Professional Documents
Culture Documents
Selection of Materials Biomedical Application
Uploaded by
sciencystuffOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Selection of Materials Biomedical Application
Uploaded by
sciencystuffCopyright:
Available Formats
CHAPTER 37 SELECTION OF MATERIALS FOR BIOMEDICAL APPLICATIONS
Michele J. Grimm
Co py rig hte dM ate ria l
1 2 INTRODUCTION 1165 3.2 3.3 Biocompatibility Current Material Selection ORTHOPEDIC MATERIALS: TOTAL HIP ARTHROPLASTY 2.1 Function 2.2 Biocompatibility 2.3 Current Material Selection BLOOD-CONTACTING BIOMATERIALS: VASCULAR PROSTHESES 3.1 Function 1166 1167 1174 1178 4 3 5 SUMMARY 1180 1181 BIBLIOGRAPHY
Bioengineering Center Wayne State University Detroit, Michigan
1183 1186
SPACE-FILLING BIOMATERIALS: BREAST IMPLANTS 1188 4.1 Function 1188 4.2 Biocompatibility 1188 4.3 Current Material Selection 1191 1191 1192
INTRODUCTION
Materials have been used for medical implant applications for centuries. Starting even before George Washingtons famous wooden teeth, before the use of coconut shells in the 1800s by South Seas natives to replace missing portions of the skull (Sanan and Haines, 1997), humans have attempted to use materials from biological and inorganic sources to replace diseased or damaged tissues. In fact, some examples of biomaterial implants, particularly in the form of gold and silver, date back to prehistoric times (Sanan and Haines, 1997). These material selections of the past, based more on the availability of materials and anecdotal evidence than scientic method, resulted in varying degrees of success. The development of aseptic surgical technique in the midnineteenth century by Lister provided the basic medical tool needed for the more widespread and successful use of biomedical implants (Park and Lakes, 1992). Since the twentieth century, as knowledge of the biological mechanisms behind the interactions of implanted materials and tissues has increased, the selection of materials for medical implants has been based on progressive improvements and experimental evidence. When selecting a material for use in a medical implant application, two general considerations need to be taken into account: the functional requirements
Handbook of Materials Selection, Edited by Myer Kutz 2002 John Wiley & Sons, Inc., New York ISBN 0-471-35924-6 1165
Copyright 2002 John Wiley & Sons Retrieved from: www.knovel.com
1166
SELECTION OF MATERIALS FOR BIOMEDICAL APPLICATIONS
Co py rig hte dM ate ria l
2 ORTHOPEDIC BIOMATERIALS: TOTAL HIP ARTHROPLASTY
of the implant and how it will interact with the body. The function of the implant includes the physiologic role that it will replace, as well as the length of time that it is designed to fulll that role. The interaction of the body and the implanted material must be examined from two perspectivesthe effect of the biological environment on the material properties and the effect of the material, and any degradation that may occur, on the local and systemic physiology of the body. It is not possible within the scope of this chapter to discuss the optimum choice of materials and the supporting rationale for every medical implant application. This task is made even more difcult by the fact that the development and selection of materials is an ever-changing eld. In light of this fact, the following pages will use three implant examples to serve as the background for a discussion of the considerations in the selection and evaluation of materials for medical implants. Each section will rst be organized around the functional requirements of the implant, with the resulting concerns regarding material tissue interaction being discussed for the materials that would rst meet the functional demands. Geometrical considerations and overall implant design will also play a major role in the success of an implant; however, this chapter will focus on the selection of biomaterials as a discrete step in the design process. The hip (Fig. 1) is one of the most commonly replaced joints, due to the high incidence of both osteoarthritis and osteoporotic hip fracture within the population. As with the other joints in the skeletal system, the hip has two main functions: (1) to transfer load from one bone to another and (2) to allow for motion between the bones. The loads on the hip have been found to vary from 0.5 to 8 times body weight during activities of daily living, including brisk walking (Paul, 1999). The loads can be expected to reach even higher levels during events such as a stumble. The hip is essentially a ball-and-socket joint
Fig. 1 Anatomy of the hip.
Copyright 2002 John Wiley & Sons
Retrieved from: www.knovel.com
ORTHOPEDIC BIOMATERIALS: TOTAL HIP ARTHROPLASTY
1167
Co py rig hte dM ate ria l
2.1 Function Load Support
Fig. 2 Example of total hip implant, including femoral and acetabular components. Copyright 2002 John Wiley & Sons Retrieved from: www.knovel.com
with 6 degrees of freedom constrained by the bony and ligamentous structures of the joint. These functional constraints have generally dened the goals for design of hip implants over the past half-century. The total joint replacement for the hip is divided into three components: the femoral stem and femoral head, which may be integrated or modular, and the acetabular cup (Fig. 2). The combination of the femoral head and the acetabular cup provide the bearing surface for the joint. The femoral stem transfers the load to the femur and provides resistance to the bending moment caused by the anatomy of the joint. Total hip replacement began in the 1930s, with stainless steel used for both the acetabular cup and the femoral head, which was bolted onto the natural femoral neck. In the 1950s, the general design of the implant was expanded by McKee to include the stemmed femoral component familiar today. In 1959, Charnley introduced a plastic acetabular component, which articulated with the metallic femoral component. This idea for low-friction arthroplasty remains the basis for the predominant implant designs used today (Swanson, 1977).
Because of its primary role in mechanical support, the stem of a femoral prosthesis can realistically be manufactured from a metal, a ceramic, or a composite material. For this discussion, composite materials will not be included, as they have not yet been utilized in commercially available total joint replacements (they are available for bone plate applications). However, as development of
1168
SELECTION OF MATERIALS FOR BIOMEDICAL APPLICATIONS
composite materials for this application continues, they must meet the same requirements to be discussed for ceramic and metallic materials. Strength. The rst property to be considered for a load-bearing implant is its mechanical strength. The loading of the femur is dynamic and, while estimated to range up to 8 times body weight, is difcult to determine precisely. Therefore, as the implant will be loaded in essentially the same way as the natural bone, it is reasonable to assume that a material that will provide the same or greater load-bearing capacity as bone will meet the necessary mechanical requirements. The mechanical properties of cortical bone (Table 1) form the lower limit for properties of materials to be selected for the femoral stem. If the neck of the femoral stem is designed to be longer than the normal range of femoral neck lengths [approximately 9 cm, from the edge of the greater trochanter to the apex of the femoral head (Center et al., 1998)], then the increased bending moment in this region should also be considered. The primary mode or modes of loading that will be seen for a particular implant application will also be important factors in the determination of whether a material meets the constraints regarding mechanical strength. The hip will be loaded primarily in bending and compression, due to its unique geometry. Tensile and shear strength of any replacement material therefore become of great importance. In addition to the yield or ultimate strength of an implant material, the fatigue strength is also important for structures that will be cyclically loaded over an extended period of time. At the current time, hip replacements are designed to last for approximately 20 years. As an individual typically loads and unloads the joint thousands of times per day during normal daily activities, fatigueinduced failure at this location is of paramount concern. In contrast to the materials that might be chosen to replace the original tissue, healthy bone has the capacity to repair any microfractures that may occur through continuous cycling. This normal remodeling function helps to eliminate the occurrence of fatigue fractures in normal bone. Based on the cyclic loading that a material is likely to undergo when implanted in the body, it is reasonable when evaluating selections to compare the endurance limit of the materials under consideration to the experimentally determined strength values for bone. One further complication in this process, however, is that materials will fatigue differently in a typical, air-based laboratory environment than they will in the ionic soup of the human body. Because of this, it is important to measure the fatigue performance of materials in an environment that closely mimics that of the implant locationincluding the ionic composition, temperature, and pH. Substantial work has been conducted
Co py rig hte dM ate ria l
Table 1 Bone Representative Properties of Cortical
Compressive strength (MPa) Tensile strength (MPa) Shear strength (MPa)
131224 longitudinal 106133 transverse 80172 longitudinal 5156 transverse 5370
Source: Data from Cowin (1989).
Copyright 2002 John Wiley & Sons
Retrieved from: www.knovel.com
ORTHOPEDIC BIOMATERIALS: TOTAL HIP ARTHROPLASTY
1169
Co py rig hte dM ate ria l
Copyright 2002 John Wiley & Sons Retrieved from: www.knovel.com
to develop testing methodologies for this purpose, and many have been compiled by the American Society for Testing and Materials (ASTM), the International Standards Organization (ISO), and other bodies interested in standardization. For instance ISO-7206 (1989) discusses many aspects of testing for partial and total hip replacements. Thus, individuals who are working to design new materials for biomedical implants do not need to reinvent the wheel when it comes to evaluation tests. Finally, when the mechanical strength of a potential implant material is evaluated, the failure behavior of the material must be taken into consideration. The ability of the material to absorb energy during potential abnormal loading events, such as a fall or a jump, will affect its overall, long-term performance. Metals are signicantly less brittle than ceramics, and as a result are less likely to fail during a high-energy or high-rate loading event. Ceramics are also more susceptible to failure in bending than metals, due to their relatively low tensile strength and low resistance to crack propagation. These factors do not eliminate ceramics from consideration for orthopedic implants; however, an understanding of a materials behavior under a range of loading modes and rates is needed before a nal determination of its suitability for a particular application can be determined. Stress Shielding. In bony prosthetics, exceeding the minimum strength requirements of the application is not the only mechanical behavior of concern. Bone is a living tissue and not merely a structural material. As a result, bone changes in response to its loading environment. In 1892, Wolff rst noted that the pattern of the trabecular bone in the head and neck of the femur was similar to the stress trajectories of a Culmann crane, an engineering structure with a similar loading pattern (Wolff, 1892). Based on this observation, Wolff hypothesized that bone develops and remodels in response to the load that it experiences. Over 100 years later, Wolffs law is still the governing principle behind our understanding of how bone behaves in response to stress. In general terms, bone requires a minimal, time-averaged stress in order to maintain its mass. If the stress falls below this threshold level, bone will be lost. If the stress increases beyond this threshold, bone will be added until the stress experienced returns to its desired level. This is evidenced by the loss of bone seen in individuals after sustained bed rest or in astronauts after missions spent in low-gravity environments. As a result of this characteristic property, bone is susceptible to a phenomenon termed stress shielding. This occurs when the stress in bone is reduced below its maintenance threshold as a result of the mechanical role of an implanted structure. Figure 3a shows the radiograph of a femur in which signicant bone loss has occurred around the proximal end of the implant, with stress shielding being one of the underlying causes. Bone loss such as this is one of the leading reasons for implant failure and revision. The formation of a callus at the distal end of the implant, as also shown in Fig. 3b, is additional evidence of the response of bone to its stress environment. In many hip implant designs, while the stress in the bone in the proximal region of the implant is reduced, an increase in stress is seen in the distal region that results in the deposition of additional bone.
1170
SELECTION OF MATERIALS FOR BIOMEDICAL APPLICATIONS
Co py rig hte dM ate ria l
Fig. 3 X-rays of hip implants showing changes in bone mass resulting from stress shielding around an implant. (A) Circled areas indicate regions of signicant bone loss in the proximal region of the femur. The arrow indicates the area where the collar of the prosthesis is no longer in contact with bone on the medial side. (B) Proximal bone loss (indicated in the circled regions at the edge of the prosthesis) is accompanied by increased bone deposition (indicated by the rectangle) in the distal region of the implant. The latter phenomenon is caused by increased stress transfer in this region.
In any loaded structure consisting of two or more materials, the distribution of stress and strain between the component materials will depend on their geometric arrangement and relative material properties. For a structure in which the materials are in parallel with the loading axis and where the materials are sufciently well bondedsuch as a well-xed femoral implantit can be assumed that the materials deform to the same extent and therefore experience the same strain. In this isostrain condition, the stress in one of the components of a two-phase composite can be calculated from the equation: E1P1 E1A1 E2 A2 (1)
where P is the total load on the structure, and E and A are the Youngs modulus and cross-sectional area of each of the components. Thus, the fraction of the load carried by each material, and the resulting stress, is related to its Youngs modulus and cross-sectional area in relation to those of the other components of the composite structure. The stiffer materials in the composite will carry a greater proportion of the load per unit cross-sectional area. As stated above, the important parameter for maintenance of bone is the stress that it experiences compared to a threshold value. If bone in its natural state is compared to bone with an implant, the effect of this intervention on the stress
Copyright 2002 John Wiley & Sons
Retrieved from: www.knovel.com
ORTHOPEDIC BIOMATERIALS: TOTAL HIP ARTHROPLASTY
1171
in the bone, and therefore its remodeling response, can be estimated. For a femoral implant, or a bone plate as another example, the implant is in parallel with the bone tissue with respect to the main loading axis. Therefore, Eq. 1 can be used to estimate the effect of the implant on the stress in the bone. The applied load can be assumed to be the same pre- and postimplant, which yields the following equations for the stress in the bone in the two congurations:
Co py rig hte dM ate ria l
Preimplant (Eimplant 0; Aimplant 0)
bone
EboneP Ebone Abone
P Abone
(2a)
Postimplant
bone
EboneP Ebone Abone Eimplant Aimplant
(2b)
Thus, the stress in the bone is reduced by the inclusion of the implant, with the amount of the reduction dependent on the modulus and area of the implant. Implants with a higher modulus and a larger cross-sectional area will shield the bone from a greater proportion of its normal, physiological stress, resulting in bone loss according to Wolffs law.
Joint Motion
Friction. Frictional forces between the articulating surfaces of a joint have two primary effects: (1) to increase the muscle force required to overcome the internal friction and allow motion to occur and (2) to increase the torque experienced by the implant and/or bone, such as at the location of the femoral neck. Large internal bending moments due to high frictional forces may lead to failure of the implant, and therefore should be avoided. The natural joint, with its cartilage bearing surfaces and synovial uid lubrication, possesses a remarkably low coefcient of friction that minimizes the tangential and bending forces at the joint. It has been recognized that, in an articial hip, the coefcient of friction between the femoral head and the acetabular cup must be minimized in order to most closely approximate the normal physiology. While no material combinations currently provide a coefcient of friction of the level seen naturally, a number of options have been identied that provide sufciently low friction forces in the joint. Table 2 provides the coefcients of friction of some commonly paired materials used in hip replacement in comparison to the natural state. Once implanted, the joint will be lubricated with physiologic or synovial uid, although it will no longer be contained within the original joint capsule. Therefore, the friction values provided were measured using physiological uid or bovine albumin as a lubricating material. Alumina has a relatively high surface tension, allowing it to develop a good lubrication lm that minimizes friction in vivo (Ravaglioli and Krajewsk, 1992). As friction forces are proportional to the coefcient of friction and the normal force between the contact surfaces, the loading conguration of an implant will also determine the forces that inuence joint motion and applied bending mo-
Copyright 2002 John Wiley & Sons
Retrieved from: www.knovel.com
1172
SELECTION OF MATERIALS FOR BIOMEDICAL APPLICATIONS
Table 2 Coefcient of Friction for Sample Material Combinations Used in Total Hip Replacementa Material Combination Coefcient of Friction
Co py rig hte dM ate ria l
a UHMWPE, ultra-high-molecular-weight polyethylene; CoCr, cobaltchromium alloy. Source: Data from Park and Lakes (1992), Streicher et al. (1992).
Cartilage / cartilage CoCr / UHMWPE Zirconia / UHMWPE Alumina / UHMWPE CoCr / CoCr Alumina / alumina
0.002 0.094 0.090.11 0.080.12 0.12 0.050.1
ments. Therefore, materials that will provide a sufciently reduced friction environment for a relatively low force location, such as the wrist, can result in a friction force in the hip that may cause implant failure to occur or cannot be adequately overcome by normal muscle forces to allow unhindered motion. Thus, once again, the specic application of an implant must be considered when selecting materialsgeneralized assumptions and choices do not necessarily produce the optimum selection.
Wear. Whenever contact surfaces and motion are combined, material wear must be taken into consideration. Wear is the process whereby one object, through motion, removes material from the surface of the contacting object. Generally, the harder material will cause wear to occur on the softer material. Three basic types of wear can occur: abrasive wear, adhesive wear, and thirdbody wear. Abrasive wear exists when a hard material, such as a metal, moves cyclically against a soft material, such as a polymer. Adhesive wear involves the sliding motion of two similar materials, where molecular bonds can be formed at the interface of the structures. In rough materials, the surfaces appear as a series of peaks and valleys. The two articulating surfaces typically come into contact at the peaks of the surface roughness, concentrating the contact load over a much smaller area and increasing the contact stress. As the molecular bonds between the objects are broken through motion, they also break off particles of the underlying material. Third-body wear includes the effect of particles between the articulating surfaces that tend to accelerate wear. The amount of wear that occurs between two surfaces will depend on several factors: (1) the hardness of the two materials (p), (2) the normal force at the surface (Fn), (3) the Archard coefcient for the pair of materials (k), (4) the area of contact between the surfaces during the cyclic motion, and (5) the number of cycles expected. Archards coefcient is similar in concept to the coefcient of friction and describes the degree to which a normal force at the surface is translated into a wear-producing force. A harder material will always sustain less wear when in motion against a given surface than a softer material. As two materials sweep out a larger surface of contact for each cycle of motion, there will be a greater fraction of the surface area experiencing wear, thus resulting
Copyright 2002 John Wiley & Sons
Retrieved from: www.knovel.com
ORTHOPEDIC BIOMATERIALS: TOTAL HIP ARTHROPLASTY
1173
in an increase in the overall rate of wear. And, with little explanation required, if a given amount of wear occurs per cycle, then an increased number of cycles will result in a greater total amount of wear. The wear rate, or volume of wear particles produced (V), can be approximated for adhesive wear by the equation:
Co py rig hte dM ate ria l
V kFn x 3p
Fig. 4 Illustration of the development of a new socket within an acetabular cup due to excessive wear. Copyright 2002 John Wiley & Sons Retrieved from: www.knovel.com
(3)
where x is the total sliding distance between the surfaces (Black, 1999). The total sliding distance can be determined for a single cycle, a dened period of time (e.g., one hour), or estimated for the entire life of the implant, thus allowing for the calculation of a rate for wear particle production. Wear can be exacerbated through corrosion or fatigue processes, indicating that in vivo wear rates may differ from those measured in laboratory. The occurrence of wear in an implant may affect both its mechanical function and the response of the body to the implant. The former will be discussed here, while the effect of wear debris will be described in the discussion of biocompatibility. As wear occurs on one or both of the opposing surfaces of an articulating joint, the shape of the implant may change as material is removed. This is especially evident when signicant wear occurs in a polymeric acetabular cup within a total hip replacement. Figure 4 shows how signicant wear can result in the creation of a new socket, typically with a reduced diameter. This change in the conguration of the acetabulum can affect the range of motion of the hip as well as whether any joint impingement occurs. As the socket deepens, the femur will shift upward, which will increase the laxity of some of the ligaments and tendons, thus affecting overall joint performance.
1174
SELECTION OF MATERIALS FOR BIOMEDICAL APPLICATIONS
2.2
Biocompatibility
Co py rig hte dM ate ria l
Corrosion
Once a material is selected for an implant application based on the functional requirements, it must be evaluated in terms of materialbody interactions. An implant material will react chemically with the local environment, with the type of reaction dependent on the class of material. Metals are susceptible to corrosion, polymers experience leaching and absorption, while ceramics are generally considered to be chemically inertunless designed to be bioactive. The effects of chemical degradation may affect both the tissue and the material itself, especially its mechanical properties, and so both aspects must be considered. In addition, degradation products can affect the physiology locally, at a remote location, or systemically.
Metallic materials are susceptible to corrosion, particularly in the ionic uid environment of the body. To assess the corrosion potential of a metal, it is necessary to examine the half-cell potential of that metalwhich will act as an anode when it releases electronswith respect to the material acting as the cathode. This cathode may be another metal or the ionic environment itself. An electrochemical series lists the half-cell potentials of metals in order from the most noble (or cathodic) to the most anodic. When two materials are in contact with each other directly or through an ionic solution, the metal listed rst in the list will act as the cathode while the other will behave as the anode. Practical electrochemical series typically relate half-cell potentials as measured in an application-specic environment and may include alloys. This contrasts with ideal series, which list only pure metals as measured with respect to a hydrogen half cell reaction. The ideal series approximates the behavior of metals in pure water. Table 3 shows the half-cell potentials of common metals as measured in an ideal
Ideal and Practical Electrochemical Series for Common Metalsa Half-Cell Potential (mV) of Ideal Series with Respect to H / H Half-cell
Table 3
Ideal Series
Practical Series
Cathodic
Gold Platinum Silver Copper Lead Tin Nickel Iron Chromium Aluminum Titanium Magnesium
1.50 0.86 0.80 0.47 0.12 0.14 0.23 0.44 0.56 1.70 2.00 2.40
Platinum Gold Passivated stainless steel Titanium Silver Unpassivated stainless steel Copper Tin Lead Wrought iron Aluminum Magnesium
Anodic
a The half-cell potentials listed are for the ideal series and are with respect to a H / H half-cell. Source: Data from Black (1999), Park and Lakes (1992).
Copyright 2002 John Wiley & Sons
Retrieved from: www.knovel.com
ORTHOPEDIC BIOMATERIALS: TOTAL HIP ARTHROPLASTY
1175
Co py rig hte dM ate ria l
Copyright 2002 John Wiley & Sons Retrieved from: www.knovel.com
electrochemical series, as well as the qualitative series of metals in a saltwater solution. This latter series reasonably approximates what would be found in the body, where sodium chloride is a major constituent of the ionic soup. The low half-cell potentials of gold and platinum are a result of their essential inertness. For other materials, their resistance to corrosion may be due to the formation of a protective oxide layer on the objects surface. A second way to determine how a metallic material is likely to behave in vivo from a chemical standpoint is to examine Pourbaix diagrams that have been developed based on theoretical chemical relationships. These curves, such as the one shown in Fig. 5, describe the expected corrosive behavior of materials as a function of pH and the surrounding electrical potential. By determining the expected environment at an implant site, it is possible to predict which materials are likely to meet the outlined requirements for implantation. In regions of buffered pH, which are common within the human body, the partial pressures of O2 and H2 can be used to estimate the electrical potential at the site (Black, 1999). Three general behaviors can exist for a metallic material in an ionic environment: corrosion, passivation, or immunity. Corrosion is the chemical reaction in which a metal is oxidized, producing metallic ions within the uid environment. As a metal corrodes, it can effect both the overall implant propertiesresulting in premature failureand the body. In the latter case, the ions produced through the oxidation reaction can interfere with the normal physiologic process of the body at either a local or a systemic level. It cannot be assumed that the ions produced will have no adverse reaction in the body if they are normally present in trace amounts. For instance, iron, a mineral required for normal red blood cell production, will prove to be toxic at elevated concentrations in the body, causing liver and pancreatic failure (Smith, 1983). Therefore, it is important to select materials that will exist within their passivation or immunity regions in the in vivo environment. Passivation is the creation of a protective, oxide or
Fig. 5 Pourbaix diagram for chromium in aqueous solution of 1 N Cl . The diagram indicates the electrochemical environment of various regions of the body. [From John H. Dumbleton and Jonathan Black, An Introduction to Orthopaedic Materials, Thomas Publishing, Springeld, IL, 1975, with permission].
1176
SELECTION OF MATERIALS FOR BIOMEDICAL APPLICATIONS
Co py rig hte dM ate ria l
1. Minimize the number of different metals used in the implant. Two metals that differ in electrochemical potential, due to differences in elemental composition or processing, will create a galvanic potential when connected either directly or through an ionic uid. This can include parts manufactured of the same material but by different companies or different techniques, as the processing schedule may differ enough to create differences in the electrical potentials of the components. 2. Minimize the possibility of surface damage. Any scratches to the surface of a metallic implant can serve as foci for corrosion once it is implanted. Thus, it is important to protect the implant from the stage of nal processing through implantation to prevent damage. 3. Reduce the number of crevices or regions where oxygen depletion is possible. A region with a low-oxygen concentration, such as the interfaces between modular components of a total joint implant or the threads of a bone screw, is likely to become anodic with respect to the surrounding metaleven with respect to the remaining bulk of the metal. Corrosion will therefore occur with the small, anodic region providing electrons to
Copyright 2002 John Wiley & Sons Retrieved from: www.knovel.com
hydroxide layer on the surface of the metal. Immunity is the region in which minimum oxidation is going to occur as the equilibrium concentration of metallic ions is low. (The equilibrium concentration refers to the levels of ions in the immediate, surrounding environment at which the oxidation reaction reaches equilbirium, thus producing no further net release of ions.) Both passivation and immunity require that less than 10 6 M of ions be produced (Park and Lakes, 1992). Thus, in neither of these cases is oxidation eliminated for a metallic material; however, the effect on the implants properties and the ion concentration produced will be negligible. As a nal check of biocompatibility, it is important to ascertain that the trace levels of ions produced by passivated or immune metals will not produce toxic effects at even those low concentrations. Pourbaix diagrams can only provide information on the ideal behavior of a metal within its immunity or passivation regions. As the limitation of corrosion in these environments is due to the establishment of a chemical equilibrium, the ionic environment of the implant surface and the surrounding physiologic uid must remain undisturbed. Therefore, any damage to the passivation layer, or any uid ow that removes the equilibrium ions from the region immediately adjacent to the implant, may cause renewed corrosion. Cyclically loaded implants could be expected to experience both surface damage, due to wear or contact with other tissues, and movement of the uid surrounding the implant. In addition, the local pH at a site may be affected by common physiologic insults, such as injury and infection. Finally, most Pourbaix diagrams are determined for pure water environments, and therefore do not include the role of additional ionic components in the physiologic uid. This would also be expected to inuence the corrosion behavior of a material. Therefore, the behavior predicted by the Pourbaix diagrams may be taken as a base line expectation, but must be conrmed through both animal and clinical testing. Some additional rules can be applied to minimize the occurrence of corrosion for an implant with metallic components. These are:
ORTHOPEDIC BIOMATERIALS: TOTAL HIP ARTHROPLASTY
1177
the entire cathode. If there is a discrepancy in the size of the regions, as would normally be expected, then corrosion within the crevice can be accelerated, leading to potential mechanical failure.
Leaching and Absorption
Co py rig hte dM ate ria l
F D C x
Copyright 2002 John Wiley & Sons Retrieved from: www.knovel.com
Polymers placed in a uid environment can experience two opposite phenomena. In leaching, unreacted monomer molecules, llers, or small chains of polymers can diffuse from the bulk of the polymer to the surrounding uid. As in corrosion products, these released molecules may have a negative effect on the local physiology or, if transported through the bloodstream or lymphatic system, on systemic or remote processes. In addition, signicant leaching may reduce the density of the polymer and consequently have an adverse effect on the properties of the structure. Absorption occurs when water molecules, proteins, or lipids diffuse from the uid into the mass of the polymer. The absorbed molecules become distributed between the molecules of the polymer, reducing the mechanical strength of the structure and increasing its susceptibility to wear. Both absorption and leaching occur as a result of diffusion processes across the surface of the implant. Ficks rst law of diffusion describes the rate of solute transfer across a permeable barrier: (4)
where F is the rate of solute transfer per unit cross-sectional area of the surface, D is the diffusion coefcient, and C/ x is the concentration gradient. The diffusion coefcient is dependent on the solute (the molecule that is being absorbed or released), the matrix through which it is moving (the remainder of the bulk polymer), and the type of diffusion that is occurring. Thus larger molecules moving through more tightly bonded matrices are likely to leach out at a lower rate than small molecules diffusing through a more open, amorphous structure. All materials, including metals and ceramics, can absorb molecules particularly waterfrom the surrounding environment. However, this occurs much more readily in the relatively loosely bonded polymers. Absorption in polymers can also result in swelling, due to their low elastic modulus, which may cause geometric changes that interfere with the performance of an implant. The strain that a polymeric object experiences due to swelling may induce cracks and may also reduce the ultimate strength of the object. This latter phenomenon occurs because, due to the new baseline strain in the material, less stress is needed to reach the materials ultimate strain. If the absorbed molecules are small, such as water, they will act as plasticizers and weaken the bonds between the polymer chains, thus reducing the Young modulus of the material. If a polymer is hydrophobic in nature, it is less likely to absorb water. However, absorption of nonpolar molecules such as lipids may still occur. Leaching generally has a smaller effect on the mechanical properties of a polymeric structure than absorption. However, as was the case in corrosion, local changes in properties may occur as material is lost. In fact, if sufcient leaching occurs to create adjacent or expanded voids within the chemical structure of the polymer, these regions may act as stress risers. A high amount of leaching will
1178
SELECTION OF MATERIALS FOR BIOMEDICAL APPLICATIONS
Co py rig hte dM ate ria l
Wear Debris
act to increase the porosity of the polymer. In both of these cases, the elastic modulus and the mechanical strength of the polymer would be affected. In general, low-molecular-weight or highly amorphous polymers are more susceptible to leaching or absorption processes than high-molecular-weight, highly crystalline, or highly cross-linked polymers. As diffusion coefcients increase for smaller molecule sizes, in general, it can be expected that additives and free monomers have a higher rate of leaching than the large polymer chains themselves, while the relatively small water molecule will be absorbed by hydrophilic polymeric structures at a relatively high rate. The behavior of free monomers and additives within polymers is of particular interest, as they may have a different effect on the surrounding tissue than tests based on the bulk polymer suggest. In fact, free monomer should be expected to have a different physiologic effect than molecules that have reacted to form the bulk polymer, due in part to the difference in chemical reactivity of the structures.
The material produced through the wear process is typically in the form of particulate debris. The size of the particles is dependent on the material involved and may range from submicon dimensions to millimeter-sized pieces. In polyethylene, particles typically range from 0.5 to 50 m in their largest dimension, while polymethylmethacrylate (PMMA, bone cement) particles tend to be signicantly larger (Willert and Semlitsch, 1996). These particles can have several adverse effects on implant performance beyond the geometric changes discussed above. First, if the debris becomes trapped between the articulating surfaces of the joint, it will act as a collection of third-body particles to accelerate the wear process. Second, the presence of particulate debris in the tissue surrounding the bone triggers an immune response that can result in signicant bone loss through the process of osteolysis. When this occurs without an associated infection, it is termed aseptic loosening. The presence of histiocytes, macrophages, and foreign body giant cells in locations with both mild and severe osteolysis indicate that the process is inammatory or immunological in nature. It is currently hypothesized that the presence of particulate debris results in macrophage and giantcell recruitment (Jacobs, et al., 1994). The larger particles are engulfed by giant cells through phagocytosis and form granulation tissue, while macrophages react with the smaller particles. Normally, foreign debris on a small scale will be removed through the lymphatic system. However, if the volume of debris produced overloads the lymphatic system, then macrophages at the implant site may release cellular mediators that trigger the bone resorption observed.
2.3 Current Material Selection
The traditional materials that have been used for total hip arthroplasties are ultrahigh molecular-weight polyethylene (UHMWPE) for the articulating surface of the acetabular cup and a metal, today typically an alloy of titanium or of cobalt chromium, for the femoral stem, head, and backing of the acetabluar cup. In a smaller number of designs, ceramics such as alumina (Al2O3) and zirconia (ZrO2) have been used for a modular femoral head component, both to reduce friction within the acetabulum and minimize the number of metallic components that may exacerbate corrosion. Table 4 provides a summary of some of the
Copyright 2002 John Wiley & Sons
Retrieved from: www.knovel.com
ORTHOPEDIC BIOMATERIALS: TOTAL HIP ARTHROPLASTY
1179
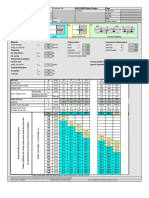
Table 4 Summary of Mechanical Properties for Materials Commonly Used in Current Total Joint Replacement Designsa Property HMWPE Titanium Alloy CoCr Alloy Alumina Cortical Bone
Co py rig hte dM ate ria l
620 500 0.930.94 4.5 3500 9.2 30004000 3.9 20,000 1.8
Copyright 2002 John Wiley & Sons Retrieved from: www.knovel.com
Elastic Modulus [GPa] Comp. Strength [MPa] Tensile Strength [MPa] Endurance Limit [MPa] at 107 cycles Density [g / cm3] Hardness [MPa]
2.2
110
220234
350400 4000
1020 130280 80160
860
6001000
270
a Titanium alloy, Ti6Al4V; CoCr alloy, wrought CoNiCrMo. Source: Data from ASTM-F136 (1998), ASTM-F562 (2000), ASTM-F648 (2000), BernacheAssolant (1991), Brunski (1996), Cowin (1989), and Park and Lakes (1992)
mechanical properties of these common materials and lists cortical bone for comparison purposes. In the selection of metals, cobaltchromium alloys with molybdenum have been preferentially chosen over those with nickel. Despite the fact that the mechanical properties are slightly reduced in the molybdenum alloy compared to the nickel variant, it has been shown to have improved wear properties. Titanium is often chosen due to the fact that its elastic modulus is half of that seen in cobaltchromium or stainless steel alloys, therefore reducing the stiffness of the implant and the accompanying bone loss due to stress shielding. During the past decade, substantial research has been conducted to develop different pairs of materials for the bearing surface in order to reduce the wear phenomenon commonly seen in HMWPE, which often leads to premature failure of an implant. Metal-on-metal and ceramic-on-ceramic headcup combinations have shown promise in terms of long-term outcomes, especially when used in younger patients for whom an implant life of greater than 20 years would be desirable (Delaunay, 2000; Skinner, 1999; Wagner and Wagner, 2000). The ceramics typically selected have been alumina and zirconia, while the metal is generally a cobaltchromium alloy. Titanium does not lend itself to metalmetal bearing surfaces due to the fact that it tends to seize when in contact with other metals. The success of these material combinations is due in large part to the improvements in materials processing, machining, and polishing that have been achieved in the last quarter century, allowing for the development of high-quality materials, excellent geometric matches, and highly polished surfaces. This progress also indicates that designs that were tried out at an earlier point in history, and were perhaps abandoned, may deserve to be reexamined. Metal-on-metal bearings were originally used in total hip replacements in the 1950s, with limited success. Complete ceramic bearings were seen as early as the 1970s, but fracture of the ceramic components and high wear were attributed to problems in processing that resulted in defects and inadequate grain sizes (Plenk, et al., 1992; Sedel, et al., 1991). In time, they were almost completely replaced in the clinical world by metalpolymer combinations. However, their revival in the past few
1180
SELECTION OF MATERIALS FOR BIOMEDICAL APPLICATIONS
years, spurred on by developments in materials engineering, indicates that the original developers had the right ideathey were just a few years ahead of their time.
3 BLOOD-CONTACTING BIOMATERIALS: VASCULAR PROSTHESES
Co py rig hte dM ate ria l
Fig. 6 Schematic diagram of an artery showing the three tissue layers: adventitia (outer), media (middle), and intima (inner). Copyright 2002 John Wiley & Sons Retrieved from: www.knovel.com
When blood vessels are damaged through injury or disease, they often must be replaced or bypassed in order to maintain adequate blood ow to and from the regions of the body. Disease-induced damage, such as atherosclerosis and aneurisms, occurs more often in arteries than in veins, due in large part to the higher working pressure of the blood within these vessels. Injury can occur to any blood vessel; however, collateral circulation typically eliminates the need to replace small veins, and the low venous return pressure provides an environment in the larger veins that is much more conducive to traditional surgical repair or autograft use. As a result, this section will focus on the selection of materials for the development of arterial prostheses. Arteries are three-layer hollow tubes (Fig. 6) composed of a combination of elastin, collagen, and smooth musclewith the proportions of each component dependent on the size of the artery. The size of an artery also varies substantially along the arterial tree, from a typical diameter of about 4 cm for the aorta in an adult to a diameter of less than 1 mm for arterioles. The age and size of the individual will also affect the dimensions of the arteries. Normal arterial pressure is approximately 120 mmHg during the systolic phase (contraction) of the cardiac cycle, decreasing to approximately 70 mmHg during the diastolic phase (relaxation). However, pressures can rise as high as 200 mmHg or more in individuals with either transient or chronic hypertension, and hypertension itself is a risk factor for a number of the pathological processes that may require arterial replacement or bypass. Elastic arteries, such as the aorta, are expected to expand during systole as blood is forced into them by the heart. The elastic recoil of these vessels, due in large part to the high amount of elastin in the wall, acts to maintain arterial pressure during the relaxation phase of the cardiac cycle, further transporting blood away from the heart. Distributing arteries, which (as their name indicates) distribute blood from the larger, elastic arteries to the various regions of the body, have more collagen than elastin in their walls. However, the physiologically important component of these vessel walls is the smooth muscle, which
BLOOD-CONTACTING BIOMATERIALS: VASCULAR PROSTHESES
1181
Co py rig hte dM ate ria l
3.1 Function Blood Transport
Copyright 2002 John Wiley & Sons Retrieved from: www.knovel.com
allows the distributing arteries to adjust their diameter and therefore their resistance. By controlling the arterial resistance to blood ow in various regions of the body through vasodilation and constriction, blood can be directed to regions that have the highest metabolic demandthe muscles during exercise or the gastrointestinal system during digestion. Vascular grafts were rst introduced in the early twentieth century as solid tubular structures. Fabric grafts were developed in the 1950s and provide the basis for the grafts that are currently in use or under development. An arterial graft or arterial prosthesis has one obvious functionto transport blood from vessels that are proximal to the graft to those that are distal to the graft. In addition, the vasodilation/constriction and elastic recoil capabilities of the various types of arteries assist the heart with transport and direction of blood to the diverse tissues of the body. However, there are additional functional constraints that are equally as important. First, the prosthesis must maintain hemostasis not allow blood to leak from the artery into the surrounding tissues. Second, interaction of the blood cells with the vessel must not act to initiate coagulation, which could result in thrombus formation and embolisms, nor hemolysis, the destruction of red blood cells. These functional constraints will be considered in the discussion on biocompatibility.
To transport blood between two connecting vascular segments, a tubular structure is required. However, given modern material processing techniques, this requirement does not itself limit the selection of materials substantially. The graft must also, however, be connected to the ends of the remaining vascular segments in some way, either through ligatures or sutures. Using a maximum arterial pressure of 200 mmHg (30 kPa), the circumferential and axial wall stresses within a graft (diameter of 1 cm, thickness of 0.5 mm) can be approximated to reach 270 and 135 kPa, respectively. This is well within the mechanical limits of most undegraded articial materials; however, it may become a substantial constraint for vessels engineered from natural materials in the future. In addition, the physiological environment, combined with the cyclic loading seen by the vessel due to the normal vascular pressure variations, will affect the properties of the graft material. As discussed above for hip replacement, corrosion, absorption, and leaching processes that occur when a material is placed in vivo will all negatively affect the ultimate strength of a material. The expansion and recoil observed in elastic arteries must be taken into consideration when selecting a material for grafts at these locations. It is reasonable to assume that a relatively short length of the graft does not itself need to dynamically change dimensions to maintain blood ow through the segment of vasculature. However, any mismatch in the behavior of the graft to the connected vessels will result in substantial stresses on the ligatures, sutures, or the vessel itself. In certain applications, the graft may replace a substantial portion of an artery, such as in the descending aorta. In this case, elastic recoil in the graft will play an important role in maintaining the velocity of blood ow through
1182
SELECTION OF MATERIALS FOR BIOMEDICAL APPLICATIONS
Co py rig hte dM ate ria l
Fig. 7 Schematic diagram showing the characteristic nonlinear forcedeformation relationship of an artery. Initial region of high compliance is characteristic of the elastin component in the walls, while the later, low-compliance region exemplies the deformation of the collagen bers. Copyright 2002 John Wiley & Sons Retrieved from: www.knovel.com
the distal vessels, and the pulsatile ow may be important to maintaining function in organs supplied by the arterial tree (Mergerman and Abbott, 1983). The same philosophy would apply to distributing arteries. At the current time, no articial material exists that would respond to the physiologic control mechanisms in order to dilate and constrict in conjunction with surrounding vessels. However, a graft that is less compliant than the attached vessel would result in substantial stress concentrations at the junction between the articial and natural materials. This elevation in stress could lead to failure of the sutures or ligatures connecting the structure, as well as accelerate fatigue processes within the graft ends (Wilkerson and Zalina, 1994). In addition, a less compliant graft can also result in a stenosis in the vascular tree during systole, when the proximal segment of artery expands under pressure, but the blood then encounters the length of reduced diameter graft that acts to retard ow (Herring, 1983). These issues, along with the fact that blood vessels experience signicant deformation due to general body motion, essentially dictate that a soft, exible material be used for the graft. An ideal graft would exactly match the compliance of the attached blood vessel, allowing it to expand and recoil to the same extent as the natural structure. This would require a nonlinear response, with an initial region of highly compliant stretch, attributed to the unkinking and realigning of the collagen bres and a simultaneous stretching of the elastin. After the collagen in the vessel wall is straightened, its higher elastic modulus dominates the behavior of the vessel, and the compliance is signicantly reduced. It is this behavior (Fig. 7) that is thought to limit the overexpansion of arteries during acute episodes of elevated blood pressure. The compliance of each segment of artery therefore depends on the proportion of collagen, elastin, and smooth muscle (which has a negligible effect on compliance in its passive state) within the vessel wall.
BLOOD-CONTACTING BIOMATERIALS: VASCULAR PROSTHESES
1183
Typical values for compliance (in units of percent radial change per millimeter of mercury) for cadaveric human arteries range between 10.9 at 60 mmHg and 3.8 at 150 mmHg (Mergerman and Abbott, 1983).
3.2 Biocompatibility
Co py rig hte dM ate ria l
Neointima Formation
Copyright 2002 John Wiley & Sons Retrieved from: www.knovel.com
The primary functional need of a blood vesseltransport of bloodcan easily be met through general implant design. However, due to the delicate nature of blood cells and the ease at which the clotting cascade can be initiated, biocompatibility issues place substantial limitations on material selection for this application. The natural vessel provides an optimal environment for blood ow, and the mimicking or replacing of its intimal layer is one of the underlying ideas in work to improve biocompatibility in vascular grafts.
Natural blood vessels consist of three layers: the outer adventicia, the middle media, and the inner intima. The intima has a layer of endothelial cells that contact the moving blood in order to minimize damage to the cellular elements of the uid. Some articial materials that are implanted into the body as vascular grafts have been shown to develop a neointimabrin and broblasts that develop as a lining on the inside surface of the tube (Herring, 1983). The rate of neointima formation and its constituents may depend on the material used in the vascular graft. A carbonceramic composite with a large degree of surface porosity showed almost instantaneous ( 10 s) development of a brin mesh with limited platelet adhesion (Chignier et al., 1987). This developed into a 5- to 7-cell thick layer of broblasts, collagen, and elastin by 15 days, with endothelial-like cells present and fully developed by 2 months. Herring (1983) provides a good description of the healing of vascular grafts and the development of the neointima. In most human vessels, complete endothelialization occurs only in the vicinity of the anastomoses with the natural vessels, as cells grow in from the ends of the connected tissue. To expand the area of vessel that experiences complete healingsuch that the lining resembles that of a natural, healthy vesselresearch is being conducted into seeding the vessel wall with endothelial cells (Consigny, 2000; Herring, 1983). This can either be done during the preclotting process, in the operating room, using a small number of cells taken from a vein that is exposed during the surgical procedure, or preoperatively using cells from the jugular vein that are cultured to provide a greater volume for the seeding process. In both cases, the use of autologous (patient specic) cells is important to eliminate issues of rejection. The geometry of the vessel also affects neointima formation. The initial interaction between the blood and the graft is the formation of a clot, or thrombus, on the inner surface of the vessel. The thickness of the implant wall is directly proportional to the thickness of the thrombus formed on its surface (Park and Lakes, 1992). As the thrombus must be remodeled to form the mature neointima, a smaller clot results in faster organization of the neointima. Neointima formation must be limited, however, to prevent vessel occlusion. This is one of the issues with small diameter vascular grafts, where the brin layer may continue to grow past 1 mm in thickness (Wilkerson and Zalina, 1994). Finally, it is important to ensure that the neointimal layer that develops maintains its integrity
1184
SELECTION OF MATERIALS FOR BIOMEDICAL APPLICATIONS
and does not change in such a way, either through mineralization or adsorption of additional organic components, that it no longer promotes the continued patency of the vessel (Hufnagel, 1983).
Hemostasis
Co py rig hte dM ate ria l
Hemolysis
For vessels to adequately transport blood, the blood must remain within the lumen of the vessel and not leak into the surrounding tissues in any great amount. The obvious answer to this problem is to employ solid materials for vascular grafts, nonporous structures that will adequately contain the blood. However, the development of a neointima within a vessel provides a second design option, as it will act to seal a porous blood vessel against blood leakage. However, the time course for neointima formation is not short enough to provide the immediate seal needed during surgery and postoperatively. Therefore, many vascular grafts are preclotted in the operating room before they are implanted by exposing both the inner and outer surfaces to the patients blood. This provides an initial surface that serves as the basis for neointima formation.
Hemolysis, or the damage and destruction of red blood cells, occurs continually within the body. The cells are constantly replaced by new erythrocytes produced by the bone marrow. However, chronic damage to these cells and the release of their cellular contents into the plasma of the bloodstream can result in anemia, kidney failure, and other toxic reactions (Hershko, et al., 1998). Hemolysis due to nonphysiologic mechanisms typically occurs due to high shear stresses. A shear stress as low as 400 Pa can damage or rupture a red blood cell that comes in contact with another solid surface (Sallam and Hwang, 1984). Turbulent ow can also result in sufcient shear stresses to cause hemolysis. Therefore, two goals of vascular graft design are to minimize the contact between red blood cells and the graft surfaces and minimize the turbulence that may occur at branches or divisions of blood vessels. The latter falls within the domain of uid mechanics, rather than biomaterial selection. To minimize the contact between blood cells and graft walls that may lead to hemolysis, it is desirable to form a natural tissue layer between the two. Graft materials with high surface tensions tend to initially attract platelets and brin molecules, which aggregate and form the natural boundary that is then remodeled to become the neointima. The elements of the tissue layer also exhibit a slight negative electrical charge (Collins, 1983), which may act to repel the negatively charged red blood cells, therefore additionally reducing the contact between the cells and the vessel wall.
Coagulation
Blood clotting, or coagulation, is a necessary physiologic process that allows the body to heal and maintain its blood pressure through hemostasis. However, the formation of stationary clots within blood vessels (thromboses) and the movement of those clots with the blood ow (emboli) can result in vascular blockage, tissue damage, and even death. Therefore, it is important to select materials for graft use that will minimize the initiation of the clotting cascade. The effect of a material on blood clotting is not easy to assess, particularly as it is difcult to separate the effect of the material from the natural physiologic
Copyright 2002 John Wiley & Sons Retrieved from: www.knovel.com
BLOOD-CONTACTING BIOMATERIALS: VASCULAR PROSTHESES
1185
process of coagulation. Blood will also behave slightly differently in vivo than it will in vitro and, like other tissues, can differ between individuals. Therefore, an in vitro coagulation test with blood from a dog may not be fully indicative of how that material will behave when implanted into a human. Standards have been developed, however, for coagulation tests (Bruck, 1980), and these progress from static, in vitro tests to dynamic, in vivo tests. Surface tension, surface charge, and surface roughness are properties of a material that will affect the rate and amount of coagulation that takes place when it is in contact with blood. Polymeric materials tend to adsorb a mixture of proteins to their surfaces in the rst 3060 s of contact with physiologic uid (Baier, 1975), the composition of which depends on the polar or nonpolar nature of the polymer (Herring, 1983). Adsorbtion and activation of key molecules from blood, including Hageman factor, factor XI, and others, will trigger the clotting cascade (Forbes, 1993). Rougher surfaces, including crimped grafts, have been shown to increase the rate of coagulation that occurs when in contact with blood (Collins, 1983). This is probably due to the larger surface area that can come in contact with the blood. A rough surface may be desirable, however, in order to promote preclotting on the surface of a porous graft. In the case of crimping, the process also prevents kinking of the vessels during surgery or prolonged implantation, which itself can lead to occlusion. Surface charge can help to minimize the contact between the graft and the blood elements. The formed elements of the bloodred and white blood cells and plateletshave been shown to have a negative surface charge. As a result, a vascular surface with a slight negative charge, through the presence of either a neointima or a naturally or articially induced surface charge, will act to repel the blood cells and platelets away from the vascular wall (Collins, 1983). When platelets do not come in contact with the vascular wall or foreign bodies, they are less prone to initiate the clotting cascade. The natural lining of blood vessels possesses unique properties that cannot be easily mimicked. It was originally believed that the smooth surface and the negative surface charge were the properties of an endothelial lining that prevented clot formation. However, studies have shown this to be more complex. In particular, the presence of endothelial cells allows for the secretion of paracrine agents that act to break down small thromboses and interfere with clot formation (Bruck, 1980). Smooth muscle and broblasts did not exhibit the same function, and in some cases precipitated platelet activation. Thus, as was the case in bones resistance to fatigue, the living function of vascular tissue cannot be fully replaced using current technologies and articial materials. To reduce clotting in articial materials, several approaches have been taken. Heparin, a negatively charged polysaccharide that is commonly used to prevent clottting in many clinical applications, has been coated on implants. Using the same logic, anionic radicals have been included in an articial material to produce the negative surface charge that only naturally can occur in polymers. Taking a different approach, materials with low surface tensions have been proposed, as they are less likely to attract the formed blood elements to the material surface and initiate a clotting cascade. This last tact is, of course, in contradiction to the suggested use of high surface tension materials to minimize hemolysis! This latest dilemma is indicative of many decisions that must be made in selecting a material for use in biomedical applications. No materialbesides
Copyright 2002 John Wiley & Sons Retrieved from: www.knovel.com
Co py rig hte dM ate ria l
1186
SELECTION OF MATERIALS FOR BIOMEDICAL APPLICATIONS
possibly the original tissuewill perfectly match all of the goals and constraints of the design. It is generally necessary to weigh the benets and drawbacks of each material that makes the short list and to select the one that shows the best balance. While this is frustrating from a design aspect, it is what spurs material development and allows for the continuing work in the area of material synthesis and implant design.
Co py rig hte dM ate ria l
Property Degradation
Once a material is selected that does not seem to have a signicant, adverse effect on the blood itself, it is necessary to evaluate how the properties of the graft are affected during the expected contact with the physiological environment. As discussed above for orthopedic implants, polymers can react to the physiologic environment by either leaching smaller molecules into the surrounding tissue or absorbing water or other materials from the tissue. In the case of vascular grafts, the constant ow of blood past the implant surface will eliminate the possibility to develop an equilibrium between the molecule concentrations inside and outside of the implant material. As an example, nylon has been found to absorb water from the surrounding environment when implanted (Edwards, 1983). The water molecules act as plasticizers, which reduce the cohesion and bonding between the chains of the polymer. The nal result is a reduction in strength. Whether property degradation will be a determining factor in material selection for vascular implants depends largely on the planned time of implantation for the device. For a graft that will permanently replace a section of blood vessel, it is extremely important to maintain the tissue properties at an appropriate level. However, many blood contacting applications involve short-term usefor instance intravenous catheters for administering blood or pharmaceuticals. In these cases, the length of intended use is typically less than a few days, and the catheter can be relatively easily replaced if necessary. Therefore, for short-term implants, the prevention of blood clot formation and blood cell damage, along with ease of use and cost, become the determining factors in material selection.
3.3 Current Material Selection
Since the 1950s, polymer fabrics have been the primary material used for longterm vascular grafts. Nylon was introduced in 1955, but was withdrawn from use after the occurrence of aneurisms within the grafts indicated a loss of mechanical integrity in vivo (Edwards, 1983). Teon (PTFE, Gore-Tex) and polyethylene terephthalate (PET, Dacron) have been shown to have acceptable amounts of property degradation when implanted for 20 years or more (Snyder, 1983). Table 5 shows results on the loss of strength in various polymers that were implanted for 100 days. The Dacron showed an initial drop in strength that then stablized at an acceptable level. Typical vascular grafts are constructed of a woven or knitted fabric and are crimped, to both prevent kinking and to allow for longitudinal expansion (Fig. 8). The response of the graft in vivo will depend not only on the constituent material selected, but also on the weave of the fabric and on its processing (Sawye, et al., 1983). Grafts are typically tested to validate their tensile or bursting strength, and the values obtained for the constructed vessel will differ from those of the bulk material due to the knitted or woven nature of the fabric.
Copyright 2002 John Wiley & Sons Retrieved from: www.knovel.com
BLOOD-CONTACTING BIOMATERIALS: VASCULAR PROSTHESES
Table 5 Average Changes in Tensile Properties of Synthetic Grafts Implanted for 100 Days Material Loss of Strength (%)
1187
Co py rig hte dM ate ria l
Source: Data from (Edwards, 1983)
Fig. 8 Left and right: Examples of fabric arterial grafts, illustrating the crimped structure that prevents kinking in vivo. Center: Extruded PTFE graft lined with pyrolytic carbon. Copyright 2002 John Wiley & Sons Retrieved from: www.knovel.com
Nylon Orlon Dacron Teon
81 6.9 10.1 3.2
Pyrolitic or LTI (low-temperature isotropic) carbon has been found to have excellent anticoagulation properties (Bruck, et al., 1973), without the need for heparin coating of the material. The original LTI formulation required a solid substrate and so was more conducive for use on shunts or leaets of heart valves. A newer, ultra-low-temperature iostropic carbon (ULTI) can be vapor deposited onto fabrics as well (Bruck, 1980), allowing for its use in regions that require exibility (Fig. 8). ULTI carbon, which can be deposited with a thickness of less than 1 m, has been shown not to affect the compliance of the underlying fabric (Sharp, 1983), indicating that it will maintain its exibility when deposited on a fabric graft. For short-term implants, generally in the form of catheters, silicone rubber has become the standard. Its optical translucence makes it easy to monitor uid transfer, it is easy to use, and it is highly biocompatible. Fabric grafts and silicone tubes, however, are not adequate for the small-vessel replacement that may be required during reconstructive surgery. As a result,
1188
SELECTION OF MATERIALS FOR BIOMEDICAL APPLICATIONS
tissue engineering techniques are currently being employed to construct smalldiameter vessels from natural materials, such as chitosan (Chupa, et al., 2000). Research such as this is working to expand the possibilities for material selection, not only for vascular prostheses but also for all biomedical implants.
4 SPACE-FILLING BIOMATERIALS: BREAST IMPLANTS
Co py rig hte dM ate ria l
4.1 Function Space Filler
Implants designed to ll voids where tissue has either been removed or destroyed are commonly used in reconstructive surgery. Hard tissue, soft tissue, and combination materials have been utilized to replace or augment cranial defects, the loss of an ear, nose, or eye due to trauma or disease, and congenital facial abnormalities, among others. Perhaps the most familiar and infamous spacelling implant was, and is, the breast implant. Originally designed for reconstructive surgery following mastectomies, breast implants became increasingly popular for cosmetic enhancement during the 1970s and 1980s. The question of whether the implants were the cause of the illnesses and disabilities reported in the 1990s has never been answered to everyones satisfaction, and probably never will be. It is an example of a biocompatibility issue that, if true, went unnoticed for many years. It also serves notice to all biomedical implant designers that because an implant does not indicate any problems after 5 years does not mean that monitoring of potential complications should stop. Breast implants were designed with one function in mindto replace tissue that had either been removed through surgery or that an individual felt nature had left lacking. There was no other physiologic role for the implant, which made its design much simpler. The rst breast augmentation utilized injections of silicone, parafn wax, or bees wax directly into the tissue surrounding the breast. This method was banned by the Food and Drug Administration (FDA) in the 1960s as the injected material was seen to migrate and lose its shape. In addition, because of the large contacting surface area between the injected material and surrounding tissue, adverse tissue reactions were seen (Frisch, 1983). Since that time, breast implants have utilized conned volumes of materials (Figure 9).
As stated above, the single role of a breast implant is to ll up a given volume of space within the body. However, cosmetic appearance and feel have also dictated much of the development of the implants. The density of the implant should be similar to or less than the surrounding tissue, so that tissue damage does not occur due to increased weight. The consistency of the material should also be somewhat similar to the composite of fatty and connective tissue that it has replaced. Thus, metals, ceramics, and solid pieces of polymer would be inappropriate.
4.2 Biocompatibility
Capsule Formation
No articial material that is implanted into the body will be ignored completely. The degree of the reaction from the immune system will depend on a number
Copyright 2002 John Wiley & Sons
Retrieved from: www.knovel.com
SPACE-FILLING BIOMATERIALS: BREAST IMPLANTS
1189
Co py rig hte dM ate ria l
Copyright 2002 John Wiley & Sons Retrieved from: www.knovel.com
Fig. 9 Examples of saline-lled breast implants showing the silicone elastomer envelope. Surfaces can either be textured (upper) or smooth (lower). The textured design is thought to reduce the incidence of capsular contraction.
of factors, including the chemical or electrical activity of the material. The initial reaction of the body to a foreign object is to wall it off. A brous capsulea result of the normal wound healing response of the bodywill develop around the structure, with the thickness of the capsule increasing in regions of high chemical activity, high electrical activity, or sharp corners. The presence of this brous capsule formation can be taken advantage of to assist with implant xation, however. For objects with smooth surfaces, the brous capsule will simply grow around the outer surface of the material. If the surface of the foreign body is porous, however, brous tissue will begin to grow into the interconnected pores of the structure. For bony implants, this tissue can become calcied and develop into a bony junction between the implant and the surrounding tissue. For soft tissue implants, this brous capsule can become integrated with the surrounding connective tissue of the body to provide rm anchorage of the implant at a desired location. Complete brous tissue integration with the implant material will be most efciently achieved with a pore size ranging from 5 to 30 m (Rose and Litske, 1989; Wilkerson and Zalina, 1994). The amount of desirable brous capsule integration with the implant must, however, be assessed and the area of porous surface determined as part of the overall design. One breast implant design that failed because of an overabundance of brous capsule integration was the sponge design developed in the 1950s (Dukes and Mitchley, 1962; Edgerton and McClary, 1958). This implant,
1190
SELECTION OF MATERIALS FOR BIOMEDICAL APPLICATIONS
Co py rig hte dM ate ria l
Carcinogenesis and Immunological Complications
which met the space-lling requirements and was composed of polyvinyl alcohol foam, was found to experience complete brous ingrowth. Although the implant was rmly xed in the correct anatomical position, the brous capsule tended to contract and calcify, resulting in a condition known as marble breast syndrome. All breast implant designs have shown some incidence of capsular contraction, which in severe instances has required the implant to be removed. This has led to the FDA requirement in the United States that all implant manufacturers inform prospective patients of this potential complication and the fact that breast implants should not be considered to be lifetime prostheses. While no implant design has been developed that eliminates this phenomenon, the area of xation patches on the posterior surface has been reduced, textured (though nonporous) surfaces have been introduced for the silicone envelope, and clinical interventions, including massage, have been prescribed in attempts to minimize the problem. For both carcinogenesis and general immunological considerations, it is important to examine the response of not only the bulk material that is to be used but also the components of the materials. This includes unreacted monomer, plasticizers, llers, and any products that can result from the metabolic breakdown of the bulk material in vivo. Any chemical compound that could be released by an implant is a potential hazard. The complexity of this analysis becomes readily evident. The exact mechanism, or mechanisms, by which healthy cells in the body mutate into malignant cells and cause cancer is not fully understood. However, it is a well-accepted principal that all possible attempts should be made to avoid implanting a material into the body that would increase the risk of cancer. As cell mutations and tumor development can take many years to become evident, how can this be done practically for newly developed materials? Carcinogenesis, or the production of cancer, can occur in the immediate vicinity of an implant, due to the presence of various chemicals, or at a remote location in the body, due to the transport of released materials. Materials in the body can act in one of three ways to cause cancer: (1) as a complete carcinogen, resulting in cancerous changes by itself; (2) as a procarcinogen, a benign chemical that is metabolically modied into a carcinogen by the body; or (3) as a cocarcinogen that is not likely to itself cause cancer, but will increase the activity of a complete or procarcinogen with which it comes into contact. It is hypothesized that there is no threshold below which a carcinogen present in the body is completely safe; however, as concentrations of a chemical increase, the probability that they will induce cellular changes that result in cancer also increase (Black, 1999). A tumor may also develop in response to the presence of a solid foreign body made of a noncarcinogenic material, due to the disruption of the normal environment of the surrounding tissues (Black, 1999). Testing of materials for their carcinogenic potential ranges from cell culture studies that examine whether a material causes cells to mutate (Forster, 1986), to in vivo animal tests and the development of databases to track the occurrence
Copyright 2002 John Wiley & Sons
Retrieved from: www.knovel.com
SUMMARY
1191
Co py rig hte dM ate ria l
4.3 Current Material Selection 5 SUMMARY
Copyright 2002 John Wiley & Sons Retrieved from: www.knovel.com
of tumors in implant recipients. There are drawbacks to all of these tests, and none, with the exception of a longitudinal study of tens of thousands of patients with the same implant, can denitively determine if there is a link to cancer for an implant or a material that does not initially appear to be carcinogenic. The primary benet of these tests is to eliminate from consideration materials that appear to have a high likelihood of causing tumors. General guidelines for basic biocompatibility testing have been issued by the International Standards Organization and other regulatory agencies (ISO-10993, 19922000). Similar problems exist for the documentation of other systemic or remote tissue complications. Techniques have been developed to evaluate the immunological response to a material (Marritt, 1986); however, the link between local immunological sensitivity and a systemic autoimmune reaction may not be easily discernable. It is important to determine whether the occurrence of a particular disorder, whether it is lymphoma or rheumatoid arthritis, is occurring within the implanted population at rate that is higher than the general population. One of the difculties in tracking the incidence of these occurrences is the fact that many implant materials and combinations change on a time scale that is short compared to the development of cancer and other immunological conditions. As these material combinations change, it introduces another variable that requires a higher number of subjects before a statistical determination can be made. However, the establishment of databases at the national, or preferably international, level for tracking of all complications associated with biomedical implants will allow for a more complete analysis and more rapid understanding of the problems associated with this imperfect science. Prior to 1992, the most common form of breast implant involved a small bag of silicone elastomer lled with silicone gel. Originally introduced in 1962 (Cronin, 1983), this implant was popular among patients and physicians alike. While the silicone elastomer of the bag has been utilized in biomedical implants for many years without signicant adverse effects, the breast implant scare of the 1990s was based on rumors that the silicone gel had a tendency to leak from the surrounding bag and cause adverse reactions at both local and remote locations. Since that time, the majority of breast implants have utilized saline within the same silicone rubber bag. If the saline does leak, or the implant does rupture, the reaction with the tissue will be completely benign. This design has been an option since 1965 (Rubin, 1983); however, most patients opted for the silicone version due to its improved cosmetic appearance. There are few, if any, current implants that can be described as perfectly meeting their design goals and constraints so that no further investigation of design or material selection is warranted. As materials continue to be developed, whether specically for biomedical applications or in some different discipline, the selection of biomaterials for implants will remain a challenge in the design of the optimum implant. The evolution of tissue engineering from a bench-top science to a clinically workable tool for new implant design will also open new doors
1192
SELECTION OF MATERIALS FOR BIOMEDICAL APPLICATIONS
for the development and use of biomaterials. In all of these cases, however, the same principles apply to the selection of a material for a biomedical application. The selection process can be summarized in the following way: 1. Determine the functional requirements of the material for the particular application (preferably with an idea of the overall design in hand). 2. Select a group of materials that appear to meet those functional requirements and ensure that all conrming tests are conducted in an environment that simulates human physiology. 3. Determine the biocompatibility of the materials in terms of material degradation, tissue effects, blood compatibility, implant xation, and longterm physiologic consequences. 4. Complete the design and approval process, with mechanisms in place to obtain data on functional or material complications for many years after clinical use is initiated.
Co py rig hte dM ate ria l
As with all aspects of engineering design, selection of materials for biomedical implants is like solving a puzzlegiven all of the goals and constraints, what is the one solution that best answers the question that has been posed? And if a current solution does not exist, can one be developed? Some may argue that careful selection of materials for medical applications is more important than for other realms of engineering, due primarily to the overriding fear most people have of disease or injury. Others may disagree. It is certain, however, that development, evaluation, and selection of biomaterials is one of the most challenging areas of materials science. No two physiologic environments are exactly the same; therefore, no two implants will respond in exactly the same way. It is also much more difcult to predict the loading, chemical, and biological environment that an implant will see in a particular individual than it is to model the potential variations in loading of a car or a building. The science of biomedical materials has improved tremendously since the days of George Washingtons wooden teethand the development of new materials has just begun.
BIBLIOGRAPHY
ASTM-F136, Standard Specication for Wrought Titanium-6 Aluminum-4 Vanadium ELI (Extra Low Interstitial) Alloy (UNS R56401) for Surgical Implant Applications, American Society for Testing and Materials, W. Conshohocken, PA, 1998. ASTM-F562, Standard Specication for Wrought Cobalt-35 Nickel-20 Chromium-10 Molybdenum Alloy for Surgical Implant Applications, American Society for Testing and Materials, W. Conshohocken, PA, 2000. ASTM-F648, Standard Specication for Ultra-High-Molecular-Weight Polyethylene Powder and Fabricated Form for Surgical Implants, American Society for Testing and Materials, W. Conshohocken, PA, 2000. Baier, R. E., Blood Compatibility of Synthetic Polymers: Perspectives and Problems. in Polymers in Medicine and Surgery, R. L. Kronenthal, Z. Osei, and E. Martin (eds.), Plenum, New York, 1975, pp. 139159. Bernache-Assolant, D., Bioceramics: Processing-Properties, in Biomaterials Degradation: Fundamental Aspects and Related Clinical Phenomena, M. A. Barbosa (ed.), Elsevier Science Publishers, Amsterdam, 1991, pp. 111168. Black, J., Biological Performance of Materials: Fundamentals of Biocompatibility, Marcel Dekker, New York, 1999.
Copyright 2002 John Wiley & Sons Retrieved from: www.knovel.com
BIBLIOGRAPHY
1193
Bruck, S. D., Properties of Biomaterials in the Physiological Environment, CRC Press, Boca Raton, 1980. Bruck, S. D., Rabin, S., and Ferguson, R. J., Evaluation of Biocompatible Materials, Biomaterials, Medical Devices, and Articial Organs, 1(1), 191222 (1973). Brunski, J. B., Classes of Materials Used in Medicine: Metals, in Biomaterials Science: An Introduction to Materials in Medicine, B. D. Ratner, A. S. Hoffman, F. J. Schoen, and J. E. Lemons (eds.), Academic, San Diego, 1996. Center, J. R., Nguyen, T. V., Pocock, N. A., Noakes, K. A., Kelly, P. J., Eisman, J. A., and Sambrook, P. N., Femoral Neck Axis Length Height Loss and Risk of Hip Fracture in Men and Women, Osteoporosis Int., 8(1), 7581 (1998). Chignier, E., Monties, J. R., Butazzoni, B., Dureau, G., and Eloy, R., Haemocompatibility and Biological Course of Carbonaceous Composites for Cardiovascular Devices, Biomaterials, 8(1), 1823 (1987). Chupa, J. M., Foster, A. M., Sumner, S. R., Madihally, S. V., and Matthew, H. W., Vascular Cell Response to Polysaccharide Materials: In Vitro and In Vivo Evaluation, Biomaterials, 21(22), 23152222 (2000). Collins, G. J., Thrombosis, in Vascular Grafting: Clinical Applications and Techniques, C. B. Wright, R. W. Hobson, II, L. F. Hiratzka, and T. G. Lynch (eds.), John Wright PSG, Boston, 1983, pp. 245274. Consigny, P. M., Endothelial Cell Seeding on Prosthetic Surfaces, J. Long Term Effects of Medical Implants, 10(12), 7995 (2000). Cowin, S. C., Mechanical Properties of Cortical Bone, in Structure and Function of Cortical Bone, S. C. Cowin (ed.), CRC Press, Boca Raton, FL, 1989, pp. 97127. Cronin, T. D., Silicone Breast Implants, in Biomaterials in Reconstructive Surgery, L. R. Rubin (ed.), Mosby, St. Louis, 1983, pp. 552563. Delaunay, C., Second Generation Metallic Bearings in Cementless Primary Total Hip Arthroplasty: Rationale, Homologation, and Preliminary Results, Rev. Chir. Orthop. Reparatrice Appar. Mot., 86(8), 809824 (2000). Dukes, C. E., and Mitchley, B. C., Polyvinyl Sponge Implants: Experimental and Clinical Observations, Brit. J. Plastic Surgery, 15, 225 (1962). Edgerton, M. I., and McClary, A. R., Augmentation Mammoplasty with Specic Reference to Use of Polyvinyl Alcohol (Ivalon) Sponge, Plastic and Reconstructive Surgery, 21, 279 (1958). Edwards, W. S., Teon Grafts, in: Vascular Grafting: Clinical Applications and Techniques, C. B. Wright, R. W. Hobson, II, L. F. Hiratzka, and T. G. Lynch (eds.), John Wright PSG, Boston, 1983, pp. 2730. Forbes, C. D., Articial SurfacesBlood Interactions, J. Medical Eng. Tech., 17(5), 190193 (1993). Forster, R., Mutagenicity Testing and Biomaterials, in Techniques of Biocompatibility Testing, Vol. 2, D. F. Williams (ed.), CRC Press, Boca Raton, FL, 1986, pp. 137149. Frisch, E. E., Technology of Silicones in Biomedical Applications, in Biomaterials in Reconstructive Surgery, L. R. Rubin (ed.), Mosby, St. Louis, 1983, pp. 7390. Herring, M. B., Endothelial Seeding of Blood Flow Surfaces, in Vascular Grafting: Clinical Applications and Techniques, C. B. Wright, R. W. Hobson, II, L. F. Hiratzka, and T. G. Lynch, eds., John Wright PSG, Boston, 1983, pp. 275314. Hershko, C., Link, G., and Cabantchik, J., Pathophysiology of Iron Overload, Ann. New York Acad. Sci., 850, 191201 (1998). Hufnagel, C. A., Experimental, Preclinical, and Clinical Pretesting of Vascular Prostheses, in C. B. Wright, R. W. Hobson II, L. F. Hiratzka, and T. G. Lynch (eds.), Vascular Grafting: Clinical Applications and Techniques, John Wright PSG, Boston, 1983, pp. 2326. ISO-7206, Implants for SurgeryPartial and Total Hip Joint Replacement. Methods for Determination of Endurance Properties with Application of Torsion, International Standards Organization, Geneva, 1989. ISO-10993, Biological Evaluation of Medical Devices, International Standards Organization, Geneva, 19922000. Jacobs, J. J., Shanbhag, A., Glant, T. T., Black, J., and Galante, J. O., Wear Debris in Total Joint Replacement, J. Am. Acad. Orthopaedic Surgery, 2(4), 212220 (1994). Merritt, K., Immunological Testing of Biomaterials, in Techniques in Biocompatibility Testing, Vol. 2, D. F. Williams (ed.), CRC Press, Boca Raton, FL, 1986, pp. 123136.
Co py rig hte dM ate ria l
Copyright 2002 John Wiley & Sons Retrieved from: www.knovel.com
1194
SELECTION OF MATERIALS FOR BIOMEDICAL APPLICATIONS
Co py rig hte dM ate ria l
Copyright 2002 John Wiley & Sons Retrieved from: www.knovel.com
Mergerman, J., and Abbott, W. M., Compliance in Vascular Grafts, in C. B. Wright, R. W. Hobson II, L. F. Hiratzka, and T. G. Lynch (eds.), Vascular Grafting: Clinical Applications and Techniques, John Wright PSG, Boston, 1983, pp. 344364. Park, J. B., and Lakes, R. S., Biomaterials: An Introduction, Plenum, New York, 1992. Paul, J. P., Strength Requirements for Internal and External Prosthetics, J. Biomech., 32(4), 381 393 (1999). Plenk, H., Jr., Bohler, M., Walter, A., Knahr, K., and Saltzer, M., 15 Years Experiences with Alu mina-Ceramic Total Hip Joint Endo-Prostheses. A Clinical, Histological, and Tribological Analysis, in Bioceramics and the Human Body, A. Ravaglioli and A. Krajewsk, (eds.), Elsevier Applied Science, New York, 1992, pp. 1725. Ravaglioli, A., and Krajewsk, A., Skeletal Implants: From Metals, to Polymers, to Ceramics, in Bioceramics in the Human Body, A. Ravaglioli and A. Krajewsk (eds.), Elsevier Applied Science, New York, 1992, pp. 116. Rose, R. M., and Litske, A. S., Biomechanical Considerations in the Loosening of Hip Replacement Prostheses, in: Current Perspectives on Implantable Devices, Vol. 1, D. F. Williams (ed.), JAI Press, Greenwich, CT, 1989, pp. 145. Rubin, L. R., Degradation of the Saline-Filled Silicone-Bag Breast Implant, in Biomaterials in Reconstructive Surgery, L. R. Rubin (ed.), Mosby, St. Louis, 1983, pp. 260272. Sallam, A. M., and Hwang, N. H., Human Red Blood Cell Hemolysis in a Turbulent Shear Flow: Contribution of Reynolds Shear Stresses, Biorheology, 21(6), 783797 (1984). Sanan, A., and Haines, S. J., Repairing Holes in the Head: A History of Cranioplasty, Neurosurgery, 40(3), 588603 (1997). Sawye, P. N., Slaczewski, B., Mistry, F. D., Malik, L. N., and Jones, M. T., Analysis of Major Artery Vessel Replacements in Laboratory and Clinical Use, in Biomaterials in Reconstructive Surgery, L. R. Rubin (ed.), Mosby, St. Louis, 1983, pp. 689734. Sedel, L., Meunier, A., Nizard, R. S., and Witvoet, J., Ten Year Survivorship of Cemented CeramicCeramic Total Hip Replacements, in Bioceramics, Vol. 4, W. Boneld, G. W. Hastings, and K. E. Tanner (eds.), Butterworth-Heinemann, Oxford, 1991. Sharp, W. V., Present Status of Carbon Grafts, in Vascular Grafting: Clinical Applications and Techniques, C. B. Wright, R. W. Hobson II, L. F. Hiratzka, and T. G. Lynch (eds.), John Wright PSG, Boston, 1983, pp. 326330. Skinner, H. B., Ceramic Bearing Surfaces, Clin. Orthopaedics and Related Res., 369, 8391 (1999). Smith, G. K., Systemic Aspects of Metallic Implant Degradation, in Biomaterials in Reconstructive Surgery, L. R. Rubin (ed.), Mosby, St. Louis, 1983, pp. 229251. Snyder, R. W., Fabrication and Testing of Textile Vascular Prostheses, in Vascular Grafting: Clinical Applications and Techniques, C. B. Wright, R. W. Hobson II, L. F. Hiratzka, and T. G. Lynch, (eds.), John Wright PSG, Boston, 1983, pp. 1322. Streicher, R. M., Senlitsch, M., and Schon, R., Articulation of Ceramic Surfaces Against Polyeth ylene, in Bioceramics and the Human Body, A. Ravaglioli, and A. Krajewsk (eds.), Elsevier Applied Science, New York, 1992, pp. 118123. Swanson, S. A. V., The State of the Art in Joint Replacement, Part 1: Background and History, J. Med. Eng. Tech., 1(5), 255259 (1977). Wagner, M., and Wagner, H., Medium-Term Results of a Modern Metal-on-Metal System in Total Hip Replacement, Clin. Orthopaedics Related Res., 379, 123133 (2000). Wilkerson, D. K., and Zalina, M. A., Biomaterials Used in Peripheral Vascular Surgery. in Implantation Biology: The Host Response and Biomedical Devices, R. S. Greco, (ed.), CRC Press, Boca Raton, FL, 1994, pp. 179190. Willert, H. G., and Semlitsch, M., Tissue Reactions to Plastic and Metallic Wear Products of Joint Endoprostheses, Clin. Orthopaedics and Related Res., 333, 414 (1996). Wolff, J., Das Gesetz der Transformation der Knochen, Hirchwald, Berlin, 1892.
You might also like
- Clay MarbleDocument22 pagesClay Marblesciencystuff0% (1)
- Handbook of Materials For Medical DevicesDocument310 pagesHandbook of Materials For Medical DevicesRetal MohamedNo ratings yet
- Micro Carrier Cell Culture Principles and MethodsDocument140 pagesMicro Carrier Cell Culture Principles and MethodssciencystuffNo ratings yet
- 01 Metals BiomaterialsDocument121 pages01 Metals BiomaterialsM Kidam HadyNo ratings yet
- DI Pipe Catalogue JSAW 2019Document176 pagesDI Pipe Catalogue JSAW 2019Aneesh ConstantineNo ratings yet
- Friction Coefficient of Steel On Concrete or Grout PDFDocument7 pagesFriction Coefficient of Steel On Concrete or Grout PDFLuis Ernesto Ramirez OsorioNo ratings yet
- Flat Slab Formwork Falsework1Document80 pagesFlat Slab Formwork Falsework1Amin ZuraiqiNo ratings yet
- Highline Anchors 102 COMBINED 10-5-20Document81 pagesHighline Anchors 102 COMBINED 10-5-20steven cheungNo ratings yet
- Design Segmental Precast Linning Tunnel LiningDocument29 pagesDesign Segmental Precast Linning Tunnel LiningMirna KristiyantoNo ratings yet
- 1B. - Tension Members Ce134p - Escruz - LRFDDocument43 pages1B. - Tension Members Ce134p - Escruz - LRFDJed CernechezNo ratings yet
- Analysis of Carbon Fiber Reinforced Polymer Composite Hip Prosthesis Based On Static and Dynamic LoadingDocument6 pagesAnalysis of Carbon Fiber Reinforced Polymer Composite Hip Prosthesis Based On Static and Dynamic LoadingPraveen KumarNo ratings yet
- Design Specification and Material Selection of Total Hip ImplantsDocument14 pagesDesign Specification and Material Selection of Total Hip ImplantsMehmet DincerNo ratings yet
- Very Good To ReadDocument15 pagesVery Good To ReadGunall SNo ratings yet
- Andani 2014Document49 pagesAndani 2014qwerty fkvorkcjdkNo ratings yet
- Finite Element Investigation of The Loadin Grate Effect On The Spinal Load-Sharing Changes Under Impact ConditionsDocument11 pagesFinite Element Investigation of The Loadin Grate Effect On The Spinal Load-Sharing Changes Under Impact ConditionsNico FranckNo ratings yet
- Journal of Biomechanics: Junyan Li, Todd D. Stewart, Zhongmin Jin, Ruth K. Wilcox, John FisherDocument7 pagesJournal of Biomechanics: Junyan Li, Todd D. Stewart, Zhongmin Jin, Ruth K. Wilcox, John FisherRenka BlodersNo ratings yet
- MB41Document6 pagesMB41GERARDO TORRES RUIZNo ratings yet
- 2023 - Mechanical Characterization of A NovelDocument9 pages2023 - Mechanical Characterization of A NovelAbdelrahman AbdelgawadNo ratings yet
- Arrianna 1002162633 Assignment BEP1033Document44 pagesArrianna 1002162633 Assignment BEP1033Arrianna PeterNo ratings yet
- Jang 2008Document9 pagesJang 2008Marco Morillo RodríguezNo ratings yet
- New and ImportantDocument10 pagesNew and ImportantPrashanth GurramNo ratings yet
- Biomaterials Selection For A Joint Replacement CASBJREN21Document10 pagesBiomaterials Selection For A Joint Replacement CASBJREN21BerkanErolNo ratings yet
- What Can We Learn From Nature (No Está Tan Bueno)Document7 pagesWhat Can We Learn From Nature (No Está Tan Bueno)Paula CrociNo ratings yet
- Materials 14 04224 v3Document16 pagesMaterials 14 04224 v3B01Aadarsh SharmaNo ratings yet
- Titanium AlloysDocument19 pagesTitanium AlloysMila DevitaNo ratings yet
- Mechanical Properties of Compact Bone Defined by TDocument16 pagesMechanical Properties of Compact Bone Defined by T01fe18bme033No ratings yet
- Biomaterials in Hip Joint Replacement: June 2016Document14 pagesBiomaterials in Hip Joint Replacement: June 2016Muhammad Dilawar khanNo ratings yet
- Weizel 2020Document29 pagesWeizel 2020Weihao CaiNo ratings yet
- Puleo 1999Document11 pagesPuleo 1999Alejandro FereñoNo ratings yet
- Polymer Composites Bone CementsDocument20 pagesPolymer Composites Bone Cementshr granulabNo ratings yet
- Biomedical Applications of Polymer-Composite Materials, A ReviewDocument36 pagesBiomedical Applications of Polymer-Composite Materials, A ReviewMine Küçük100% (2)
- Hollensteiner2019 - Development of Open-Cell Polyurethane-Based Bone Surrogates ForDocument7 pagesHollensteiner2019 - Development of Open-Cell Polyurethane-Based Bone Surrogates Foridham05No ratings yet
- Materials For Hip Prostheses: A Review of Wear and Loading ConsiderationsDocument26 pagesMaterials For Hip Prostheses: A Review of Wear and Loading ConsiderationsEka NatsvlishviliNo ratings yet
- Mechanical Aspects of Dental ImplantDocument53 pagesMechanical Aspects of Dental ImplantFreddy BenalcázarNo ratings yet
- Overview of Biomaterials and Their Use in Medical Devices: Uses For Biomaterials (Ref 3)Document12 pagesOverview of Biomaterials and Their Use in Medical Devices: Uses For Biomaterials (Ref 3)rg1326No ratings yet
- Case Study Biomaterials Selection For A Joint ReplacementDocument8 pagesCase Study Biomaterials Selection For A Joint ReplacementBjarne Van haegenbergNo ratings yet
- Hybrid Ceramo-Polymeric Nano-Diamond Composites: February 2018Document18 pagesHybrid Ceramo-Polymeric Nano-Diamond Composites: February 2018Gerson JoelNo ratings yet
- Experimental Investigation of Maximum Stress Concentrations in A Femur Bone by Photoelastic ApproachDocument10 pagesExperimental Investigation of Maximum Stress Concentrations in A Femur Bone by Photoelastic ApproachMorteza AtaeiNo ratings yet
- Biomimetics: Finite Element Analysis of Orthopedic Hip Implant With Functionally Graded Bioinspired Lattice StructuresDocument16 pagesBiomimetics: Finite Element Analysis of Orthopedic Hip Implant With Functionally Graded Bioinspired Lattice StructuresAli Cem GöçerNo ratings yet
- Materials: Metallic Scaffolds For Bone RegenerationDocument43 pagesMaterials: Metallic Scaffolds For Bone RegenerationWookyoung LeeNo ratings yet
- Kim, Chang, Jung - 2010 - The Finite Element Analysis of A Fractured Tibia Applied by Composite Bone Plates Considering Contact ConditioDocument10 pagesKim, Chang, Jung - 2010 - The Finite Element Analysis of A Fractured Tibia Applied by Composite Bone Plates Considering Contact ConditioMorteza AtaeiNo ratings yet
- Article 2 - Bearing Surfaces in Hip ReplacementDocument6 pagesArticle 2 - Bearing Surfaces in Hip ReplacementAbishkar ShresthaNo ratings yet
- Medical Engineering and Physics: Girish Chandra, Ajay Pandey, Sushrut PandeyDocument11 pagesMedical Engineering and Physics: Girish Chandra, Ajay Pandey, Sushrut PandeyGirish Chandra DewanganNo ratings yet
- Manteghi 2017Document30 pagesManteghi 2017Sofiene helailiNo ratings yet
- Abel Chapter OneDocument6 pagesAbel Chapter OnebryanbotofficialmailNo ratings yet
- Halonen 2016Document32 pagesHalonen 2016sina salehpourNo ratings yet
- Modern Methods For Increasing Wear Resistance of Hip Prostheses SurfacesDocument8 pagesModern Methods For Increasing Wear Resistance of Hip Prostheses SurfacesSatria Adi NugrohoNo ratings yet
- Alloplastic Bone GraftsDocument62 pagesAlloplastic Bone GraftsMaysaa mahdiNo ratings yet
- J Tissue Eng Regen Med - 2014 - Detsch - The Role of Osteoclasts in Bone Tissue EngineeringDocument17 pagesJ Tissue Eng Regen Med - 2014 - Detsch - The Role of Osteoclasts in Bone Tissue EngineeringVinícius Gabriel da SilvaNo ratings yet
- Design and Characterization of A Scaffold For Bone Tissue EngineeringDocument46 pagesDesign and Characterization of A Scaffold For Bone Tissue EngineeringLelia Zahra ZakiyahNo ratings yet
- Analysis of Bone Tissue Mechanical Properties: Diana Mil I), Jadranka Keros and Andrija Bo (NjakDocument7 pagesAnalysis of Bone Tissue Mechanical Properties: Diana Mil I), Jadranka Keros and Andrija Bo (Njaksamuel rajNo ratings yet
- Bone and Metal An Orthopaedic Perspective On Osseointegration of MetalsDocument15 pagesBone and Metal An Orthopaedic Perspective On Osseointegration of MetalsClaudia UngureanuNo ratings yet
- Corrosion of Bio ImplantsDocument37 pagesCorrosion of Bio ImplantsDaniel de la CruzNo ratings yet
- A Review of Mechanical Properties of Scaffold in TDocument7 pagesA Review of Mechanical Properties of Scaffold in TeManNo ratings yet
- 1893 1896 PDFDocument4 pages1893 1896 PDFJoshua PooleNo ratings yet
- 4b PDFDocument43 pages4b PDFsbhushanarya2546No ratings yet
- Haug 1999Document7 pagesHaug 1999Desrainy InhardiniNo ratings yet
- Overview of Biomaterials and Their Use in Medical Devices: Uses For Biomaterials (Ref 3)Document6 pagesOverview of Biomaterials and Their Use in Medical Devices: Uses For Biomaterials (Ref 3)anwarr4040No ratings yet
- The Problem and Its ScopeDocument10 pagesThe Problem and Its Scope김나연No ratings yet
- J Apsusc 2017 02 185Document7 pagesJ Apsusc 2017 02 185pariNo ratings yet
- Periodontology 2000 - 2019 - Guglielmotti - Research on implants and osseointegrationDocument12 pagesPeriodontology 2000 - 2019 - Guglielmotti - Research on implants and osseointegrationalinagaxiolaariasNo ratings yet
- Total Knee Prosthesis - Final - Andaç - Anıl - ÇOBANDocument19 pagesTotal Knee Prosthesis - Final - Andaç - Anıl - ÇOBANAndaç ÇobanNo ratings yet
- Femoro-Acetabular Impingement. ClassificDocument10 pagesFemoro-Acetabular Impingement. ClassificPriscilla PriscillaNo ratings yet
- Biomimetic Porous Titanium Scaffolds For Orthopedic and Dental ApplicationsDocument36 pagesBiomimetic Porous Titanium Scaffolds For Orthopedic and Dental ApplicationsSocarisNo ratings yet
- Orthodontically Driven Corticotomy: Tissue Engineering to Enhance Orthodontic and Multidisciplinary TreatmentFrom EverandOrthodontically Driven Corticotomy: Tissue Engineering to Enhance Orthodontic and Multidisciplinary TreatmentFederico BrugnamiNo ratings yet
- Bone Remodeling Process: Mechanics, Biology, and Numerical ModelingFrom EverandBone Remodeling Process: Mechanics, Biology, and Numerical ModelingNo ratings yet
- Control of The Interferon Response in RNAi ExperimentsDocument29 pagesControl of The Interferon Response in RNAi ExperimentssciencystuffNo ratings yet
- Growing and Analyzing Static BiofilmsDocument18 pagesGrowing and Analyzing Static BiofilmsMoti BaumNo ratings yet
- Introduction To Molecular Biology - Anthony WeissDocument7 pagesIntroduction To Molecular Biology - Anthony WeisssciencystuffNo ratings yet
- Preparation of Human Leukocyte CulturesDocument1 pagePreparation of Human Leukocyte CulturessciencystuffNo ratings yet
- Introduction To Microbiology LaboratoryDocument16 pagesIntroduction To Microbiology LaboratorysciencystuffNo ratings yet
- Molecular EvolutionDocument134 pagesMolecular Evolutionsciencystuff100% (1)
- A Microplate Spectrofluorometric Assay For Bacterial BiofilmsDocument4 pagesA Microplate Spectrofluorometric Assay For Bacterial BiofilmssciencystuffNo ratings yet
- Introduction To Cell and Tissue CultureDocument314 pagesIntroduction To Cell and Tissue CultureSathiyaraj95% (19)
- HORTON MTT Cell Assay Protocol CheckpointDocument4 pagesHORTON MTT Cell Assay Protocol CheckpointaaaaustinNo ratings yet
- General Protocol For 2DPAGEDocument9 pagesGeneral Protocol For 2DPAGEsciencystuffNo ratings yet
- Glenmark Pharmaceuticals 13 DEC 2007Document4 pagesGlenmark Pharmaceuticals 13 DEC 2007sciencystuffNo ratings yet
- Computational Methods For Prediction of Drug LikenessDocument10 pagesComputational Methods For Prediction of Drug LikenesssciencystuffNo ratings yet
- Computational Molecular BiologyDocument28 pagesComputational Molecular BiologysciencystuffNo ratings yet
- Cell CultureDocument4 pagesCell CulturesaforatorkashvandNo ratings yet
- Antibiotic Resistance and The Susceptibility of Bacteria LabDocument19 pagesAntibiotic Resistance and The Susceptibility of Bacteria LabsciencystuffNo ratings yet
- Molbio PDFDocument9 pagesMolbio PDFRicardo GonzalezNo ratings yet
- Preparation of Human Leukocyte CulturesDocument1 pagePreparation of Human Leukocyte CulturessciencystuffNo ratings yet
- Application of AFM in Microbiology - A ReviewDocument13 pagesApplication of AFM in Microbiology - A ReviewsciencystuffNo ratings yet
- Fatigue Failure Theories ExplainedDocument32 pagesFatigue Failure Theories Explainedlth770310No ratings yet
- Ceramite Ins: Bauxite Refractory CastingsDocument2 pagesCeramite Ins: Bauxite Refractory CastingsSHRINIVASAN GTKNo ratings yet
- Characteristic Shear Strength Values For EC7Document8 pagesCharacteristic Shear Strength Values For EC7Brian ConnerNo ratings yet
- Bioplastic From Plant Starch AnalysisDocument3 pagesBioplastic From Plant Starch AnalysisViene XeloNo ratings yet
- Nature Materials Reviews Aug 2019 High-Entropy Alloys PDFDocument20 pagesNature Materials Reviews Aug 2019 High-Entropy Alloys PDFAnand Prakash SinghNo ratings yet
- Effect of Nano-Silica On Concrete Containing MetakaolinDocument9 pagesEffect of Nano-Silica On Concrete Containing MetakaolinIAEME PublicationNo ratings yet
- Optimum Design of Pile Foundation by Automatic Grouping Genetic AlgorithmsDocument18 pagesOptimum Design of Pile Foundation by Automatic Grouping Genetic AlgorithmsKatherine StuartNo ratings yet
- Kolmakov2021 Article MaterialsForBulletCoresDocument13 pagesKolmakov2021 Article MaterialsForBulletCoresM HzNo ratings yet
- MCQ Physics Regulations 2017Document18 pagesMCQ Physics Regulations 2017Thaya GanapathyNo ratings yet
- Technical Specifications For Bird Flight DiverterDocument19 pagesTechnical Specifications For Bird Flight DiverterVidyavathiDavuluriNo ratings yet
- Flust-Extended End Plate ConnectionDocument8 pagesFlust-Extended End Plate ConnectionamachmouchiNo ratings yet
- Construction Materials Properties and ApplicationsDocument9 pagesConstruction Materials Properties and ApplicationsEverson Murungweni0% (1)
- Ce6505 Svce QBDocument72 pagesCe6505 Svce QBdinu69inNo ratings yet
- HHPC in BridgeDocument12 pagesHHPC in BridgeAbrahamHidalgoBermúdezNo ratings yet
- Utilization of Recycled Crumb Rubber As Ne Aggregates in Concrete Mix DesignDocument6 pagesUtilization of Recycled Crumb Rubber As Ne Aggregates in Concrete Mix DesignGuzalgNo ratings yet
- Hilti Re500 Embedded LengthDocument1 pageHilti Re500 Embedded LengthPYAINo ratings yet
- Kerto Manual Bolted ConnectionsDocument17 pagesKerto Manual Bolted ConnectionsM Refaat FathNo ratings yet
- Core Shear Properties of Sandwich Constructions by Beam FlexureDocument8 pagesCore Shear Properties of Sandwich Constructions by Beam FlexureBarang TeknikNo ratings yet
- Final To PrintDocument63 pagesFinal To Printsamuel fekadeNo ratings yet
- SPH Bearing Draft (09.06.11)Document38 pagesSPH Bearing Draft (09.06.11)Dave ThompsonNo ratings yet
- Geotextil TencateDocument2 pagesGeotextil TencateHugo HiddNo ratings yet
- Effects of solution heat treatment on microstructure and mechanical properties of AZ61-0.7Si magnesium alloyDocument5 pagesEffects of solution heat treatment on microstructure and mechanical properties of AZ61-0.7Si magnesium alloysujit_sekharNo ratings yet
- Partial Replacement of Coarse Aggregates by ExpandedDocument4 pagesPartial Replacement of Coarse Aggregates by ExpandedInternational Journal of Research in Engineering and TechnologyNo ratings yet
- A Comprehensive Review On The Performance Analysis of Composite Overwrapped Pressure VesselsDocument16 pagesA Comprehensive Review On The Performance Analysis of Composite Overwrapped Pressure VesselsJosePPMolinaNo ratings yet