Professional Documents
Culture Documents
Pharmacology 2: Diabetes Assignment 1
Uploaded by
Daniel PerlasOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pharmacology 2: Diabetes Assignment 1
Uploaded by
Daniel PerlasCopyright:
Available Formats
Diabetes assignment
PHARMACOLOGY 2
Submitted by: Daniel Perlas & Haddy Keita Class: 173 Due date: march 11, 2010 Submitted for: Caroline Murphy
James Bell is an 80- year- old client in the facility where you work as a practical nurse. He has recently been diagnosed with Type 1 diabetes mellitus. He is taking
Diabetes assignment daily insulin injections. You are the primary care nurse and give all care including
medication administration. His physician has written the following orders Humulin R Insulin 10 units and Humulin N 16 units ac breakfast and ac supper; fasting blood sugar ac breakfast daily.
1. Outline a basic explanation of type 1 diabetes that would be suitable for Mr. Bell. Include the following: a.) What is insulin and where is it produced in the body? (1 mark) Type 1 diabetes is referred to as insulin- dependent Diabetes Mellitus. Insulin keeps the blood glucose levels within a normal range and affects carbohydrate, lipid and protein metabolism of the cells in our body. It is produced in the Islet of Langerhans in the pancreas. (Adams, Holland, Bostwick, King, 2010, p. 569) b.) Why does a patient with Type 1 diabetes require insulin injections? (1 mark) Because Type 1 diabetes is an autoimmune destruction of pancreatic betacells, causing the pancreas to no longer produce insulin. (Adams et al, 2010, p. 570) 2. Describe the specific purpose of each of the following test as well as''when'' and why they might be done.
Diabetes assignment a) FPG (Fasting plasma glucose) (1 marks): It is a blood glucose obtained in the laboratory after fasting for more than eight hours to measure blood glucose levels in the body. (Brunner and Suddarth, 2007 p. 1158) b) HgA1c (glycosylated hemoglobin) (1 marks): It is also a blood test use to
check the level of glucose molecules that attach to hemoglobin in red blood cells. It is done every three months because red blood cells live for 120 days. (Brunner and Suddarth, 2007 p. 1168) c) urine for glucose and ketones (3 marks): It is usually done with patients with
type 1 diabetes that have glucosuria or glucose in their urine or have continuously high blood sugar levels (more than 13.2mmol/L for two consecutive test and during illness in pregnancy with pre- existing diabetes and in gestational diabetes.(Brunner and Suddarth, 2007 p.1168) 3) State the normal range in mmol/l in FBS. (1 mark) The normal range in mmol/l in FBS is 4.0- 6.0mmol/l. (Adams et al, 2010 P. 572) 4) Monitoring blood glucose a) What are the types of glucometers are used for testing blood sugar in your facility or pharmacy? (1 mark) Accu- check aviva is the glucometer that is usually used for testing blood glucose level. Louis Brier Home & Hospital b) What are the safety and asepsis guidelines for the use of a glucose meter? (2 marks)
Diabetes assignment Wash and dry hands. Introduce self and identify client. Assess the client's skin at the puncture site to determine skin integrity. Prepare the lancing device by inserting test strips into the meter in the direction of the arrow.
Select a puncture site, clean with alcohol swab, dry and warm to assist the flow of blood.
Don gloves and prick site with lancet or needle using darting motion. Discard the test strips and gauze in a bio-hazard container, and then lancet into sharps container.
Remove gloves, wash hands and document the results. (Kozier & Erb pp. 1194-1195)
5. There are several types of insulin available based on onset, peak & duration. Regular insulin (short acting) and NPH insulin (intermediate acting) are the most commonly prescribed insulins, while the rapid acting and ultralente (long acting) insulins are less common. All insulins are available in multidose vials or may be mixed together by the manufacturer then called mixtures. For mixtures, different types of concentrations are available. Some examples of insulin mixtures will be explored in Question 8. a.) Make a table that shows the onset, peak and duration for each of these 4 types of insulin: Regular, NPH, Rapid- acting and Ultralente. (4 marks)
Diabetes assignment Insulin Preparations TYPE Regular (fast acting insulin) clear (Brunner &Suddarth, 2007 p.1169) (Brunner &Suddarth, 2007 p.1169) Onset 30- 60 minutes Peak Action 2-4 hours Duration 5- 8 hours
NPH (intermediate - acting insulin) cloudy Rapid- acting insulin clear Ultralente (long acting insulin)
1-3 hours
5- 8 hours
Up to 18 hours
10- 15 minutes
60- 90 minutes
4-5 hours
3-4 hours
8-15 hours
22- 26 hours
(Adams et al, 2010, p. 573)
Diabetes assignment
b.) Why does the nurse need to know about the onset, peak and duration for insulin? (1 mark) The nurse needs to know about the onset, peak and duration for insulin to assess the patient for signs and symptoms of hypoglycemia. Also, the nurse needs to know when to check blood glucose level at appropriate time. (Adams et al, 2010, p. 572)
c.) Explain why it is important for insulin to be given ``on time``, in reference to daily routines and meal times? (2 marks) According to Adams , Holland, Bostwick and King, it is necessary to give insulin on time because without insulin, glucose rises in the blood from a meal causing hyperglycemia. It usually occurs when a client forgets to administer insulin during meals. (Adams et al, 2010, p.571)
d.) Mr. Bell is receiving Humulin insulin. Another name used for this insulin in Canada is Novolin insulin. What type of drug names are these? (1 mark) They are both trade names.
e.) State the guidelines for the safe storage of insulin. (1 mark)
Diabetes assignment
According to Brunner & Suddarth, Insulin vials should be refrigerated when not in use, not to be exposed in extremely hot or cold temperature. In addition, if a vial of insulin should be used up in a month, it should be kept at a room temperature. (Brunner & Suddarth, 2007, p. 1179)
f.) Calculate the total amount of insulin that will be in your syringe after drawing up the correct dose for Mr. Bell. (1 mark) 10 unit + 16 units= 26 units of insulin
6. What does sliding scale for insulin refer to? How is the dose of insulin calculated when using a sliding scale? What type of client or situation might require a sliding scale? (3 marks) What does sliding scale for insulin refer to? (1 mark) It is an order in which insulin doses are regulated according to blood sugar levels. (Murphy,C.2009, slide# 65) How is the dose of insulin calculated when using a sliding scale? (1 mark) 0-9.9mmol/l give 0 units 10.0- 14.9mmol/l give 6 units 15.0- 19.9mmol/l give 8 units
Diabetes assignment 20.0- 24.9 give 10units
(Murphy,C., 2009, slide# 66). What type of client or situation might require a sliding scale? (1 mark) It is used for acutely ill patients with diabetes.
(Murphy, C., 2009,slide # 67). 7.) Mr Bell sometimes exhibits symptoms of hypoglycemia. a.) What is hypoglycemia? (1 mark) According to Adams , Holland, Bostwick and King, hypoglycemia occurs when a person has more insulin in the blood than is needed for the amount of glucose in the blood. Some symptoms of hypoglycemia include pale, cool and moist skin, with blood glucose that is less than 4 mmol/L, and may result to death if not treated appropriately. (Adams et al, 2010 p. 572) b.) Describe at least 3 causes of hypoglycemia and the usual signs and symptoms. (2 marks) First, if a person takes too little food or increase his or her physical activity, blood glucose level decreases Second, if a person takes too much insulin or oral hypoglycaemic agent, hypoglycemia occurs Third, if a person who has not eaten a bed time snack could result into midnight hypoglycemia
Diabetes assignment (Brunner & Suddarth, 2007, p. 1183) The common signs and symptoms of hypoglycemia are: Mild hypoglycemia: Sweating, tremors, tachycardia, palpitation, nervousness and hunger Moderate hypoglycemia: Headache, lightheadedness, confusion, memory lapses, slurred speech and numbness of the tongue Severe hypoglycemia: Seizures and disoriented behaviours (Brunner & Suddarth, 2007, p. 1183)
c.) In his routine day, when would be the most likely time for Mr. Bell to have a hypoglycemic reaction? (1 mark) Mr. Bell will most likely experience hypoglycemia early in the morning because fasting blood sugar needs to be taken before breakfast. Mr. Bell needs to eat his breakfast after taking his insulin shot. Also, he might experience middle of the night hypoglycemia because Insulin NPH peaks at evening. Therefore, he must eat his bedtime snack. (Brunner & Suddarth, 2007, p. 1183)
Diabetes assignment 8) Mr. Bell's insulin order was later changed to Humulin 70/30 16 units ac
10
breakfast and ac supper. What does the 70/30 mean and what is the onset, peak, and duration of this insulin? How is humulin 70/30 different from humalog 75/25? Humulin70/30 is pre- mixed insulin meaning 70% NPH insulin and 30% regular acting insulin. Onset: 30 mins peak: 4- 8 hours Duration: 24 hours
(Deglin & Vallerand, 2007 p. 679)
Humulin 70/30 is a mixture of NPH and regular insulin,while Humalog 75/25 means 75% of the
insulin is lispro- protamin suspension and 25% insulin lispro solution mix. (Deglin & Vallerand, 2007, p. 680)
9) Mr. Bell's glucose meter testing is done before breakfast. One morning his FBS is 16mmol/l. He states that he feels very sleepy, has stomach cramps and is very thirsty. a.) Mr. Bell is experiencing hyperglycemia. Identify 3 possible causes of hyperglycemia. (1 mark) Causes of hyperglycemia include hormones in our body including epinephrine, thyroid hormones, growth hormones & corticosteroids.
Diabetes assignment Common drugs such as phenytoin, NSAIDS, Angiotensin- converting enzyme inhibitors (ACE inhibitors) and diuretics raise blood sugar levels. Increase consumption of foods rich in calories like sugar. (Adams et al, 2010 p. 570)
11
b.) Give 5 specific nursing responsibilities / interventions that would do for Mr. Bell at the time( ie during the rest of your shift) you realize he has a glucose meter reading of 16mmol/l. (2 marks) Assess for signs of hyperglycemia ie confusion, drowsiness, flushed & dry skin, odour, polyuria, loss of appetite periodically during therapy.
fruit- like breath
Monitor body weight periodically because changes in weight may necessitate
changes in insulin dose. blood. Monitor vital signs because increased pulse and blood pressure are signs of Monitor blood sugar levels every six hours during therapy. Monitor changes in magnesium, potassium and other electrolyte levels in the
hyperglycemia. (Deglin & Vallerand, 2007 p. 680)
c.) Develop a teaching plan appropriate for MR. Bell. Include at least 5 guidelines, covering topics such as (but not limited to) keeping a stable blood sugar, nutrition, dealing with a new diagnosis, etc. (2 marks)
Diabetes assignment Teach patient proper technique for insulin administration.
12
Explain to the patient that the medication controls hyperglycemia but does not cure diabetes.
Instruct patient ways of testing serum glucose and ketones. Teach patient the importance of compliance with nutritional guidelines and regular exercise.
Instruct the patient on signs and symptoms of hypoglycemia and hyperglycemia and what to do if any occurs.
Stress the importance of regular follow up during first week of therapy. (Deglin & Vallerand, 2007 p.680)
10.) Research the 2 oral antidiabetic agents: Metformin and Glyburide. a.) List the classification, action, uses, route, normal dose, side effects, and nursing implications for each of these drugs. (2 marks for each drug) metformin (Glucophage) Class: antidiabetics, biguanides Action: decrease the hepatic production of glucose, rises the sensitivity to insulin and reduces glucose absorption in the intestines Uses: to manage diabetes type 2; can be utilized with diet, insulin or sulfonylurea oral hypoglycemics Route: PO (Deglin & Vallerand, 2009, p. 793)
Diabetes assignment Normal dose: In adult, a total of 500 mg qd- tid (max 3 g/d)
13
Side effects: nausea and diarrhea, abdominal bloating, vomiting and hypoglycemia
Nursing implications: A client who has been taking metformin for a long period of time and developed illness or abnormalities during laboratory test, assess for ketoacidosis or lactic acidosis. Check for serum electrolytes, ketones, glucose and pH level in the blood. Give metformin with meals to decrease GI effects. Assess for any signs and symptoms of hypoglycemia such as abdominal pain, diaphoretic skin, dizziness and weakness, tremors, when metformin is combined with oral sulfonylureas. During therapy, it is significant to monitor serum glucose and glycosylated haemoglobin periodically to evaluate the effectiveness of the therapy. (Deglin et.al, 2009, p. 794)
glyburide (Diabeta) Class: antidiabetics, sulfonylureas
Diabetes assignment
14
Action: lower blood glucose level by stimulating the pancreas to secrete more insulin and increases the sensitivity of insulin at the receptor sites. Uses: control of Type 2 diabetes mellitus (Deglin et.al, 2009, p. 648) Route: PO Normal dose: (adults) 2.5 5 mg daily once daily initially range: (1.25-20 mg/day) (geriatric patients) 1.25 mg daily initially Side effects: hypoglycemia, photosensitivity, dizziness, drowsiness, aplastic anemia, diarrhea, nausea and vomiting (Deglin et.al, 2009, p. 649) Nursing Implications: Monitor signs and symptoms of hypoglycemia including: diaphoretic skin, hunger, weakness, dizziness, tremor, tachycardia, anxiety. Assess if the client is allergic to sulphonamides. Check if patient is on beta- blocker therapy which may have signs of hypoglycemia. Report immediately if blood count falls when monitoring CBC periodically during therapy.
Diabetes assignment
15
In order to evaluate the effectiveness of treatment during therapy, serum glucose and glycosylated haemoglobin should be monitored periodically
(Deglin et.al, 2009, p. 650) b.) Explain why these drugs are useful for someone with Type 2 diabetes. (1 mark) Brunner and Suddarth says that these oral antihyperglycemic agents are useful for patients who have an existing diabetes type 2 by lowering the blood glucose level, which cannot be treated by diet and exercise alone. (Brunner & Suddarth, 2007, p. 1175)
11) What is the primary use and expected therapeutic outcome of glucagon, the anti-hypoglycemia agent? By what route is this drug given? (2 marks) It is an emergency replacement therapy for diabetic clients, and it is given when their blood glucose decreases below normal level to break down stored glycogen and converts it to glucose which increases blood sugar to a normal level, and it can be given IV, IM, and Subcutaneously. (Adams et al, 2010 p. 570)
Diabetes assignment
16
Reference Lists: 1. Adams et al, (2010). Pharmacology for Nurses: Canadian Edition. A pathophysiological Approach. Toronto: Pearson. 2. Brunner & Suddarth,(2007). Medical- surgical Nursing: First Canadian Edition. USA. Lippincort Williams & Wilkins. 3. Deglin & Vallerand, (2007). Davis's Drug Guide For Nurses: Eleventh Edition. USA. Davis Company. 4. Kozier, B. et al, (2010). Fundamental of Canadian Nursing 2nd Edition. Canada: Elservier. 5. Murphy, C. (2009). Endocrine handout.
Diabetes assignment
17
You might also like
- Blood Glucose-Insulin Administration-Study GuideDocument8 pagesBlood Glucose-Insulin Administration-Study GuideChandra MuraliNo ratings yet
- NR 325 Diabetes Power-Student Copy1118Document39 pagesNR 325 Diabetes Power-Student Copy1118John MixerNo ratings yet
- Insulin Administration Revised 1Document43 pagesInsulin Administration Revised 1Cheryl Tabañag TalledoNo ratings yet
- Managing Diabetes Complications and EmergenciesDocument21 pagesManaging Diabetes Complications and EmergenciesHanna BaddiriNo ratings yet
- Nurs220 Diabetes Case Study CtolentinoDocument6 pagesNurs220 Diabetes Case Study Ctolentinoapi-339295205No ratings yet
- All About Insulin: Jill E. Vollbrecht, MDDocument41 pagesAll About Insulin: Jill E. Vollbrecht, MDkeylapireNo ratings yet
- Insulin Initiation and MonitoringDocument35 pagesInsulin Initiation and Monitoringeka prasepti darusmanNo ratings yet
- Name University Course Professor DateDocument13 pagesName University Course Professor DateKaliunga CleophasNo ratings yet
- Pharm Quiz 1Document59 pagesPharm Quiz 1Anonymous vXOM1Wxt100% (1)
- New Insulin PolicyDocument8 pagesNew Insulin Policybelle dyNo ratings yet
- Diabetes MellitusDocument16 pagesDiabetes MellitusApril Joy V. QuinoNo ratings yet
- Diabetes and NephrologyDocument36 pagesDiabetes and NephrologydrpbendreNo ratings yet
- Common Endocrine Disorders: Iril I. Panes, RN, MANDocument63 pagesCommon Endocrine Disorders: Iril I. Panes, RN, MANJona Phie Domingo MonteroNo ratings yet
- InsulinDocument4 pagesInsulinHa Zizzle100% (1)
- Diabetic EssayDocument6 pagesDiabetic Essayreet kaurNo ratings yet
- Exercise Benefits for DiabeticsDocument64 pagesExercise Benefits for DiabeticsAnthonyChapotinNo ratings yet
- Hayatt Univesity College. Faculty of Medicine. Family Medicine. Mohamed Gassim Mohamed. Insulin ManagementDocument14 pagesHayatt Univesity College. Faculty of Medicine. Family Medicine. Mohamed Gassim Mohamed. Insulin ManagementMohammed GassimNo ratings yet
- What Is DiabetesDocument9 pagesWhat Is Diabeteskdubb90No ratings yet
- Diabetes Insulin InitiationDocument12 pagesDiabetes Insulin InitiationSatinder BhallaNo ratings yet
- Using Insulin: What Is Insulin? Types of InsulinDocument4 pagesUsing Insulin: What Is Insulin? Types of InsulinRyo RyozNo ratings yet
- Peran Perawat DLM Rawat Inap DMDocument57 pagesPeran Perawat DLM Rawat Inap DMMuhidin AeNo ratings yet
- Diabetes Study GuideDocument4 pagesDiabetes Study GuideNicole Brassington0% (1)
- Diabetes Cases: Nahda College Program of Pharmacy Department of Clinical Pharmacy 2020-2021Document23 pagesDiabetes Cases: Nahda College Program of Pharmacy Department of Clinical Pharmacy 2020-2021Basil DomiNo ratings yet
- Understanding DiabetesDocument21 pagesUnderstanding DiabetesAmir Izzuddin SuibNo ratings yet
- Blood Sugar Levels in Children and AdultsDocument4 pagesBlood Sugar Levels in Children and AdultsreskyNo ratings yet
- CH 39 Anaesthesia and Diabetes MellitusDocument6 pagesCH 39 Anaesthesia and Diabetes MellitusChristian LeepoNo ratings yet
- 1 RBH Icu Insulin Guidelines May 2009Document6 pages1 RBH Icu Insulin Guidelines May 2009bastarduniverseNo ratings yet
- Diabetes MellitusDocument93 pagesDiabetes MellitusAllen Reyes SantosNo ratings yet
- Insulin Initiation and Intensification in Type 2 DiabetesDocument54 pagesInsulin Initiation and Intensification in Type 2 DiabetesAshraf Shaaban MahfouzNo ratings yet
- Antidiabetic DrugsDocument43 pagesAntidiabetic Drugssamakayigrace808No ratings yet
- c3 Type 1 Diabetes MellitusDocument10 pagesc3 Type 1 Diabetes Mellitusjulio perezNo ratings yet
- Intensive Insulin TherapyDocument54 pagesIntensive Insulin TherapySiva RamanNo ratings yet
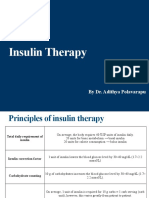
- Insulin Therapy: by Dr. Adithya PolavarapuDocument18 pagesInsulin Therapy: by Dr. Adithya Polavarapuadithya polavarapuNo ratings yet
- Vete 4305 - Group 2 Case Study - Cat With DiabetesDocument19 pagesVete 4305 - Group 2 Case Study - Cat With Diabetesapi-242607157No ratings yet
- MS3 Review NotesDocument11 pagesMS3 Review NotesPaul Anthony LoricaNo ratings yet
- Insulin Infusion Protocol for LabourDocument4 pagesInsulin Infusion Protocol for LabourJohb CaballeroNo ratings yet
- Clinical Practice Guidelines For The Inpatient Management of Diabetes/Hypergylcemia in AdultsDocument4 pagesClinical Practice Guidelines For The Inpatient Management of Diabetes/Hypergylcemia in AdultselexboyNo ratings yet
- Hizon, EndocrineDocument3 pagesHizon, EndocrineDan HizonNo ratings yet
- All Types of InsulinDocument18 pagesAll Types of Insulinali mohammedNo ratings yet
- Diabetes Mellitus (TYPE 1) : Risk FactorsDocument8 pagesDiabetes Mellitus (TYPE 1) : Risk FactorsLovely DaroleNo ratings yet
- DM Presentation NewDocument44 pagesDM Presentation NewKipz JonsNo ratings yet
- Diabetic Emergencies Case StudiesDocument32 pagesDiabetic Emergencies Case StudiesLamria Maloni Siahaan0% (1)
- Diabetes MellitusDocument3 pagesDiabetes MellitusNoviley Amor TianiaNo ratings yet
- Blood Sugar: Insulin and Other MedicationsDocument9 pagesBlood Sugar: Insulin and Other MedicationscataNo ratings yet
- Insulin: Mert Aygüler 13O2O2O32Document16 pagesInsulin: Mert Aygüler 13O2O2O32deryaaaNo ratings yet
- DM Brochure For NCM 106Document12 pagesDM Brochure For NCM 106Kimsha ConcepcionNo ratings yet
- Diabetes Exam With AnswersDocument12 pagesDiabetes Exam With AnswersJed TumaliwanNo ratings yet
- Insulin Resistance Subab 5-7Document22 pagesInsulin Resistance Subab 5-7Alya PianaNo ratings yet
- HHNSDocument20 pagesHHNSVitis Vinivera KhasanahNo ratings yet
- Imbalanced Nutrition Less Than Body Requirements - Diabetes - NCPDocument5 pagesImbalanced Nutrition Less Than Body Requirements - Diabetes - NCPJulie Ann Jimenez Manlangit50% (4)
- INSULIN CONTROLS BLOOD GLUCOSEDocument7 pagesINSULIN CONTROLS BLOOD GLUCOSEMIR SARTAJNo ratings yet
- د.ريهام الفرا 2Document45 pagesد.ريهام الفرا 2جمال محمود السيايدةNo ratings yet
- Lantus UsageDocument10 pagesLantus UsageSyed Masood AliNo ratings yet
- Do All of The AboveDocument16 pagesDo All of The AboveMeazaNo ratings yet
- NRNP 6566 Advanced Care of Adults in Acute Settings I Week11 Knowledge Check 2023-2024Document9 pagesNRNP 6566 Advanced Care of Adults in Acute Settings I Week11 Knowledge Check 2023-2024mary011danielNo ratings yet
- DR Shahjada Selim: Assistant Professor Department of Endocrinology, BSMMU Organizing Secretary, BESDocument63 pagesDR Shahjada Selim: Assistant Professor Department of Endocrinology, BSMMU Organizing Secretary, BESABDUL BARINo ratings yet
- Test Bank For The Nurse The Math The Meds 3rd Edition by Mulholland DownloadDocument10 pagesTest Bank For The Nurse The Math The Meds 3rd Edition by Mulholland Downloadsarahwatsonmfjtabceri100% (14)
- Pharmacology - Endocrine DrugsDocument123 pagesPharmacology - Endocrine DrugsBenjamin Joel BreboneriaNo ratings yet
- Insulin GNTDocument41 pagesInsulin GNTV Narayan Rao TummalaNo ratings yet
- Practical Insulin: A Handbook for Prescribing ProvidersFrom EverandPractical Insulin: A Handbook for Prescribing ProvidersRating: 5 out of 5 stars5/5 (2)
- Forcep Delivery..Document3 pagesForcep Delivery..Kristelle Joy Capili SicatNo ratings yet
- Correlation of Mouth Ulcer and Cow's Milk Protein IntakeDocument4 pagesCorrelation of Mouth Ulcer and Cow's Milk Protein IntakeLiviliaMiftaNo ratings yet
- Assessment Nursing Diagnosis Planning Implementation OutcomeDocument2 pagesAssessment Nursing Diagnosis Planning Implementation OutcomeBethel Ann Cordova100% (1)
- Psychia AnamnesisDocument9 pagesPsychia AnamnesisKen Harry MirafuentesNo ratings yet
- DRUG STUDY MetoprololDocument1 pageDRUG STUDY MetoprololSymone Jay Lapiz100% (2)
- PIMS Hospital, JALLANDHARDocument13 pagesPIMS Hospital, JALLANDHARParminder Singh Virdi100% (1)
- ASRM (2012) Guidelines On Number of Embryos PDFDocument3 pagesASRM (2012) Guidelines On Number of Embryos PDFGerardo Solano-ElizondoNo ratings yet
- Crowe S ClassificationDocument3 pagesCrowe S ClassificationErnesto Ewertz MiquelNo ratings yet
- RhythmDocument8 pagesRhythmparkmickyboo100% (1)
- Nabimara Charles Cit PGD ReportDocument56 pagesNabimara Charles Cit PGD ReportArsalan FarooqNo ratings yet
- Baptist Health South Florida Group OverviewDocument11 pagesBaptist Health South Florida Group OverviewTony MasaruNo ratings yet
- MCQ AnaesthesiaDocument15 pagesMCQ AnaesthesiaProf-Ashraf Emara100% (2)
- Into The Magic Shop - IntroductionDocument4 pagesInto The Magic Shop - IntroductionSara NemetNo ratings yet
- Introduction To Electrical Systems For Medical FacilitiesDocument40 pagesIntroduction To Electrical Systems For Medical Facilitiespano356No ratings yet
- Medical English VocabularyDocument21 pagesMedical English VocabularyGil Ruano100% (2)
- 2Document50 pages2Scott Russell McGillivray100% (1)
- Green Buildings & Green Hospitals: 26 March 2010 KochiDocument32 pagesGreen Buildings & Green Hospitals: 26 March 2010 KochiSrinivas GoudNo ratings yet
- Fever Without A Source in Children 3 To 36 Months of AgeDocument19 pagesFever Without A Source in Children 3 To 36 Months of AgeRajiv KabadNo ratings yet
- DysmenorrheaDocument35 pagesDysmenorrheaAs-sifa KharismaNo ratings yet
- Alternatives to Terifrac injection for osteoporosisDocument2 pagesAlternatives to Terifrac injection for osteoporosisrameshg2020No ratings yet
- SPRAVATO Medication GuideDocument41 pagesSPRAVATO Medication Guidethor888888No ratings yet
- Hemiplegia Resource Book ModifiedDocument60 pagesHemiplegia Resource Book ModifiedAnonymous czrvb3hNo ratings yet
- Tecfidera (Dimethyl Fumarate) MonographDocument7 pagesTecfidera (Dimethyl Fumarate) Monographamin138irNo ratings yet
- Icici Lombard Health Care Insurance Claim FormDocument5 pagesIcici Lombard Health Care Insurance Claim FormsperoNo ratings yet
- The Power of Informed Consent (Essay)Document2 pagesThe Power of Informed Consent (Essay)Super KNo ratings yet
- Hospital Assessment Tool GuideDocument50 pagesHospital Assessment Tool GuideShu Dizon100% (1)
- MAC Vs TIVADocument2 pagesMAC Vs TIVARicky JalecoNo ratings yet
- SchizophreniaDocument40 pagesSchizophreniaAzba MalikNo ratings yet
- Neurologic Assessment: Chapter OutlineDocument22 pagesNeurologic Assessment: Chapter Outlinekenthepa100% (1)
- Cleaning Policy 6.0Document27 pagesCleaning Policy 6.0saadNo ratings yet