Professional Documents
Culture Documents
Fluid Imbalance (NCP)
Uploaded by
Putry RainismOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Fluid Imbalance (NCP)
Uploaded by
Putry RainismCopyright:
Available Formats
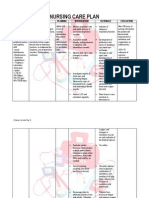
Nursing Diagnosis: Deficient Fluid Volume
Hypovolemia; Dehydration
NOC Outcomes (Nursing Outcomes Classification)
Suggested NOC Labels Fluid Balance Hydration
NIC Interventions (Nursing Interventions Classification)
Suggested NIC Labels Fluid Monitoring Fluid Management Fluid Resuscitation
NANDA Definition: Decreased intravascular, interstitial, and/or intracellular fluid. This refers to dehydration, water loss alone without change in sodium Fluid volume deficit, or hypovolemia, occurs from a loss of body fluid or the shift of fluids into the third space, or from a reduced fluid intake. Common sources for fluid loss are the gastrointestinal (GI) tract, polyuria, and increased perspiration. Fluid volume deficit may be an acute or chronic condition managed in the hospital, outpatient center, or home setting. The therapeutic goal is to treat the underlying disorder and return the extracellular fluid compartment to normal. Treatment consists of restoring fluid volume and correcting any electrolyte imbalances. Early recognition and treatment are paramount to prevent potentially life-threatening hypovolemic shock. Elderly patients are more likely to develop fluid imbalances. Defining Characteristics: Decreased urine output Concentrated urine Output greater than intake Sudden weight loss Decreased venous filling Hemoconcentration Increased serum sodium Hypotension Thirst Increased pulse rate Decreased skin turgor Dry mucous membranes Weakness Possible weight gain Changes in mental status
Related Factors: Inadequate fluid intake Active fluid loss (diuresis, abnormal drainage or bleeding, diarrhea) Failure of regulatory mechanisms Electrolyte and acid-base imbalances Increased metabolic rate (fever, infection) Fluid shifts (edema or effusions) Expected Outcomes Patient experiences adequate fluid volume and electrolyte balance as evidenced by urine output greater than 30 ml/hr, normotensive blood pressure (BP), heart rate (HR) 100 beats/min, consistency of weight, and normal skin turgor.
Ongoing Assessment
Obtain patient history to ascertain the probable cause of the fluid disturbance. This can help to guide interventions. Causes may include acute trauma and bleeding, reduced fluid intake from changes in cognition, large amount of drainage post-surgery, or persistent diarrhea. Assess or instruct patient to monitor weight daily and consistently, with same scale, and preferably at the same time of day. This facilitates accurate measurement and follows trends. Evaluate fluid status in relation to dietary intake. Determine if patient has been on a fluid restriction. Most fluid enters the body through drinking, water in foods, and water formed by oxidation of foods. Monitor and document vital signs. Sinus tachycardia may occur with hypovolemia to maintain an effective cardiac output. Usually the pulse is weak, and may be irregular if electrolyte imbalance also occurs. Hypotension is evident in hypovolemia. Monitor blood pressure for orthostatic changes (from patient lying supine to high-Fowlers). Note the following orthostatic hypotension significance: Greater than 10 mm Hg drop: circulating blood volume is decreased by 20%. Greater than 20 to 30 mm Hg drop: circulating blood volume is decreased by 40%. Assess skin turgor and mucous membranes for signs of dehydration. The skin in elderly patients loses its elasticity; therefore skin turgor should be assessed over the sternum or on the inner thighs. Longitudinal furrows may be noted along the tongue. Assess color and amount of urine. Report urine output less than 30 ml/hr for 2 consecutive hours. Concentrated urine denotes fluid deficit. Monitor temperature. Febrile states decrease body fluids through perspiration and increased respiration.
Monitor active fluid loss from wound drainage, tubes, diarrhea, bleeding, and vomiting; maintain accurate input and output. Monitor serum electrolytes and urine osmolality and report abnormal values. Elevated hemoglobin and elevated blood urea nitrogen (BUN) suggest fluid deficit. Urine-specific gravity is likewise increased. Document baseline mental status and record during each nursing shift. Dehydration can alter mental status. Evaluate whether patient has any related heart problem before initiating parenteral therapy. Cardiac and elderly patients often have precarious fluid balances and are prone to develop pulmonary edema. Determine patients fluid preferences: type, temperature (hot or cold). During treatment, monitor closely for signs of circulatory overload (headache, flushed skin, tachycardia, venous distention, elevated central venous pressure [CVP], shortness of breath, increased BP, tachypnea, cough). This prevents complications associated with therapy. If hospitalized, monitor hemodynamic status including CVP, pulmonary artery pressure (PAP), and pulmonary capillary wedge pressure (PCWP) if available. This direct measurement serves as optimal guide for therapy.
Therapeutic Interventions
Encourage patient to drink prescribed fluid amounts. If oral fluids are tolerated, provide oral fluids patient prefers. Place at bedside within easy reach. Provide fresh water and a straw. Be creative in selecting fluid sources (e.g., flavored gelatin, frozen juice bars, sports drink). Oral fluid replacement is indicated for mild fluid deficit. Elderly patients have a decreased sense of thirst and may need ongoing reminders to drink. Assist patient if unable to feed self and encourage caregiver to assist with feedings as appropriate. Plan daily activities. Planning prevents patient from being too tired at mealtimes. Provide oral hygiene. This promotes interest in drinking.
For more severe hypovolemia:
Obtain and maintain a large-bore intravenous (IV) catheter. Parenteral fluid replacement is indicated to prevent shock. Administer parenteral fluids as ordered. Anticipate the need for an IV fluid challenge with immediate infusion of fluids for patients with abnormal vital signs. Administer blood products as prescribed. These may be required for active GI bleeding.
Assist the physician with insertion of a central venous line and arterial line as indicated. This allows more effective fluid administration and monitoring. Maintain IV flow rate. Should signs of fluid overload occur, stop infusion and sit patient up or dangle. These decrease venous return and optimize breathing. Elderly patients are especially susceptible to fluid overload.
Institute measures to control excessive electrolyte loss (e.g., resting the GI tract, administering antipyretics as ordered). Once ongoing fluid losses have stopped, begin to advance the diet in volume and composition. For hypovolemia due to severe diarrhea or vomiting, administer antidiarrheal or antiemetic medications as prescribed, in addition to IV fluids.
Education/Continuity of Care
Describe or teach causes of fluid losses or decreased fluid intake. Explain or reinforce rationale and intended effect of treatment program. Explain importance of maintaining proper nutrition and hydration. Teach interventions to prevent future episodes of inadequate intake. Patients need to understand the importance of drinking extra fluid during bouts of diarrhea, fever, and other conditions causing fluid deficits. Inform patient or caregiver of importance of maintaining prescribed fluid intake and special diet considerations involved. If patients are to receive IV fluids at home, instruct caregiver in managing IV equipment. Allow sufficient time for return demonstration. Responsibility for maintaining venous access sites and IV supplies may be overwhelming for caregiver. In addition, elderly caregivers may not have the cognitive ability and manual dexterity required for this therapy. Refer to home health nurse as appropriate.
Nursing Diagnosis: Excess Fluid Volume
Hypervolemia; Fluid Overload
NOC Outcomes (Nursing Outcomes Classification)
Suggested NOC Labels Fluid Balance
NIC Interventions (Nursing Interventions Classification)
Suggested NIC Labels Fluid Monitoring Fluid Management
NANDA Definition: Increased isotonic fluid retention Fluid volume excess, or hypervolemia, occurs from an increase in total body sodium content and an increase in total body water. This fluid excess usually results from compromised regulatory mechanisms for sodium and water as seen in congestive heart failure (CHF), kidney failure, and liver failure. It may also be caused by excessive intake of sodium from foods, intravenous (IV) solutions, medications, or diagnostic contrast dyes. Hypervolemia may be an acute or chronic condition managed in the hospital, outpatient center, or home setting. The therapeutic goal is to treat the underlying disorder and return the extracellular fluid compartment to normal. Treatment consists of fluid and sodium restriction, and the use of diuretics. For acute cases dialysis may be required. Defining Characteristics: Weight gain Edema Bounding pulses Shortness of breath; orthopnea Pulmonary congestion on x-ray Abnormal breath sounds: crackles (rales) Change in respiratory pattern Third heart sound (S3) Intake greater than output Decreased hemoglobin or hematocrit Increased blood pressure Increased central venous pressure (CVP) Increased pulmonary artery pressure (PAP) Jugular vein distension Change in mental status (lethargy or confusion) Oliguria Specific gravity changes Azotemia Change in electrolytes Restlessness and anxiety
Related Factors: Excessive fluid intake Excessive sodium intake Renal insufficiency or failure Steroid therapy Low protein intake or malnutrition Decreased cardiac output; chronic or acute heart disease Head injury Liver disease Severe stress Hormonal disturbances Expected Outcomes Patient maintains adequate fluid volume and electrolyte balance as evidenced by vital signs within normal limits, clear lung sounds, pulmonary congestion absent on x-ray, and resolution of edema.
Ongoing Assessment
Obtain patient history to ascertain the probable cause of the fluid disturbance. This can help to guide interventions. May include increased fluids or sodium intake, or compromised regulatory mechanisms. Assess or instruct patient to monitor weight daily and consistently, with same scale and preferably at the same time of day. Instruction facilitates accurate measurement and helps to follow trends. Monitor for a significant weight change (2 pounds) in 1 day. Evaluate weight in relation to nutritional status. In some heart failure patients, weight may be a poor indicator of fluid volume status. Poor nutrition and decreased appetite over time result in a decrease in weight, which may be accompanied by fluid retention even though the net weight remains unchanged. If patient is on fluid restriction, review daily log or chart for recorded intake. Patients should be reminded to include items that are liquid at room temperature such as Jell-O, sherbet, and Popsicles. Monitor and document vital signs. Sinus tachycardia and increased blood pressure are seen in early stages. Elderly patients have reduced response to catecholamines, thus their response to fluid overload may be blunted, with less rise in heart rate. Monitor for distended neck veins and ascites. Monitor abdominal girth to follow any ascites accurately. Auscultate for a third sound, and assess for bounding peripheral pulses. These are signs of fluid overload.
Assess for crackles in lungs, changes in respiratory pattern, shortness of breath, and orthopnea. These are early signs of pulmonary congestion. Assess for presence of edema by palpating over tibia, ankles, feet, and sacrum. Pitting edema is manifested by a depression that remains after ones finger is pressed over an edematous area and then removed. Grade edema from trace (indicating barely perceptible) to 4 (severe edema). Measurement of an extremity with a measuring tape is another method of following edema. Monitor chest x-ray reports. As interstitial edema accumulates, the x-rays show cloudy white lung fields. Monitor input and output closely. Although overall fluid intake may be adequate, shifting of fluid out of the intravascular to the extravascular spaces may result in dehydration. The risk of this occurring increases when diuretics are given. Patients may use diaries for home assessment. Evaluate urine output in response to diuretic therapy. Focus is on monitoring the response to the diuretics, rather than the actual amount voided. At home, it is unrealistic to expect patients to measure each void. Therefore recording two voids versus six voids after a diuretic medication may provide more useful information. NOTE: Fluid volume excess in the abdomen may interfere with absorption of oral diuretic medications. Medications may need to be given intravenously by a nurse in the home or outpatient setting. Monitor for excessive response to diuretics: 2-pound loss in 1 day, hypotension, weakness, blood urea nitrogen (BUN) elevated out of proportion to serum creatinine level. Monitor serum electrolytes, urine osmolality, and urine-specific gravity. Assess the need for an indwelling urinary catheter. Treatment focuses on diuresis of excess fluid. During therapy, monitor for signs of hypovolemia. Monitoring prevents complications associated with therapy. If hospitalized, monitor hemodynamic status including CVP, PAP, and PCWP, if available. This direct measurement serves as optimal guide for therapy.
Therapeutic Interventions
Institute/instruct patient regarding fluid restrictions as appropriate. This helps reduce extracellular volume. For some patients, fluids may need to be restricted to 1000 ml/day. Provide innovative techniques for monitoring fluid allotment at home. For example, suggest that patients measure out and pour into a large pitcher the prescribed daily fluid allowance (e.g., 1000 ml); then every time patient drinks some fluid, he or she is to remove that amount from the pitcher. This provides a visual guide for how much fluid is still allowed throughout the day. Restrict sodium intake as prescribed. Sodium diets of 2 to 3 g are usually prescribed.
Administer or instruct patient to take diuretics as prescribed. Diuretic therapy may include several different types of agents for optimal therapy, depending on the acuteness or chronicity of the problem. For chronic patients, compliance is often difficult for patients trying to maintain a normal lifestyle. Instruct patient to avoid medications that may cause fluid retention, such as over-the-counter nonsteroidal antiinflammatory agents, certain vasodilators, and steroids. Elevate edematous extremities. This increases venous return and, in turn, decreases edema. Reduce constriction of vessels (e.g., use appropriate garments, avoid crossing of legs or ankles). This prevents venous pooling. Instruct in need for antiembolic stockings or bandages as ordered. These help promote venous return and minimize fluid accumulation in the extremities. Provide interventions related to specific etiological factors (e.g., inotropic medications for heart failure, paracentesis for liver disease).
For acute patients:
Consider admission to acute care setting for hemofiltration or ultrafiltration. This is a very effective method to draw off excess fluid. Collaborate with the pharmacist to maximally concentrate IVs and medications. This decreases unnecessary fluids. Apply saline lock on IV line. This maintains patency but decreases fluid delivered to patient in a 24-hour period. Administer IV fluids through infusion pump, if possible. This ensures accurate delivery of IV fluids. Assist with repositioning every 2 hours if patient is not mobile. This prevents fluid accumulation in dependent areas.
Education/Continuity of Care
Teach causes of fluid volume excess and/or excess intake to patient or caregiver. Provide information as needed regarding the individuals medical diagnosis (e.g., congestive heart failure [CHF], renal failure). Explain or reinforce rationale and intended effect of treatment program. Identify signs and symptoms of fluid volume excess. Explain importance of maintaining proper nutrition and hydration, and diet modifications. Identify symptoms to be reported.
MNEMONIC Hypernatremia: Think of SALT -Skin flushed -Agitation -Low-grade fever -Thirst Reciprocal relationship between calcium and phosphorus: INCREASED Ca2+ = DECREASED PO43-Increasing serum calcium levels decreases phosphate levels -Decreasing serum calcium increases phosphate Chvosteks and Trousseaus signs; Tetany, irritability, and seizures: Hypocalcemia Hypomagnesemia Hyperphosphatemia Electrolyte imbalances which can potentiate dig toxicity: Hypokalemia Hypomagnesemia Hypercalcemia Electrolyte imbalances which can cause dysrhythmias: Hypo/ hypokalemia Hypomagnesemia Hypocalcemia Both HYPO and HYPER natremia can cause mental confusion, seizures, and coma Both HYPO and HYPER kalemia can cause cardiac dysrhythmias progressing to ventricular fibrillation and asystole. Think "cardiac" with both. Hyperkalemia is the most deadly of all electrolyte imbalances.
You might also like
- 1 Ineffective Breathing PatternDocument8 pages1 Ineffective Breathing PatternNoel MontemayorNo ratings yet
- NCP CKDDocument3 pagesNCP CKDRiel TumandaNo ratings yet
- Nursing Care Plans For UTIDocument2 pagesNursing Care Plans For UTIHannah Pin50% (2)
- Nursing Care Plan: Congestive Heart Failure-Deep Vein ThrombosisDocument19 pagesNursing Care Plan: Congestive Heart Failure-Deep Vein ThrombosisRiza Angela BarazanNo ratings yet
- Activity Intolerance Care PlanDocument4 pagesActivity Intolerance Care Planapi-315890029No ratings yet
- NCP of Difficulty of BreathingDocument2 pagesNCP of Difficulty of BreathingMan GatuankoNo ratings yet
- Ineffective Airway ClearanceDocument2 pagesIneffective Airway ClearanceHanya Bint PotawanNo ratings yet
- Decrease Cardiac OutputDocument6 pagesDecrease Cardiac OutputGerardeanne ReposarNo ratings yet
- Careplan For Sickle Cell DiseaseDocument21 pagesCareplan For Sickle Cell DiseaseEcaroh Hew SmailliwNo ratings yet
- Hypokalemia NCP PDFDocument4 pagesHypokalemia NCP PDFMussaib MushtaqNo ratings yet
- Cardiogenic and Septic Shock LectureDocument27 pagesCardiogenic and Septic Shock LectureMohd EdieNo ratings yet
- Altered Nutrition Nursing DiagnosisDocument4 pagesAltered Nutrition Nursing DiagnosisAndrea BroccoliNo ratings yet
- NCP - Excess Fluid Volume (Aortic Stenosis)Document3 pagesNCP - Excess Fluid Volume (Aortic Stenosis)Daniel Vergara Arce100% (3)
- Mrs. Bagent 1-9 BWAKANANG SHETDocument5 pagesMrs. Bagent 1-9 BWAKANANG SHETaaron tabernaNo ratings yet
- NCP Ineffective Airway Clearance Related To The Accumulation of Secretions As Evidence by Decrease in Respiratory Rate and NGT and ET Tube Attached and Crackles at The Left Base of The LungsDocument3 pagesNCP Ineffective Airway Clearance Related To The Accumulation of Secretions As Evidence by Decrease in Respiratory Rate and NGT and ET Tube Attached and Crackles at The Left Base of The LungsSarah Ann Jamilla FaciolanNo ratings yet
- Nursing 215 Care Plan 2 FinalDocument7 pagesNursing 215 Care Plan 2 Finalapi-283303129No ratings yet
- Ate Gara NCP (Activity Intolerance)Document2 pagesAte Gara NCP (Activity Intolerance)Kimsha ConcepcionNo ratings yet
- NCP For CHF 3 Activity IntoleranceDocument2 pagesNCP For CHF 3 Activity IntoleranceAngelyn ArdinesNo ratings yet
- Ineffective Tissue PerfusionDocument2 pagesIneffective Tissue PerfusionDiane ReyNo ratings yet
- Risk For InfectionDocument18 pagesRisk For InfectionValiant Baybay0% (1)
- Nursing Care Plan For Heart Failure ChronicDocument26 pagesNursing Care Plan For Heart Failure ChronicbrantNo ratings yet
- Hyper Nat Remi ADocument6 pagesHyper Nat Remi Ayeof_kang08No ratings yet
- 10 CaritosDocument3 pages10 CaritosDARREN EDMARK100% (4)
- NCPDocument9 pagesNCPKarell Eunice Estrellado Gutierrez100% (1)
- Nursing Care Plan HF FinalDocument10 pagesNursing Care Plan HF FinalCristina L. JaysonNo ratings yet
- Nursing Diagnosis Impaired Gas ExchangeDocument7 pagesNursing Diagnosis Impaired Gas ExchangeZycon Rodney Ae'zecquel Gachallan50% (2)
- Impaired Gas Exchange Care PlanDocument5 pagesImpaired Gas Exchange Care Planjakifer50% (2)
- NCPDocument11 pagesNCPJaziel Remo100% (1)
- Ineffective Tissue PerfusionDocument2 pagesIneffective Tissue PerfusionClaidelyn De Leyola100% (1)
- NURSING CARE PLAN Sensory-Perception DisturbanceDocument2 pagesNURSING CARE PLAN Sensory-Perception DisturbanceBernadette100% (1)
- NCPDocument9 pagesNCPTracy Camille EscobarNo ratings yet
- ABC: Sickle-Cell Anemia, Shock, PoisoningDocument46 pagesABC: Sickle-Cell Anemia, Shock, Poisoningroneln100% (1)
- Nursing Care PlanDocument14 pagesNursing Care PlanVin Landicho100% (1)
- Case Study RespiDocument3 pagesCase Study RespiMark Jheran AlvarezNo ratings yet
- HyponatremiaDocument6 pagesHyponatremiaJaymart Saclolo CostillasNo ratings yet
- Fluid Volume DeficitDocument2 pagesFluid Volume DeficitRuby AnneNo ratings yet
- NCP Inffective Tissue PerfusionDocument3 pagesNCP Inffective Tissue PerfusionPaul Cubacub0% (1)
- NCP Ineffective Cardiopulmonary PerfusionDocument3 pagesNCP Ineffective Cardiopulmonary PerfusionjamiemapanaoNo ratings yet
- Ineffective Cerebral Tissue Perfusion Related ToDocument7 pagesIneffective Cerebral Tissue Perfusion Related TohannahNo ratings yet
- Nursing Care PlanDocument11 pagesNursing Care Planaycee0316100% (1)
- Daily NCPDocument5 pagesDaily NCPKuennie SabalNo ratings yet
- Ineffective Airway ClearanceDocument6 pagesIneffective Airway Clearanceapi-252726911No ratings yet
- Concept Map Pleural EffusionDocument1 pageConcept Map Pleural Effusionapi-341263362No ratings yet
- Left-Sided Heart FailureDocument3 pagesLeft-Sided Heart FailureKhalid Mahmud ArifinNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective Short Term Short TermDocument2 pagesAssessment Diagnosis Planning Intervention Rationale Evaluation Subjective Short Term Short TermFrancis Xavier S. MendezNo ratings yet
- Risk For Decreased Cardiac OutputDocument3 pagesRisk For Decreased Cardiac OutputSid Artemis FriasNo ratings yet
- Ineffective Airway ClearanceDocument2 pagesIneffective Airway Clearancejancel_bollaNo ratings yet
- NCPDocument2 pagesNCPNichole Audrey SaavedraNo ratings yet
- Fluid Volume DeficitDocument3 pagesFluid Volume Deficitprickybiik100% (1)
- Short Term: Independent: Independent: Short TermDocument2 pagesShort Term: Independent: Independent: Short TermAndre ImperialNo ratings yet
- Problem Nursing Diagnosis Outcome Plan Intervention Evaluation Subjective Data: "Masakit Po Yung Sa Short Term: IndependentDocument2 pagesProblem Nursing Diagnosis Outcome Plan Intervention Evaluation Subjective Data: "Masakit Po Yung Sa Short Term: IndependentkyawNo ratings yet
- Monitoring cerebral perfusion in stroke patientDocument9 pagesMonitoring cerebral perfusion in stroke patientKarel LuNo ratings yet
- Impaired Gas ExchangeDocument1 pageImpaired Gas Exchangeruggero07No ratings yet
- Nursing Diagnosis: Urinary Retention: NOC Outcomes (Nursing Outcomes Classification)Document4 pagesNursing Diagnosis: Urinary Retention: NOC Outcomes (Nursing Outcomes Classification)rem_No ratings yet
- Nursing DiagnosisDocument4 pagesNursing DiagnosisMavy AndresNo ratings yet
- Medical Surgical Fluid and Electrolytes FVD FVEDocument7 pagesMedical Surgical Fluid and Electrolytes FVD FVEMichaelaKatrinaTrinidadNo ratings yet
- Fluid Volume Deficit (Dehydration) Nursing Care Plan - NurseslabsDocument17 pagesFluid Volume Deficit (Dehydration) Nursing Care Plan - NurseslabsA.No ratings yet
- Deficient Fluid Volume Nursing Diagnosis & Care Plan - RNlessonsDocument11 pagesDeficient Fluid Volume Nursing Diagnosis & Care Plan - RNlessonsA.No ratings yet
- Excess Fluid Volume - Nursing Diagnosis & Care Plan - NurseslabsDocument8 pagesExcess Fluid Volume - Nursing Diagnosis & Care Plan - NurseslabsEricsonMitraNo ratings yet
- Medical Diagnosis: Kidney Failure and Fluid Volume ExcessDocument74 pagesMedical Diagnosis: Kidney Failure and Fluid Volume ExcessSheela Khrystyn LeeNo ratings yet
- Pathology Quality ManualDocument83 pagesPathology Quality Manualrose_almonteNo ratings yet
- Swami Paramarthananda's Talks on Self-KnowledgeDocument332 pagesSwami Paramarthananda's Talks on Self-Knowledgemuralipmd100% (1)
- Risk of Ovarian Cancer Algorithm (ROCA) Using Serial CA 125Document9 pagesRisk of Ovarian Cancer Algorithm (ROCA) Using Serial CA 125primadian atnaryanNo ratings yet
- Cardiovascular SystemDocument10 pagesCardiovascular SystemitsmesuvekshaNo ratings yet
- Anger Management For Teens: by Fredric Provenzano, PHD, NCSP Seattle, WaDocument3 pagesAnger Management For Teens: by Fredric Provenzano, PHD, NCSP Seattle, WaJonathanKiehlNo ratings yet
- 1.agglutination ReactionDocument30 pages1.agglutination ReactionEINSTEIN2DNo ratings yet
- Final Siop Lesson Plan Name: Marla Leland Content Area: Science Grade Level: 4 Grade (New Standards) English LearnersDocument13 pagesFinal Siop Lesson Plan Name: Marla Leland Content Area: Science Grade Level: 4 Grade (New Standards) English Learnersapi-285366742No ratings yet
- The Bobath Concept (NDT) As Rehabilitation in Stroke Patients - Revisión SistemáticaDocument8 pagesThe Bobath Concept (NDT) As Rehabilitation in Stroke Patients - Revisión SistemáticaCristian Manuel Goicochea ChuqueNo ratings yet
- Public Notice Dated 16.11.2018-Disability-AppendixHDocument4 pagesPublic Notice Dated 16.11.2018-Disability-AppendixHDisability Rights AllianceNo ratings yet
- 01 - Chance - Fletcher, Clinical Epidemiology The Essentials, 5th EditionDocument19 pages01 - Chance - Fletcher, Clinical Epidemiology The Essentials, 5th EditionDaniel PalmaNo ratings yet
- Turmeric Benefits: Health Benefits of Turmeric - Are There Any Side Effects of Turmeric?Document5 pagesTurmeric Benefits: Health Benefits of Turmeric - Are There Any Side Effects of Turmeric?Angelyn Taberna NatividadNo ratings yet
- 504 Vs IEP Power PointDocument11 pages504 Vs IEP Power Pointbmorgan5No ratings yet
- Gold Foil: Safety Data SheetDocument4 pagesGold Foil: Safety Data SheetSyawatulshuhada SyawalNo ratings yet
- Cranial Base Dan Emergency CaseDocument34 pagesCranial Base Dan Emergency Caserahmad wahyuNo ratings yet
- Anatomic Therapy English PDFDocument339 pagesAnatomic Therapy English PDFBabou Parassouraman100% (3)
- TCM Cases - PainDocument671 pagesTCM Cases - PainGeander G. Bacheti100% (5)
- Failures in Periodontal Therapy: Review ArticleDocument6 pagesFailures in Periodontal Therapy: Review ArticlezinniaNo ratings yet
- Reproductive Health BillDocument22 pagesReproductive Health BillPhoebe CasipitNo ratings yet
- Headache History Checklist For PhysiciansDocument3 pagesHeadache History Checklist For PhysiciansFarazNo ratings yet
- 1 Gram Positive Bacterial InfectionDocument87 pages1 Gram Positive Bacterial InfectionCoy NuñezNo ratings yet
- How To Lower Your TriglyceridesDocument4 pagesHow To Lower Your TriglyceridesNoli CanlasNo ratings yet
- The MAST Test: A Simple Screening Tool for Alcohol ProblemsDocument3 pagesThe MAST Test: A Simple Screening Tool for Alcohol Problemsmysteryvan1981No ratings yet
- MSDS Berkat Saintifindo PDFDocument27 pagesMSDS Berkat Saintifindo PDFDianSelviaNo ratings yet
- Pharmacy Math CalculationsDocument8 pagesPharmacy Math CalculationsRahmawati KuswandiNo ratings yet
- Q A Random - 16Document8 pagesQ A Random - 16ja100% (1)
- 2322 Part B DCHB IndoreDocument278 pages2322 Part B DCHB Indoreksanjay209No ratings yet
- Ucmc DepartmentsDocument39 pagesUcmc DepartmentsAllen ZhuNo ratings yet
- 1536106348Document144 pages1536106348Saman SarKoNo ratings yet
- Levorphanol - The Forgotten Opioid PDFDocument6 pagesLevorphanol - The Forgotten Opioid PDFfchem11No ratings yet
- Yoga y AyurvedaDocument50 pagesYoga y AyurvedaManuel100% (1)