Professional Documents
Culture Documents
Nurse Practitioner Wound Management Clinical Protocols
Uploaded by
Brian HarrisOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nurse Practitioner Wound Management Clinical Protocols
Uploaded by
Brian HarrisCopyright:
Available Formats
Sir Charles Gairdner Hospital Nurse Practitioner Wound Management Clinical Protocols
Nurse Practitioner Clinical Protocols for Wound Management Services
Prepared by: Pam Morey, RN BN STN, MN(NP) MRCNA
March 2007 Sir Charles Gairdner Hospital North Metropolitan Health Service
Acknowledgement: L. MacLellan, G. Gardner, A. Gardner, Canberra Hospital T. Swanson, J.Smart, S.Morrison, South West Healthcare, Warnambool, Victoria M. Asimus, Hunter New England Health (the Maitland Hospital), New South Wales D. Angel, Royal Perth Hospital, Perth Western Australia Issued: Review: 2007 2009
Sir Charles Gairdner Hospital Nurse Practitioner Wound Management Clinical Protocols
Wound Diagnostics and Treatment
Clinical Protocol 1.
Introduction The following protocol (see Table 1) outlines the sequence of events in the assessment, investigation, diagnosis and management of a patient with a wound and forms the basis for the protocols which follow. This is further outlined in a flow chart (see Figure 1). Table 1. Assessment and Management of the Patient with a Wound PROCESS
HISTORY
ACTION
A complete history is taken
GUIDANCE
Medical, surgical, allergy history Wound history Current medications (prescribed and over the counter [OTC]) Previous diagnostic investigations Social and Occupational history including carer or home support Physical mobility Activities of daily living
EXAMINATION
Physical examination of the wound and associated area/limb More generalised assessment as necessary
Clinical features of the wound and skin Presence of other wounds/lesions Peripheral perfusion Peripheral neurological examination (eg using Semmes Weinstein 10g monofilament, tendon reflexes, vibration) Signs and symptoms of infection Footwear (diabetes, lower limb wounds)
Physical and joint mobility Explore differential diagnosis
-1-
Sir Charles Gairdner Hospital Nurse Practitioner Wound Management Clinical Protocols
PROCESS
INVESTIGATIONS
ACTION
Determine which investigations may be required to assist in a diagnosis or provide a baseline of nutrition and health
GUIDANCE
Pathology Haematology FBP, ESR, CRP, INR Biochemistry U & Es LFT, (Total Protein, Albumin), Pre-albumin Glucose, HbA1C Lipids Thyroid function Microbiology and Histology Wound fluid/swabs microscopy, culture and sensitivity (MC&S) Wound/tissue biopsy MCS and histopathology Skin Scraping, Immunofluorescence Biopsy This may be required if the wound has been non-healing, despite optimal treatment, for greater than 4 weeks; or the duration is greater than 6 months; and/or is assessed as atypical. Radiology / Medical Imaging Ankle Brachial Pressure Index (ABPI) Toe Doppler Pressures/Index Duplex Scan (Arterial & Venous) Photoplethysmography (PPG) X-Ray MRI
Referral for: Arterial Duplex Scan: To determine presence and/or severity or arterial disease in the lower limb Venous Duplex Scan: To determine disease or impairment of superficial, deep, and perforating veins and valves.
ABPI performed on all outpatient leg ulcer patients. If the ABPI does not complement the clinical assessment or is inconclusive then further diagnostic investigation may be required. Arterial/Venous Duplex Scan Non-invasive investigation is recommended for initial diagnosis X-Ray If there is a suspicion of osteomyelitis, sinus, fistula, significant undermining or foreign body, then an x-ray may be ordered. Bone Scan / MRI If there is a suspicion of osteomyelitis, then a Bone Scan or MRI may be ordered following consultation with an Infectious Diseases physician or Vascular Surgeon.
-2-
Sir Charles Gairdner Hospital Nurse Practitioner Wound Management Clinical Protocols
PROCESS
DIAGNOSIS
ACTION
Make provisional diagnosis
GUIDANCE
On clinical picture, available assessment data and results of investigations. Referrals If the wound fails to heal despite optimal therapy then consultation with other health care practitioners and further investigations may be required at that time.
MANAGEMENT
Urgent Referrals: Life/limb threatening infection Abnormal test results that require medical intervention Treatment required outside the NP scope of practice Acute DVT New patient with a ABI <0.7 or ankle systolic <80 mmHg Patient that requires surgical intervention Ulcers on the plantar aspect of the foot to have immediate Podiatry referral Significant deterioration in wound since last review Nurse Practitioner: Non-pharmacological treatment
Non-pharmacological treatment Appropriate dressings and/or compression bandages based on diagnosis and patient lifestyle preferences Cleansing and debridement of wound Patient /Carer education for self care Hygiene (cleansing self and waterproofing as required) Diet (the importance of essential vitamins and minerals as required). Indications to seek medical help Bandaging/dressing techniques Exercise regimes Lifestyle changes Disease process and health maintenance Prevention of recurrence Pain management Medication (Includes relevant consumer handouts) Pharmacological treatment Analgesics Topical antimicrobials/antifungals Local anaesthetics Topical corticosteroids Oral antibiotics Moisturisers Barrier ointments, creams and wipes Skin cleansers Lower leg ulcer Minor surgical procedures (further protocols to follow)
Patient education for self care
Pharmacological treatment - Based on diagnostic investigations, clinical assessment, and Therapeutic Guidelines
Refer to other Clinical Practice Guidelines
-3-
Sir Charles Gairdner Hospital Nurse Practitioner Wound Management Clinical Protocols
PROCESS
MANAGEMENT PARTNERSHIPS
ACTION
Appropriate referrals to assist in overall management
GUIDANCE
Other Health Professionals as required: Medical: Vascular Surgeon Plastic Surgeon Infectious Diseases Physician Dermatologist Endocrinologist Pain Management Palliative Care General Practitioner Allied Health: Dietitian Podiatrist Diabetic Educator Occupational Therapist Physiotherapist Pharmacist Community care providers: Silver Chain Nursing Other home care providers (eg Stanhope)
ONGOING MANAGEMENT
Follow-up
Review as appropriate: Test results Monitor progress Maintenance of wound Review treatment plan in accordance with investigative results As appropriate: Wound healing achieved Referral to community services for long term management Referral for Specialist care.
SEPARATION
Discharge from service
-4-
Sir Charles Gairdner Hospital Nurse Practitioner Wound Management Clinical Protocols
Figure 1.
Wound Diagnostics and Treatment: Flow Chart
Patient History Medical history/Co-morbidities Wound History Current medications Social and occupational history Activities of daily living
1.Assessment
Physical examination Clinical features of wound and skin Presence of other wounds/lesions Peripheral perfusion Neurological examination eg tendon reflexes and monofilament testing
!! Consider conditions for urgent referral e.g. Ischaemic limb/s Serious infection e.g. wet gangrene Diabetic foot infections
2. Diagnosis
Investigations as indicated Full blood examination Urea & Electrolytes Blood glucose levels and HBA1C, other haematology, biochemical tests Ankle Brachial Index/Doppler signal characteristics Toe Doppler index Duplex scan X-Ray Wound swab/s Wound biopsy
3a. Conditions for specialist referral Urgent conditions as indicated above Treatment outside of NP scope of practice e.g. ischaemia, severe infection
3b. Treatment options / Conditions for NP treatment All wound conditions outside urgent treatment Management as per specific protocols
Non-pharmalogical approaches Cleansing and debridement of wound Appropriate dressings/bandages Skin care and moisturisers Patient education for self care Hygiene Diet Exercise Dressing/bandaging regimes Disease process and health maintenance Medication
3c. Integrated management of comorbidities Includes diabetes, autoimmune disease, cardiac failure Endocrinologist Vascular surgeon Dermatolologist Infectious diseases physician Plastic surgeon Pain Management Palliative Care General Practitioner Diabetic Educator Dietitian Podiatrist/Orthotist Pharmacist Other health professionals as required 4. Follow-up Review as appropriate Test results Monitor progress Maintenance of healed wound
Pharmacological agents Antibiotics Antifungals Analgesics Topical agents (eg corticosteroids, antimicrobials)
Adapted from MacLellan, L., Gardner, G., Gardner, A (2002) Designing the future in wound care: The role of the nurse practitioner. Primary Intention 10(3): 97-112 ACT Government, reprinted with permission.
-5-
Sir Charles Gairdner Hospital Nurse Practitioner Wound Management Clinical Protocols
Minor Surgical Procedures
Clinical Protocol 2.
Introduction To provide appropriate management of wounds, there are occasions where either wound biopsy or sharp debridement procedures are required. Both of these are minor surgical procedures. The flow chart demonstrates the protocol (see Figure 2)
Biopsy Skin and wound biopsy are used for diagnosis and may identify the presence (or absence) or various skin conditions or diseases. In addition, biopsy may be performed for semi-quantitative bacteriology where surface swabs are inadequate. Wounds considered for biopsy may include long-standing wounds, those that are atypical in location or appearance, or those that have not responded to treatment (Trent, Federman, & Kirsner, 2003). Biopsy may be considered for lesions suspicious of malignancy where there is increase in size; malodour and pain; have excess granulation tissue, bleeding, or drainage; are exophytic; or have an irregular base or margin. The procedure involves prior assessment of the wound or lesion; preparation of the patient including explanation of the procedure; cleansing of the area, and anaesthetisation with local anaesthetic. There are various methods of biopsy and in this instance the preferred options are incisional or punch biopsy. Particular wound conditions that may be identified include squamous cell carcinoma, basal cell carcinoma, vasculitis, and calciphylaxis.
Debridement Debridement is the removal of devitalised (non-viable) tissue, particulate matter and foreign material (Fowler & van Risjwijk, 1995). Conservative sharp wound debridement (CSWD) is a procedure used to debride non-viable tissue from a wound down to non-bleeding tissue using sharp instruments (eg scalpel, scissors and forceps). Debridement may be undertaken to remove contaminated, dead and damaged tissue that may inhibit healing or contribute to infection in the wound . It may also be undertaken to prepare a wound for skin grafting, application of skin substitutes, or topical negative pressure therapy (e.g. VAC Vacuum Assisted Closure). Sharp debridement may be necessary in either acute wounds (eg skin tear with non-viable tissue), or chronic wounds (eg pressure ulcers), and the decision about this type of procedure being undertaken requires consideration of both local and systemic factors. These include but are not limited to knowledge of underlying -6-
Sir Charles Gairdner Hospital Nurse Practitioner Wound Management Clinical Protocols
anatomical structures, local tissue perfusion, the presence of impaired clotting or the use of anticoagulant medication, and the presence of malignancy (Carville, 2005).
The outline of assessment process, investigations and management are outlined in Table 2.
Table 2 Assessment and Management: Minor Surgical Procedures. PROCESS
HISTORY
ACTION
A complete history is taken
GUIDANCE
Medical, surgical, allergy history/comorbidities Wound history Current medications (prescribed and OTC) Previous diagnostic investigations Social and Occupational history including carer or home support Physical mobility Activities of daily living
EXAMINATION
Physical examination of the wound and associated area/limb More generalised assessment as necessary
Findings from assessment of complex, infected wounds, leg ulcers, and diabetic foot ulcers Abnormal clinical presentation: Raised/unusual clinical features Suspicion of neoplastic disease Senescent tissue Hypergranulation tissue Non healing despite optimal treatment
Presence of: Infection not responding to antibiotic treatment Contaminated/non-viable material Foreign bodies
-7-
Sir Charles Gairdner Hospital Nurse Practitioner Wound Management Clinical Protocols
PROCESS
INVESTIGATIONS
ACTION
Biopsy of wound for histology and/or microbiology Histology
GUIDANCE
To confirm wound aetiology Microbiology To identify organisms (semiquantitative) and sensitivities
DIAGNOSIS
Make provisional diagnosis
On clinical picture, available assessment data and results of investigations. Notify medical practitioners of investigations ordered and referrals organised If the wound fails to heal despite optimal therapy then consultation with other health care practitioners and further investigations may be required at that time. Non-pharmacological treatment Appropriate dressings/bandaging based on diagnosis and patient lifestyle preferences Cleansing and debridement of wound Patient / Carer education for self care Hygiene (cleansing self and wound waterproofing as required) Diet (the importance of essential vitamins and minerals as required). Signs and symptoms of complications Bandaging/dressing techniques Exercise regimes Lifestyle changes Disease process and health maintenance Prevention of recurrence Pain management Medication (Includes relevant consumer handouts)
MANAGEMENT
Urgent Referrals: Life/limb threatening infection Abnormal test results that require medical intervention Treatment required outside the NP scope of practice Significant deterioration in wound since last review Nurse Practitioner: Non-pharmacological treatment
Patient education for self care
Pharmacological treatment - Based on diagnostic investigations, clinical assessment, and Therapeutic Guidelines
Pharmacological treatment Analgesics Topical antimicrobials/antifungals Local anaesthetics Topical corticosteroids Oral antibiotics Conservative Sharp Surgical Debridement To remove: Contaminated material Foreign bodies
Conservative Sharp Surgical Debridement
-8-
Sir Charles Gairdner Hospital Nurse Practitioner Wound Management Clinical Protocols Non-viable tissue To prepare the wound environment for: Topical Negative Pressure Therapy (VAC) Skin grafts Substitutes to accelerate the healing process
MANAGEMENT PARTNERSHIPS
Appropriate referrals to assist in overall management
Other Health Professionals as required: Medical: General Practitioner Plastic Surgeon Dermatologist Infectious Diseases Physician Consultation with the medical practitioner if required for further treatment and investigation. Allied Health: Dietitian Podiatrist Diabetic Educator Occupational Therapist Physiotherapist Pharmacist Community care providers: Silver Chain Nursing Other home care providers
ONGOING MANAGEMENT
Follow-up
Review as appropriate: Test results Monitor progress Maintenance of wound Review treatment plan in accordance with investigative results As appropriate: Wound healing achieved Referral to community services for long term management Referral for Specialist care.
SEPARATION
Discharge from service
-9-
Sir Charles Gairdner Hospital Nurse Practitioner Wound Management Clinical Protocols
Figure 2.
Minor Surgical Procedures for Diagnosis and Treatment in Wound Care. Contraindications e.g. severe ischaemia (refer to specialist)
1. Findings from assessment of: Complex wounds Lower leg ulcers Infected wounds Diabetic foot wounds
1a. Abnormal clinical presentations e.g. Raised/unusual features e.g. irregular raised edges, purpura, vasculitic nodules Suspicion of neoplastic disease Senescent tissue Hypergranulation tissue Non healing despite optimal treatment
1b. Presence of infection not responding to antibiotic treatment
1c. Presence of: Contaminated dead material e.g. slough or necrotic tissue Foreign bodies e.g. sutures
Pharmacological agents Analgesics paracetamol, codeine, tramadol Local anaesthetics Lignocaine/Prilocaine, lignocaine hydrochloride
2a. Biopsy of wound Histological examination to confirm wound aetiology
2b. Biopsy of wound Microbiological examination to identify organisms and sensitivities treatment
2c. Sharp surgical debridement/curette to: Remove: - Contaminated material - Foreign bodies e.g. sutures - Non-viable tissue Prepare for grafting of skin or skin substitutes; Prepare for application of topical negative pressure therapy (VAC) Accelerate healing process
3a. Conditions for specialist referral Biopsy results indicates Neoplastic disease refer to Plastic surgeon/Dermatologist/Vascular surgeon as appropriate Biopsy findings inconclusive or suggestive of vasculitis or other dermatological conditions beyond the scope of practice of the NP refer to Dermatologist/Vascular surgeon as appropriate
3b. Conditions for specialist referral Biopsy results indicate Infection refer to Infectious Diseases physician
4. Follow up Review as appropriate Test results Monitor progress Maintenance of healed wound
Adapted from MacLellan, L., Gardner, G., Gardner, A (2002) Designing the future in wound care: The role of the nurse practitioner. Primary Intention 10(3): 97-112 ACT Government, reprinted with permission. 10 -
Sir Charles Gairdner Hospital Nurse Practitioner Wound Management Clinical Protocols
Lower Leg Ulcers (Vascular)
Clinical Protocol 3
Introduction This protocol has been designed to guide and facilitate the Nurse Practitioner (NP) in diagnosing and providing appropriate care of clients with leg ulcers.
Assessment A thorough assessment of the individual will follow as per the Protocol 1., Wound Diagnostics and Management. The following information outlines in more detail the specific process for the NP in managing patients with lower leg ulcers (see Table 3) using evidence gradings outlined on page 32-33. A flow chart outlining the Lower Leg Ulcer Clinical Protocol is shown in Figure 3, and the Guidelines for Compression Bandaging are represented in Figure 4. An explanation of compression bandaging components is outlined in Appendix 1.
- 11 -
Sir Charles Gairdner Hospital Nurse Practitioner Wound Management Clinical Protocols
Table 3 Assessment and Management of Lower Leg Ulcers. PROCESS ACTION
LEVEL OF EVIDENCE GUIDANCE
C
HISTORY
A complete history is taken: medical, surgical, allergy history Wound history Current medications (prescribed and OTC) Previous diagnostic investigations Social and Occupational history including carer or home support Physical mobility Activities of daily living Assess history of ulcers, duration of current ulcer, mechanism of injury and previous methods of treatment Assess for venous insufficiency: Family history of venous disease; Patient history of DVT; Lower leg fracture or other major leg injury; Previous vein surgery; Prior history of ulceration - with or without compression bandaging.
Assess for arterial insufficiency: History of intermittent claudication or rest pain Hypertension. Heart disease; Diabetes, Ischaemic stroke Smoking (or stopped < 5 years),
B In the presence of mixed disease (arterial + venous), patients may present with both. Assess for diabetes, rheumatoid arthritis and systemic vasculitis (Specialist assessment/referral should be considered). C Assess for correctable factors that may delay healing, including smoking, anaemia, and evidence of malnutrition or poor nutrition.
Assess for pain and formulate plans that involve exercise (including ankle exercises) and leg elevation for venous ulcers and adequate analgesia irrespective of aetiology.
- 12 -
Sir Charles Gairdner Hospital Nurse Practitioner Wound Management Clinical Protocols
PROCESS
EXAMINATION
ACTION
Physical examination of the wound and associated area/limb Conduct lower limb examination of both legs Eg the presence varicose veins in venous disease Examine for signs of arterial insufficiency: Lower skin temperature, auscultation of femoral bruit and pulses (weak or absent). Unilateral signs may be present where there is acute deterioration. Assess for malignancy can be a cause and may be a sequel of leg ulceration. Signs suggestive of malignancy are: irregular nodular appearance of the surface of the ulcer, raised or rolled edge, raised granulation tissue above the ulcer base, failure to respond to treatment, rapid increase in ulcer size and abnormal pigmentation.. Assess the wound and surrounding tissue: The surface area of ulcers should be measured at regular intervals to monitor progress Venous ulcers are generally shallow, moist and appear on the gaiter area of the leg; eczema, haemosiderin pigmentation, ankle oedema and ankle flare are often present; varicose veins, atrophie blanche & lipodermatosclerosis may be present. Arterial ulcers have a punched out appearance, a poorly perfused base and are pale and dry; surrounding skin is shiny and taut; dependent rubor present. A B
EVIDENCE / GUIDANCE
Lower limb pulses palpable pulses alone are insufficient to rule out arterial disease More generalised assessment as necessary Clinical features of the wound and skin Presence of other wounds/lesions Peripheral perfusion Neurological examination (eg using Semmes Weinstein 10g monofilament) Signs and symptoms of infection Footwear (diabetes, lower limb wounds) Physical and joint mobility Explore differential diagnosis
- 13 -
Sir Charles Gairdner Hospital Nurse Practitioner Wound Management Clinical Protocols
PROCESS
INVESTIGATIONS
ACTION
ABPI performed on all outpatient leg ulcer patients. If the ABPI does not complement the clinical assessment or is inconclusive then further diagnostic investigation may be required. Measurement of ABPI by handheld Doppler
EVIDENCE / GUIDANCE
Ankle Brachial Pressure Index (ABPI). Normal 0.9
1.2. A ratio of < 0.8 indicates the presence of peripheral arterial disease (PAD). Further tests should be considered prior to initiating compression bandaging if a patient has an ABPI >0.8 in the presence of signs and symptoms of PAD, rheumatoid arthritis, systemic vasculitis or diabetes mellitus. Doppler determination of ABPI should not be used in isolation from clinical assessment. Repeat measurement of ABPI when an ulcer deteriorates; is not fully healed by 3/12; or when patient presents with recurrence (of whichever leg) Toe Doppler Pressures/Index and arterial Photophlethysmography (PPG) are adjunct tests to ascertain arterial insufficiency particularly where diabetes, incompressible vessels or calcification are present. Venous PPG will provide information on venous refilling time as an assessment of venous insufficiency
B A
A B
Determine which investigations may be required to assist in a diagnosis or provide a baseline of nutrition and health Pathology Haematology FBP, CRP
Biochemistry U & Es LFT, Total Protein, Albumin, Glucose, HbA1C Lipids Thyroid function Microbiology and Histology Wound fluid/swabs - microscopy, culture and sensitivity (MC&S) Wound/tissue biopsy MCS and histopathology Skin Scraping, Immunofluorescence Note: Routine bacteriological swabs are unnecessary unless there is evidence of clinical infection Biopsy This may be required if the wound has been non-healing for 4 6 weeks with optimal treatment; is assessed as atypical, or has been present greater than 6 months. B
- 14 -
Sir Charles Gairdner Hospital Nurse Practitioner Wound Management Clinical Protocols Radiology / Medical Imaging Duplex Scan (Arterial & Venous) X-Ray Arterial/Venous Duplex Scan Non-invasive investigation is recommended for initial diagnosis Arterial Duplex Scan: To determine presence and/or severity or arterial disease in the lower limb Venous Duplex Scan: To determine disease or impairment of superficial, deep, and perforating veins and valves X-Ray If there is a suspicion of osteomyelitis, sinus, significant undermining or foreign body, then an x-ray may be ordered. DIAGNOSIS Make provisional diagnosis On clinical picture, available assessment data and results of investigations
- 15 -
Sir Charles Gairdner Hospital Nurse Practitioner Wound Management Clinical Protocols
PROCESS
MANAGEMENT
ACTION
Urgent Referrals: Life/limb threatening infection Abnormal test results that require medical intervention Treatment required outside the NP scope of practice DVT New patient with a ABI <0.7 or ankle systolic <80 mmHg Patient that requires surgical intervention Ulcers on the plantar aspect of the foot or other areas of the foot subject to pressure from weight-bearing or footwear, to have immediate Podiatry referral Significant deterioration in wound since last review Nurse Practitioner: Non-pharmacological treatment Compression bandaging should be applied when venous insufficiency is present, and should be based on the ABI and interpretation of clinical signs and additional investigative data. (Figure 2.) Compression bandaging (elastic and inelastic) has been demonstrated to be effective in the healing of venous leg ulcers. Reduced compression may be effective in selected patients with mixed disease (venous + arterial components) where the ABI is 0.6 -0.8 however these patient should be closely monitored for signs of reduced circulation/ischaemia in a specialised clinic. Dressing techniques should be clean and aimed at preventing cross-infection strict asepsis is not necessary. Ulcers can be cleansed with either potable water or sterile saline. Ulcerated legs can be washed normally in potable water. Wound debridement may be undertaken where necrotic tissue is present. There is no evidence to favour any one method of debridement, whether mechanical, surgical, biosurgical, autolytic, chemical or enzymatic and choice would be based on patient assessment (Also see Minor procedures protocol).
EVIDENCE / GUIDANCE
Referrals If the wound fails to heal despite optimal therapy then consultation with other health care practitioners and further investigations may be required at that time.
Patient / Carer education for self care Hygiene (cleansing self and waterproofing as required) Diet (the importance of essential vitamins and minerals as required, in particular Vitamin C and Zinc). Signs and symptoms of complications Bandaging/dressing techniques Exercise regimes Exercise programmes can improve calf muscle function, walking distances and pain for people with intermittent claudication Lifestyle changes Disease process and health maintenance
- 16 -
Sir Charles Gairdner Hospital Nurse Practitioner Wound Management Clinical Protocols Prevention of recurrence Pain management Medication (Includes relevant consumer handouts)
Pharmacological treatment - Based on diagnostic investigations, clinical assessment, and Therapeutic Guidelines Pharmacological treatment Analgesics Oral antibiotics Topical antimicrobials Topical anti-fungals Topical corticosteroids Local anaesthetics Moisturisers Barrier ointments, creams and wipes Skin cleansers Note: Patients can be sensitised to treatments at any time. Products which commonly cause sensitivity such as those containing lanolin, cetyl alcohol or topical antibiotics, are best avoided. B
Associated Clinical Practice Guidelines: Wound management and diagnostics Minor surgical procedures Diabetic foot ulcer* Infected wound* Complex Wound* *undergoing formulation.
- 17 -
Sir Charles Gairdner Hospital Nurse Practitioner Wound Management Clinical Protocols MANAGEMENT PARTNERSHIPS Appropriate referrals to, or liaison with other health professionals to assist in overall management Medical: Vascular Surgeon Plastic Surgeon Infectious Diseases Physician Endocrinologist Pain Management General Practitioner Dermatologist Note: Patients with dermatitis that does not resolve following removal of common sensitisers and treatment with a moderate topical steroid should be considered for referral to a Dermatologist. Venous surgery followed by graduated compression is an option for consideration in patients with superficial venous insufficiency. Allied Health: Dietitian Podiatrist Diabetic Educator Occupational Therapist Physiotherapist Pharmacist Community care providers: Silver Chain Nursing Homelink / Hospital in the Home Residential care agencies Other home care providers ONGOING MANAGEMENT Review as appropriate**: Test results Monitor progress Maintenance of wound Prophylactic review (eg 6/12 review for patient with healed venous ulcers prescription of graduated compression stockings) ** Patient reviews will be determined according to a number of factors. This will include whether or not the client is new to the service, whether compression therapy is initiated, their access to transport and availability for appointments; partnerships in care in place, and patient and wound factors. For a patient commencing compression therapy for the first time, review is usually within 1-2 weeks. Ongoing review may vary from 4 12 weeks. In the case of the patient with a healed venous ulcer who is wearing maintenance compression therapy, reviews are usually 6 monthly. As with all patient related visits, findings of the review and treatment plans will be documented in the patients integrated medical record. C
Review treatment plan in accordance with response to treatment and investigative results.
- 18 -
Sir Charles Gairdner Hospital Nurse Practitioner Wound Management Clinical Protocols SEPARATION Discharge from service As appropriate: Wound healing achieved Referral to community services for long term management Referral for Specialist care.
- 19 -
Sir Charles Gairdner Hospital Nurse Practitioner Wound Management Clinical Protocols
Figure 3.
Flow Chart - Lower Leg Ulcer Clinical Protocol
Patient History Medical history/Co-morbidities Wound History Current medications Social and occupational history Activities of daily living
1.Assessment
Physical examination General health assessment Clinical features of wound and skin Presence of other wounds/lesions Examination of peripheral pulses Signs of autoimmune disease eg Rh Arthritis, SLE Neurological examination Signs of presence of infection eg lymphangitis,, lymphadenopathy Exclude neoplastic disease 2. Diagnosis
!! Consider conditions for urgent referral e.g. Ischaemic limb/s Serious infection Diabetic foot infection
Differential diagnosis Venous Mixed Arterial Vasculitic, Neuropathic, Infective, Neoplastic, Other
Investigations as indicated ABPI/Doppler signal characteristics/Toe pressures Duplex scan Photoplethysmography (PPG) Full blood examination Blood glucose levels, HBA1C, other haematology, biochemical tests Wound swab Wound biopsy (see Minor surgical procedures protocol)
3a. Conditions for specialist referral Urgent conditions as indicated above Treatment outside of NP scope of practice e.g. cellulitis, surgical intervention required ABPI < 0.7
3b. Treatment options / Conditions for NP treatment All wounds outside urgent treatment
Non-pharmalogical approaches Appropriate dressings and graduated compression therapy Refer to Figure 2 Debridement (see Minor surgical procedures protocol)
3c. Integrated management of comorbidities Includes diabetes, autoimmune disease, cardiac failure Medical: General Practitioner Vascular surgeon Dermatologist Infectious diseases physician Plastic surgeon Pain Management Endocrinologist Allied Health: Dietitian Podiatrist/Orthotist Pharmacist Other health professionals as required 4. Follow-up Review as appropriate Test results Monitor progress Maintenance of healed wound
Pharmacological agents as indicated Analgesics Antibiotics Topical antimicrobials Local Anaesthetic Topical corticosteroids
Patient education for self care Hygiene Diet Foot inspection (diabetes) Dressings/Bandaging/Compression Exercise regimes
- 20 Adapted from MacLellan, L., Gardner, G., Gardner, A (2002) Designing the future in wound care: The role of the nurse practitioner. Primary Intention 10(3): 97-112 ACT Government, reprinted with permission.
Sir Charles Gairdner Hospital Nurse Practitioner Wound Management Clinical Protocols
Figure 3. NP Management Pathway for Lower Leg Ulcers:
Patient presents with lower leg ulcer
Assessment
o
Patient history Examination Investigations
Diagnosis
Other
- Disease specific treatment/referral - Local ulcer treatment* - Appropriate compression for oedema control based on ABPI
Venous ulcer ABPI >0.8:
Compression therapy
Multilayer (Elastic or inelastic) Reduced compression Graduated compression stockings Intermittent Pneumatic compression (IPC) Medical and surgical treatment as necessary (referral) Local ulcer treatment* -
Mixed arterial and venous ulcer (ABPI 0.5-0.8)
- Reduced compression therapy (15 25 mmHg) - Local ulcer treatment* - Refer to Vascular surgeon if ABPI < 0.7 or patient symptomatic (eg intermittent claudication)
Mixed arterial & venous ulcer
Severe arterial insufficiency ABPI <0.5 - Refer to Vascular
surgeon - Local ulcer treatment*
Arterial Ulcer
- Refer to Vascular surgeon - Local ulcer treatment*
- NO compression
- NO compression
Reasons for referral:
Allergy Unable to tolerate compression Uncontrolled pain No reduction in ulcer size after 4-6/52 - Cellulitis unresponsive to treatment - Frequent recurrence -
Treat concurrent issues: Active/mobile patient 1st line therapy: - Multilayer compression (elastic or inelastic) 2nd line therapy - Elastic stockings Immobile/fixed ankle patient 1st line therapy: - Multilayer compression (elastic) 2nd line therapy: - Multilayer compression (elastic + IPC
- Pain eg analgesics - Infection eg antibiotics (see Protocol 3) - Dermatitis/Eczema Consider cause (eg venous or contact) and treatment: o Corticosteroids o Zinc paste bandages o Avoid sensitisers
Ulcer fails to heal (no reduction in size in 6/52) - Refer to specialist - Re-evaluation including reassessment and diagnosis - Evaluation for surgical correction or skin grafting
Healed ulcer - Prevention of recurrence including below the knee compression stocking - Evaluation for surgical correction - Education - Review
* Local ulcer treatment (Dressing) based on:
- Assessment of wound and surrounding
skin
- Allergies / Skin sensitivities - Product availability
Education - Foot and skin care - Exercise - Nutrition - Cessation of smoking - Weight loss if obese - Disease aetiology - Dressings and bandage/compression regimes - Medications
Adapted from International Leg Ulcer Advisory Board cited in Stacey, M., Falanga, V., Marston, W., Moffat, C., Phillips, T., Sibbald, R.G., Vanscheldt, W., & Lindholm. C. (2002) - 21 The use of compression therapy in the treatment of venous leg ulcers: a recommended management pathway. EWMA Journal 2(1)
Sir Charles Gairdner Hospital Nurse Practitioner Wound Management Clinical Protocols
COMPRESSION BANDAGING SYSTEMS
Multi-layer Layers - usually 3-4 layers and may include either elastic or inelastic compression bandages, cohesive/adhesive bandages, crepe bandages and/or padding layers. Zinc bandages elastic and rigid varieties. Wound & skin contact layer. Underpadding - cotton or synthetic padding to protect the skin/ bony prominences from bandage trauma and may have additional absorbent capacity. Used as base layer under most compression bandage systems Wraps - eg Webril, Sofban, Kerlix Tubular knitted padding eg Dynacast, Tubular Plus, Samme Frotte Compression bandages, - elastic with various degrees of elasticity - inelastic Cohesive elastic wraps eg Coban, CoPlus or elastic tubular support eg Tubigrip, Versagrip, Tensogrip Single layer eg Setopress, Surepress, Tensopress
Elastic May be used across range of mobile and immobile patients but particularly indicated for immobile patients or those with reduced ankle mobility/fixed ankle deformity where calf muscle contraction is limited. Provide sustained compression with minor variations during walking. Inelastic Suitable for actively mobile clients where the bandage reinforces or supports the action of the calf muscle pump. They provide high pressure on moving and low resting pressures. May be more effective in patients with extensive deep vein reflux (Marston & Vowden, 2003).
Multilayer systems: - eg Profore system, Veno 4, Proguide
Multilayer light (reduced) compression (15-25 mm Hg versus High compression 35-45 mm Hg, @ ankle) eg Profore Light, Lastodur Light Number of layers according to ABPI, full compression usually 2 layers sub-bandage pressures will vary according to a number of factors including wear-time and oedema eg Comprilan, Lastolan, Tensolan
Note: The degree of compression in governed by La Places law where sub-bandage pressure is demonstrated thus: P is proportional to : N x T CxW
P = pressure exerted by bandage N = number of layers T = bandage tension (elasticity) C = circumference of limb W= bandage width
- 22 -
Sir Charles Gairdner Hospital Nurse Practitioner Wound Management Clinical Protocols
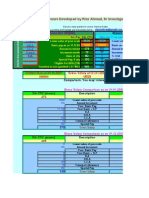
Drug Formulary Wound Management Classification
Analgesic Analgesic Analgesic Antibiotic Antibiotic Antibiotic Antibiotic Antibiotic Antibiotic Antibiotic Topical Antibiotic Topical Antibiotic Topical Antifungal Topical Antifungal Topical Antifungal Topical Antiseptic, Anti-infective Topical corticosteroid + antimicrobial Topical corticosteroid Topical corticosteroid Topical corticosteroid Topical corticosteroid Topical corticosteroid Topical Anaesthetic Local Anaesthetic Local Anaesthetic
Drug
Paracetomol Paracetamol/Codeine Tramadol Amoxycillin Clavulanate Cephalexin Dicloxacillin Flucloxacillin Ciprofloxacin Clindamycin Metronidazole Metronidazole Silver Sulphadiazine Chlorhexidine digluconate Clotrimazole Terbinafine Nystatin Mupirocin
Dosage
500-1000 mg 500mg/8-30 mg 50-100mg 500/125 875/125 mg 250 500 mg 250 500 mg 250 500 mg 250 500 mg 150 450 mg 200 400 mg 0.5% 1%, 0.2% 1% 1% 100,000units/g 2% 4-6 hourly 4-6 hourly 4-8 hourly 12 hourly 6 hourly 6 hourly 6 hourly twice daily 8 hourly 8-12 hourly twice daily 1-2 x /day 3 x /day 1-2 x /day 2-3 x /day 3 x /day
Triamcinilone/Neomycin/Nystatin 0.1%, 0.25%, 100,000U/g, 0.025% / Gramicidin 2-3 x /day Hydrocortisone Hydrocortisone acetate Triamcinolone Acetonide Betamethasone valerate Betamethasone dipropionate Lignocaine Lignocaine with Adrenaline Lignocaine with Prilocaine 0.5-1% 0.5-1% 0.02% 0.02-0.05% 0.05% 0.05-1% 0.05-1% 0.05-1% 1-2 x /day 1-2 x /day 1-2 x /day 1-2 x /day 1-2 x /day Pre-procedure Pre-procedure Pre-procedure
- 23 -
Sir Charles Gairdner Hospital Nurse Practitioner Wound Management Clinical Protocols
Analgesics
Mild Pain: Paracetamol 1000mg 4-6 hourly maximum daily dose 4000mg
For more severe pain, review causative factors and refer to appropriate specialist (eg Pain Team, Vascular Surgeon).
Mild to moderate pain: Paracetamol with Codeine 500/830mg 1-2 tablets 4 to 6 hourly maximum daily dose 4000mg paracetamol OR Tramadol 50 mg to 100mg 4 to 8 hourly maximum daily dose 400mg daily (300mg maximum dose for elderly)
(Therapeutic Guidleines: Analgesics, 2002)
Antibiotics (topical)
Localised skin infections, critical colonisation of wounds (eg leg ulcers and pressure ulcers), and minor burn prophylaxis Silver sulfadiazine (SSD) 1% + chlorhexidine 0.2% cream topically, once or twice daily.
Alternatives to consider include silver, povidoneiodine, and cadexomer iodine dressing products.
(contraindicated if sulpha or chlorhexidine allergy) Impetigo, infected small skin lesions(mild or localised infections) and elimination of Staph.aureus carriage Mupirocin 2% topically, following skin cleansing 3 times per day for up to 10 days
Cancerous malodourous wounds Metronidazole gel 0.75% topically Silver sulfadiazine (SSD) 1% + chlorhexidine 0.2% cream topically, once or twice daily.
(Sibbals, Orsted, Schultz et al., 2003; Therapeutic Guidelines: Antibiotic, 2006; Therapeutic Guidelines: Dermatology, 2002)
- 24 -
Sir Charles Gairdner Hospital Nurse Practitioner Wound Management Clinical Protocols
Antibiotics (systemic)
Skin and soft tissue infection3 Common infecting organisms may include: Staphylococcus aureus, MRSA, Streptococcus species, Pseudomonas aeruginosa, and anaerobes Empirical antibiotics to be commenced whilst waiting for sensitivities For mild to moderate infection with surrounding cellulitis, use: Di/flucloxacillin 500 mg orally 6-hourly for at least 5 days
The routine use of antibiotics is not advocated in chronic wounds. Antibiotics to be commenced only when there is clinical evidence of infection (e.g. localised erythema, localised pain, localised heat, cellulitis, and oedema). If no clinical improvement within one week (next visit) or worsening of symptoms, for medical review.
For patients hypersensitive to penicillin (excluding immediate hypersensitivity), use:
Cephalexin 500mg 6-hourly for at least 5 days For more severe infections, particularly Diarrhoea is a common adverse effect where systemic and the patient should be told to seek symptoms are present, medical attention should this occur. and for, intravenous antibiotics, medical review Alternatively, if Gram-negative will be required. organisms are suspected or known to be involved, use: Amoxycillin+clavulanate 875+125mg orally, 12 hourly for 5 days Antibiotic susceptibilities of gram negative organisms should be reviewed and advice obtained from a clinical Microbiologist or ID Physician for organisms resistant to amoxycilllin + clavulanate.
Gram-negative organisms often colonise ulcers. Therefore for less severe infections, antibiotics against gram positive organism should be used initially. If the infection is not responding then broadening to include gram-negative cover can then be considered.
(Therapeutic Guidelines: Antibiotic, 2006)
- 25 -
Sir Charles Gairdner Hospital Nurse Practitioner Wound Management Clinical Protocols
Diabetic foot infections: For mild to moderate infection with no evidence of osteomyelitis or septic arthritis, use: Or Cephalexin 500mg orally, 6-hourly for at least five days Amoxycillin+clavulanate 875+125mg orally, 12-hourly for at least five days
For severe limb- or lifethreatening infection (systemic toxicity/septic shock, bacteraemia, marked necrosis or gangrene, ulceration to deep tissues, severe cellulitis, presence of osteomyelitis) medical review is required.
Plus Metronidazole 400mg orally, 12-hourly for at least five days
Inform patients that nausea, diarrhoea and metallic taste an adverse effect whilst taking metronidazole. To seek medical attention for nausea and diarrhoea. For patients with penicillin hypersensitivity, use: Ciprofloxacin 500mg orally, 12 hourly for at least 5 days Approval is required from a Clinical Microbiologist or ID Physician for Ciprofloxacin use.
To seek medical attention if the patient develops a rash, nausea, vomiting, diarrhoea, abdominal pain, and/or dyspepsia. Plus Clindamycin 300 mg to 450 mg orally, t.d.s. for at least 5 days
Patients must be informed of the adverse effect of diarrhoea with a risk of pseudomembranous colitis, whilst taking clindamycin. Patients must be told to report these side effects and seek medical attention.
(Therapeutic Guidelines: Antibiotic, 2006)
- 26 -
Sir Charles Gairdner Hospital Nurse Practitioner Wound Management Clinical Protocols
Topical Antifungal
Tinea (body, limbs, face and interdigital) Terbinafine 1% topically, daily for 7 days
Or an imidazole: Clotrimazole 1% topically, 2 to 3 times daily for 2 to 4 weeks, continued for 14 days after symptoms resolve.
Diagnosis of fungal infection can be confirmed via microscopy and culture of skin scrapings, subungal debris, nails or plucked hair.
Cutaneous candidiasis Clotrimazole 1% topically, 2 to 3 times daily for 2 to 4 weeks, continued for 14 days after symptoms resolve. Or Nystatin 100,000 units/g cream topically, 2 to 3 times per day. Continue treatment for 2 weeks after symptoms resolve.
If necessary for inflammation, add Hydrocortisone cream1% topically, 2 to 3 times daily If poor response, or topical treatment is impracticable, refer to Microbiologist or dermatologist for consideration of systemic treatment.
(Therapeutic Guidelines: Dermatology, 2004)
- 27 -
Sir Charles Gairdner Hospital Nurse Practitioner Wound Management Clinical Protocols
Topical Corticosteroid
Stasis/contact dermatitis 2 Mild Hydrocortisone cream1% topically, 2 to 3 times daily Or Hydrocortisone acetate 1% cream or ointment 30g. Apply once or twice daily Moderate Betamethasone valerate 0.02% 0.05% cream or ointment topically, once or twice daily Or Triamcinolone acetonide 0.02% topically once or twice daily Severe Betamethasone dipropionate cream or ointment 0.05%, topically once or twice daily (use sparingly, and for as short a period of time as possible, due to potency and potential local adverse effects).
(Therapeutic Guidelines: Dermatology, 2004)
Uncomplicated stasis dermatitis is common in chronic leg ulcers. Stasis dermatitis is frequently complicated by allergic contact dermatitis, which usually resolves with the removal of the sensitising agents (frequently encountered in many dressing products) and treatment with a mild/moderate topical corticosteroid. If poor response, refer to a dermatologist.
Topical corticosteroid + antimicrobial
Skin infections and small areas of overgranulation Triamcinolone 0.1% / Neomycin 0.25% / Nystatin 100,000U/g / Gramicidin 0.025% cream topically 2 to 3 times per day for up to one week.
Local anaesthetic
Biopsy Lignocaine (7mg/kg) with Adrenaline (5 micrograms/ml). Lignocaine%, adrenaline 1:100 000, 5mL. Lignocaine 1%, 5mL Lignocaine with adrenaline should not be used on an extremity, such as a digit, especially in the presence of PAD, to avoid potential necrosis. For infiltration 1-2 mL is sufficient to provide anaesthesia and will not distort the histology
Local wound debridement (pre procedure) where appropriate Lignocaine with Prilocaine 0.05-1% topically.
(Rossi [Ed], 2005; Therapeutic Guidelines: Dermatology, 2004).
- 28 -
You might also like
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- November NewsletterDocument4 pagesNovember NewsletterlawyergirlNo ratings yet
- Aprn Observation PaperDocument7 pagesAprn Observation PaperSharon ScottNo ratings yet
- Colorado Peace Officer Manual 2013Document373 pagesColorado Peace Officer Manual 2013Brian Harris100% (1)
- Answer-A Rationale: Pityriasis Rosea Presents With Papulo-Squamous Lesions of 2 To 20 CM Diameter, inDocument15 pagesAnswer-A Rationale: Pityriasis Rosea Presents With Papulo-Squamous Lesions of 2 To 20 CM Diameter, inarunatejaNo ratings yet
- Common Bacteria by Site of Infection: Mouth Skin/Soft Tissue Bone and JointDocument72 pagesCommon Bacteria by Site of Infection: Mouth Skin/Soft Tissue Bone and JointMuthia FadhilaNo ratings yet
- Olivia Engle NP ResumeDocument1 pageOlivia Engle NP Resumeapi-654403621No ratings yet
- ICN - APN Report - 2020Document44 pagesICN - APN Report - 2020Daniela Silva100% (1)
- Chapter38 Assessment and Management of Patients With Rheumatic DisordersDocument38 pagesChapter38 Assessment and Management of Patients With Rheumatic Disordersjericho dinglasanNo ratings yet
- Maternity Antepartum Genetic TestingDocument21 pagesMaternity Antepartum Genetic TestingBobbie N Melinda RussellNo ratings yet
- Certified Family Nurse Practitioner in West Palm Beach FL Resume Pamela ValleDocument3 pagesCertified Family Nurse Practitioner in West Palm Beach FL Resume Pamela VallePamelaValleNo ratings yet
- Patient Case Presentation StructureDocument30 pagesPatient Case Presentation StructureAmira HelayelNo ratings yet
- Basic Foot Assessment ChecklistDocument2 pagesBasic Foot Assessment ChecklistPalwasha MalikNo ratings yet
- Arizona Pharmacy Board Regulations and RequirementsDocument5 pagesArizona Pharmacy Board Regulations and Requirementseze24No ratings yet
- Nails Diagnosis, Therapy, Surgery Richard K Scher MD, C Ralph DanielDocument319 pagesNails Diagnosis, Therapy, Surgery Richard K Scher MD, C Ralph DanieldrNo ratings yet
- Test Bank Advanced Practice Nursing Essential Knowledge For The Profession 4th Edition DeNiscoDocument3 pagesTest Bank Advanced Practice Nursing Essential Knowledge For The Profession 4th Edition DeNiscoFit ragner0% (1)
- APN Adult Gerontology PresentationDocument57 pagesAPN Adult Gerontology PresentationMelissa Makhoul100% (1)
- Antibiotic Prescribing in Primary Care - Therapeutic Guidelines Summary Table 2019Document2 pagesAntibiotic Prescribing in Primary Care - Therapeutic Guidelines Summary Table 2019RL100% (1)
- FNP Resume Jenna Gibson 2022Document2 pagesFNP Resume Jenna Gibson 2022api-619271904No ratings yet
- 32-Week OB CheckDocument4 pages32-Week OB CheckG. Crusor-PriceNo ratings yet
- AMSN Scope Standards MS NursingDocument27 pagesAMSN Scope Standards MS NursingPaulEspartinezNo ratings yet
- South Maine HMO Allied ProfessionalsDocument364 pagesSouth Maine HMO Allied ProfessionalsMaine Trust For Local NewsNo ratings yet
- Juvenile Hallux Valgus PDFDocument14 pagesJuvenile Hallux Valgus PDFŞtefaniuc IulianNo ratings yet
- H&P For ScriptDocument12 pagesH&P For ScriptAlina KievskyNo ratings yet
- SOAP Note - ContraceptionDocument5 pagesSOAP Note - ContraceptionG. Crusor-PriceNo ratings yet
- AHP - Family Nurse PractitionerDocument6 pagesAHP - Family Nurse PractitionerMaria Fudji HastutiNo ratings yet
- Mood Disorders: Advanced Practice Education AssociatesDocument11 pagesMood Disorders: Advanced Practice Education AssociatesAndrea100% (1)
- American Nurses Credentialing Center (ANCC) Adult Nurse Practitioner Exam Study GuideDocument20 pagesAmerican Nurses Credentialing Center (ANCC) Adult Nurse Practitioner Exam Study GuideMcRee Learning CenterNo ratings yet
- Healing of UsaDocument3 pagesHealing of Usaapi-237353755No ratings yet
- Normal Foot and Ankle Radiographic Angles, Measurements, and Reference PointsDocument8 pagesNormal Foot and Ankle Radiographic Angles, Measurements, and Reference PointsCinthya BorgesNo ratings yet
- Operative Techniques in Foot and Ankle Surgery 2nd Edition Ebook PDFDocument61 pagesOperative Techniques in Foot and Ankle Surgery 2nd Edition Ebook PDFmaurice.honeycutt512100% (41)
- Behavioral Health Care Plan: Assessment DataDocument9 pagesBehavioral Health Care Plan: Assessment Dataapi-521018364No ratings yet
- Psychiatric Nurse PractitionerDocument3 pagesPsychiatric Nurse Practitionerapi-77646014No ratings yet
- C 26Document9 pagesC 26Tammie GoreNo ratings yet
- Real Resume Family Nurse Practitioner Resume Phoenix ArizonaDocument1 pageReal Resume Family Nurse Practitioner Resume Phoenix ArizonaRick WhitleyNo ratings yet
- AMBULATORY WOMEN'S HEALTH CARE NURSING: Passbooks Study GuideFrom EverandAMBULATORY WOMEN'S HEALTH CARE NURSING: Passbooks Study GuideNo ratings yet
- Guide To APRN RoleDocument4 pagesGuide To APRN RoleLaceyNo ratings yet
- List The Most Prominent Characteristics Physical Sensations Dentification ProcessDocument2 pagesList The Most Prominent Characteristics Physical Sensations Dentification ProcessMary Joy NoquiaoNo ratings yet
- Pharmacology Syllabus Bio 408 Sum 2017Document6 pagesPharmacology Syllabus Bio 408 Sum 2017Grafika DiahNo ratings yet
- FNP - NursingDocument1 pageFNP - NursingChelsea ManaloNo ratings yet
- Aseptic Wound Dressing Edited 3 Dec 2008Document11 pagesAseptic Wound Dressing Edited 3 Dec 2008zahisma89No ratings yet
- Aprn PresentationDocument12 pagesAprn Presentationapi-234511817No ratings yet
- Cronic WoundsDocument11 pagesCronic WoundsAyline Araceli AlavaNo ratings yet
- Running Head: CASE STUDY 1Document17 pagesRunning Head: CASE STUDY 1api-507206712No ratings yet
- Solomon Sallfors: Ambulatory Morning Report 1: AcneDocument3 pagesSolomon Sallfors: Ambulatory Morning Report 1: AcneSolomon Seth SallforsNo ratings yet
- The WHO Health Promotion Glossary PDFDocument17 pagesThe WHO Health Promotion Glossary PDFfirda FibrilaNo ratings yet
- SOAP NotesDocument4 pagesSOAP Notesemmag79No ratings yet
- C 21Document23 pagesC 21jackNo ratings yet
- Oral Contraceptive Reference ChartDocument6 pagesOral Contraceptive Reference Chartpdoan85No ratings yet
- Pocket Guide To 2015 Beers Criteria PDFDocument7 pagesPocket Guide To 2015 Beers Criteria PDFYuliEdySeringnyungsepNo ratings yet
- Initial Approach to Trauma LectureDocument74 pagesInitial Approach to Trauma LectureOjambo FlaviaNo ratings yet
- The Complete Medical Record and Electronic Charting: Chapter OutlineDocument25 pagesThe Complete Medical Record and Electronic Charting: Chapter OutlineabedelmasriNo ratings yet
- Family Nurse Practitioner PortfolioDocument3 pagesFamily Nurse Practitioner Portfolioapi-313534615No ratings yet
- Chapter 001Document9 pagesChapter 001Rachael CrossgroveNo ratings yet
- NURSING THE CHILDBEARING FAMILY: Passbooks Study GuideFrom EverandNURSING THE CHILDBEARING FAMILY: Passbooks Study GuideNo ratings yet
- Guide to Physical Assessment DocumentationDocument3 pagesGuide to Physical Assessment Documentationsandaman2225No ratings yet
- State by State Nurse Practitioner RequirementsDocument29 pagesState by State Nurse Practitioner RequirementsRick Whitley100% (1)
- Technique: Preventing and Controlling Infections in Home Care and HospiceDocument7 pagesTechnique: Preventing and Controlling Infections in Home Care and HospiceOlaMostafaNo ratings yet
- Hypertension PDFDocument19 pagesHypertension PDFVicta RyzaNo ratings yet
- Chapter 2 Family Centered Community Based CareDocument2 pagesChapter 2 Family Centered Community Based CareBlake McCabeNo ratings yet
- Spices ToolDocument2 pagesSpices ToolTrisha Fae Loyola BalagotNo ratings yet
- Professional Nursing OrganizationsDocument6 pagesProfessional Nursing OrganizationsJohn Askof NyabutiNo ratings yet
- Diabetes and Complications: When Documenting Diabetes, It's Important To Note The FollowingDocument2 pagesDiabetes and Complications: When Documenting Diabetes, It's Important To Note The Followingmeikaizen100% (1)
- California school immunization recordDocument2 pagesCalifornia school immunization recordWillNo ratings yet
- Patho Exam QuestionsDocument3 pagesPatho Exam QuestionsAndin GangNo ratings yet
- When Accepting A Gift Can Be Professional Misconduct and Theft.Document3 pagesWhen Accepting A Gift Can Be Professional Misconduct and Theft.Arlene MarasiganNo ratings yet
- Nursing 660 - PresentationDocument12 pagesNursing 660 - Presentationapi-282992446No ratings yet
- Providing Culturally Appropriate Care: A Literature ReviewDocument9 pagesProviding Culturally Appropriate Care: A Literature ReviewLynette Pearce100% (1)
- An AntipsychoticDocument4 pagesAn AntipsychoticJoMa TuazonNo ratings yet
- Colorado CRS 18 18 - Uniform Controlled Substances Acto of 1992 Effective 7-1-2009Document69 pagesColorado CRS 18 18 - Uniform Controlled Substances Acto of 1992 Effective 7-1-2009Brian HarrisNo ratings yet
- Colorado Revised Statutes (CRS 12 42.5) Title 12 Article 42.5 Professions and Occupations Pharmacists, Pharmacy Businesses, and PharmaceuticalsDocument48 pagesColorado Revised Statutes (CRS 12 42.5) Title 12 Article 42.5 Professions and Occupations Pharmacists, Pharmacy Businesses, and PharmaceuticalsBrian HarrisNo ratings yet
- Colorado Medical Use of Marijuana Department of Public Health and Environment Health and Environmental Information and Statistics Division 5 CCR 1006-2Document18 pagesColorado Medical Use of Marijuana Department of Public Health and Environment Health and Environmental Information and Statistics Division 5 CCR 1006-2Brian HarrisNo ratings yet
- Colorado Medical Use of Marijuana Revised Statutes 18-18-406.3Document2 pagesColorado Medical Use of Marijuana Revised Statutes 18-18-406.3Brian HarrisNo ratings yet
- Colorado CRS 18 18 - Uniform Controlled Substances Acto of 1992 Effective 7-1-2009Document69 pagesColorado CRS 18 18 - Uniform Controlled Substances Acto of 1992 Effective 7-1-2009Brian HarrisNo ratings yet
- Colorado Revised Statutes (CRS 12 12)Document65 pagesColorado Revised Statutes (CRS 12 12)Brian HarrisNo ratings yet
- Colorado Medical Board Policy Guidelines For The Use of Controlled Substances For The Treatment of Pain 12-36-117, C.R.S.Document5 pagesColorado Medical Board Policy Guidelines For The Use of Controlled Substances For The Treatment of Pain 12-36-117, C.R.S.Brian HarrisNo ratings yet
- Colorado Revised Statutes (CRS 12 36) Title 12 Article 36 and Article 36.5 Professions and Occupations, Medical Practice, Professional Review of Health Care ProvidersDocument57 pagesColorado Revised Statutes (CRS 12 36) Title 12 Article 36 and Article 36.5 Professions and Occupations, Medical Practice, Professional Review of Health Care ProvidersBrian HarrisNo ratings yet
- Colorado Preferred Drug List (PDL) 2013Document25 pagesColorado Preferred Drug List (PDL) 2013Brian HarrisNo ratings yet
- Colorado Guidelines of Professional Practice For Controlled Substances AddendumDocument14 pagesColorado Guidelines of Professional Practice For Controlled Substances AddendumBrian HarrisNo ratings yet
- Colorado Guidelines of Professional Practice For Controlled Substances AddendumDocument14 pagesColorado Guidelines of Professional Practice For Controlled Substances AddendumBrian HarrisNo ratings yet
- Colorado House Bill 11-1043 Concerning Medical Marijuana, and Making An Appropriation ThereforDocument24 pagesColorado House Bill 11-1043 Concerning Medical Marijuana, and Making An Appropriation ThereforBrian HarrisNo ratings yet
- Colorado Drug Control UpdateDocument7 pagesColorado Drug Control UpdateBrian HarrisNo ratings yet
- 42 CFR Part 8 Opioid Drugs in Maintenance and Detoxification Treatment of Opiate Addiction Final RuleDocument28 pages42 CFR Part 8 Opioid Drugs in Maintenance and Detoxification Treatment of Opiate Addiction Final RuleBrian HarrisNo ratings yet
- Colorado Guidelines of Professional Practice For Controlled SubstancesDocument65 pagesColorado Guidelines of Professional Practice For Controlled SubstancesBrian HarrisNo ratings yet
- Colorado Medical Marijuana Laws, Statutes, and CodesDocument60 pagesColorado Medical Marijuana Laws, Statutes, and CodesGreenpoint Insurance ColoradoNo ratings yet
- Colorado Licensing of Controlled Substances Act 2013 Sunset ReviewDocument31 pagesColorado Licensing of Controlled Substances Act 2013 Sunset ReviewBrian HarrisNo ratings yet
- Colorado Medical Board Policy Guidelines Pertaining To The Release and Retention of Medical Records Policy Number 40-07Document2 pagesColorado Medical Board Policy Guidelines Pertaining To The Release and Retention of Medical Records Policy Number 40-07Brian HarrisNo ratings yet
- Colorado Revised Statutes (CRS 12 42.5) Title 12 Article 42.5 Professions and Occupations Pharmacists, Pharmacy Businesses, and PharmaceuticalsDocument48 pagesColorado Revised Statutes (CRS 12 42.5) Title 12 Article 42.5 Professions and Occupations Pharmacists, Pharmacy Businesses, and PharmaceuticalsBrian HarrisNo ratings yet
- 42 CFR Part 8 Opioid Drugs in Maintenance and Detoxification Treatment of Opiate Addiction Final RuleDocument28 pages42 CFR Part 8 Opioid Drugs in Maintenance and Detoxification Treatment of Opiate Addiction Final RuleBrian HarrisNo ratings yet
- Colorado Guidelines of Professional Practice For Controlled SubstancesDocument65 pagesColorado Guidelines of Professional Practice For Controlled SubstancesBrian HarrisNo ratings yet
- Medical Injuries or Illnesses To Use Medical Marijuana in ColoradoDocument5 pagesMedical Injuries or Illnesses To Use Medical Marijuana in ColoradoGreenpoint Insurance ColoradoNo ratings yet
- Colorado Guidelines of Professional Practice For Controlled SubstancesDocument65 pagesColorado Guidelines of Professional Practice For Controlled SubstancesBrian HarrisNo ratings yet
- ASAM The Role of The Physician in "Medical" MarijuanaDocument60 pagesASAM The Role of The Physician in "Medical" MarijuanaBrian HarrisNo ratings yet
- Alcohol and Drug Abuse Division (ADAD) Substance Use Disorder Treatment Rules Colorado DHSDocument80 pagesAlcohol and Drug Abuse Division (ADAD) Substance Use Disorder Treatment Rules Colorado DHSBrian HarrisNo ratings yet
- Pharmacist's Manual - An Information Outline of The Controlled Substances Act - 2010Document85 pagesPharmacist's Manual - An Information Outline of The Controlled Substances Act - 2010James LindonNo ratings yet
- The DEA Position On MarijuanaDocument63 pagesThe DEA Position On MarijuanaBrian HarrisNo ratings yet
- ProPublica MethodologyDocument5 pagesProPublica MethodologySouthern California Public RadioNo ratings yet
- 08 10 Main3Document41 pages08 10 Main3Lindsey RobbinsNo ratings yet
- Klasifikasi WagnerDocument8 pagesKlasifikasi WagnerNina AmeliaNo ratings yet
- Check Out The Buyers Guide On FacebookDocument28 pagesCheck Out The Buyers Guide On FacebookCoolerAdsNo ratings yet
- A Guide Benefits of PodiatryDocument20 pagesA Guide Benefits of PodiatryIga AmandaNo ratings yet
- Emb 2011Document5 pagesEmb 2011navnaNo ratings yet
- Women in Business GuideDocument20 pagesWomen in Business GuidewednesdayjournalNo ratings yet
- 2008-11-05Document24 pages2008-11-05CoolerAdsNo ratings yet
- Mirfield Word JulyDocument84 pagesMirfield Word JulyjennaNo ratings yet
- 2016 FINAL Program - 01 - 25 - 16 - Low Res PDFDocument72 pages2016 FINAL Program - 01 - 25 - 16 - Low Res PDFbaoNo ratings yet
- Hallux Valgus TriplanarDocument10 pagesHallux Valgus TriplanarFreddy Churata SuriNo ratings yet
- Equipment Permit App Inst PDFDocument10 pagesEquipment Permit App Inst PDFDorothy ZadrineNo ratings yet
- Atta Asef 1 PDFDocument32 pagesAtta Asef 1 PDFWKYC.comNo ratings yet
- 17 Annual National Clinical Conference: AbstractsDocument50 pages17 Annual National Clinical Conference: AbstractsbaoNo ratings yet
- Nchcap WorkshopDocument72 pagesNchcap WorkshopHeather-Summer AndersonNo ratings yet
- Biomechanics of a Sit-Up: 4 Phases and Muscle ActivityDocument3 pagesBiomechanics of a Sit-Up: 4 Phases and Muscle ActivityLiezel-jheng Apostol LozadaNo ratings yet
- Diabetic FootDocument7 pagesDiabetic FootWiindha Tahta Alfina CiigejeeNo ratings yet
- Extra ExtraDocument24 pagesExtra ExtrabaoNo ratings yet
- Physiotherapy Belfast - Apex Clinic BrochureDocument2 pagesPhysiotherapy Belfast - Apex Clinic BrochureApexclinicNo ratings yet
- Mddo PhysicianshandbookDocument88 pagesMddo Physicianshandbookmary engNo ratings yet
- 31412Document369 pages31412aptureinc100% (5)
- NSWNMA Guidelines On Provision of Basic Foot Care by NursesDocument3 pagesNSWNMA Guidelines On Provision of Basic Foot Care by NursesKlinik KitamuraNo ratings yet
- Nbpme Part III Cib 20140207Document24 pagesNbpme Part III Cib 20140207TPod2014No ratings yet