peptide that inhibits protein synthesis.
Figure 10: Structure of Capreomycin Pharmacokinetics: It is administered parenterally. Capreomycin is primarily reserved for the treatment of multidrug-resistant tuberculosis. Adverse effects: Careful monitoring of the patient is necessary because of this drug may induce nephrotoxicity and ototoxicity.
G. Cycloserine
Anti-tubercular 11
Cycloserine is an orally effective, tuberculostatic agent that appears to antagonize the steps in bacterial cell wall synthesis involving D-alanine.
Figure 11: Structure of Cycloserine Pharmacokinetics: It distributes well throughout body fluids, including the CSF. Cycloserine is metabolized, and both parent and metabolite are excreted in urine. Accumulation occurs with renal insufficiency. Adverse effects: Adverse effects involve CNS disturbances, and epileptic seizure activity may be exacerbated. Peripheral neuropathies are also a problem, but they respond to pyridoxine.
H. Ethionamide
Ethionamide is a structural analog of isoniazid, but it is not believed to act by the same mechanism. Ethionamide can inhibit acetylation of isoniazid.
Figure 12: Structure of Ethionamide Pharmacokinetics: It is effective after oral administration and is widely distributed throughout the body, including the CSF. Metabolism is extensive, and the urine is the main route of excretion. Adverse effects: Adverse effects that limit its use include gastric irritation, hepatotoxicity, peripheral neuropathies, and optic neuritis. Supplementation with vitamin B6 (pyridoxine) may lessen the severity of the neurologic side effects.
I.
Fluoroquinolones
Anti-tubercular 12
The fluoroquinolones, such as ciprofloxacin, moxifloxacin and levofloxacin, have an important place in the treatment of multidrug-resistant tuberculosis. Some atypical strains of mycobacteria are also susceptible. Newer fluorinated quinolones offer greater potency, a broader spectrum of antimicrobial activity, greater in vitro efficacy against resistant organisms, and in some cases, a better safety profile than older quinolones and other antibiotics. It seems likely that the number of drugs in this class of antibiotics will increase due to its wide antibacterial spectrum, favorable pharmacokinetic properties, and relative lack of adverse reactions. Unfortunately, their overuse has already led to the emergence of resistant strains, resulting in limitations to their clinical usefulness.
Figure 13: Structure of Ciprofloxacin Pharmacokinetics: Absorption: Only 35 to 70 percent of orally administered norfloxacin is absorbed, compared with 85 to 95 percent of the other fluoroquinolones. Intravenous preparations of ciprofloxacin, levofloxacin, and ofloxacin are available. Ingestion of the fluoroquinolones with sucralfate, antacids containing aluminum or magnesium, or dietary supplements containing iron or zinc can interfere with the absorption of these antibacterial drugs. Calcium and other divalent cations have also been shown to interfere with the absorption of these agents (Figure 14). The fluoroquinolones with the longest half-lives (levofloxacin and moxifloxacin) permit once-daily dosing.
Anti-tubercular 13
Figure 14: Effect of dietary calcium on the absorption of ciprofloxaxin Fate: Binding to plasma proteins ranges from 10 to 40 percent. All the fluoroquinolones distribute well into all tissues and body fluids. Levels are high in bone, urine, kidney, and prostatic tissue (but not prostatic fluid), and concentrations in the lung exceed those in serum. Penetration into cerebrospinal fluid is low except for ofloxacin, for which concentrations can be as high as 90 percent of those in the serum. The fluoroquinolones also accumulate in macrophages and polymorphonuclear leukocytes, thus being effective against intracellular organisms such as Legionella pneumophila. They are excreted by the renal route. Adverse effects: In general, these agents are very well tolerated. Toxicities similar to those for nalidixic acid have been reported for the fluoroquinolones.
Central nervous system problems: The most prominent central nervous system (CNS) effects of fluoroquinolone treatment are headache and dizziness or light-headedness. Thus, patients with CNS disorders, such as epilepsy, should be treated cautiously with these drugs
Gastrointestinal: The most common adverse effects of the fluoroquinolones are nausea, vomiting, and diarrhea, which occur in three to six percent of patients.
Phototoxicity: Patients taking fluoroquinolones are advised to avoid excessive sunlight and to apply sunscreens. However, the latter may not protect completely. Thus, it is advisable that the drug should be discontinued at the first sign of phototoxicity.
Connective tissue problems: Fluoroquinolones should be avoided in pregnancy, in nursing mothers, and in children less than 18 years of age, because articular cartilage erosion (arthropathy) occurs in immature experimental animals. Children with cystic
Anti-tubercular 14
fibrosis who receive ciprofloxacin have had few problems, but careful in adults, fluoroquinolones can infrequently cause ruptured tendons.
Contraindications: Moxifloxacin may prolong the QTc interval and, thus, should not be used in patients who are predisposed to arrhythmias or are taking antiarrhythmic medications.
Drug interactions: The effect of antacids and cations on the absorption of these agents was considered above. Ciprofloxacin and ofloxacin can increase the serum levels of theophylline by inhibiting its metabolism. This is not the case with the third- and fourth-generation fluoroquinolones, which may raise the serum levels of warfarin, caffeine, and cyclosporine.
J. Rifabutin Rifabutin is a derivative of rifampin, is the preferred drug for use in tuberculosis-infected with the human immunodeficiency virus (HIV) patients who are concomitantly treated with protease inhibitors or nonnucleoside reverse transcriptase inhibitors, because it is a less potent inducer of cytochrome P450 enzymes.
Figure 15: Structure of Rifabutin Dosage: 300 mg/day Adverse effects: Rifabutin has adverse effects similar to those of rifampin but can also cause uveitis, skin hyperpigmentation, and neutropenia.
K. Rifapentine
Anti-tubercular 15
Rifapentine has activity comparable to that of rifampin but has a longer half-life than rifampin and rifabutin, which permits weekly dosing. However, for the intensive phase (initial 2 months) of the short-course therapy for tuberculosis, rifapentine is given twice weekly. In the subsequent phase, rifapentine is dosed once per week for 4 months. To avoid resistance issues, rifapentine should not be used alone but, rather, be included in a three to four-drug regimen.
Figure 16: Structure of Rifapentine L. p-aminosalicylic Acid
Figure 17: Structure of P-aminosalicylic acid Pharmacokinetics: P-aminosalicylic acid is a bacteriostatic drug with poor CSF penetration. It acts by inhibiting folate synthesis and interferes with incorporation of p-amino benzoic acid. Dosage: The dose is 150 mg/kg per oral in divided doses with meals. Maximum allowed dose is 12 gm. Side effects: Side effects like gastrointenstinal disturbances, hypersensitivity like rash, feve malaise, arthralgia, and changes in blood count like leucopenia, agranulocytosis, eosinophilia, lymphocytosis, atypical mononucleosis, thrombocytopenia, hemolytic anemia. This drug is active against mycobacterium tuberculosis only.
You might also like
- Heart Attack ND WaterDocument1 pageHeart Attack ND WaterRadowan AhmadNo ratings yet
- Phytochemical and In-Vitro Study of Ethyl Acetate Extract ofDocument8 pagesPhytochemical and In-Vitro Study of Ethyl Acetate Extract ofRadowan AhmadNo ratings yet
- Pharmaceutical Quality ControlDocument6 pagesPharmaceutical Quality ControlRadowan AhmadNo ratings yet
- Giantbicycles 66253 Sedona - DXDocument1 pageGiantbicycles 66253 Sedona - DXRadowan AhmadNo ratings yet
- Refference: Palaestinum On Uterine Smooth Muscle of Rats and Guinea Pigs. J Ethnopharmacol. 65: 173Document3 pagesRefference: Palaestinum On Uterine Smooth Muscle of Rats and Guinea Pigs. J Ethnopharmacol. 65: 173Radowan AhmadNo ratings yet
- Occidentale), and Pink Peppercorn (Schinus Terebinthifolia), Are Enjoyed Worldwide While OtherDocument11 pagesOccidentale), and Pink Peppercorn (Schinus Terebinthifolia), Are Enjoyed Worldwide While OtherRadowan AhmadNo ratings yet
- Pinnata: Chapter 3: Design of in Vivo Investigations of The SDocument3 pagesPinnata: Chapter 3: Design of in Vivo Investigations of The SRadowan AhmadNo ratings yet
- Brine Shrimp Lethality Bioassay For Cytotoxic ActivityDocument4 pagesBrine Shrimp Lethality Bioassay For Cytotoxic ActivityRadowan Ahmad0% (1)
- ContraceptivesDocument8 pagesContraceptivesRadowan AhmadNo ratings yet
- Narcotic AnalgesicsDocument7 pagesNarcotic AnalgesicsRadowan AhmadNo ratings yet
- Vaccine:storage ConditionsDocument23 pagesVaccine:storage ConditionsRadowan AhmadNo ratings yet
- Antioxidant TestsDocument11 pagesAntioxidant TestsRadowan Ahmad100% (1)
- A Paperless Department of PharmacyDocument15 pagesA Paperless Department of PharmacyRadowan AhmadNo ratings yet
- Who Can Appraise PerformanceDocument5 pagesWho Can Appraise PerformanceRadowan AhmadNo ratings yet
- PharmacogeneticsDocument46 pagesPharmacogeneticsRadowan AhmadNo ratings yet
- Natural Climates Problem (Flood, Bangladesh Perspective) )Document7 pagesNatural Climates Problem (Flood, Bangladesh Perspective) )Radowan AhmadNo ratings yet
- Natural Ways of Reducing BPDocument25 pagesNatural Ways of Reducing BPRadowan AhmadNo ratings yet
- Anatomy of The SkinDocument33 pagesAnatomy of The SkinRadowan AhmadNo ratings yet
- Pellet and PelletizationDocument13 pagesPellet and PelletizationRadowan Ahmad100% (2)
- Applications of ChromatographyDocument11 pagesApplications of ChromatographyRadowan Ahmad92% (24)
- Bio Transforming EnzymesDocument13 pagesBio Transforming EnzymesRadowan AhmadNo ratings yet
- Code of Ethics For PharmacistsDocument9 pagesCode of Ethics For PharmacistsRadowan AhmadNo ratings yet
- Application of IR (Infra-Red) SpectrosDocument8 pagesApplication of IR (Infra-Red) SpectrosRadowan Ahmad100% (1)
- OmeprazoleDocument14 pagesOmeprazoleRadowan Ahmad0% (1)
- Science Behind Global WarmingDocument13 pagesScience Behind Global WarmingRadowan AhmadNo ratings yet
- GPCRs (G-Protein Coupled Receptor)Document25 pagesGPCRs (G-Protein Coupled Receptor)Radowan AhmadNo ratings yet
- NucleusDocument3 pagesNucleusRadowan AhmadNo ratings yet
- Acids and BasesDocument6 pagesAcids and BasesRadowan AhmadNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Leprosy & Pregnancy: DR Y Sri HarshaDocument53 pagesLeprosy & Pregnancy: DR Y Sri HarshaBhawna Joshi100% (1)
- MycetomaDocument16 pagesMycetomapedrixon123No ratings yet
- 200+ Correct Solved BCQS Pharmacology 6th Semester MBBS LUMHSDocument61 pages200+ Correct Solved BCQS Pharmacology 6th Semester MBBS LUMHSSaqib MustafaNo ratings yet
- Pharmacology QuizDocument33 pagesPharmacology QuizWardah KhanNo ratings yet
- Islam S, Rahman F, Saurab K M, Ahmed J, Kamal SMM, Noor RDocument9 pagesIslam S, Rahman F, Saurab K M, Ahmed J, Kamal SMM, Noor RLUIS ALBERTO DE LA HOZ BARRIENTOSNo ratings yet
- Anti TBDocument68 pagesAnti TBGunjan YadavNo ratings yet
- The Penile Implant For Erectile DysfunctionDocument12 pagesThe Penile Implant For Erectile Dysfunctiongigi1123100% (1)
- Central Nervous System: Drug of Choices Notes - Kent Andrei Paelma Bsn-2FDocument22 pagesCentral Nervous System: Drug of Choices Notes - Kent Andrei Paelma Bsn-2FOfficially RandomNo ratings yet
- Drug Study HRZEDocument4 pagesDrug Study HRZEChristine Gold Apduhan AguilarNo ratings yet
- Metabolism: Dr. Muslim Suardi, Msi., AptDocument28 pagesMetabolism: Dr. Muslim Suardi, Msi., AptNisha AnggiaNo ratings yet
- Notes - Lec 20 - Antimycobacterial AgentsDocument14 pagesNotes - Lec 20 - Antimycobacterial AgentsChesmar MacapalaNo ratings yet
- Intravenous Antibiotics Diagnostic Tests Urinalysis Sputum CultureDocument18 pagesIntravenous Antibiotics Diagnostic Tests Urinalysis Sputum CultureJennifer ChuaNo ratings yet
- Anti-TB Drug RegimensDocument8 pagesAnti-TB Drug Regimensbo gum parkNo ratings yet
- 50 Item Pharmacology Exam With Answers and RationaleDocument17 pages50 Item Pharmacology Exam With Answers and Rationalebibot189% (18)
- ChemotherapyDocument11 pagesChemotherapyNedaAbdullahNo ratings yet
- Case Presentation - Pedia Ward Wing 2Document74 pagesCase Presentation - Pedia Ward Wing 2Rijane Tabonoc OmlangNo ratings yet
- LPD - Myrin P Forte (Pakistan)Document17 pagesLPD - Myrin P Forte (Pakistan)Azeem Abbas0% (1)
- Effect Centella Anti TB Drugs Vol3 - Issue5 - 02Document6 pagesEffect Centella Anti TB Drugs Vol3 - Issue5 - 02Kiky HaryantariNo ratings yet
- Microbiology at A GlanceDocument126 pagesMicrobiology at A GlanceMuhammad UsmanNo ratings yet
- Mahon CompileDocument13 pagesMahon CompileSheinor Fae GalzoteNo ratings yet
- Truenat MTB RIF DX Packinsert V04Document4 pagesTruenat MTB RIF DX Packinsert V04yousra zeidanNo ratings yet
- Antituberculous DrugDocument29 pagesAntituberculous DrugMalueth AnguiNo ratings yet
- Clinical Trials For Tuberculosis in India - Soumya SwaminathanDocument53 pagesClinical Trials For Tuberculosis in India - Soumya SwaminathanShailly GuptaNo ratings yet
- What Are AntibioticsDocument31 pagesWhat Are Antibiotics1211988610No ratings yet
- Primary Complex in ChildrenDocument1 pagePrimary Complex in ChildrenMae Novelle EspinosaNo ratings yet
- 7610 (24) Antimicrobial Drugs I (Antibiotics) - UpdatedDocument59 pages7610 (24) Antimicrobial Drugs I (Antibiotics) - UpdatedAli AlhayaliNo ratings yet
- LEPROSYDocument55 pagesLEPROSYGeraldine Marie SalvoNo ratings yet
- Levenson MCQDocument55 pagesLevenson MCQZainab Hasan100% (1)
- List of AntibioticsDocument9 pagesList of Antibioticsdesi_mNo ratings yet
- Warren Clinical Bacteriology MCQs + AnsDocument21 pagesWarren Clinical Bacteriology MCQs + Ansponocet247No ratings yet