Professional Documents
Culture Documents
Ossification
Uploaded by
Fatin Nabihah JamilOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ossification
Uploaded by
Fatin Nabihah JamilCopyright:
Available Formats
Ossification is a bone formation process. It is a process where other connective tissue is replaced by bone connective tissue.
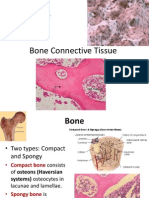
There are two types of ossification, namely intramembranous ossification and endochondral ossification. Intramembranous ossification Intramembranous ossification is a process where the mesenchyme will be replaced with bone tissue. This ossification does not use the cartilage model. It forms flat bones of skull, facial bones, mandible and clavicle (collarbone). There are four main stages in intramembranous ossification. The first stage is the formation of ossification centre. This formation starts with mesenchymal cells which are centrally located migrates and cluster together to form ossification centres. More than one ossification centres will form. Then, the mesenchymal cells in ossification centres will differentiate into osteoprogenitor cells and later these osteoprogenitor cells differentiate into osteoblasts. Osteoblast then will secrete osteoid. Osteoblasts will continuously produce more osteoid until they are surrounded by osteoid. Once they are surrounded by osteoid, they will separate from each other but still remain attached by thin cytoplasmic process. Next stage is calcification. In this stage, calcium phosphates are deposited in the osteoid to calcify bone matrix. This calcification of bone matrix traps osteoblasts in spaces. Osteoblast are now called as osteocytes and housed in lacuna. Formation of trabeculae is the third stage of intramembranous ossification. More osteoprogenitor cells rest on surface of calcified bone matrix and differentiate osteoblasts. Osteoblasts add more osteoid and causes bone matrix to enlarge. The bone matrix from adjacent ossification centres fuse to form trabeculae. In the spaces between trabeculae, the blood vessels within mesenchyme start to grow. Meanwhile, the mesenchyme remaining in between trabeculae differentiate into red bone marrow. The last stage of intramembranous process is the formation of periousteum. The mesenchyme at the periphery of the bone condenses to form periosteum. Initially, bone consists of trabeculae only. Then, spaces between trabeculae at outer part of bone are filled with bone matrix to form compact bone. Meanwhile, the remaining trabeculae in centres will form spongy bone.
Endochondral ossification Endochondral ossification occurs within cartilage. Cartilage model is needed for bone formation. The endochondral ossification results formation of long bones, vertebrae and pelvis. In long bones formation, during early embryonic development, limb buds which contain mesenchyme appear. The mesenchyme will form bones of the limb. There are six stages occurred in endochondral ossification. 1. Formation of hyaline cartilage model.
Mesenchymal cells aggregate and proliferate at the site of future bone. Mesenchymal cells differentiate into chondroblast, where chondroblasts secrete cartilage matrix (ECM) to form a hyaline cartilahe model. Now, chondroblasts that are surrounded by ECM are called chondrocytes. Perichondrium also develops around the cartilage model.
2.
Growth of hyaline cartilage model.
Basically, hyaline cartilage model grows in length and width, involving two mechanisms of growth namely interstitial growth and appositional growth. For growth in length, we called it as interstitial growth. Here, chondrocytes in the cartilage model do several works. One is undergoing mitosis and the other one is secreting cartilage matrix. New cartilage matrix is formed inside the existing cartilage model where we called as growth from within. This will thus cause the cartilage to increase in length. The second mechanism is appositional growth, where it will cause the cartilage to increase in width. New chondrboblasts are formed by the inner chondrogenic layer of perichondrium. These new chondroblasts will deposit new cartilage matrix on the outer surface of the existing cartilage model, causing increasing in width of cartilage.
3.
Formation of periosteal bone collar.
Cells in the perichondrium of the diaphysis of the model form osteoblasts. Thus, perichondrium will become periosteum. Osteoblasts form a layer of bone around the diaphysis which is called as periosteal bone collar.
4.
Calcification of cartilage in centre of diaphysis.
Chondrocytes in the centre of the cartilage model mature & enlarges (hypertrophy). Simultaneously, surrounding cartilage matrix begins to calcify. Periosteal bone collar & calcified cartilage does not allow diffusion of nutrients. Chondrocytes that does not receive nutrients will eventually die. Calcified cartilage breaks down because no chondrocytes to maintain cartilage. Walls of lacuna breakdown thus, adjacent lacunae become confluent, forming central cavity with remnants of calcified cartilage.
5.
Formation of primary ossification centre.
In this stage, periosteal bud (blood vessels) enter central cavity of the cartilage model while bringing osteoprogenitor celss and hemopoietic cells. Osteoprogenitor cells will form periosteum while hemopoietic cells form bone marrow. Here, the osteoprogenitor cells rest on surface of remnants of calcified cartilage and differentiate into osteoblasts. The osteoblasts then lay down osteoid on surface of remnants of calcified cartilage while simultaneously removing the remnants of calcified cartilage. This site is called as the primary ossification centre which it is the first site where cartilage is replaced by bone tissue. After that, osteoid becomes calcified while osteoblasts continue laying down more osteoid on the calcified bone matrix. The calcified matrix then enlarges to form trabeculae. This process continues. The primary ossification centre grows towards epiphyses. Eventually, all cartilage of diaphysis is replaced by bone (trabeculae). Then, osteoclasts resorb trabeculae in the diaphysis, thus forming medullary cavity.
6. Formation of secondary ossification centre. Secondary ossification centre, which occurs in epiphyses, is the centre of the bone formation that appears later than the primary ossification centre. The bone formation of secondary ossification centre is similar to the primary ossification centre except perioestal bone collar is not formed. Here, chondrocytes in cartilage hypertrophy; the cartilage matrix calcifies and chondrocytes die. The calcified cartilage matrix will be broken down. Also, the blood vessels together with osteoprogenitor cells that differentiate into osteoblast will enter epiphyses. Similar to the primary ossification centre, these osteoblasts lay down osteoid on the remants of calcified cartilage before removes the calcified cartilage to form trabeculae. In simple words, the only cartilage that remains is articular cartilage, which located at the articular surface at ends of bone and epiphyseal cartilage, which locates between the epiphyses and diaphysis.
You might also like
- 05 Locomotor SkeletalDocument288 pages05 Locomotor SkeletalkalumbaaquilaNo ratings yet
- Skeletal System More On ProcessDocument4 pagesSkeletal System More On Processsayie potatoNo ratings yet
- Skeletal System Lesson 2Document40 pagesSkeletal System Lesson 2Ella Nika FangonNo ratings yet
- Ossification of Bone.Document22 pagesOssification of Bone.Shimmering MoonNo ratings yet
- BoneDocument3 pagesBonePeter 'Pierre' RobsonNo ratings yet
- Endochondoral Ossification: A) Development of Cartilage ModelDocument5 pagesEndochondoral Ossification: A) Development of Cartilage ModelMadhi DinahNo ratings yet
- 2) Development and Growth of The BonesDocument3 pages2) Development and Growth of The BonesAris PaparisNo ratings yet
- Bone Formation & GrowthDocument3 pagesBone Formation & GrowtherinNo ratings yet
- BONE DEVELOPMENT XDocument5 pagesBONE DEVELOPMENT XabdulNo ratings yet
- Dev Skeletal SystemR2023Document83 pagesDev Skeletal SystemR2023amandagnaw19No ratings yet
- Bone Tissue-Growth and DevelopmentDocument53 pagesBone Tissue-Growth and Developmentgalaxyduck100% (1)
- HANDOUTS Prelim CH 6Document40 pagesHANDOUTS Prelim CH 6Abia Annieson A. LorenzoNo ratings yet
- Skeletal System: CartilageDocument20 pagesSkeletal System: CartilageGrace PascualNo ratings yet
- Dr. Sassia Lecture Bone Histology Part II July 4 2023Document39 pagesDr. Sassia Lecture Bone Histology Part II July 4 2023Ali ELKARGHALYNo ratings yet
- Bones OssificationDocument9 pagesBones OssificationNaveed AfridiNo ratings yet
- Chapter 6 Content Review Questions 1-8Document3 pagesChapter 6 Content Review Questions 1-8Rhonique MorganNo ratings yet
- Bones Ossification.Document9 pagesBones Ossification.Shimmering MoonNo ratings yet
- DO - DPM Bone Formation D2L 2014Document7 pagesDO - DPM Bone Formation D2L 2014snlee06No ratings yet
- Tolentino, Edjey Week4histolectDocument5 pagesTolentino, Edjey Week4histolectEDJEY TOLENTINONo ratings yet
- Anatomy and PhysiologyDocument26 pagesAnatomy and Physiologymusondaaugustine07_4No ratings yet
- Bone Development and Growth: Rosy Setiawati and Paulus RahardjoDocument20 pagesBone Development and Growth: Rosy Setiawati and Paulus Rahardjoputri aisheNo ratings yet
- Anaphy AnalysisDocument6 pagesAnaphy AnalysisLuna ScorpiusNo ratings yet
- Bone Formation - Ossification 2 PDFDocument35 pagesBone Formation - Ossification 2 PDFalan100% (1)
- Bone Development: Osteogenesis (Ossification) Endochondral OssificationDocument2 pagesBone Development: Osteogenesis (Ossification) Endochondral OssificationVanshika SethiNo ratings yet
- Bone FormationDocument26 pagesBone FormationNmesomaNo ratings yet
- Chapter 6 MariebDocument6 pagesChapter 6 Mariebmissy23papNo ratings yet
- BSN1 Unit 5 Skeletal SystemDocument101 pagesBSN1 Unit 5 Skeletal SystemCherub Chua100% (1)
- BoneDocument33 pagesBoneNihal BilalNo ratings yet
- Module-5-The Skeletal SystemDocument13 pagesModule-5-The Skeletal SystemMARIA CORAZON CONTANTENo ratings yet
- BC (H) - IV-Human Physiology-Bone Structure and Formation-2 & 3Document32 pagesBC (H) - IV-Human Physiology-Bone Structure and Formation-2 & 3Starco ForeverNo ratings yet
- Bone As A Living Dynamic TissueDocument14 pagesBone As A Living Dynamic TissueSuraj_Subedi100% (6)
- Intramembranous Ossification Involves (Meliputi) The ReplacementDocument8 pagesIntramembranous Ossification Involves (Meliputi) The ReplacementMuhammad SaifullohNo ratings yet
- BONEDocument48 pagesBONEnivethaseshaNo ratings yet
- Skeletal SystemDocument40 pagesSkeletal System119286kinNo ratings yet
- Histogenesis of BoneDocument6 pagesHistogenesis of BoneAlya Putri KhairaniNo ratings yet
- Human Anatomy 5Th Edition Saladin Solutions Manual Full Chapter PDFDocument28 pagesHuman Anatomy 5Th Edition Saladin Solutions Manual Full Chapter PDFJenniferWhitebctr100% (10)
- FRACTURESDocument85 pagesFRACTURESSteven OdhiamboNo ratings yet
- Human Anatomy 5th Edition Saladin Solutions ManualDocument7 pagesHuman Anatomy 5th Edition Saladin Solutions Manualjillhenrysetcjnzrfp100% (25)
- Ossification: ClavicleDocument7 pagesOssification: ClavicleAzmal FuadNo ratings yet
- Chapter 6 Bone Tissue 2304Document37 pagesChapter 6 Bone Tissue 2304Sav Oli100% (1)
- Compilations of Quick NotesDocument79 pagesCompilations of Quick NotesZaira MangalimanNo ratings yet
- The Skeletal System HDocument23 pagesThe Skeletal System HRajorshi MishraNo ratings yet
- Bones As A Living Dynamic TissueDocument13 pagesBones As A Living Dynamic TissueSanish Basnet100% (1)
- Script Case PressDocument7 pagesScript Case PressMa. Gina DerlaNo ratings yet
- CHAPTER 6 - Skeletal SystemDocument4 pagesCHAPTER 6 - Skeletal SystemArlen Joy V. AMPARONo ratings yet
- Bone & Ossification: Histology Part: Module2, Unit 3Document14 pagesBone & Ossification: Histology Part: Module2, Unit 3Obansa John100% (1)
- SkeletAl SystemDocument18 pagesSkeletAl SystemYen BailadoNo ratings yet
- Development of Cartilage, Bone and JointsDocument51 pagesDevelopment of Cartilage, Bone and JointsJetGoliath 26No ratings yet
- Embriology Muskuloskeletal: DR - Elli Kusmayati, Sp.ADocument20 pagesEmbriology Muskuloskeletal: DR - Elli Kusmayati, Sp.Ariyadhi_pascaNo ratings yet
- Bone and CartilageDocument56 pagesBone and CartilageGodwin ZengeniNo ratings yet
- LP 7 Connective Tissue BoneDocument3 pagesLP 7 Connective Tissue BoneAndrei TimofteNo ratings yet
- Practical Work No. 7: Faculty of MedicineDocument3 pagesPractical Work No. 7: Faculty of MedicineAndrei TimofteNo ratings yet
- Bone FormationDocument9 pagesBone FormationKamalakannanNo ratings yet
- Concept Map of Bone Formation, Growth, and RemodellingDocument1 pageConcept Map of Bone Formation, Growth, and RemodellingSylvanus Rein LangreoNo ratings yet
- Bone Growth and Factors That Associated With It1234Document7 pagesBone Growth and Factors That Associated With It1234Amanuel TarekegnNo ratings yet
- Fisiologi Sistem Skeletal NFDocument25 pagesFisiologi Sistem Skeletal NFIka NoviaNo ratings yet
- 1 Bone Tissue 2021-22Document35 pages1 Bone Tissue 2021-22Ali AfifNo ratings yet
- Reviewer Zoo LecDocument27 pagesReviewer Zoo LecayeyedumpNo ratings yet
- Oral Manifestations of Connective Tissue Disease (CTDDocument34 pagesOral Manifestations of Connective Tissue Disease (CTDFatin Nabihah Jamil67% (3)
- BismillahDocument1 pageBismillahFatin Nabihah JamilNo ratings yet
- BismillahDocument1 pageBismillahFatin Nabihah JamilNo ratings yet
- Don'T Say Goodbye - TVXQ/DBSKDocument1 pageDon'T Say Goodbye - TVXQ/DBSKFatin Nabihah JamilNo ratings yet
- PHYSICS Newton's Second Law ExperimentDocument21 pagesPHYSICS Newton's Second Law ExperimentFatin Nabihah Jamil100% (1)
- QuotesDocument1 pageQuotesFatin Nabihah JamilNo ratings yet
- CartilagoDocument40 pagesCartilagoIlham DwiNo ratings yet
- Connective TissueDocument7 pagesConnective TissueRoy Michael Trinidad0% (1)
- Chapter 7 (Cartilage)Document5 pagesChapter 7 (Cartilage)Jovilyn SilongaNo ratings yet
- Connective TissuesDocument11 pagesConnective TissuesCamille Ann Faigao FamisanNo ratings yet
- Symphytum Off VermDocument7 pagesSymphytum Off Vermvedha mungaraNo ratings yet
- Worksheet-5 Musculoskeletal-System Group3 BFFDocument79 pagesWorksheet-5 Musculoskeletal-System Group3 BFFAldrin LimcuandoNo ratings yet
- 4-Cartilage MCQ Asnan Ainshams DR - Zahra 2020Document6 pages4-Cartilage MCQ Asnan Ainshams DR - Zahra 2020Shay Os100% (2)
- DMS2 K3 (Kelas A) LECTURE CARTILAGE&BONE2020 PDFDocument67 pagesDMS2 K3 (Kelas A) LECTURE CARTILAGE&BONE2020 PDFdiqa aridaniNo ratings yet
- Connective Tissue IDocument8 pagesConnective Tissue IElena ArvanitiNo ratings yet
- CartilageDocument8 pagesCartilageT.c. Muhammed YükselNo ratings yet
- Veterinary Embryology (Class Notes) PDFDocument77 pagesVeterinary Embryology (Class Notes) PDFluis feo0% (3)
- Histo 1st ShiftDocument25 pagesHisto 1st ShiftIvy CruzNo ratings yet
- Histology of The Cartilage (Week 7)Document8 pagesHistology of The Cartilage (Week 7)Robaina WisNo ratings yet
- Pi Is 0002941669901742Document4 pagesPi Is 0002941669901742Gabriela LouNo ratings yet
- Embryology BoneDocument6 pagesEmbryology BoneMarera DomnicNo ratings yet
- Joint Preservation of The Knee: A Clinical CasebookDocument328 pagesJoint Preservation of The Knee: A Clinical Casebookosmann52No ratings yet
- Essential of Facial GrowthDocument18 pagesEssential of Facial GrowthTiwi SitompulNo ratings yet
- St. Luke's College of Medicine - William H. Quasha Memorial: AnatomyDocument6 pagesSt. Luke's College of Medicine - William H. Quasha Memorial: AnatomyMavic VillanuevaNo ratings yet
- AJODO-90 Petrovic Et Al Role of The Lateral Pterigoid Muscle and Menisco Temporomandibular...Document12 pagesAJODO-90 Petrovic Et Al Role of The Lateral Pterigoid Muscle and Menisco Temporomandibular...ortodoncia 2018No ratings yet
- Veterinary Anatomy and EmbryologyDocument77 pagesVeterinary Anatomy and EmbryologyFor AstroNo ratings yet
- (Supportive Tissue) - (DVM 1st Semester) - (Morning) - (A Section)Document10 pages(Supportive Tissue) - (DVM 1st Semester) - (Morning) - (A Section)hely shahNo ratings yet
- Cartilage: Histology Dr. BernalDocument4 pagesCartilage: Histology Dr. BernalA18- Jessa Mae DayagNo ratings yet
- Vet Histo Notes Chap 3Document15 pagesVet Histo Notes Chap 3Mia Kristhyn Calinawagan SabanalNo ratings yet
- Anatomy and Physiology: Bone Histology Lecture OutlineDocument42 pagesAnatomy and Physiology: Bone Histology Lecture OutlineFokeerbux ZyadNo ratings yet
- Condylar CartilageDocument11 pagesCondylar CartilageMahesh kumarNo ratings yet
- Histo Trans 1.4 - Cartilage and BoneDocument6 pagesHisto Trans 1.4 - Cartilage and BonePim AramNo ratings yet
- lab6انسجة مترجمةDocument12 pageslab6انسجة مترجمةAzofNo ratings yet
- Histology-World! Histology Testbank-Cartilage 2aDocument7 pagesHistology-World! Histology Testbank-Cartilage 2aAya AhmedNo ratings yet
- Chapter 7 - CartilageDocument17 pagesChapter 7 - CartilageREMAN ALINGASANo ratings yet
- Bone Development and GrowthDocument21 pagesBone Development and GrowthRania ThiniNo ratings yet