Professional Documents
Culture Documents
Investigative Hepatology
Uploaded by
Mahmoud Ahmed MahmoudOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Investigative Hepatology
Uploaded by
Mahmoud Ahmed MahmoudCopyright:
Available Formats
Biochemical Tests
Investigations for Liver Diseases
Adequate evaluation of an infant, child or adolescent with suspected liver disease involves an appropriate and accurate history, a carefully performed physical examination and skillful interpretation of signs and symptoms. Further evaluation is aided by judicious selection of diagnostic tests followed by the use of imaging modalities or a liver biopsy.
BIOCHEMICAL TESTS
Indication:
Estimation of synthetic and excretory functions: Where there is increase in serum bilirubin (total and fractionated), prolongation of prothrombin time (PT) or international normalized ratio (INR) and decrease in albumin level. Detection of Hepatocellular Damage: Acute liver cell injury (parenchymal disease) in viral hepatitis, drug- or toxin-induced liver disease, shock, hypoxemia or metabolic disease is best reflected by marked increases in serum aminotransferase levels. Detection of biliary Disease: Cholestasis (obstructive disease) involves regurgitation of bile components into serum so the serum levels of total and conjugated bilirubin and serum bile acids are elevated. Also elevations in serum AP, 5 nucleotidase (5NT), and -glutamyl transpeptidase (GGT) levels are sensitive indicators of obstruction or inflammation of the biliary tract. Determination of the type of jaundice: Fractionation of the total serum bilirubin level into conjugated and unconjugated bilirubin fractions helps to distinguish between elevations caused by hemolysis and those caused by hepatic dysfunction. Detection of certain diseases: Patients with autoimmune hepatitis often have high gamma-globulin levels and increased titers of anti-smooth muscle, antinuclear and anti-liver-kidney-microsome antibodies. Resurgence in -fetoprotein levels may suggest hepatoma, hepatoblastoma, or hereditary tyrosinemia.
Investigations for Liver Diseases
Biochemical Tests
Interpretation:
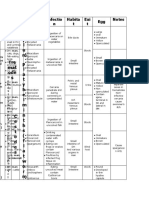
Interpretation of results of biochemical tests of hepatic structure and function must be made in the context of age-related changes. Aminotransferases (ALT: 7-56 IU/L & AST: 5-47 IU/L): Alanine aminotransferase (ALT) is liver specific, whereas aspartate aminotransferase (AST) is derived from other organs in addition to the liver. o The most marked rises of both AST and ALT levels may occur with acute hepatocellular injury. o In acute hepatitis, the rise in ALT may be greater than the rise in AST. o In chronic liver disease or in intrahepatic and extrahepatic biliary obstruction, AST and ALT elevations may be less marked. Alkaline phosphatase (30-120 IU/L): Normal growing children have significant elevations of serum AP activity originating from influx into serum of the isoenzyme that originates in bone. Therefore, an isolated increase in AP does not indicate hepatic or biliary diseases if other liver function test results are normal. Albumin (3.5-5.3 g/dL): Albumin is a protein made specifically by the liver that can be measured cheaply and easily. It is the main constituent of plasma protein. Albumin levels are decreased in chronic liver disease such as cirrhosis. Coagulation tests (PT: 10-14 sec & INR: 0.8-1.2): The liver is responsible for the production of coagulation factors. The INR will be increased only if the liver is so damaged that synthesis of vitamin K-dependent coagulation factors has been impaired. Increased levels of INR means that blood is taking more time than usual to coagulate or clot. It is very important to normalize the INR before operating on people with liver problems (usually by transfusion with blood plasma containing the deficient factors) as they could bleed excessively. 5 nucleotidase and -glutamyl transpeptidase (0-42 IU/L): 5NT and GGT are increased in cholestatic conditions and may be more specific for hepatobiliary disease. Cholesterol (<200 mg/dL): Cholesterol levels may be markedly elevated in patients with intra or extrahepatic cholestasis and decreased in severe acute liver disease such as hepatitis. Serum glucose (82-110 mg/dL): Gluconeogenesis is usually the last function to be lost in the setting of fulminant liver failure. Investigations for Liver Diseases
Biochemical Tests Bilirubin (Total: 0.2-1.2 mg/dL & Direct: 0.1-0.4 mg/dL): Bilirubin is a breakdown product of heme. Bilirubin is taken up into hepatocytes, conjugated with glucuronic acid then secreted into the bile to the intestine. Increased total bilirubin (TBIL) causes jaundice, and can signal a number of problems: o Pre-hepatic: Increased bilirubin production as in hemolytic anemias and internal hemorrhage. o Hepatic: Problems with the liver, which are reflected as deficiencies in bilirubin metabolism (e.g., reduced hepatocyte uptake, impaired conjugation of bilirubin, and reduced hepatocyte secretion of bilirubin) as in cirrhosis and viral hepatitis. o Post-hepatic: Obstruction of the bile ducts either within the liver or in the bile duct. The diagnosis is narrowed down by looking at the levels of direct & indirect bilirubin: o If indirect is elevated: Hemolysis, viral hepatitis or cirrhosis can be suspected. o If direct bilirubin is elevated: Bile duct obstruction by gallstones or cancer should be suspected.
URINE TEST:
Dipstick tests are available for bilirubin and urobilinogen in the urine. Bilirubinuria is due to the presence of conjugated bilirubin. It is found in the jaundiced patient with hepatobiliary disease; its absence implies that the jaundice is due to increased unconjugated bilirubin. Urobilinogen in the urine is, in practice, of little value but suggests hemolysis or hepatic dysfunction of any cause.
Investigations for Liver Diseases
Imaging Procedures
IMAGING PROCEDURES
Various techniques help define the size, shape, architecture of the liver and the anatomy of the intrahepatic and extrahepatic biliary trees.
Ultrasonography (US):
o Ultrasonography provides information about the size, composition and blood flow of the liver. o Increased echogenicity is observed with fatty infiltration; mass lesions as small as 12 cm may be shown. o US can assess gallbladder size, detect dilatation of the biliary tract and define a choledochal cyst even in neonates o In infants with biliary atresia, US findings may include small or absent gallbladder, nonvisualization of the common duct and presence of the triangular cord sign, a triangular/tubular-shaped echogenic density in the bifurcation of the portal vein, representing fibrous remnants at the porta hepatis. o In patients with portal hypertension, Doppler US can evaluate patency of the portal vein, demonstrate collateral circulation and assess size of spleen and amount of ascites. Relatively small amounts of ascitic fluid can also be detected. o The use of Doppler US has been helpful in determining vascular patency after liver transplantation.
Computerized Tomography (CT) & Magnetic Resonance Imaging (MRI):
o CT scan or MRI is more accurate than US in detecting focal lesions such as tumors, cysts and abscesses. o When enhanced by contrast medium, CT scanning may reveal a neoplastic mass density only slightly different from that of a normal liver. o When a hepatic tumor is suspected, CT scanning is the best method to define anatomic extent, solid or cystic nature and vascularity. o In differentiating obstructive from non-obstructive cholestasis, CT scanning or MRI identifies the precise level of obstruction more frequently than US.
Angiographic Studies:
Selective angiography of the celiac, superior mesenteric or hepatic artery can be used to visualize the hepatic or portal circulation. Both arterial and venous circulatory systems of the liver can be examined. Angiography is frequently required to define the blood supply of tumors before surgery and is useful in the study of patients with known or presumed portal hypertension where the patency of the portal system, the extent of collateral circulation and the caliber of vessels under consideration for a shunting procedure can be evaluated.
Investigations for Liver Diseases
Imaging Procedures
Cholangiography:
Cholangiography, direct visualization of the intrahepatic and extrahepatic biliary tree after injection of opaque material, may be required in some patients to evaluate the cause, location or extent of biliary obstruction.
Endoscopic Retrograde Cholangiopancreatography (ERCP):
ERCP is an alternative method of examining the bile ducts in older children. The papilla of Vater is cannulated under direct vision through a fiberoptic endoscope, and contrast material is injected into the biliary and pancreatic ducts to outline the anatomy.
Magnetic Resonance Cholangiopancreatography (MRCP):
This technique involves the manipulation of a volume of data acquired by MRI. A heavily T2-weighted sequence enhances visualization of the water-filled bile ducts and pancreatic ducts to produce high-quality images of ductal anatomy. This non-invasive technique is replacing diagnostic ERCP.
Radionuclide Scanning:
Radionuclide scanning relies on selective uptake of a radiopharmaceutical agent as technetium 99m-labeled sulfur colloid and gallium 67. The 99mTc-sulfur colloid scan can detect focal lesions (tumors, cysts, abscesses) >23 cm in diameter. This modality can help to evaluate patients with possible cirrhosis and with patchy hepatic uptake and a shift of colloid uptake from liver to bone marrow. The 99mTc-substituted iminodiacetic acid dyes may differentiate intrahepatic cholestasis from extrahepatic obstruction in neonates. Imaging results are best when scanning is preceded by a 57 day period of treatment with phenobarbital to stimulate bile flow. After intravenous injection, the isotope is normally detected in the bowel within 12 hr. In the presence of extrahepatic obstruction, excretion of the isotope is delayed; accordingly, serial scans should be made for up to 24 hour after injection. Early in the course of biliary atresia, hepatocyte function is usually good; uptake (clearance) occurs rapidly, but excretion into the intestine is absent. In contrast, uptake is poor in parenchymal liver disease, such as neonatal hepatitis, but excretion into the bile and intestine eventually ensues.
Investigations for Liver Diseases
Liver Biopsy
LIVER BIOPSY
Liver biopsy combined with clinical data can suggest a cause in most cases.
Indications:
Specimens of liver tissue can be used: to provide a precise histologic diagnosis in: o o o o o o o o o o o Neonatal cholestasis. Chronic active hepatitis. Metabolic liver disease. Suspected Reye syndrome. Intrahepatic cholestasis. Congenital hepatic fibrosis. Undefined portal hypertension. Enzyme analysis to detect inborn errors of metabolism. Analysis of stored material such as iron, copper, or specific metabolites. Monitoring responses to therapy. Detection of complications of treatment with potentially hepatotoxic agents.
Approaches:
Percutaneous approach: It can be performed safely in infants as young as 1 week of age. Patients usually require only conscious sedation and local anesthesia. Open laparotomy (wedge) approach: It is done by a general surgeon. Transjugular approach: Transjugular approach is done under ultrasound and fluoroscopic guidance.
REFERENCES:
o Nelson Textbook of Pediatrics, 19th Edition. o Kumar & Clark's Clinical Medicine, 7th Edition.
BY
Dr. Mahmoud Ahmed Mahmoud Alexandria University of medicine
Investigations for Liver Diseases
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Oscar Wilde - The Importance of Being EarnestDocument79 pagesOscar Wilde - The Importance of Being EarnestIvo Pires Das Neves100% (2)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Peripheral Vascular DiseaseDocument53 pagesPeripheral Vascular DiseaseShenbagam Mahalingam100% (1)
- PATHOLOGY Board Exam ANsWERSDocument22 pagesPATHOLOGY Board Exam ANsWERSchristinejoan100% (1)
- CAPE Biology Unit 2 ProjectDocument13 pagesCAPE Biology Unit 2 ProjectAudi Sweetangel0% (1)
- Anti-Microbial Therapy Final With AlarmsDocument245 pagesAnti-Microbial Therapy Final With AlarmsMahmoud Ahmed MahmoudNo ratings yet
- A-Autonomic Drugs: 1) CholinergicDocument28 pagesA-Autonomic Drugs: 1) CholinergicMahmoud Ahmed MahmoudNo ratings yet
- "Usmle Cs2Document27 pages"Usmle Cs2Drbee10No ratings yet
- An Essay On Yoga and HealthDocument2 pagesAn Essay On Yoga and HealthGentleStrength100% (1)
- Health TipsDocument102 pagesHealth Tipsgurkirt100% (1)
- Insulin Adjustment Workbook CompleteDocument53 pagesInsulin Adjustment Workbook CompletetskumarphdNo ratings yet
- Acog Practice Bulletin Summary: Gestational Hypertension and PreeclampsiaDocument4 pagesAcog Practice Bulletin Summary: Gestational Hypertension and PreeclampsiaKevin CasavilcaNo ratings yet
- Leprominium A Glimpse With Comparative Study (Nosode of Leprosy)Document3 pagesLeprominium A Glimpse With Comparative Study (Nosode of Leprosy)Homoeopathic Pulse100% (3)
- Equine Colic Lecture 1Document135 pagesEquine Colic Lecture 1Victor TsigoNo ratings yet
- Ovarian Hyperstimulation SyndromeDocument3 pagesOvarian Hyperstimulation SyndromeMahmoud Ahmed MahmoudNo ratings yet
- Non-Ischemic Central Retinal Vein OcclusionDocument17 pagesNon-Ischemic Central Retinal Vein OcclusionMahmoud Ahmed MahmoudNo ratings yet
- Branch Retinal Vein Occlusion (BRVO)Document4 pagesBranch Retinal Vein Occlusion (BRVO)Mahmoud Ahmed MahmoudNo ratings yet
- Fetal MalnutritionDocument2 pagesFetal MalnutritionMahmoud Ahmed MahmoudNo ratings yet
- Livor MortisDocument16 pagesLivor MortisMahmoud Ahmed MahmoudNo ratings yet
- Fetal Malnutrition: DR. Mahmoud Ahmed Mahmoud Ahmed Faculty of Medicine Alexandria UniversityDocument11 pagesFetal Malnutrition: DR. Mahmoud Ahmed Mahmoud Ahmed Faculty of Medicine Alexandria UniversityMahmoud Ahmed MahmoudNo ratings yet
- Investigative HepatologyDocument24 pagesInvestigative HepatologyMahmoud Ahmed MahmoudNo ratings yet
- Non-Ischemic Central Retinal Vein OcclusionDocument6 pagesNon-Ischemic Central Retinal Vein OcclusionMahmoud Ahmed MahmoudNo ratings yet
- Livor MortisDocument5 pagesLivor MortisMahmoud Ahmed MahmoudNo ratings yet
- Management of AgitationDocument8 pagesManagement of AgitationMahmoud Ahmed MahmoudNo ratings yet
- Drug Management of AgitationDocument14 pagesDrug Management of AgitationMahmoud Ahmed MahmoudNo ratings yet
- Diphtheria VaccineDocument5 pagesDiphtheria VaccineMahmoud Ahmed MahmoudNo ratings yet
- Iphtheria Accine Oxoid: Mahmoud Ahmed Mahmoud 846Document23 pagesIphtheria Accine Oxoid: Mahmoud Ahmed Mahmoud 846Mahmoud Ahmed MahmoudNo ratings yet
- Endoscopic Surgery For Cancer LarynxDocument13 pagesEndoscopic Surgery For Cancer LarynxMahmoud Ahmed MahmoudNo ratings yet
- Endoscopic Surgery For Cancer LarynxDocument11 pagesEndoscopic Surgery For Cancer LarynxMahmoud Ahmed MahmoudNo ratings yet
- Phylum Platyhelminths (Flat Worms)Document2 pagesPhylum Platyhelminths (Flat Worms)Mahmoud Ahmed MahmoudNo ratings yet
- Top 8 Pain Herbs EbookDocument35 pagesTop 8 Pain Herbs EbookMari BuôgoNo ratings yet
- Sandra Shroff Rofel College of NursingDocument27 pagesSandra Shroff Rofel College of NursingMehzbeen NavsariwalaNo ratings yet
- "Virtopsy" Virtual Alternative For Post-Mortem Investigation in Pandemic Era of Covid-19: Diagnostic Approach To Reduce The Menace of Contagion: - A ReviewDocument6 pages"Virtopsy" Virtual Alternative For Post-Mortem Investigation in Pandemic Era of Covid-19: Diagnostic Approach To Reduce The Menace of Contagion: - A ReviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Owen 2012Document5 pagesOwen 2012bodocsdomiNo ratings yet
- Short Term Disability Overview 2020Document1 pageShort Term Disability Overview 2020tim cleavelandNo ratings yet
- Numbness: Tyas Mayangputri Hadiana - 10100118204Document7 pagesNumbness: Tyas Mayangputri Hadiana - 10100118204refimaya arlitaNo ratings yet
- #19 SY Vs CA Case DigestDocument1 page#19 SY Vs CA Case DigestJunna Rose PascoNo ratings yet
- Obesity: Sharmila A/P Rajendran E20141008930 Diploma Sains Dan MatematikDocument18 pagesObesity: Sharmila A/P Rajendran E20141008930 Diploma Sains Dan MatematikSharmila RajNo ratings yet
- UROLITHIASISDocument9 pagesUROLITHIASISmardsz100% (13)
- MCQ Anemia Antiplatelete MalariaDocument5 pagesMCQ Anemia Antiplatelete Malariasherif mamdoohNo ratings yet
- Glaucoma 2003Document24 pagesGlaucoma 2003Aryu-hanafiey BoyzzsNo ratings yet
- Alzheimers Disease,,syringoyeloma by VineethaDocument42 pagesAlzheimers Disease,,syringoyeloma by VineethaDR. KUMARASWAMI HEALTH CENTRE COLLEGE OF NURSING KANYAKUMARINo ratings yet
- Drug Study - CeftizidimeDocument2 pagesDrug Study - CeftizidimeRay Daniel E. BilbaoNo ratings yet
- GalemedicaljournalphobiasDocument4 pagesGalemedicaljournalphobiasapi-3954809780% (1)
- Delmar's Pediatric Nursing Care Plans, 3 Edition, Karla L. Luxner, RNC, ND, Pg. 67Document2 pagesDelmar's Pediatric Nursing Care Plans, 3 Edition, Karla L. Luxner, RNC, ND, Pg. 67KMNo ratings yet
- Journal Reading Ilmu Penyakit DalamDocument15 pagesJournal Reading Ilmu Penyakit DalamSeffia riandiniNo ratings yet
- Nursing Health History: Princess Jamela Camu Celline Isabelle ReyesDocument11 pagesNursing Health History: Princess Jamela Camu Celline Isabelle ReyesCelline Isabelle ReyesNo ratings yet
- Pharma PPT TodocDocument40 pagesPharma PPT TodocPrincess Jovelyn GutierrezNo ratings yet
- Certificado Medico PDFDocument2 pagesCertificado Medico PDFSaurav Ghosh RoyNo ratings yet