Professional Documents
Culture Documents
2011 - Practical Guide Insulin Therapy
Uploaded by
theva_thyOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2011 - Practical Guide Insulin Therapy
Uploaded by
theva_thyCopyright:
Available Formats
Insulin Therapy
Practical guide to
in Type 2 Diabetes Mellitus
Ministry of Health, Malaysia 2010 First published March 2011 Perkhidmatan Diabetes dan Endokrinologi Kementerian Kesihatan Malaysia
Quick Reference For Health Care Providers
Bedtime Pre X
KEY MESSAGES
1. 2. Dinner Pre Post X Following diagnosis, progressive insulin deficiency combined with insulin resistance results in worsening glycaemic control and failure of oral anti-diabetic therapy. Insulin therapy should be initiated early when HbA1c is persistently above 8% despite optimal doses of oral anti-diabetic therapy. X The insulin regimen and insulin doses initiated should be individualised, based on the patients blood glucose profile, lifestyle factors and patients preferences. Metformin, an insulin sensitizer, should be continued at optimal doses following initiation of insulin therapy unless contraindications or intolerance exist. Self monitoring of blood glucose along with simple patient-directed dose adjustments enable gradual, safe and prompt insulin dose optimization. Glycaemic targets need to be individualised based on patients risk of hypoglycaemia, presence of complications and co-morbidities. Pancreatic beta cell dysfunction begins many years prior to diagnosis of Type 2 diabetes X
Pre-bed intermediate/long-acting insulin or pre-dinner premixed X X
Pre-lunch rapid-acting or pre-breakfast premixed insulin. X X X Lunch Post X Pre X X Recommended timing of SMBG in different Insulin Regimens Breakfast Pre Post X X X X X X X
Pre-lunch short-acting or pre-breakfast premixed insulin.
Pre-breakfast rapid-acting or premixed insulin analogue.
3. 4.
5.
6.
7.
9.
SMBG in Premixed Regimen
SMBG and Insulin Titratuion
To Control
2-hours Post-breakfast BG
Pre-mixed Analogues TDS
Basal bolus (short-acting)
Basal bolus (rapid-acting)
Pre-mixed Analogues BD
10. Continuous patient education and support is a key element for optimal treatment adherence, patient empowerment and successful insulin therapy.
SMBG in basal/basal-bolus regimen
Minimizing both hypoglycemia and weight gain are important additional treatment targets for patients with Type 2 diabetes requiring insulin therapy.
TARGETS AND MONITORING
8.
Insulin regimens may need to be changed or intensified with time if glycaemic targets are unmet despite dose optimization.
Basal only
The development of this quick reference guide was supported by an educational grant from sanofi-aventis
Pre-dinner BG
Pre-lunch BG
SOURCES OF FUNDING
Post-dinner/Pre-bed BG Pre-mixed Human BD Pre Breakfast BG
2 hours Post-lunch BG
Pre-dinner rapid-acting or pre-dinner premixed insulin. X X X X
Pre-breakfast short-acting or premixed insulin.
Adjust
Intensification from Premixed Regimen to Basal Bolus Regimen PREMIXED INSULIN BD or TDS (Insulin analogue) FPG / premeals > 6 mmol/L HbA1c > 6.5 7% Switch to BASAL BOLUS REGIMEN Starting dose 0.5units/kg/day or total dose transfer Split dose 50:50 for basal and prandial insulin Divide prandial doses into 3 main meals Fix FPG < 6mmol/L using basal insulin Titrate bolus dose once / twice a week to achieve FPG and preprandial goal < 6mmol/L Stop SU, continue metformin Intensification from Prandial Regimen to Basal Bolus Regimen PRANDIAL TDS (Optimised prandial doses) FPG > 6 mmol/L HbA1c > 6.5 8% Addition of BASAL INSULIN BASAL BOLUS REGIMEN 10 units or 0.2U / kg at pre-dinner Monitor FPG , target 4-6 mmol/L Adjust basal insulin doses after 3 consecutive BG values obtained (every 3 7 days) - < 4 mmol/L ( > 1 value ) reduce dose by 2 units - 4-6 mmol/L ( all values ) maintain current dose - > 6 mmol/L ( >1 value, no hypos ) increase by 2 units
INSUlIN PREPARATIONS AvAIlAblE IN MAlAYSIA AND THEIR PHARMACOKINETIC PROFIlES
Brand (Generic) Name
a) Short-acting, regular - Actrapid* - Humulin R* b) Rapid-acting analogue - Novorapid (Aspart)* - Humalog (Lispro)* - Apidra (Glulisine) c) Intermediate-acting, NPH - Insulatard* - Humulin N* d) Long-acting analogue - Glargine* - Detemir* e) Premixed human (30% regular insulin+70% NPH) - Mixtard 30* - Humulin 30/70* f) Premixed analogue - NovoMix 30 - Humalog Mix 25
* Available at Ministry of Health, Malaysia.
Onset
30 min 30 min 10-20 min 0-15 min 5-15 min 1.5 Hr 1 Hr 2-4 Hr 1 Hr 30 min 30 min 10-20 min 0-15 min
Peak (Hr)
1-3 2-4 1-3 1 1-2 4-12 4-10 peakless peakless dual dual dual dual
Duration (Hr)
8 6-8 3-5 3.5-4.5 3-5 18-23 16-18 20-24 17-23 18-23 16-18 18-23 16-18
Timing of insulin
30 mins before meal 5-15 mins before or immediately after meals
Pre-breakfast / Pre-bed
Same time everyday at anytime of the day 30-60 mins before meals 5-15 mins before meals
INSUlIN REGIMENS AND FREQUENCY OF INjECTIONS PER DAY
No. of injections per day
1
Insulin regimen
BASAL BASAL PREMIXED OD BASAL PREMIXED BD BASAL-PLUS (1) BASAL-PLUS (2) PRANDIAL PREMIXED TDS PREMIXED-PLUS PREMIXED-PLUS BASAL-BOLUS BASAL-BOLUS
Type of insulin and timing
Intermediate acting (NPH) insulin pre-bed Long-acting analogue once daily Premixed/ premixed analogue pre-dinner Intermediate acting (NPH) pre-breakfast and pre-dinner Premixed insulin pre-breakfast and pre-dinner Basal insulin once daily + 1 prandial insulin Basal insulin once daily + 2 prandial insulin Prandial insulin pre-breakfast, pre-lunch and pre-dinner Premixed analogue pre-breakfast, pre-lunch and pre-dinner Premixed insulin pre-breakfast, pre-dinner + 1 prandial insulin pre-lunch
Prandial insulin pre-breakfast and pre-lunch + premixed insulin pre-dinner Basal insulin once daily + prandial insulin pre-breakfast, pre-lunch and pre-dinner
4 5
Intermediate acting (NPH) insulin pre-breakfast and pre-dinner + prandial insulin pre-breakfast, pre-lunch and pre-dinner
INSUlIN THERAPY 3 STAGE PROCESS INITIATION
Starting insulin
Strat requires selection of appropriate insulin regimen, insulin type and starting dose.
OPTIMISATION
Dose titration to ensure maximum benefit from prescribed treatment
Dose should be adjusted every 3-7 days
INTENSIFICATION
Modification of an insulin regimen to acieve glycemic control
Requires switching to more intensive regimens for better glycemic control
Intensification of Premixed Regimen to Premix Plus
PREMIXED OD (pre-dinner) or BD
PREMIXED ONCE DAILY (pre-dinner) FPG 4-6 mmol/L, pre-lunch and pre-dinner > 6mmol/L Add PRANDIAL INSULIN (at morning and midday meal) PREMIXED TWICE DAILY (pre-breakfast, pre-dinner) Pre-dinner > 6 mmol/L Add PRANDIAL INSULIN (at midday meal)
Add prandial insulin 6 units or 0.1unit/kg Titrate to next prandial BG target daily If subsequent pre-meal BG is - < 4 mmol/L ( > 1 value ) reduce dose by 2 units - 4-6 mmol/L ( all values ) maintain current dose - > 6 mmol/L ( >1 value, no hypos ) increase by 2 units
Intensification from Premixed Regimen
PREMIXED OD PREMIXED BD
PREMIXED BD PLUS PRELUNCH PRANDIAL PREMIXED TDS (FOR ANALOGUES) BASAL BOLUS
Intensification of Premixed Regimen
PREMIXED OD (pre-dinner) or BD
FPG and / or pre-dinner 4-6 mmol/L HbA1c > 6.5 8% FPG and / or pre-dinner > 6 mmol/L Titrate Premix OD or BD to achieve FPG and / or predinner < 6mmol/L
SWITCH TO PREMIXED BD OR TDS (analogues only) DAILY (OD) TWICE DAILY (BD) Starting dose 0.3units/kg/day or total dose transfer Split the dose 50:50 pre-breakfast and pre-dinner Titrate insulin dose to achieve FPG and pre-dinner<6mmol/L TWICE DAILY (BD) THREE TIMES DAILY (TDS) Add 6 units or 10% total daily dose at lunch Titrate dose once or twice a week to next pre prandial goal < 6mmol/L Down titrate morning dose ( 2 4 units ) may be needed after adding lunch dose Continue metformin Consider premixed analogues if hypos
SUMMARY OF TREATMENT AlGORITHM
Newly diagnosed DM & Type 2 DM Symptomatic (osmotic symptoms) regardless HbA1c or FBS HbA1c > 10% or FPG > 13 mmol/L Type 2 DM on maximal OADs (single/double/triple) HbA1c > 8%
Glycemic abnormality? FPG, SMBG Normal Fasting / prebreakfast BG High daytime BG High Fasting / prebreakfast BG Normal daytime BG Start PREMIXED OD (predinner) Optimise dose PREMIXED TDS* (premeals) Optimise dose High Fasting / prebreakfast BG High daytime BG Start PREMIXED BD (prebreakfast & predinner) Optimise dose Start BASAL BOLUS (premeals, bedtime) Optimise dose
INITIATE & OPTIMISE
Start PRANDIAL only (usually TDS premeals) Optimise dose Add basal insulin Sequential addition of prandial insulin
Start BASAL only (bedtime) Optimise dose Add 3 prandial insulin
INTENSIFY
BASAL PLUS (premeal and bedtime)
Optimise dose
PREMIXED BD PLUS PRANDIAL (prelunch) Optimise dose
BASAL BOLUS (prandial insulin at premeals, basal insulin at bedtime) Optimise dose
* refers to insulin analogues only
Note: 1. Metformin should be continued while on insulin therapy unless contraindicated or intolerant 2. Sulphonylureas / Meglitinides should be withdrawn once prandial insulin is used regularly with meals 3. Insulin dose should be optimized prior to switching / intensifying regimens
INSUlIN INITIATION AND OPTIMISATION
Insulin Regimen Starting Dose
10 units or 0.2U/kg at bedtime (0.1 units / kg if higher risk for hypos) Once daily: 10 units or 0.2U/kg at pre-dinner Twice daily: 10 units or 0.2U/ kg at pre-breakfast and predinner (0.1units/kg if higher risk for hypos)
Dose Optimisation Adjust insulin doses after 3 consecutive BG values obtained (every 3 7 days) Refer to (*) Adjust insulin doses after 3 consecutive BG values obtained (every 3 7 days) Refer to (*)
Pre-breakfast BG determine pre-dinner premixed dose adjustment Pre-dinner BG determine pre-breakfast premixed dose adjustment
Optimal Dose 0.2 0.3 units/kg in lean patients 0.4 0.5 units/kg in most patients Up to 0.7 units/kg in obese patients Total daily dose of 0.5 1.0 units/kg in most patients (Maybe more than 1.0 units/kg/day in obese, insulin resistant patients)
Basal
Premixed
Prandial
6 units or 0.1units/kg for each meal with short-acting or rapid-acting analogue.
Adjust insulin doses after 3 consecutive BG values obtained (every 3 7 days) Refer to (*)
Adjust the dose of prandial insulin of the preceding meal (eg: if pre lunch BG is high, adjust pre-breakfast prandial insulin)
Prandial dose for each meal will vary according to carbohydrate content and amount. Dose should ideally not exceed 0.5U/kg/dose. Generally basal insulin would contribute 50% of total daily insulin dose and prandial insulin would contribute remaining 50% (distributed over three main meals).
Refer to Prandial Section & Basal Section
Basal Bolus
Prandial Insulin: 6 units or 0.1U/kg before each meal Basal insulin: 10 units or 0.2U/kg at bedtime
Refer to Prandial Section Refer to Basal Section Aim for normal pre-breakfast BG first by adjusting the dose of bed-time basal insulin before adjusting the prandial (bolus) insulin dose.
(*) - < 4 mmol/L (> 1 value) reduce dose by 2 units - 4-6 mmol/L (all values) maintain current dose - > 6 mmol/L (>1 value, no hypos) increase by 2 units
INSUlIN INTENSIFICATION
Intensification from Basal Regimen
BASAL
PREMIXED BD BASAL BOLUS BASAL PLUS (1 / 2 / 3 PRANDIAL)
Note: Optimise Basal Before Intensification Fix Fasting Blood Glucose (FBG) first using basal insulin (dose optimisation) Goal FBG 4 6 mmol/L Consider adding bolus / meal insulin when: Hb A1c > 7% and FBG at goal or basal insulin dose > 0.5U/kg
Intensification from Basal to Premixed Regime
Switch to PREMIXED TWICE DAILY Total dose transfer Split dose 50:50 pre-breakfast : pre-dinner Titrate dose once / twice a week to next preprandial goal Stop SU, continue metformin Consider premixed analogue
Intensification from Basal to Basal Bolus regimen
Add prandial insulin 6 units or 0.1unit/kg at each meal Monitor BG up to 4 times per day Titrate to next pre-meal / bedtime BG target daily If subsequent pre-meals BG are Refer to (*) Stop SU and continue metformin
Intensification from Basal to Basal Plus regimen
Add initial dose of prandial 6 units or 0.1unit/kg at largest meal Titrate to next pre-meal / bedtime BG target daily If subsequent premeals BG are Refer to (*) Discontinue SU on addition of prandial insulin Continue metformin Patients may need to perform SMBG up to 4 times per day If HbA1c > 6.5 - 7% after 3 months despite titrating doses, or prandial doses > 30U per meal, consider: Add 2nd dose of prandial insulin at 6 units or 0.1unit/kg at 2nd largest meal and titrate as before Subsequently may add 3rd dose of prandial insulin if required
If HbA1c > 6.5 - 7% after 3 months despite titrating prandial doses or prandial doses > 30 units per meal, consider: Resume optimisation of basal insulin up to 0.7 U/kg Perform 7- point BG profile
(*) - < 4 mmol/L (> 1 value) reduce dose by 2 units - 4-6 mmol/L (all values) maintain current dose - > 6 mmol/L (>1 value, no hypos) increase by 2 units
You might also like
- Insulin Initiation PPT - PPTX 2Document53 pagesInsulin Initiation PPT - PPTX 2Meno Ali100% (1)
- Terapi Insulin-1Document46 pagesTerapi Insulin-1Yanti MoonNo ratings yet
- Warfarin LeafletDocument2 pagesWarfarin LeafletchampbeeNo ratings yet
- DIET FOR RAMADAN by Guru Mann PDFDocument1 pageDIET FOR RAMADAN by Guru Mann PDFNazmul Islam0% (1)
- 3 - Case Study 2-Insulin For IntensificationDocument30 pages3 - Case Study 2-Insulin For IntensificationBiswojit BeheraNo ratings yet
- CretDocument63 pagesCretMtpa MashoorNo ratings yet
- Clinical Case 1 Diabetic Foot Infection TaskDocument4 pagesClinical Case 1 Diabetic Foot Infection TaskHari EshwaranNo ratings yet
- Log Book GCFM MockDocument135 pagesLog Book GCFM Mocknurul asyikin abdullahNo ratings yet
- Insulin Case Studies AACE 5-20-05Document56 pagesInsulin Case Studies AACE 5-20-05Leanne Shepherd100% (2)
- CFCSDocument77 pagesCFCSNurul NadiahNo ratings yet
- Neonatology Cambridge Pocket ClinicianDocument601 pagesNeonatology Cambridge Pocket Clinicianjuanse1994No ratings yet
- 02.borang Diabetes Clinical Audit MELAYUDocument3 pages02.borang Diabetes Clinical Audit MELAYUnorhaslizaNo ratings yet
- Nutritional AnemiaDocument90 pagesNutritional AnemiaIrham KhairiNo ratings yet
- Diabetes Medication SummaryDocument1 pageDiabetes Medication Summarywoody_2512No ratings yet
- MRCGPDocument2 pagesMRCGPMohammad IslamNo ratings yet
- 99 Topics StudynotesDocument138 pages99 Topics StudynotesM.Dalani100% (1)
- SOSCG 6jul2013 v5Document32 pagesSOSCG 6jul2013 v5Suhazeli Abdullah100% (2)
- Checklistfor 45 Yr OldsDocument1 pageChecklistfor 45 Yr OldsyohaneskoNo ratings yet
- Oedematous Children OSCE Nephrotic NephriticDocument5 pagesOedematous Children OSCE Nephrotic NephriticJJ LimNo ratings yet
- Racgp GuideDocument28 pagesRacgp Guidemyat252100% (1)
- Emedica MRCGP AKT Curriculum ChecklistDocument42 pagesEmedica MRCGP AKT Curriculum ChecklistSana Mustafa100% (1)
- Docslide - Us Family Medicine Shelf Reviewpptx Read OnlyDocument142 pagesDocslide - Us Family Medicine Shelf Reviewpptx Read OnlyDavid DengNo ratings yet
- DiabeticeducationDocument11 pagesDiabeticeducationapi-316157555No ratings yet
- Jaundice 20 PDFDocument54 pagesJaundice 20 PDFHaziq KamardinNo ratings yet
- Basic Tools For Diabetics PowerPoint Templates Standard 2Document8 pagesBasic Tools For Diabetics PowerPoint Templates Standard 2Charm MeelNo ratings yet
- Steps To Becoming A Licensed, Practicing Physician in CanadaDocument10 pagesSteps To Becoming A Licensed, Practicing Physician in CanadaMicheal KhandaniNo ratings yet
- Canadian Screening GuidelinesDocument8 pagesCanadian Screening GuidelinesaayceeNo ratings yet
- RCPI Management of Early Pregnancy MiscarriageDocument24 pagesRCPI Management of Early Pregnancy MiscarriagerazorazNo ratings yet
- Fertility: Meal PlanDocument17 pagesFertility: Meal PlanDwi Ayu KusumawardaniNo ratings yet
- Diabetes Melitus: Makbul M AmanDocument69 pagesDiabetes Melitus: Makbul M AmanDwi YantiNo ratings yet
- 08&09 Oral Hypoglycemics-Level 11Document48 pages08&09 Oral Hypoglycemics-Level 11Usman Ali AkbarNo ratings yet
- Primary Newborn CareDocument93 pagesPrimary Newborn CareZharina VillanuevaNo ratings yet
- Practice Guidelines For Family Physicians Volume 1Document108 pagesPractice Guidelines For Family Physicians Volume 1sdoryna100% (2)
- Identification of CKD: Algorithm ADocument3 pagesIdentification of CKD: Algorithm ArawanNo ratings yet
- Update On Medical Disorders in Pregnancy An Issue of Obstetrics and Gynecology Clinics The Clinics Internal MedicineDocument217 pagesUpdate On Medical Disorders in Pregnancy An Issue of Obstetrics and Gynecology Clinics The Clinics Internal Medicinemeriatmaja100% (1)
- Timely Intensification Using Bolus Insulin Therapy - HimawanDocument50 pagesTimely Intensification Using Bolus Insulin Therapy - HimawanVictoria BrandedBagNo ratings yet
- Rational Laboratory and Diagnostic TestsDocument26 pagesRational Laboratory and Diagnostic TestsCeline dela cruzNo ratings yet
- National Practice SAMP 2018Document57 pagesNational Practice SAMP 2018Kmërgim BinNo ratings yet
- Guidelines To Open A ClinicDocument1 pageGuidelines To Open A ClinicSashi Rajan100% (1)
- CPG Diabetic RetinopathyDocument49 pagesCPG Diabetic RetinopathyRebecca WongNo ratings yet
- CASE Study Insulin InitiationDocument54 pagesCASE Study Insulin InitiationAshraf Shaaban MahfouzNo ratings yet
- Insulin Initiation and MonitoringDocument35 pagesInsulin Initiation and Monitoringeka prasepti darusmanNo ratings yet
- The Basal Insulin/Bolus Insulin ConceptDocument1 pageThe Basal Insulin/Bolus Insulin Conceptocean329No ratings yet
- EInsulin RegiemDocument18 pagesEInsulin RegiemzahrabokerNo ratings yet
- DM OHA and InsulinDocument33 pagesDM OHA and InsulinPraba NanthanNo ratings yet
- DR - Rihab Pediatrics 02.pediatric DM Part TwoDocument7 pagesDR - Rihab Pediatrics 02.pediatric DM Part TwoMujtaba JawadNo ratings yet
- Antenatal Managemennt by DSKDocument14 pagesAntenatal Managemennt by DSKSanthosh Kumar DskNo ratings yet
- Insulin Therapy Guide 2Document3 pagesInsulin Therapy Guide 2AimanRiddleNo ratings yet
- Fit-Diploma 3-2-2024Document57 pagesFit-Diploma 3-2-2024light tweenNo ratings yet
- Basal Bolus InsulinDMT22009Document92 pagesBasal Bolus InsulinDMT22009scribdNo ratings yet
- Diabetes Insulin InitiationDocument12 pagesDiabetes Insulin InitiationSatinder BhallaNo ratings yet
- Management of Gestational DiabetesDocument3 pagesManagement of Gestational DiabetesNazia SalmanNo ratings yet
- 60-2005 - Pregestational Diabetes MellitusDocument11 pages60-2005 - Pregestational Diabetes MellitusGrupo Atlas100% (1)
- GUIDELINES FOR INPATIENT DIABETES MANAGEMENT هااامDocument1 pageGUIDELINES FOR INPATIENT DIABETES MANAGEMENT هااامAbu HuzaifaNo ratings yet
- A Practical Guide To Insulin TherapyDocument42 pagesA Practical Guide To Insulin Therapyseun williams100% (2)
- DiabetesMellitisChap09 SpecialPopulationsDocument12 pagesDiabetesMellitisChap09 SpecialPopulationsarmandoNo ratings yet
- Type 1 Diabetes Mellitus: TreatmentDocument25 pagesType 1 Diabetes Mellitus: TreatmentironNo ratings yet
- Insulin Treatment in DiabetesDocument86 pagesInsulin Treatment in DiabetesAhsan Rauf100% (1)
- Inpatient DM MX in Twenty First CenturyDocument65 pagesInpatient DM MX in Twenty First CenturyTRP TSYONo ratings yet
- Thera L15 PracticalDocument21 pagesThera L15 PracticalFatmaNo ratings yet
- MRCPCH Clinical The Whole Book PDFDocument108 pagesMRCPCH Clinical The Whole Book PDFtheva_thy100% (3)
- Neonatal Hypoglycemia APNECDocument27 pagesNeonatal Hypoglycemia APNECtheva_thyNo ratings yet
- AACE GuidelinesDocument23 pagesAACE GuidelinesHatem GamalNo ratings yet
- NSAIDsDocument37 pagesNSAIDstheva_thyNo ratings yet
- Insulin TherapyDocument76 pagesInsulin TherapyDk YadavNo ratings yet
- Cardiovascular Safety of Anti-Diabetic Drugs - KarklinDocument42 pagesCardiovascular Safety of Anti-Diabetic Drugs - KarklinCharles SaputraNo ratings yet
- Insulin ManagementDocument38 pagesInsulin ManagementMelinda Rose FernandezNo ratings yet
- 2017 05 GC Pocket CardDocument2 pages2017 05 GC Pocket Cardapi-312241089No ratings yet
- List Obat Kronis BpjsDocument6 pagesList Obat Kronis BpjsHelmi AgustianNo ratings yet
- Insulin Therapy: by Dr. Adithya PolavarapuDocument18 pagesInsulin Therapy: by Dr. Adithya Polavarapuadithya polavarapuNo ratings yet
- Rincian Tagihan ObatDocument48 pagesRincian Tagihan Obatferi rotinsuluNo ratings yet
- Basal Bolus InsulinDMT22009Document92 pagesBasal Bolus InsulinDMT22009scribdNo ratings yet
- AAFP Diabetes MedicationsDocument7 pagesAAFP Diabetes MedicationsThaysa LimaNo ratings yet
- Rekap Data Peserta PRB Oktober 2021 Puskesmas SimalingkarDocument119 pagesRekap Data Peserta PRB Oktober 2021 Puskesmas SimalingkarChatryn PasaribuNo ratings yet
- DM AAFP ManagementDocument8 pagesDM AAFP ManagementphilsguNo ratings yet
- Sparsh Gupta 14e-Anti Diabetes MCQDocument12 pagesSparsh Gupta 14e-Anti Diabetes MCQSubodh ChaudhariNo ratings yet
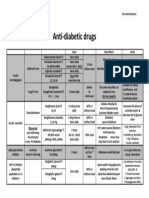
- Anti Diabetic DrugsDocument1 pageAnti Diabetic DrugsWael hadNo ratings yet
- 3-23-22 Sa Gamot Na Abot Kaya, Sakit Makakaya 3Document21 pages3-23-22 Sa Gamot Na Abot Kaya, Sakit Makakaya 3Rachelle Joy G. Bugatan100% (1)
- DM GuidelinesDocument7 pagesDM GuidelinesslojnotakNo ratings yet
- Joslin Diabetes Center Clinical GuideDocument16 pagesJoslin Diabetes Center Clinical GuideNikolaus TalloNo ratings yet
- Insulin CorretionDocument5 pagesInsulin CorretionArshad SyahaliNo ratings yet
- Insulin Initiation GuidanceDocument4 pagesInsulin Initiation GuidanceRahma WatiNo ratings yet
- Metformin: Its Botanical Background: Practical Diabetes International April 2004Document4 pagesMetformin: Its Botanical Background: Practical Diabetes International April 2004made dwi novitasariNo ratings yet
- Wjarr 2022 1252Document9 pagesWjarr 2022 1252Eduardo Luis Flores QuispeNo ratings yet
- Mendez How To Use The Type 2 Diabetes Treatment Algorithm PDFDocument29 pagesMendez How To Use The Type 2 Diabetes Treatment Algorithm PDFUrutoraman TigitNo ratings yet
- Diabetic MedicationsDocument2 pagesDiabetic Medicationsapi-288062111No ratings yet
- Skugor TreatmentofdiabetesmellitusDocument5 pagesSkugor TreatmentofdiabetesmellitusyomiboyNo ratings yet
- Insulin Degludec: Dr. Taufik Hidayat Regional Medical Advisor Novo Nordisk IndonesiaDocument35 pagesInsulin Degludec: Dr. Taufik Hidayat Regional Medical Advisor Novo Nordisk IndonesiaAndi SedaNo ratings yet
- 2022 Insulin Calculations Cheat Sheet ARDocument4 pages2022 Insulin Calculations Cheat Sheet ARGulsama BabarNo ratings yet
- Diabetes Medication ChartDocument21 pagesDiabetes Medication CharttmleNo ratings yet
- ( (Drugs For Diabetes Mellitus) ) PDFDocument7 pages( (Drugs For Diabetes Mellitus) ) PDFMohamedYosefNo ratings yet
- GUIDELINES FOR INPATIENT DIABETES MANAGEMENT هااامDocument1 pageGUIDELINES FOR INPATIENT DIABETES MANAGEMENT هااامAbu HuzaifaNo ratings yet
- Type 1 Type 2 Gestational: Cost of Therapy Patient PerceptionDocument2 pagesType 1 Type 2 Gestational: Cost of Therapy Patient PerceptionPrasanth PrasanthNo ratings yet
- How To Switch Insulin Products - Pharm LetterDocument6 pagesHow To Switch Insulin Products - Pharm LetterAraceli LeonNo ratings yet