Professional Documents
Culture Documents
Parkinson's Disease Symptoms Are Differentially Affected by Massage Therapy vs. Progressive Muscle Rel
Uploaded by
ARCHON SCAROriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Parkinson's Disease Symptoms Are Differentially Affected by Massage Therapy vs. Progressive Muscle Rel
Uploaded by
ARCHON SCARCopyright:
Available Formats
MASSAGE: RESEARCH
Parkinsons disease symptoms are dierentially aected by massage therapy vs. progressive muscle relaxation: a pilot study
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Maria Hernandez-Reif, Tiany Field, Shay Largie, Christy Cullen, Julia Beutler, Chris Sanders, William Weiner, Dinorah Rodriguez-Bateman, Lisette Zelaya, Saul Schanberg, Cynthia Kuhn
Abstract Sixteen adults diagnosed with idiopathic Parkinsons disease (M age=58) received 30-min massage therapy or progressive muscle relaxation exercise sessions twice a week for 5 weeks (10 sessions total). Physicians rated participants in the massage therapy group as improved in daily living activities by the end of the study. The massaged group also rated themselves as improved in daily functioning, and having more eective and less disturbed sleep. Urine samples revealed that at the end of the 10 sessions, the massage therapy group had lower norepinephrine and epinephrine (stress hormone) levels, suggesting they were less stressed. The progressive muscle relaxation group had higher dopamine levels, which is interesting in that Parkinsons is associated with a decrease in dopamine. The relaxation group also showed higher epinephrine levels, suggesting that although the relaxation exercises might have been benecial, some Parkinsons participants might have found the relaxation technique stressful. r 2002 Elsevier Science Ltd. All rights reserved.
Maria Hernandez-Reif, Tiany Field, Shay Largie, Christy Cullen, Julia Beutler, Chris Sanders Touch Research Institutes, USA William Weiner, Dinorah Rodriguez-Bateman, Lisette Zelaya Department of Neurology, University of Miami School of Medicine, USA Saul Schanberg and Cynthia Kuhn Department of Pharmacology, Duke University, USA
........................................... Journal of Bodywork and Movement Therapies (2002) 6(3),177^182 r 2002 Elsevier Science Ltd. All rights reserved. doi: 10.1054/jbmt.2002.0282, available online at http://www.idealibrary.com on
Parkinsons Symptoms are Reduced by Massage Therapy
Idiopathic Parkinsons disease (PD), a progressive central nervous system disorder, aects approximately 50,000 Americans every year, or one in every 100 Americans over the age of 60 (The National Institute of Neurological Disorders and Stroke of the National Institutes of Health
177
2000). Characteristic symptoms of PD include tremors, rigidity, bradykinesia (or slowness in executing movements) and dopamine deciency (Lien & Mutch 1997). Other symptoms that impact quality of life include diculty concentrating, impaired daily living activities, fatigue and diculty sleeping (Herndon et al. 2000; Pal et al. 2001; Tom & Cummings 1998).
J O U R NAL O F B O DY WO R K A N D MOV E M E N T TH E R API E S JULY 20 02
Hernandez-Reif et al.
Standard medical care for individuals with PD includes oral Levodopa (L-dopa), which acts like a neurotransmitter and leads to an increase in brain dopamine (Chase 1998; Jenner & Brin 1998). Dopamine is essential in modulating motor functioning and substance P (that causes pain) in the basal ganglia pathways (Contreras et al. 1998). However, L-dopa therapy may rapidly advance symptoms in a mild-to-moderate PD patient (Chase 1998; Fariello 1998). Other aversive eects of L-dopa include motor uctuations and dyskinesias (involuntary limb and facial movements) (Chase 1998; Jenner & Brin 1998; Koller, 1998) and possible cell degeneration (Jenner & Brin 1998, Contreras et al. 1998). Moreover, the ecacy of the drug diminishes with prolonged use (Chase 1998). Other medications (e.g., Selegiline) used to reduce PD symptoms also feature side eects including dizziness, insomnia, nausea and headache (Rinne et al. 1998). Alternative therapies may attenuate side eects of PD without some of the adverse eects of drug therapy. For example, lowfrequency muscle stimulation, or electroconvulsive therapy, and magnetic stimulation/pulse therapy have been shown to reduce rigidity (Henneberg 1998; Wengel et al. 1998), and music therapy has been shown to attenuate emotional distress and improve motor functions and quality of life in patients with Parkinsons disease (Pacchetti et al. 1998). Massage therapy may also reduce symptoms associated with PD based on previous research. For example, massage therapy decreased fatigue, improved sleep, and led to changes in urinary biochemical levels, including increased urinary dopamine and/or serotonin levels for patients with eating disorders (e.g., anorexia and bulimia nervosa)
(Field et al. 1998; Hart et al. 2001), chronic fatigue syndrome (Field et al. 1997), chronic lower back pain (Hernandez-Reif et al. 2000), migraine headaches (HernandezReif et al. 1998a), bromyalgia (Sunshine et al. 1996), and for pregnant women (Field et al. 2000). In addition, massage therapy enhanced activities of daily living (self-care and household activities) in individuals with multiple sclerosis (Hernandez-Reif et al. 1998b). The purpose of the present study was to examine massage therapy as compared to progressive muscle relaxation eects on disease-related symptoms and biochemical levels in individuals with Parkinsons disease. Specically, massage therapy was expected to stabilize disease progression, improve sleep and daily living activities in individuals with Parkinsons. A progressive muscle exercise group was included as an attention control comparison group.
severe) and (3) medication stability for the month prior to admission into the study. Exclusion criteria included: (1) initiation of levodopa (L-dopa) therapy, (2) severe resting tremor with the UPDRS tremor score in one location X3, (3) signs of dementia (score of 2, 3, or 4 on item 1 of UPDRS), (4) psychiatric disorders, (5) drug or alcohol dependence, (6) participation in any other clinical study within 30 days prior to screening, and (7) any other concomitant diseases. Following stratication for disease severity and dyskinesias, assessed via the UPDRS, 16 participants (n=8 females) were randomly assigned to a massage therapy or progressive muscle relaxation group. The participants were from middle socioeconomic class as rated on the Hollingshead Two Factor Index (M=2.4) and were ethnically distributed, 69% Caucasian and 31% Hispanic. Demographic data did not dier between groups (all ps40.10). Procedures Massage therapy Participants in this group received two 30-min sessions a week for 5 weeks by a trained massage therapist. The massage therapy included the following steps with the patient in the prone position for the rst 15 min: Back: (1) long gliding strokes to the back (2 min); (2) kneading and friction of the shoulder area and upper arms and then general kneading to the back muscles (3 min) ; Buttocks: (1) kneading and pressure to the gluteal muscle area, including application of pressure to specic points where muscle tightness or tender points are noted until the muscles relax, (2 min); (2) friction to tight tendons (1 min); Ribs: stretching small muscles between the ribs (1 min) ; Thigh: kneading, friction and tendon stretches to the
Method
Participants Sixteen adults (M=58 years, SD=12.5) in the early stages of PD (M=1.84, SD=0.30 on the Hoehn Yahr scale 1967) were recruited at a PD treatment center. The Severity Stage Classication Scale (HoehnYahr, 1967) grades Parkinsons disease severity in the individual from 0 (asymptomatic) to 3 (mildto-moderate bilateral involvement) to 5 (wheelchair bound or bedridden). This scale was administered in conjunction with the Unied Parkinsons Disease Rating Scale (UPDRS) (Martinez-Martin et al. 1991) and Schwabb and England scale (1958) to screen for inclusion/ exclusion criteria. Inclusion criteria included: (1) Idiopathic PD age between 50- and 70-years old, (2) r stage 2.5 on the HoehnYahr scale (a disease severity scale from 1 to 5, with 1 being mild and 5 being
178
J O U R NAL O F B O DY WO R K A N D MOV E M E N T TH E R API E S JULY 20 02
Parkinsons disease
hamstrings (2 min); Calf: kneading and friction to the back of the calf with emphasis on the Achilles tendon, attending to tight areas or tender points found (2 min); Feet: (1) general kneading of the feet; (2) with the knee slightly bent, exing the foot toward the back of the calf (2 min). With participant in the supine position for the nal 15 min: Thigh: (1) friction and pressure to the front, upper thigh area, including applying pressure to specic points where muscle tightness or tender points are noted until muscles relax (2 min), (2) friction to the small muscles focused just above the knee (1 min); Lower leg: stretching (longitudinal and transverse) and small nger kneading of the underside of the leg (2 min); Feet: kneading the foot followed by exing the foot to stretch the Achilles tendon (1 min); Range of motion: taking each joint (hips, knees, ankles and toes) into exion and lightly into other ranges of motion (2 min); Hands: kneading the hands and ngers (1 min); Forearms: kneading and friction to tendons and muscles (1 min); Upper arms: kneading and friction to biceps and triceps (2 min); Neck: gentle squeezing of muscle immediately inferior to the hairline with moderate pressure, using caution to avoid the major blood vessels (1 min); Face: circular ngertip kneading to the face, especially the forehead, under the eyes (all around the eyes) and around the jaw (1 min); Head: scalp kneading (i.e., shampooing) (1 min). Progressive muscle relaxation The attention control group received progressive muscle relaxation therapy that consisted of the participants lying on their back while listening to a cassette tape leading them through the exercise steps. These 30-min sessions involved the participant tightening and then relaxing the same large
muscle groups that were massaged in the massage group starting at the feet and progressing to the face. The muscle groups that were exercised included the feet, calves, thighs, back, arms (including hands), and face. Assessments First day/last day measures (longterm eects) On the rst and last days of the study, participants (1) were rated by their physicians, (2) completed selfreports on functioning, sleep and fatigue and (3) provided a urine sample to assay biochemical levels. Physicians diagnostic assessments The following scale was completed by the participants physician who was unaware of their patients group assignment. Although having one physician rate all participants would have been optimal, this was not feasible. It is also possible that more accurate ratings were made because the participants physician was more familiar with the participants clinical condition. Physicians treatment assessment Activities of daily life scale (Schwab & England1958) This scale rated at 10% increments measures the amount of daily living activities a PD patient can perform. For example, a score of 100% reects complete independence and normal performance of chores and a score of 40% identies a patient who is very dependent, can conduct few chores alone but can assist with all chores. Reliability for this scale is acceptable (0.81) (Schwab & England 1958). High concurrent validity (p o0.001) has been established between the UPDRS and the Schwabb and England
179
Activities of Daily Life Scale (Martinez-Martin et al. 1991; Shwab & England, 1958).
Self-reports Activities of Daily Life Scale (Schwab & England1958). Same as the physicians scale. Sleep Scale (Verran & SnyderHalperin1988) Questions on this 15-item scale are rated on a visual analogue anchored at one end with eective sleep responses (e.g., Did not awaken, Had no trouble sleeping) and at the opposite end with ineective responses (e.g., Was awake 10 hours, Had a lot of trouble falling asleep). Participants marked the line at the point that best reected their last nights sleep. The scale yields subcategories of sleep disturbance (I had a lot of trouble with disrupted sleep), sleep eectiveness (Awoke refreshed) and supplementary sleep (After morning awakening, stayed awake). A reliability coecient of 0.82 has been reported for this scale (Verran & Snyder-Halperin 1988). Urine samples These were collected early in the morning on the rst and last days of the study to assess treatment eects on biochemistry levels. An aliquot of each sample was frozen and sent to Duke University. The aliquot of urine using a Biorex-70 column was extracted and analyzed by highpressure liquid chromatography with electrochemical detection (HPLC-ECD). Based on previous massage therapy studies, participants in the massage group were expected to show decreased cortisol, norepinephrine and epinephrine and increased dopamine and serotonin levels by the end of the 5-week period.
J O U R NAL O F B O DY WO R K A N D MOV E M E N T TH E R API E S JULY 20 02
Hernandez-Reif et al.
Results
Physicians diagnostic assessments An analysis of variance (ANOVA) revealed no baseline dierences between the two groups on the Unied Parkinsons disease rating Scale (Massage M=38.4, SD=18.6; Exercise M=37.0, SD=13.7) or the Severity Stage Classication Scale (HoehnYahr) , (Massage M=1.9, SD=0.4; Exercise M=1.8, SD =0.3), suggesting that the stratication procedure was successful. First vs. last day measures Because of the small sample size, non-parametric Wilcoxon Signed Ranks paired t-tests were conducted for the massage therapy and progressive muscle relaxation exercise group separately for the following measures.
Table 1 Means (and standard deviations in parentheses) for the Physicians Diagnostic Scale for the MassageTherapy and Progressive Muscle Relaxation Exercise groups Massage Variables First day Last day p-value Relaxation exercise First day Last day p-value r 89(8.6)a 89(8.9)
a
Activities of Daily Life Scale (Schwab & England) Physician rating (%) Subject rating (%) 87(7.1)a 87(7.1)
a
91(8.2)b 91(8.2)
b
0.05 0.05
87(6.8)a 89(5.5)a
NS NS
Note: Dierent letter superscripts denote dierences in means (within group) for that variable.
Urinary measures Wilcoxon Signed Ranks tests revealed (1) reduced norepinephrine (stress hormone) levels, Z=2.10, p o 0.05, and reduced epinephrine (stress hormone) levels, Z=1.96, p r 0.05, for the massage therapy group, and (2) increased dopamine values, Z=2.52, p o 0.05 and epinephrine (stress hormone) values, Z=2.52, p o0.05 for the exercise group.
Discussion
Physicians assessments The physicians rated the participants in the massage therapy group as improved on the Activities of Daily Life Scale, Z=1.90, p o0.05 (one-tailed), and the massage therapy participants also reported improved scores for this measure, Z=1.73, p o 0.05 (one-tailed), suggesting greater independence and more normal functioning on chores (see Table 1). Self-reports Sleep scale. Less sleep disturbance was reported by the massage therapy group for the last day of the study, Z=2.52, p o 0.01. Both the massage therapy group, Z=1.90, p o 0.05, and the progressive muscle relaxation group, Z=2.0, p o 0.05, reported more eective sleep by the end of the study (see Table 2). Following a 5-week massage therapy program, ratings of physician and self-ratings improved for the massage therapy group on the Activities of Daily Life Scale, suggesting slight improvement in increased independence and functioning on chores. These data are consistent with previous research showing improvement on activities of daily living following massage therapy, for example, for patients with multiple sclerosis (HernandezReif et al. 1998b) and spinal cord injuries (Diego et al. 2002). Taken together, these ndings suggest that massage therapy may enhance some level of functioning in progressive or degenerative central nervous system disorders or conditions. The lack of improvement for the progressive muscle relaxation group may relate to the possibility that the participants had little or no relaxation exercises prior to the
180
study and/or found the progressive muscle relaxation exercises fatiguing. Both groups reported more eective sleep for the last day of the study and the massage therapy group reported less sleep disturbance as well. Improved sleep following massage therapy has been reported in other studies for individuals with Chronic Fatigue Syndrome (Field et al. 1997), Fibromyalgia Syndrome (Sunshine et al. 1996) and Migraine headaches (Hernandez-Reif et al. 1998a). The report of less sleep disturbance by the massage therapy group might have reected their more relaxed state as evidenced by their decreased urinary norepinephrine and epinephrine (stress hormone) levels at the end of the study. Of additional interest were the ndings of increased dopamine levels and epinephrine (stress hormone) for the progressive muscle relaxation group. That progressive muscle relaxation exercises were associated with increased dopamine levels is encouraging in that Parkinsons disease is characterized by the progressive death of dopaminergic neurons, which leads to decrease in the overall dopamine content (Tekumalla et al. 2001). Why massage therapy was not associated with increased dopamine levels in this study is unclear, as it has been shown to increase in other groups (see Field et al. 1998).
J O U R NAL O F B O DY WO R K A N D MOV E M E N T TH E R API E S JULY 20 02
Parkinsons disease
Table 2 Means (and standard deviations in parentheses) for the Self-Report and Biochemistry measures for the MassageTherapy and Progressive Muscle Relaxation Exercise groups Massage Variables Sleep Scale Disturbance* Eective Supplementary Biochemistry Creatinine 5-HIAA Cortisol Norepinephrine Epinephrine Dopamine 0.99(.79)a 3953(942) 245(94)a 48(30)a 7(9) a 208 (146)a
a
Relaxation Exercise p-value First day Last day p-value r
First day
Last day
42.4(10.9)a 47.1(12.8) 7.9(9.6)a
a
22.4(14.3)b 61.8(12.0)
b
0.01 0.05 NS
33.8(25.0)a 43.8(11.5)
a
28.5(14.7)a 60.9(20.9)b 19.6(23.9)a
NS 0.05 NS
19.5(23.2)a
18.3(19.2)a
0.68(.28)a 3498(772) 218(36)a 25(18)b 12(9)b 174 (110)a
a
NS NS NS 0.05 0.05 NS
1.1(.74)a 4791(2575) 257(144)a 25(18)a 8 (6)a 153 (97)a
a
1.2(.69)a 4596(3778) 254(132)a 33(14)a 14 (8)b 280(131) b
a
NS NS NS NS 0.05 0.05
Note:* Lower score is optimal. Dierent letter superscripts denote dierences in means (within group) for that variable.
Perhaps, initial level eects were operating in that the massage therapy group level was higher than the relaxation group level at the start of the study, and the groups dopamine levels moved in the opposite direction. The increased epinephrine values in the exercise group suggest that the progressive muscle relaxation exercise might have also stressed the Parkinsons disease participants. Future research might also consider including a standard care control group and larger sample sizes, as the small sample size for the current study warrants caution in interpreting the ndings. Additional measures might include massage and movement therapies eect for reducing tremors, dyskinesias, rigidity (hypertonicity), and bradykinesia (or slowness in executing movements). In at least one study, massage therapy reduced hypertonicity (in young children with cerebral palsy), and spasticity (Hernandez-Reif et al. 2001). In sum, the preliminary ndings from this pilot study support the use of massage therapy for central nervous system disorders like Parkinsons
disease to ameliorate symptoms associated with the disease and to improve sleep and activities of daily living. Acknowledgements
We would like to thank the participants and the massage therapist volunteers in this study. Special thanks are extended to Iris Burman from Educating Hands and Diana Grin from SutherlandChan School of Massage in Toronto for designing the massage routine. This research was supported by an NIMH Senior Research Scientist Award (#MH00331) to Tiany Field and funding from Johnson & Johnson to the Touch Research Institutes. Correspondence and requests for reprints should be sent to Maria Hernandez-Reif, Ph.D., Touch Research Institutes, University of Miami School of Medicine, PO Box 016820(D-820), Miami, FL 33101. E-mail:mhernan4@med.miami.edu
REFERENCES
Chase T 1998 The signicance of continuance dopaminergic stimulation of Parkinsons disease. Drugs 55: 19 181
Contreras V, Pohluha P, Telulings H, Stelmach G 1998 Neural dynamics of short and medium-term motor control eects of levodopa therapy in Parkinsons disease. Articial Intelligence and Medicine 13: 5779 Diego M, Field T, Hernandez-Reif M, Field T, Brucker B, Hart S, Burman I 2002 Spinal cord injury benets from massage therapy. International Journal of Neuroscience 112: 133142 Fariello R 1998 Pharmacodynamic and pharmocokinetic features of cabergoline: rationale for use in Parkinsons disease. Drugs 55: 1016 Field T, Hernandez-Reif M, Hart S, Theakston H, Schanberg S, Kuhn C 2000 Pregnant women benet from massage therapy. Journal of Psychosomatic Obstetrics and Gynecology 20: 3138 Field T, Schanberg S, Kuhn C, Field T, Fierro K, Hentele T, Mueller C, Yando R, Shaw S, Burman I 1998. Bulimic adolescents benet from massage therapy. Adolescence 33: 555563 Field T, Sunshine W, Hernandez-Reif M, Quintino O, Schanberg S, Kuhn C, Burman I 1997 Massage therapy eects on depression in chronic fatigue syndrome. Journal of Chronic Fatigue Syndrome 3: 4351 Hart S, Field T, Hernandez-Reif M, Shaw S, Schanberg S, Kuhn C 2001 Anorexia nervosa symptoms are reduced by massage therapy. Eating Disorders 9: 217228
J O U R NAL O F B O DY WO R K A N D MOV E M E N T TH E R API E S JULY 20 02
Hernandez-Reif et al.
Henneberg A 1998 Additional therapies in Parkinsons disease patomets: Useful tools for the improvement of the quality of life or senseless loss of resources. Journal of Neurology 245: 2327 Hernandez-Reif M, Dieter J, Field T, Swerdlow B, Diego M 1998a Migraine headaches are reduced by massage therapy. International Journal of Neuroscience 96: 111 Hernandez-Reif M, Field T, Field T, Theakston H 1998b Multiple Sclerosis patients benet from massage therapy. Journal of Bodywork and Movement Therapies 2: 168174 Hernandez-Reif M, Field T, Krasnegor J, Theakston H, Burman I 2000 Lower back pain is reduced and range of motion increased after massage therapy. International Journal of Neuroscience 106: 115 Hernandez-Reif M, Field T, Largie S, Diego M, Manigat N, Seoanes J, Bornstein J 2001 Cerebral palsy symptoms in children decreased following massage therapy (in review) Herndon C, Young K, Herndon A, Dole E 2000 Parkinsons disease revisited. Journal of Neuroscience and Nursing 32: 216221 Hoehn M, Yahr M 1967 Parkinsonism: onset, progression, and mortality. Neurology 17: 427442
Jenner P, Brin M 1998 Levodopa neuorotoxicity: experimental studies versus clinical relevance. Neurology 50: 3948 Koller W 1998 Neuroprotection for Parkinsons disease. Annals of Neurology 13: 155159 Lien C, Mutch W 1997 The treatment of Parkinsons disease in older people. Scottish Medical Journal 194: 147150 Martinez-Martin P, Gil-Nagel A, Balseiro J et al 1991 Estudio comparativo de dos escalas para la enfermedad de Parkinson: la NEV frente a la UPDS. Reunion Extraordinaria de la Sociedad Espanola de Neurologia, Bilbao National Institute of Neurological Disorders and Stroke of the National Institutes of Health 2000 Parkinsons Disease: Hope Through Research. NIH Publication Bethesda, MD, USA. June 2000 Pacchetti C, Aglieri R, Mancini F, Martignoni E, Nappi G 1998 Active music therapy and Parkinsons disease: methods. Functional Neurology 13: 5767 Pal S, Bhattacharya K, Agapito C, Chaudhuri K 2001 A study of excessive daytime sleepiness and its clinical signicance in three groups of Parkinsons disease patients taking pramipexole, cabergoline and levodopa mono and combination therapy.
Journal of Neural Trasmission 108: 7177 Rinne U, Bracco F, Chouza C, Dupont E, Gershanik O, Marti Masso J, Montastru J Marsden C 1998 Safety of selegiline in the treatment of Parkinsons disease. Drug Safety 55: 1122 Scwhab R, England A 1958 Parkinsons Disease. Journal of Chronic Diseases 8: 488 Sunshine W, Field T, Quintino O, Fierro K, Kuhn C, Burman I, Schanberg S 1996 Fibromyalgia benets from massage therapy and transcutaneous electrical stimulation. Journal of Clinical Rheumatology 2: 18222 Tekumalla P, Calon F, Rahman Z et al 2001 Elevated levels of DFosB and RGS9 in Stratium in Parkinsons disease. Biological Psychiatry 50: 813816 Tom T, Cummings J 1998 Depression in Parkinsons disease. Pharmacological characteristics and treatment. Drugs and Aging 50: 5574 Verran J, Snyder-Halperin R 1988 Do patients sleep in the hospital? Applied Nursing Research 1: 95 Wengel S, Burke W, Pfeier R, Roccaforte W, Paige S 1998 Maintenance electroconvulsive therapy for intractable Parkinsons disease. The American Journal of Geriatric Psychiatry 6: 263269
182
J O U R NAL O F B O DY WO R K A N D MOV E M E N T TH E R API E S JULY 20 02
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Gastronomia 10 Competition GuideDocument21 pagesGastronomia 10 Competition Guidefpvillanueva100% (1)
- AP000100 EngDocument9 pagesAP000100 EngLucas WrightNo ratings yet
- My Study Plan Guide For AmcDocument7 pagesMy Study Plan Guide For Amc0d&H 8No ratings yet
- Abas 3 Chapter 5Document62 pagesAbas 3 Chapter 5GF David SalasNo ratings yet
- Shot List SLMDocument4 pagesShot List SLMARCHON SCARNo ratings yet
- Ironsworn Assets Master Set PDFDocument20 pagesIronsworn Assets Master Set PDFSophy RamirezNo ratings yet
- A4 Storyboard Template - 16-Panel - Portrait - StudioBinderDocument1 pageA4 Storyboard Template - 16-Panel - Portrait - StudioBinderSantiago Olarte AyalaNo ratings yet
- B 18000848Document58 pagesB 18000848ARCHON SCARNo ratings yet
- A4 Storyboard Template - 6-Panel - Portrait - StudioBinderDocument1 pageA4 Storyboard Template - 6-Panel - Portrait - StudioBinderARCHON SCARNo ratings yet
- A4 Storyboard Template - 3-Panel - Landscape - StudioBinderDocument1 pageA4 Storyboard Template - 3-Panel - Landscape - StudioBinderARCHON SCARNo ratings yet
- A4 Storyboard Template - 16-Panel - Landscape - StudioBinderDocument1 pageA4 Storyboard Template - 16-Panel - Landscape - StudioBinderARCHON SCARNo ratings yet
- Film production shot planning templateDocument1 pageFilm production shot planning templateARCHON SCARNo ratings yet
- A4 Storyboard Template - 2-Panel - Landscape - StudioBinderDocument1 pageA4 Storyboard Template - 2-Panel - Landscape - StudioBinderARCHON SCARNo ratings yet
- Storyboard TMPTLDocument1 pageStoryboard TMPTLshuga seijiNo ratings yet
- Project Page Scene & Shot ListDocument1 pageProject Page Scene & Shot ListARCHON SCARNo ratings yet
- A4 Storyboard Template - 12-Panel - Landscape - StudioBinderDocument1 pageA4 Storyboard Template - 12-Panel - Landscape - StudioBinderARCHON SCARNo ratings yet
- Summary of Changes: Changes Made Since Version 4.0 Are Marked in BlueDocument20 pagesSummary of Changes: Changes Made Since Version 4.0 Are Marked in BlueARCHON SCARNo ratings yet
- Fundamental-Event-Document 21 FinalDocument11 pagesFundamental-Event-Document 21 FinalARCHON SCARNo ratings yet
- Regulations 3.2Document10 pagesRegulations 3.2peterNo ratings yet
- Netrunner Deck SheetDocument1 pageNetrunner Deck SheetARCHON SCARNo ratings yet
- Honor Glory Status: Craft or Repair A WDocument2 pagesHonor Glory Status: Craft or Repair A WARCHON SCARNo ratings yet
- WWW Antasy LI GHT Ames COM: Net R Unner Net R UnnerDocument1 pageWWW Antasy LI GHT Ames COM: Net R Unner Net R UnnerARCHON SCARNo ratings yet
- l5r02 - Discord Wheel SheetDocument1 pagel5r02 - Discord Wheel SheetARCHON SCARNo ratings yet
- Tournament Sheet Tournament Sheet: The Card Game The Card GameDocument1 pageTournament Sheet Tournament Sheet: The Card Game The Card Gamefleabag8194No ratings yet
- Android: Netrunner Floor Rules SummaryDocument26 pagesAndroid: Netrunner Floor Rules SummarypeterNo ratings yet
- L5R Fillable Character SheetDocument2 pagesL5R Fillable Character SheetShawn YorkNo ratings yet
- Character SheetDocument2 pagesCharacter SheetARCHON SCARNo ratings yet
- Heroscape Faqs Updated 106 13.4Document16 pagesHeroscape Faqs Updated 106 13.4ARCHON SCARNo ratings yet
- l5r10 - Twenty Questions WorksheetDocument4 pagesl5r10 - Twenty Questions WorksheetARCHON SCARNo ratings yet
- l5r10 - Create A School WorksheetDocument2 pagesl5r10 - Create A School WorksheetARCHON SCARNo ratings yet
- L5R Fillable Character SheetDocument2 pagesL5R Fillable Character SheetShawn YorkNo ratings yet
- Honor Glory Status: Craft or Repair A WDocument2 pagesHonor Glory Status: Craft or Repair A WARCHON SCARNo ratings yet
- Path of Waves Campaign Sheet Path of Waves Campaign Sheet: Character Name VigilanceDocument2 pagesPath of Waves Campaign Sheet Path of Waves Campaign Sheet: Character Name VigilanceARCHON SCARNo ratings yet
- L5R05 GM Kit BookletDocument32 pagesL5R05 GM Kit BookletARCHON SCARNo ratings yet
- ZCT ZCT ZCT ZCT: 40S 60S 80S 120S 210SDocument1 pageZCT ZCT ZCT ZCT: 40S 60S 80S 120S 210SWilliam TanNo ratings yet
- Microsoft Word - SOP ON DispensingDocument4 pagesMicrosoft Word - SOP ON DispensingPalawan Baptist HospitalNo ratings yet
- CIVIL BILL OF QUANTITIESDocument16 pagesCIVIL BILL OF QUANTITIESTomNo ratings yet
- Cakes Amp Sugarcraft - April-May 2019 EditDocument45 pagesCakes Amp Sugarcraft - April-May 2019 Editapi-197110397100% (1)
- Sohail KhanDocument3 pagesSohail KhanRashid Muhammad SarwarNo ratings yet
- Vitamin D DeficinyDocument11 pagesVitamin D DeficinyسالمNo ratings yet
- Household Chemical Poisoning GuideDocument9 pagesHousehold Chemical Poisoning GuideAshley DayagNo ratings yet
- B Fire BehaviorDocument39 pagesB Fire BehaviorDon VitoNo ratings yet
- Samsung Un40c5000 Un46c5000 QF Chassis N98aDocument114 pagesSamsung Un40c5000 Un46c5000 QF Chassis N98ajosue otonielNo ratings yet
- Spez KR QUANTEC Prime enDocument155 pagesSpez KR QUANTEC Prime enDave FansolatoNo ratings yet
- Heat Affected Zone: Page 1 of 5Document5 pagesHeat Affected Zone: Page 1 of 5sujkubvsNo ratings yet
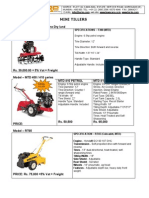
- Optimize soil preparation with a versatile mini tillerDocument2 pagesOptimize soil preparation with a versatile mini tillerRickson Viahul Rayan C100% (1)
- The Following Present A List of Different Attributes and Rules For Assigning Numbers To Objects. Try ToDocument4 pagesThe Following Present A List of Different Attributes and Rules For Assigning Numbers To Objects. Try Togetacdeme2011No ratings yet
- Burns SeminarDocument66 pagesBurns SeminarPratibha Thakur100% (1)
- Clarifying Questions on the CPRDocument20 pagesClarifying Questions on the CPRmingulNo ratings yet
- Definitions of Abnormality by Dr. Kanwal QadeerDocument7 pagesDefinitions of Abnormality by Dr. Kanwal QadeerHaya EishaNo ratings yet
- Cottonhill - Red Collection PDFDocument33 pagesCottonhill - Red Collection PDFVioricaNo ratings yet
- Human Persons As Oriented Towards Their Impendeing DeathDocument28 pagesHuman Persons As Oriented Towards Their Impendeing DeathMaxwell LaurentNo ratings yet
- ImpetigoDocument31 pagesImpetigoUmmu Insyirah100% (1)
- Presentation On: Perfetti Van MelleDocument20 pagesPresentation On: Perfetti Van MelleAkash RaiNo ratings yet
- Deck Damage and Penetrations: Prepared by Richard B. Heagler, P.EDocument9 pagesDeck Damage and Penetrations: Prepared by Richard B. Heagler, P.ENelzon MamaniNo ratings yet
- Automotive ElectronicsDocument44 pagesAutomotive ElectronicsRohit Kumar100% (1)
- List of PharmaDocument4 pagesList of PharmaJamielle SanchezNo ratings yet
- Cooking - Sauces and Marinade RecipesDocument96 pagesCooking - Sauces and Marinade Recipesagape_1st7100% (3)
- Personnel management: Hiring & developing employeesDocument5 pagesPersonnel management: Hiring & developing employeesАлина УсялитеNo ratings yet
- Aruna Prasnam v2 PDFDocument204 pagesAruna Prasnam v2 PDFvenkat_nzNo ratings yet