Professional Documents
Culture Documents
Radiographic Exposure Factors
Uploaded by
Sai FujiwaraOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Radiographic Exposure Factors
Uploaded by
Sai FujiwaraCopyright:
Available Formats
Radiographic Exposure Factors
h p://www.e-radiography.net/radtech/e/exposurefactors.htm
al dierence between lm and anode ng power) of the x-ray beam is controlled by the voltage adjustment. This control usually is labelled in keV (thousand electron volts) and some mes the level is referred to as kVp (kilovoltage poten al). Do not be confused by the dierent terminology, just remember there is a control by which the dierence in poten al between the cathode and anode can be controlled. The higher the voltage se ng, the more energe c will be the beam of x-ray. A more penetra ng beam will result in a lower contrast radiograph than one made with an x-ray beam having less penetra ng power. It is probably obvious that the more energe c the beam, the less eect dierent levels of ssue density will have in a enua ng that beam. The generator waveform if is not constant poten al (medium frequency etc) will aect the eec ve Kv. mA Tube Current The second control of the output of the x-ray tube is called the mA (milliamperage) control. This control determines how much current is allowed to ow through the lament which is the cathode side of the tube. If more current (and therefore more hea ng) is allowed to pass through the lament, more electrons will be available in the "space charge" for accelera on to the target and this will result in a greater ux of photons when the high voltage circuit is energized. The eect of the mA circuit is quite linear. If you want to double the number of "x" photons produced by the tube, you can do that by simply doubling the mA. Changing the number of photons produced will aect the blackness of the lm but will not aect the lm contrast. S Time The third control of the x-ray tube which is used for medical imaging is the exposure mer. This is usually denoted as an "S" (exposure me in seconds) and is combined with the mA control. The combined func on is usually referred to as mAs or milliampere seconds so, if you wanted to give an exposure using 10 milliampere seconds you could use a 10 mA current with a 1.0 second exposure or a 20 mA current for a 0.5 second exposure or any combina on of the two which would result in the number 10. Both of these factors and their combina on aect the lm in a linear way. That is, if you want to double lm blackness you could just double the mAs. The X-Ray beam The x-ray beam has two main proper es you need to understand. 1) Beam QUALITY is the ability of the beam to penetrate an object, its all about the penetra ng power of the x-ray photons, this is controlled by the KV control. 2) Beam INTENSITY this is the number of x-ray photons in the beam and is principally controlled by the mAS
1 of 7
9/27/2012 2:34 PM
Radiographic Exposure Factors
h p://www.e-radiography.net/radtech/e/exposurefactors.htm
But note as you increase the KV not only does the QUALITY harden (more penetra ng) but you do actually get more photons so INTENSITY increases too. Pu ng it all together the exposure Any radiographic subject has a minimum Kv required for the x-ray photons penetrate the most dense part of the subject, the most radiographicaly dense part of the subject will depend upon what the part is chemicaly composed of (Atomic number) and its thickness (remember linear a enua on coecients and HVL!?) The thicker the subject the more absorp on of x-rays so the thicker the part the more mAS you require. In theory the more Kv you use the less the contrast of the image will have However in prac ce lm screen / processing condi ons aect contrast much more In prac ce it is not as simple as this as sca er is produced which is not image forming but adds density to the lm and needs to be controlled, if you remember all those complex diagrams about interac ons of x-rays with ma er you will realise the amount and direc on of sca er depends on the Kv and the material absorbing the x-rays.
Image 1 The Kv is too low the femoral condyle is under pentrated you cannot see the bone trabecualr pa erns. the contrast is too high to demonstrate all the so ssues.
2 of 7
9/27/2012 2:34 PM
Radiographic Exposure Factors
h p://www.e-radiography.net/radtech/e/exposurefactors.htm
Image 2 Much be er the all the subject is penetrated and all the so ssues are visible
A well exposed abdomen image demonstra ng all the so ssue structures.
A good chest image the medias num is pentrated the image is exposed well demonstra ng the bones and so ssues.
3 of 7
9/27/2012 2:34 PM
Radiographic Exposure Factors
h p://www.e-radiography.net/radtech/e/exposurefactors.htm
Under penetrated
OK
Under penetrated
4 of 7
9/27/2012 2:34 PM
Radiographic Exposure Factors
h p://www.e-radiography.net/radtech/e/exposurefactors.htm
Too much mAS
Too Li le mAS
A few myths Changing the Kv by 2 or 3 makes almost no perceptable image change! Adding 10 Kv does not double the image density Exposure factors are an exact science ! (the image you produce must sa sfy the radiologist who interprets the image - not all radiologists like the same penetra on / density / contrast for the same body part) Image Contrast Here, we need to spend a li le more me discussing the issue of radiographic contrast. This is an important concept because image contrast plays a cri cal part in the interpreter's ability to detect abnormali es which are only slightly dierent from the density of the surrounding material. It is not possible to say what is the op mal contrast (or the op mal radiographic technique) for all situa ons. Dierent body parts have dierent inherent ssue contrast. This can be illustrated by using the extreme examples of the chest and the breast. In the chest, there is good inherent ssue contrast with densi es ranging all the way from
5 of 7
9/27/2012 2:34 PM
Radiographic Exposure Factors
h p://www.e-radiography.net/radtech/e/exposurefactors.htm
bone at the high end to air at the low end. On the other hand, the breast is inherently very low in ssue contrast only containing structures which are water density (glandular material or tumor) or fat density. For the moment, we will disregard small calcica ons which are really not normal structures. Because of this dierence in inherent ssue contrast, we would be likely to use a very low contrast radiographic technique for the chest because we have good ssue contrast. Conversely we would be likely to use a very high contrast technique for the breast because the breast has minimal, inherent ssue contrast. Remember, image contrast is controlled by the energy of the "x" photon beam. Therefore, high kV techniques result in low contrast images (the assump on is always made that the image will have approximately the same average lm density so if kV is increased, there must be a compensa on in mAs to keep lm density constant). To increase image contrast in situa ons where there is low ssue contrast, a low kV, high mAs technique should be used. This is obvious for mammography but you should also remember this possibility for other special situa ons such as looking for low-density foreign bodies embedded in so ssue. To improve lm contrast for mammograms we would need to use a very low energy x-ray beam. Mammograms are frequently done with beams in the 25 keV range. For the chest x-ray, we would like to use a low contrast technique which requires a rela vely high-energy beam. Chest x-rays are frequently done with beam energies above 100 keV. You should understand that for similar lm densi es, the high KV technique usually results in lower pa ent radia on exposure. Think about this long enough to clearly understand why less radia on is absorbed in the pa ent when a high-energy beam is used. Grids One of the problems in ge ng a sharply dened image in clinical radiology is the presence of sca ered or secondary radia on. These photons are created in the body of the pa ent or closely surrounding objects by the interac on of that material and the primary "x" photons coming from the x-ray tube. Several possible interac ons occur in the diagnos c energy range. At rela vely low energies, the photoelectric eect is probable. The photoelectric eect is actually the desirable, photon/ ssue interac on because there is complete absorp on of the photon with no produc on of a secondary photon. The more common ssue interac on at the photon energies used for the majority of clinical procedures is called the Compton eect or coherent sca ering. In this interac on, a secondary photon is produced at the site of interac on. The secondary photon will always have lower energy than the primary photon and will be going in an altered direc on. These secondary photons, if allowed to reach the lm, will actually produce erroneous informa on by recording gray tone varia on (and therefore indica ng rela ve ssue densi es) at some distance from the site at which the photon/ ssue interac on actually occurred. The net result of allowing a signicant number of secondary photons to reach the lm is a reduc on in image sharpness. There will always be a loss of spa al resolu on. Several methods have been devised to reduce the problem of sca ered radia on. The simplest and most direct is to simply limit the eld of exposure. If a small image area is adequate to make the clinical diagnosis, the image area should be "coned down" to that small size. For instance, if you want to image the gallbladder, you will get a much sharper picture if you bring the shu ers down to include an area only the size of the gallbladder instead of including the en re upper abdomen on the image. Just remember that the smaller the area of the x-ray beam the fewer sca ered photons you will produce.
6 of 7 9/27/2012 2:34 PM
Radiographic Exposure Factors
h p://www.e-radiography.net/radtech/e/exposurefactors.htm
In the typical clinical imaging situa on, the most common method of reducing sca er is to use a radiographic grid. The grid looks like a at metallic plate the size of the x-ray lm if you look at it directly. However, it is more complicated than that. It actually is composed of alterna ng radiopaque (lead) and radiolucent (aluminum) strips. These are arranged on edge, sort of like looking at the strips of a vene an blind which is arranged to let light come between the strips. The edge of these strips is turned towards the source of x-rays and in the most commonly used grid, the focused grid, the anglula on of the strips is arranged to match the divergence of the x-ray beam. This arrangement of the radiographic grid will give the highest probability for primary "x" photons passing between the lead grid strips and reaching the lm, while the o-focus or secondary photons are likely to interact in the lead strips and never reach the lm. The use of this radiographic grid will greatly improve image sharpness when a rela vely thick body part is being imaged. Unfortunately, there is always a trade o. Since the grid does stop some of the photons which would contribute to lm blackening, if you just add a radiographic grid without changing the tube se ngs, the lm will be greatly underexposed. If you decide to use a grid, you will have to increase the number of photons produced by the x-ray tube in order to get the correct lm exposure. This will result in giving the pa ent increased radia on exposure. Remember, the posi on of the grid is between the pa ent and the lm. The third method of reducing sca er or at least reducing the probability that sca ered photons will reach the lm is to use an air gap. This is infrequently used in clinical radiography but can s ll, some mes be used to an advantage par cularly when magnica on of the image might be helpful. Ordinarily we would have the lm posi oned as close to the pa ent's body as possible for the radiography of any body part. With an air gap technique, the lm is moved several inches away from the pa ent's body. That separa on, (because secondary photons are likely to be lower energy and moving at a greater angle than primary photons) will result in a decreased probability of the secondary photon hi ng the lm. From the diagram below, you will be able to understand that crea ng the air gap will also result in magnifying the radiographic image. Remember the x-ray beam is produced from almost a point source and it diverges as it goes towards the pa ent. Useful Link h p://www.med.sc.edu:1000/2prod&useab.htm
7 of 7
9/27/2012 2:34 PM
You might also like
- RT 203 Principles of Imaging 32 62Document31 pagesRT 203 Principles of Imaging 32 62Bea SeloterioNo ratings yet
- Notebook 7 - RevisedDocument5 pagesNotebook 7 - Revisedapi-338659956No ratings yet
- The Merck Veterinary Manual - RadiographyDocument6 pagesThe Merck Veterinary Manual - Radiographylecol351100% (1)
- Topic 2 RT202Document27 pagesTopic 2 RT202allexa jimlaniNo ratings yet
- Exposure Factors Lec 03Document26 pagesExposure Factors Lec 03Javeria KhanNo ratings yet
- Radiographic TechniqueDocument40 pagesRadiographic TechniqueShan Angelie SarmientoNo ratings yet
- Prime Factors of Radiographic ExposureDocument3 pagesPrime Factors of Radiographic ExposureThilak raj SNo ratings yet
- Making An Exposure Chart: Garry D. LasagaDocument23 pagesMaking An Exposure Chart: Garry D. LasagaGarry LasagaNo ratings yet
- SUN MON TUE WED THU FRI SAT: - Rays Are Produce by Electron DecelerationDocument6 pagesSUN MON TUE WED THU FRI SAT: - Rays Are Produce by Electron DecelerationapollyonmdNo ratings yet
- The Biomedical Engineering Handbook: Second EditionDocument37 pagesThe Biomedical Engineering Handbook: Second EditionAdrian Del CastilloNo ratings yet
- 1Document2 pages1Gloriebeth RabeNo ratings yet
- Digital Radiography: Ms - Laurencia PhilipoDocument56 pagesDigital Radiography: Ms - Laurencia PhilipoKAZOBA FRANCISNo ratings yet
- X-Ray CCD Detectors: Course NotesDocument17 pagesX-Ray CCD Detectors: Course NotesDan Clas ClasNo ratings yet
- Equipment: MammographyDocument6 pagesEquipment: MammographyDr. Shaji teleNo ratings yet
- 2 - Imaging With XrayDocument24 pages2 - Imaging With XrayomerNo ratings yet
- Ch. 5 - Radiographic QualityDocument33 pagesCh. 5 - Radiographic QualityzaldiNo ratings yet
- Modern Methods of Industrial Radiology - A Rev1ewDocument19 pagesModern Methods of Industrial Radiology - A Rev1ewphanthanhhungNo ratings yet
- C-Arm Parts and PrinciplesDocument10 pagesC-Arm Parts and PrinciplesErshad SohailNo ratings yet
- Xray PropertiesDocument32 pagesXray PropertiesJesse Yaw BaafiNo ratings yet
- Lithography: Optical, E-Beam and X-RayDocument176 pagesLithography: Optical, E-Beam and X-RaylinjefNo ratings yet
- Image Quality - v1Document50 pagesImage Quality - v1Fouzia NoorNo ratings yet
- Signal-to-Noise RatioDocument5 pagesSignal-to-Noise RatioMuhammad TausifNo ratings yet
- Standard Radiographic Technique ChartDocument12 pagesStandard Radiographic Technique ChartAlthea Amor CambarijanNo ratings yet
- Control of Sactter Radiation Week 9Document62 pagesControl of Sactter Radiation Week 9Rupali SinghNo ratings yet
- 4 Radiographic ReceptorsDocument61 pages4 Radiographic Receptors--No ratings yet
- Quantum NoiseDocument4 pagesQuantum NoiseCarlos MoraNo ratings yet
- 05 NotesDocument8 pages05 NotesShivam KumarNo ratings yet
- Prime Factors Image QualityDocument145 pagesPrime Factors Image QualityChristian Pardilla Buena100% (1)
- Chapter 013Document2 pagesChapter 013Zaid juttNo ratings yet
- Teaching DR - CR With Best Dose PracticesDocument31 pagesTeaching DR - CR With Best Dose PracticesBusiness KhmerNo ratings yet
- Exposure Factors: DR Hussein Ahmed HassanDocument39 pagesExposure Factors: DR Hussein Ahmed HassanchowhkNo ratings yet
- MCA-6 N Sample MC0086 Fall-2013Document0 pagesMCA-6 N Sample MC0086 Fall-2013Abhin MithraNo ratings yet
- Radiation Dose in Pelvic ImagingDocument9 pagesRadiation Dose in Pelvic ImagingAlmvd DelgadoNo ratings yet
- Radiology ReviewDocument52 pagesRadiology ReviewFourthMolar.com50% (2)
- Hds 1033-Lect 11 - AecDocument46 pagesHds 1033-Lect 11 - AecFairuz NasirNo ratings yet
- Radiographic Imaging and Exposure 5Th Edition Fauber Test Bank Full Chapter PDFDocument38 pagesRadiographic Imaging and Exposure 5Th Edition Fauber Test Bank Full Chapter PDFmoriskledgeusud100% (7)
- Radiographic Imaging and Exposure 5th Edition Fauber Test BankDocument17 pagesRadiographic Imaging and Exposure 5th Edition Fauber Test Bankbeatrixkhuyen9rm100% (22)
- 7 - Individual Limits For Member of The Public-8Document15 pages7 - Individual Limits For Member of The Public-8Bashar BassamNo ratings yet
- Class Notes 09.22.08Document2 pagesClass Notes 09.22.08Mike Nguyen100% (2)
- Medical Imaging Systems Example QuestionsDocument2 pagesMedical Imaging Systems Example QuestionsPika17No ratings yet
- Basic Principles of CTDocument77 pagesBasic Principles of CTcroydubsNo ratings yet
- X Ray EmissionDocument66 pagesX Ray EmissiondanasardyNo ratings yet
- Chapter 8 X-Ray EmissionDocument8 pagesChapter 8 X-Ray EmissionMegNo ratings yet
- Exercise 1Document35 pagesExercise 1Van Labasano67% (3)
- Notebook 7 PG 24-25Document3 pagesNotebook 7 PG 24-25api-334252501No ratings yet
- 2021 3528 Moesm1 EsmDocument30 pages2021 3528 Moesm1 Esm1356055749No ratings yet
- IMAGING Life Cycle and QualityDocument58 pagesIMAGING Life Cycle and QualityEdgardo CayananNo ratings yet
- TMP 42 C5Document11 pagesTMP 42 C5FrontiersNo ratings yet
- Chapter 011Document2 pagesChapter 011Zaid juttNo ratings yet
- Radiographic Sensitivity: Topics IndexDocument17 pagesRadiographic Sensitivity: Topics IndexHarshaVeeragandhamNo ratings yet
- Digital Radiography Artifacts PDFDocument9 pagesDigital Radiography Artifacts PDFYouness Ben TibariNo ratings yet
- Points, Pixels, and Gray Levels: Digitizing Image Data: James B. PawleyDocument22 pagesPoints, Pixels, and Gray Levels: Digitizing Image Data: James B. PawleyÖner AyhanNo ratings yet
- Lec 22Document7 pagesLec 22Divya AgarwalNo ratings yet
- New UltrasoundDocument30 pagesNew Ultrasoundamittewarii100% (1)
- DQE SimplifiedDocument8 pagesDQE SimplifiedBen100% (1)
- The Radiographic ImageDocument18 pagesThe Radiographic ImageMohamed AufNo ratings yet
- Espectroscopia 3 inDocument19 pagesEspectroscopia 3 inErika ApazaNo ratings yet
- Factors Relating To The Production of Radiograph Lec3Document8 pagesFactors Relating To The Production of Radiograph Lec3شبكة المستقبلNo ratings yet
- Image Noise by SprawlsDocument14 pagesImage Noise by SprawlsVincent VicuñaNo ratings yet
- American Association For Laboratory AccreditationDocument4 pagesAmerican Association For Laboratory AccreditationSai FujiwaraNo ratings yet
- Indirect Verification PDFDocument1 pageIndirect Verification PDFSai FujiwaraNo ratings yet
- Liquid Penetrant Inspection - NDT Validation CentreDocument2 pagesLiquid Penetrant Inspection - NDT Validation CentreSai FujiwaraNo ratings yet
- Hot CrackingDocument1 pageHot CrackingSai FujiwaraNo ratings yet
- Guidelines For The Welded Fabrication of Nickel-Containing Stainless Steels For Corrosion Resistant ServicesDocument0 pagesGuidelines For The Welded Fabrication of Nickel-Containing Stainless Steels For Corrosion Resistant ServicesSai FujiwaraNo ratings yet
- 05 - Diagnostic Radiology IIDocument27 pages05 - Diagnostic Radiology IISai FujiwaraNo ratings yet
- NDT PerformanceDocument5 pagesNDT PerformanceSai FujiwaraNo ratings yet
- PmiDocument6 pagesPmiSai FujiwaraNo ratings yet
- Astm E1165Document7 pagesAstm E1165Sai FujiwaraNo ratings yet
- Grit Blast Cleaning in Water-Washable Fluorescent Liquid Penetrant Examination (LPE)Document5 pagesGrit Blast Cleaning in Water-Washable Fluorescent Liquid Penetrant Examination (LPE)Sai FujiwaraNo ratings yet
- (0.33 FT To 100 FT) (0.16 FT To 200 FT) (0.16 FT To 330 FT)Document2 pages(0.33 FT To 100 FT) (0.16 FT To 200 FT) (0.16 FT To 330 FT)Sai FujiwaraNo ratings yet
- Rope Access TechniqueDocument14 pagesRope Access TechniqueSai FujiwaraNo ratings yet
- X-Ray Production: Online TextbookDocument14 pagesX-Ray Production: Online TextbookSai FujiwaraNo ratings yet
- X-Rays From Free ElectronsDocument3 pagesX-Rays From Free ElectronsSai FujiwaraNo ratings yet
- Arpansa X RaysDocument4 pagesArpansa X RaysSai FujiwaraNo ratings yet
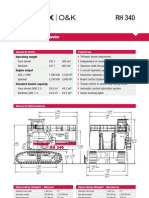
- Hydraulic Mining ExcavatorDocument8 pagesHydraulic Mining Excavatorasditia_07100% (1)
- Hand Out Fire SurpressDocument69 pagesHand Out Fire SurpressSeptiawanWandaNo ratings yet
- Union Test Prep Nclex Study GuideDocument115 pagesUnion Test Prep Nclex Study GuideBradburn Nursing100% (2)
- Soujanya Reddy (New)Document6 pagesSoujanya Reddy (New)durgaNo ratings yet
- Chapter 4 - Basic ProbabilityDocument37 pagesChapter 4 - Basic Probabilitynadya shafirahNo ratings yet
- Open Letter To Hon. Nitin Gadkari On Pothole Problem On National and Other Highways in IndiaDocument3 pagesOpen Letter To Hon. Nitin Gadkari On Pothole Problem On National and Other Highways in IndiaProf. Prithvi Singh KandhalNo ratings yet
- 10 Killer Tips For Transcribing Jazz Solos - Jazz AdviceDocument21 pages10 Killer Tips For Transcribing Jazz Solos - Jazz Advicecdmb100% (2)
- When A Snobbish Gangster Meets A Pervert CassanovaDocument62 pagesWhen A Snobbish Gangster Meets A Pervert CassanovaMaria Shiela Mae Baratas100% (1)
- Introduction To BiogasDocument5 pagesIntroduction To BiogasLouis EldertardNo ratings yet
- C4 Vectors - Vector Lines PDFDocument33 pagesC4 Vectors - Vector Lines PDFMohsin NaveedNo ratings yet
- Elpodereso Case AnalysisDocument3 pagesElpodereso Case AnalysisUsama17100% (2)
- PP Master Data Version 002Document34 pagesPP Master Data Version 002pranitNo ratings yet
- Epreuve Anglais EG@2022Document12 pagesEpreuve Anglais EG@2022Tresor SokoudjouNo ratings yet
- Upes School of Law Lac & Adr Association: PresentsDocument7 pagesUpes School of Law Lac & Adr Association: PresentsSuvedhya ReddyNo ratings yet
- Iaea Tecdoc 1092Document287 pagesIaea Tecdoc 1092Andres AracenaNo ratings yet
- Chapter 2Document8 pagesChapter 2Fahmia MidtimbangNo ratings yet
- Dakua Makadre PresentationDocument12 pagesDakua Makadre PresentationEli Briggs100% (1)
- T5 B11 Victor Manuel Lopez-Flores FDR - FBI 302s Re VA ID Cards For Hanjour and Almihdhar 195Document11 pagesT5 B11 Victor Manuel Lopez-Flores FDR - FBI 302s Re VA ID Cards For Hanjour and Almihdhar 1959/11 Document Archive100% (2)
- Low Budget Music Promotion and PublicityDocument41 pagesLow Budget Music Promotion and PublicityFola Folayan100% (3)
- Walking in Space - Lyrics and Chord PatternDocument2 pagesWalking in Space - Lyrics and Chord Patternjohn smithNo ratings yet
- Participants ListDocument13 pagesParticipants Listmailway002No ratings yet
- Owners Manual Air Bike Unlimited Mag 402013Document28 pagesOwners Manual Air Bike Unlimited Mag 402013David ChanNo ratings yet
- Grid Pattern PortraitDocument8 pagesGrid Pattern PortraitEmma FravigarNo ratings yet
- SABRE MK-3 CFT Gel SpecDocument1 pageSABRE MK-3 CFT Gel Specseregio12No ratings yet
- Artificial Intelligence Techniques For Encrypt Images Based On The Chaotic System Implemented On Field-Programmable Gate ArrayDocument10 pagesArtificial Intelligence Techniques For Encrypt Images Based On The Chaotic System Implemented On Field-Programmable Gate ArrayIAES IJAINo ratings yet
- 1916 South American Championship Squads - WikipediaDocument6 pages1916 South American Championship Squads - WikipediaCristian VillamayorNo ratings yet
- Adjective & VerbsDocument3 pagesAdjective & VerbsDennis BerkNo ratings yet
- P 348Document196 pagesP 348a123456978No ratings yet
- 2016 W-2 Gross Wages CityDocument16 pages2016 W-2 Gross Wages CityportsmouthheraldNo ratings yet
- Back Propagation Neural NetworkDocument10 pagesBack Propagation Neural NetworkAhmad Bisyrul HafiNo ratings yet
- Weapons of Mass Instruction: A Schoolteacher's Journey Through the Dark World of Compulsory SchoolingFrom EverandWeapons of Mass Instruction: A Schoolteacher's Journey Through the Dark World of Compulsory SchoolingRating: 4.5 out of 5 stars4.5/5 (149)
- The Story of the World, Vol. 1 AudiobookFrom EverandThe Story of the World, Vol. 1 AudiobookRating: 4.5 out of 5 stars4.5/5 (3)
- Stoicism The Art of Happiness: How the Stoic Philosophy Works, Living a Good Life, Finding Calm and Managing Your Emotions in a Turbulent World. New VersionFrom EverandStoicism The Art of Happiness: How the Stoic Philosophy Works, Living a Good Life, Finding Calm and Managing Your Emotions in a Turbulent World. New VersionRating: 5 out of 5 stars5/5 (51)
- Summary: The Laws of Human Nature: by Robert Greene: Key Takeaways, Summary & AnalysisFrom EverandSummary: The Laws of Human Nature: by Robert Greene: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (30)
- How to Talk to Anyone: Learn the Secrets of Good Communication and the Little Tricks for Big Success in RelationshipFrom EverandHow to Talk to Anyone: Learn the Secrets of Good Communication and the Little Tricks for Big Success in RelationshipRating: 4.5 out of 5 stars4.5/5 (1135)
- Summary: Trading in the Zone: Trading in the Zone: Master the Market with Confidence, Discipline, and a Winning Attitude by Mark Douglas: Key Takeaways, Summary & AnalysisFrom EverandSummary: Trading in the Zone: Trading in the Zone: Master the Market with Confidence, Discipline, and a Winning Attitude by Mark Douglas: Key Takeaways, Summary & AnalysisRating: 5 out of 5 stars5/5 (15)
- Learn Spanish While SleepingFrom EverandLearn Spanish While SleepingRating: 4 out of 5 stars4/5 (20)
- Cynical Theories: How Activist Scholarship Made Everything about Race, Gender, and Identity―and Why This Harms EverybodyFrom EverandCynical Theories: How Activist Scholarship Made Everything about Race, Gender, and Identity―and Why This Harms EverybodyRating: 4.5 out of 5 stars4.5/5 (221)
- Follow your interests: This will make you feel better about yourself and what you can do.: inspiration and wisdom for achieving a fulfilling life.From EverandFollow your interests: This will make you feel better about yourself and what you can do.: inspiration and wisdom for achieving a fulfilling life.No ratings yet
- The 16 Undeniable Laws of Communication: Apply Them and Make the Most of Your MessageFrom EverandThe 16 Undeniable Laws of Communication: Apply Them and Make the Most of Your MessageRating: 5 out of 5 stars5/5 (73)
- Summary: I'm Glad My Mom Died: by Jennette McCurdy: Key Takeaways, Summary & AnalysisFrom EverandSummary: I'm Glad My Mom Died: by Jennette McCurdy: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (2)
- Dumbing Us Down: The Hidden Curriculum of Compulsory SchoolingFrom EverandDumbing Us Down: The Hidden Curriculum of Compulsory SchoolingRating: 4.5 out of 5 stars4.5/5 (498)
- Financial Feminist: Overcome the Patriarchy's Bullsh*t to Master Your Money and Build a Life You LoveFrom EverandFinancial Feminist: Overcome the Patriarchy's Bullsh*t to Master Your Money and Build a Life You LoveRating: 5 out of 5 stars5/5 (1)
- Summary: The 5AM Club: Own Your Morning. Elevate Your Life. by Robin Sharma: Key Takeaways, Summary & AnalysisFrom EverandSummary: The 5AM Club: Own Your Morning. Elevate Your Life. by Robin Sharma: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (22)
- How to Improve English Speaking: How to Become a Confident and Fluent English SpeakerFrom EverandHow to Improve English Speaking: How to Become a Confident and Fluent English SpeakerRating: 4.5 out of 5 stars4.5/5 (56)
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisFrom EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisRating: 5 out of 5 stars5/5 (3)
- Rooted in Joy: Creating a Classroom Culture of Equity, Belonging, and CareFrom EverandRooted in Joy: Creating a Classroom Culture of Equity, Belonging, and CareNo ratings yet
- Make It Stick by Peter C. Brown, Henry L. Roediger III, Mark A. McDaniel - Book Summary: The Science of Successful LearningFrom EverandMake It Stick by Peter C. Brown, Henry L. Roediger III, Mark A. McDaniel - Book Summary: The Science of Successful LearningRating: 4.5 out of 5 stars4.5/5 (55)
- You Are Not Special: And Other EncouragementsFrom EverandYou Are Not Special: And Other EncouragementsRating: 4.5 out of 5 stars4.5/5 (6)
- Nobody Left to Hate: Teaching Compassion after ColumbineFrom EverandNobody Left to Hate: Teaching Compassion after ColumbineRating: 4.5 out of 5 stars4.5/5 (9)
- Learn Italian While SleepingFrom EverandLearn Italian While SleepingRating: 4.5 out of 5 stars4.5/5 (7)
- Summary: Greenlights: by Matthew McConaughey: Key Takeaways, Summary & AnalysisFrom EverandSummary: Greenlights: by Matthew McConaughey: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (6)
- Learn English: Must-Know American English Slang Words & Phrases (Extended Version)From EverandLearn English: Must-Know American English Slang Words & Phrases (Extended Version)Rating: 5 out of 5 stars5/5 (30)
- Why Smart People Hurt: A Guide for the Bright, the Sensitive, and the CreativeFrom EverandWhy Smart People Hurt: A Guide for the Bright, the Sensitive, and the CreativeRating: 3.5 out of 5 stars3.5/5 (54)