Professional Documents
Culture Documents
Chapter 44: Nursing Care of The Client With An Hematologic Disorders
Uploaded by
fLOR_ZIANE_MAEOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chapter 44: Nursing Care of The Client With An Hematologic Disorders
Uploaded by
fLOR_ZIANE_MAECopyright:
Available Formats
Chapter 44: NURSING CARE OF THE CLIENT WITH AN HEMATOLOGIC DISORDERS
SAMPLE DISORDERS BLOOD CELLS NORMAL VALUES INCREASED RBC Hematocrit Hemoglobin Reticulocytes WBC Neutrophil Eosinophil 4-6 Million cu.mm 38-48% 12-18g/100mL 0-1.5% 5K-10K cu.mm Infection 55-70% 1-3% Allergic Response and some leukemia Hyperthyroidism, some bone marrow disorders, ulcerative colitis Viral, bacterial infection and some leukemia Chronic inflammatory disorders Trauma Blood disorder Chronic hypoxia Dehydration or chronic hypoxia Hypoxia or Anemia Anemia or blood loss DECREASED
RBC Defect
Basophil
.5-1%
Lymphocytes Monocytes PLATELETS
20-35% 3-8% 150K-300K
The blood and blood forming tissues that make up the hematologic system play a vital role in body metabolism: 1. Transporting oxygen, nutrients to body cells and hormones 2. Removing waste products of the cells 3. Production of antibodies for body protection 4. Initiation of blood coagulation. 5. Regulation of body temperature, pH, and fluid balance Hematologic disorder often called Blood Dyscrasias mostly in children originate in bone marrow, where blood cells are formed. STRUCTURE AND FUNCTION OF BLOOD Formation of Blood in Intrauterine Life: Fetal yolk sac As early as week 2 of intrauterine life Liver and Spleen It begins forming blood by month 2. Extrauterine life the spleen serves as the organ for the destruction of blood cells. Marrow Cavity of Bones Becomes and remains active center for the hemapoetic site by month 4 intrauterine life. Red Marrow The hematopoietic sites occurs primary in the Red Marrow which is found in all bones at the stage of development.
1. 2. 3. 4. 5. 6. 7. 8.
Newborn to 5 years Yellow Marrow In old age, red marrow sites are slowly replaced with yellow, inactive marrow. 4-6 liters of blood in the human body. 55% is Plasma ( Water, Electrolytes, Proteins) 45% is Formed Elements (RBC, WBC and Platelets) KEY TERMS Anemia- is a decrease in number of red blood cells (RBCs) or less than the normal quantity of hemoglobin in the blood. Erythropenia - deficiency in the number of red blood cells. Erythrocytosis -an increase above the normal in the number of red cells in the blood. Leukopenia - any condition in which the number of leukocytes in the circulating blood is less than normal, the lower limit of which is generally regarded as 40005000 per cu mm. Syn: leukocytopenia. Leukocytosis - an abnormally large number of leukocytes; a white blood cell count of 10,000 or more per cu mm. Syn: neutrophilia. Thrombocytopenia -a condition in which there is an abnormally small number of platelets in the circulating blood. Syn: Thrombopenia. Thrombocytosis - an increase in the number of platelets in the circulating blood. Syn: Thrombocythemia. Pancytopenia pronounced reduction in the number of RBC, all types of WBC and Platelets in the circulating blood. RED BLOOD CELLS RBCs are formed under the stimulation of erythropoietin. Biconcave, lack nucleus, plasma membrane is strong, flexible, thin. Life span- 100-120 days Cannot reproduce due to lack of nucleus & other organelles Carry O2, contains oxygen carrying protein called hemoglobin Reticulocytes are immature RBC released by bone marrow. RBCs are destroyed through phagocytosis by the reticuloendothelial cells, found in the highest portion in the spleen. At birth, infants has approximately 5 million RBCs per cubic millimeter of blood. Then diminishes rapidly in the first months to 4-5 months of age. Then the number slowly increase until adolescence. Hemoglobin Composed: Globin - a protein dependent on nitrogen metabolism for its formation. Heme - an iron-containing pigment which combines oxygen and carbon dioxide for transport. Deficiency of either iron stores or nitrogen interfere with the synthesis of hemoglobin. Hemoglobin levels are highest at birth; they reach a low at approximately 3 months of age, and then gradually rise again until adults values are reached at puberty. - Hemoglobin F Fetal hemoglobin has a special affinity for oxygen, so it can absorb oxygen at the low oxygen tension that exist in utero. Composed: Two alpha and two gamma polypeptide chains. At birth 40-70% of the infants hemoglobin is hemoglobin F. This gradually replaced by adult hemoglobin (hemoglobin A) during the first 6 months of life. -Hemoglobin A Composed: Two alpha and two beta chains. Diseases such as sickle cell anemia and thalassemias, which are disorder of the beta chains, do not become apparent clinically until this hemoglobin change has occurred. How ever Hemoglobin A is present even in early intrauterine life, they can be diagnosed prenatally by hemoglobin analysis or electrophoresis.
-Bilirubin Formed from hemoglobin during normal and abnormal destruction of erythrocytes by the reticuloendothelial system. As the portion of heme degraded, it is converted into protoporphyrin. Protoporphyrin is then further broken down into indirect bilirubin. Indirect bilirubin - is a fat soluble and cannot be excreted by the kidneys in this state. It is therefore converted by the liver enzymes glucuronyl transferase into direct bilirubin. Direct Bilirubin is a water soluble and is excreted in bile. WHITE BLOOD CELLS Less numerous than RBC Larger than RBC Have nuclei when matures The bodys defense against diseases (bacteria, viruses, parasites & tumor cells) A typical total white cell count is 5k-10k cells per cubic millimeter of blood. In newborn 20k per cubic millimeter caused by the trauma of birth. WBC have a huge amount of variety in their life spans. Two Main forms of WBCs Granulocytes first line of cellular defense. Basophils Eosinophils Neutrophils Agranulocytes Monocytes Lymphocytes PLATELETS The function of platelets is the maintenance of hemostasis. Lifespan of a platelet is normally just 5 to 9 days. White strip often called as Buffy Coat forms that consists of the WBC and thrombocytes. Megakaryocytes are immature thrombocytes. Blood Coagulation Factors Fibrinogen Antihemophilic factor Prothrombin Christmas Factor Thromboplastin Stuart Factor Calcium Ions Plasma thromboplastin anteccedent Labile factor Hageman factor (unassigned) old name Factor Va Fibrin stabilizing factor Stable factor BLOOD COAGULATION NURSING PROCESS OVERVIEW ASSESSMENT Chief concern: Fatigue, easy bruising, epistaxis. Past medical History: Low birth weight, lack of vitamin K administration at birth Nutrition: Pickey eater or presence of pica, increased milk intake. Past illnesses Family History Physical examination NURSING DIAGNOSIS Deficient knowledge related to the cause of childs illness Imbalanced nutrition, less than body requirements, related to parental lack of knowledge of need for iron rich foods. Anxiety related to frequent blood-sampling procedures Pain related to tissue ischemia
Compromised family coping related to long term care needs of child with a chronic hematologic disorder. OUTCOME IDENTIFICATION AND PLANNING Helping parents of a realistic outcomes Prescribed of a long term medication such as corticosteroid and educating the parents about the drugs. Good nutritional planning Keep the child interested in activities that promote development. Providing resources for education and support. NURSING PROCESS OVERVIEW IMPLEMENTATION Specimen for blood testing Assisting with blood or stem cell transfusions Providing comfort in withdraw of blood. Providing parents and children often need the support of outside agencies. OUTCOME EVALUATION Parents correctly state the most frequent cause of iron-deficiency anemia. Childs feel better and able to cope up with blood sampling procedure. Parents describe realistic plans. Voice understanding importance of preventing dehydration in school-age child with sickle-anemia.
ASSESSMENT OF AND THERAPEUTIC TECHNIQUES FOR HEMATOLOGIC DISORDERS 1. BONE MARROW ASPIRATION AND BIOPSY Provides samples of bone marrow so that the type and quantity of cells can be determined. Common site for aspiration in children is the iliac crests or the spines Site for neonates anterior tibia. PROCEDURE Child lies prone on hard treatment table rather than bed. Conscious sedation to reduce the childs fear. Topical anesthesia helps reduce the pain. Site is cleaned with an antiseptic solution and draped Large-bore needle and stylus inserted into the bone when the marrow reached the stylus is removed, syringed is then attached to the needle. Aspirated with (thick blood in syringe) Pressured dressing is applied to the site Monitor vital signs until the child is fully awake. Monitor dressing every 15mins. Check the temperature 12 and 24 hours after the procedure to detect infection. 2. BLOOD TRANSFUSION Large losses of blood have serious consequences Loss of 15 to 30 percent causes weakness Loss of over 30 percent causes shock, which can be fatal Transfusions are the only way to replace blood quickly Transfused blood must be of the same blood group ABO GROUPS Testing for the presence of A and B antigens on RBCs is the most important system for classifying blood: Type A blood has A antigen on its surface Type B blood has B antigen Type AB blood has both A and B antigens Type O blood as neither A nor B antigen. ABO GROUPS A donors blood must be compatible with a recipients or the result can be fatal. The following blood groups are compatible: Type A with Type A or O
Type B with Type B or O Type AB with Type A, B, AB, or O Type O with Type O only. BLOOD TRANSFUSION REACTION Anaphylactic reaction Headache, chills, back pain, dyspnea, hypotension, hemoglobinuria D/C transfusion Maintain normal NSS infusion for accessible IV line O2 Diuretic, heparin Allergy to protein components of transfusion Pruritus, urticaria, wheezing D/C transfusion temporarily Give O2 PRN Antihistamine Contaminant in transfused blood Increased temperature D/C transfusion Obtain blood culture to rule out bacterial invasion as ordered. Circulatory overload Increased pulse, dyspnea D/C transfusion O2 Provide supportive care for pulmonary edema and CHF Diuretic Acid-citrate-dextrose anticoagulant in transfusion is combining with serum calcium and causing hypocalcemia Muscle cramping, twitching of extremities, convulsion D/C transfusion Calcium gluconate IV Hepatitis from contaminated transfusion Fever, jaundice, lethargy, tenderness over liver Obtain transfusion history of any child with hepatitis symptoms Referral to Hepatitis care Hemosiderosis - deposition of iron from transfusion in skin Bronze colored skin Support self-esteem with altered body imagine Administer iron chelating agent (deferoxamine) 3. STEM CELL TRANSPLANTATION Is the IV infusion of hematopoietic stem cells from bone marrow obtained by marrow aspiration or from peripheral or umbilical cord blood from a donor to reestablish marrow function in a child with defective or nonfunctioning bone marrow. Common procedure in children with blood dyscrasia Success depends on Human Leukocytes Antigen compatibility of donated donor. Allogeneic Transplantation- transfer of stem cells from an immune-compatible (Histocompatible) donor, usually a sibling. Synergenic Transplantation- donor and recipient are genetically identical (identical twins) Autologous Transplantation- own stem cells are used To prevent child from rejecting newly transplanted donor stem cells by the T lymphocytes, a drug such as cyclophosphamide (Cytoxan) will be administered IV to a child before the procedure to suppress marrow and T Lymphocytes production.
Fever and chills are common reaction to a stem cell transplant infusion. (Acetaminophen, diazepam, diphenhydramine hydrochloride) WBC monitoring 4. STEM CELL TRANSPLANTATION Graft-Versus-Host Disease Is a potentially lethal immunologic response of donor T cells against the tissue of the bone marrow recipient. Symptoms: Rash General Malaise High fever Diarrhea Spleenomegaly Liver enlargement No known cure Prevention is essential. 5. SPLEENECTOMY is a surgical procedure that partially or completely removes the spleen. It is removed under the following circumstances: When it becomes very large such that it becomes destructive to platelets/red blood cells When platelets are destroyed in the spleen as a result of an auto-immune process. For long-term treatment of congenital erythropoietic porphyria (CEP) if severe hemolytic anemia develops After surgery oral penicillin is given as prophylactic antibiotic for a year or two to guard against infection. Should be given Pneumococcal and meningococcal vaccines as well as routine immunizations. Teach parents sign of infection and encourage them to report this signs immediately. Nursing Diagnosis #1 Anxiety related to lack of knowledge about the procedure and expected outcome of stem cell transplant. Outcome evaluation: Parents and child understand they are not responsible for the outcome of the transplant. Emphasize that success does not depend on their behavior or what kind of person they are but on immunologic factors over which they have no control. Education of the donor and the recipients. Conscious sedation will leave them feeling exhausted for several days. Nursing Diagnosis #2 Risk for delayed growth and development related for extended restrictions and infection control precaution in hospital or at home. Outcome Evaluation: Restriction of a child from interacting with other children to prevent infection. Visit the room frequently but provide sterilized play materials as appropriate.
HEALTH PROMOTION AND RISK MANAGEMENT Many hematologic diorders such as sickle anemia and hemophilia are inherited disorders. Health promotion and disease prevention, therefore, begins with ensuring that families have access to genetic counselling so they can be aware of the incidence of a disorder in their family and the potential for the disease to develop in their child. Most frequent occurring anemia in children is iron deficiency anemia (preventable). This condition is virtually eliminated in infants if all bottle-fed infants were fed iron-fortified formula for the first year. Cereal with iron-fortified types are used.
During adolescents disease reoccur because diets tends to be low in meat and green leafy vegetables which the chief dietary sources of iron. All hematologic disorder require obtaining blood specimens for diagnosis and continued testing for follow up. DISORDER OF THE RED BLOOD CELLS Most RBC disorder fall into the category of the anemias, or a reduction in the number or function of erythrocytes. Polycythemia, or an increase in the number of RBCs, can also occur and may be as dangerous to a child as a reduction in RBC production. (Polycythemia Vera) 1. Normochromic, Normocytic Anemia Marked by impaired production of erythrocytes by the bone marrow, or by abnormal or uncompensated loss of circulating RBCs, as with acute hemorrhage. The RBCs are normal in both color and size, but there are simply too few of them. Acute Blood-Loss Anemia Trauma such as MVA with internal bleeding Acute nephritis in which blood is lost in the urine In newborn disorder placenta previa premature separation of the placenta maternal-fetal or twin to twin transfusion trauma to the cord or placenta Intestinal parasites Children are in shock from acute blood loss and appear pale. Tachycardia Tachypnea Sternal retractions Cyanosis Acute Blood-Loss Anemia Oxygen therapy is ineffective because they lack RBCs to transport and use the oxygen. Infants become lacking energy and inactive. This type of blood loss anemia generally is transitory because sudden reduction in available oxygen stimulates the release of erythropoietin from the kidney and a regeneration response in the bone marrow. Increase count of reticulocytes, evidence that the bone marrow is trying to increase production of erythrocytes to meet the sudden shortage. Anemia of Acute Infection Acute infection or inflammation, especially in infants, may lead to increased destruction of erythrocytes and therefore to decreased erythrocyte levels. Common condition include osteomylitis, ulcerative colitis, and advanced renal disease. Anemia of Renal Disease Loss of function in kidney cells, and this causes an accompanying decrease in erythropoietin production. Thereby decreasing the production of RBC in the bone marrow. Administration of recombinant human erythropoietin can increase RBC production and correct the anemia, but not the renal disease. Anemia of Neoplastic Disease Malignant growths such as leukemia or lymphosarcoma result in normochromic, normocytic anemias because invasion of bone marrow by proliferating neoplastic cells impairs RBC production. Aplastic Anemias Results from depression of hematopoietic activity in the bone marrow. Affects the formation and development of WBCs, platelets, and RBCs. Types: CONGENITAL APLASTIC ANEMIA
Fanconis Syndrome Skeletal and Renal Abnormalities Hypogenitalism Short stature Pancytopenia reduction of all blood cell components ACQUIRED APLASTIC ANEMIA Decreased bone marrow production that can occur if a child is exposed excessively to radiation, drugs, or chemicals known to cause bone marrow damage. (Chloramphenicol , Sulfonamides, arsenic, hydantoin, benzene, or quinine.) Exposure to insecticides also may cause severe bone marrow dysfunction. Chemotherapeutic Drugs Serious infection (meningococcal pneumonia) Assessment of Aplastic Anemia Lower RBC count (Anemia) Decreased Platelets (Thrombocytopenia) Decrease WBCs (Leukopenia) Cardiac Decompensation Ask about any exposure to drugs or chemicals or recent infection. Bone marrow samples will show a reduced number of blood elements. (Fatty tissues) Therapeutic Management The best therapy for both congenital aplastic anemia and acquired anemia is STEM CELL Transplantation. Suppression of T lymphocytes dependent autoimmune response with antithymocyte globulin (ATG) or cyclosporine or transfusion of new blood elements. Blood transfusion of packed RBC and platelets to maintain adequate blood elements. Oral corticosteroids (Prednisone) Testosterone to stimulate RBC growth may be tried. NURSING DIAGNOSIS AND RELATED INTERVENTIONS Nursing diagnosis #1 Risk for infection related to dramatic decrease in number of WBCs Outcome Evaluation: Temperature remains below 100 *F (38.0*C) axillary Symptoms of infection such as cough, vomiting, or diarrhea are absent. Exposure to other children must be limited as long as WBC production is inadequate to prevent infection. Remind parents of the signs and symptoms of infection and advise them to come for treatment promptly if the child shows any of these signs. Nursing diagnosis #2 Risk for disturbed body image related to changed appearance occurring as medication side effect. Outcome Evaluation: Child states s/he is a worthwhile person Does not appear to be excessively shy or reluctant to interact with peers. Children who receive corticosteroids such as prednisone to suppress the immune response almost always experience some of the side effects, such as cushingoid appearance, hirsutism, hypertension, and marked weight gain. Masculinizing effects Facial body hair Acne Deeping of voice *Due to medication but fade when the medication is withdrawn.
Adolescents may have an especially difficult time accepting weight gain and increased acne. They need a chance to express their feelings about their changed appearance. Reinforce and emphasize positive attributes.
Nursing Diagnosis #3 Risk for injury related to ineffective blood clotting mechanisms secondary to inadequate platelet formation. Outcome Evaluation: Exhibits no ecchymotic skin areas, gingival bleeding, or epistaxis; stools are negative for occult blood. Inadequate platelet formation interferes with blood coagulation, placing a child at risk for bleeding. Some techniques for reducing bleeding due to inadequate platelet formation include: Limit number of blood drawing procedures Apply pressure to any punctured site for a full 5 minutes before applying a bandage. Minimize use of adhesive tape to the skin. Pad side and crib rails to prevent bruising. Protect IVF site. Administer medication orally or intravenously Assess child diet for foods that can be chew without irritation. Urge the child to use a soft toothbrush. Check toys for sharp corners. Assess the need for routine blood pressure determinations. Tight cuffs could lead to petechiae Distract the child from rough play; suggest stimulating but quiet activities to minimize risk for injury. Keep record of blood drawn; do not draw extra amounts Just in case so children do not become more anemic. Hypoplastic Anemias Onset of hypoplastic anemia is insidious, and it must be differentiated from iron-deficiency anemia. In IDA, blood cells appear hypochromic and microcytic; in hypoplastic anemia, they are normochromic and normocytic but few in number. Congenital Hypoplastic Anemia (Blackfan-Diamond Syndrome) is a rare disorder that shows symptoms as early as the first 6 to 8 months of life. Affects both sexes No changes in the leukocytes or platelets occur. Show increased erythropoiesis with corticosteroid therapy. Is a chronic condition, however approximately one fourth of affected children undergo spontaneous permanent remission before age 13 years. Acquired Hypoplastic Anemia form is caused by infection with parvovirus, the infectious agent of fifth disease . The reduction or RBC is transient, so no therapy is necessary. Hypersplenism any condition in which the cellular components of the blood or platelets are removed at an abnormally high rate by the spleen. If the spleen is enlarged and functioning abnormally, blood cells pass through more slowly, with more cells being destroyed in the process. This increased destruction of RBCs can cause anemia and may lead to pancytopenia (deficiency of all cell elements of blood). DISORDER OF THE RED BLOOD CELLS 2. Normochromic, Normocytic Anemia Hypersplenism Therapeutic Management
Treating the underlying spleenic disorder, including possible splenectomy Summary of NORMO Chromic/Cytic Anemia Acute Blood-Loss Anemia Anemia of Acute Infection Anemia of Renal Disease Anemia of Neoplastic Disease Aplastic Anemia Hypoplastic Anemia Hypersplenism 3. Hypochromic Anemias When hemoglobin synthesis is inadequate, the erythrocytes appear pale (hypochromia). Increasing central pallor of hemoglobin. the red blood cells will also be small (microcytic), leading to substantial overlap with the category of microcytic anemia IRON DEFICIENCY ANEMIA Most common anemia of infancy and childhood, girls who are menstruating, overweight teenagers Occurs when intake of dietary iron is inadequate thereby preventing proper hemoglobin formation. RBCs are hypocytic hypochromic CAUSES IN INFANTS Infants diet lacks sufficient iron. Infants of low birth weight Pregnant mother with IDA Infants born with structural defects of the gastrointestinal system. CAUSES IN OLDER CHILDREN Due to GIT lesions, such as polyps, ulcerative colitis, crohns disease, protein-induced enteropathies, parasitic infestation, or frequent epistaxis. Girls menstruation Diet, and overconsumption of snack food low in iron. ASSESSMENT Pale mucous membrane Cardiomegaly Enlarged Spleen Poor muscle tone and reduced muscle activity Laboratory shows: Decrease Hgb and Hematocrit level RBCs are microcytic and hypochromic and possibly poikilocytic with low corpuscular volume. Therapeutic Management: Focuses on the treatment of the underlying cause Sources of gastrointestinal bleeding must be ruled out. Diet must be rich in iron and should contain extra vitamin C. Iron compounds such as ferrous sulfate for 4-6 weeks is the drug of choice. CHROMIC INFECTION ANEMIA Acute infection interferes with RBC production, producing a normochromic, normocytic anemia. When infections are chronic, anemia of a hypochromic, microcytic type occurs. This is probably caused by impaired iron metabolism as well as impaired RBC production. MACROCYTIC (MEGALOBLASTIC) ANEMIAS ANEMIA OF FOLIC ACID DEFICIENCY A deficiency of folic acid combined with vitamin C deficiency produces an anemia in which the erythrocytes are abnormally large. There is accompanying neutropenia and thrombocytopenia Food high in folate: Dark green leafy vegetables
Dried beans and peas (legumes) Citrus fruits and juices PERNICIOUS ANEMIA (VITAMIN B12 DEFICIENCY) Results from deficiency or inability to use the Vitamin B12. Lack of intrinsic factor in the intestines is the major common cause. Vitamin B12 found primarily in animal origin, including cows milk and breast milk. Treatment: Injectable Vitamin B12. The child appears pale, anorexic, irritable, with chronic diarrhea. Tongue appears smooth and beefy red due to papillary atrophy. Neuropathologic findings such as ataxia, hyporeflexia, paresthesia, and a positive Babinski reflex are less noticeable than in adults. If due to intrinsic factor life long administration of monthly IM injections of intrinsic factor. Hemolytic Anemias CONGENITAL SPHEROCYTOSIS Is a hemolytic anemia that is inherited as an autosomal dominant trait. The cell are small and defective, apparently due to abnormalities of the protein of the cell membrane that make them unusually permeable to sodium. The lifespan of the erythrocytes is diminished. This disease may be noticed shortly after birth. Hemolysis may appears to occur in the spleen, apparently from excessive absorption of sodium into the cell. The abnormal cells, ruptures, and is destroyed. Chronic jaundice and splenomegaly develop. The treatment is generally splenectomy at 5 to 6 years. GLUCOSE-6-PHOSPHATE DEHYDROGENASE DEFICIENCY Lack of enzyme results in premature destruction of RBCs. The disease is transmitted as a sex-linked recessive traits. Most frequently in children of African-American, Asia, Sephardic Jewish, and Mediterranean descent. Most individuals with G6PD deficiency are asymptomatic. DISORDER OF THE RED BLOOD CELLS Two identifiable forms CONGENITAL NONSPHEROCYTIC hemolytic anemia have hemolysis, jaundice, and splenomegaly and may have aplastic crises. DRUG INDUCED form in which the blood patterns are normal until the child is exposed to fava beans or drugs such as antipyretics, sulfonamides, antimalarials, and napthaquinolones, acetylsalicylic acid (aspirin) A blood smear will show Heinz Bodies is an oddly shaped particles in RBCs,. The degree of RBC destruction depends on the drug and the extent of exposure to it. The child may have accompanying fever and back pain. Occasionally a newborn is seen with marked hemolysis because the mother ingested an initiating drug during pregnancy. Drug induced hemolysis usually is self-limiting, and blood transfusions are rarely necessary. G6PD deficiency may be diagnosed by a rapid enzyme screening test or electrophoretic analysis of RBCs. SICKLE-CELL ANEMIA Is the presence of abnormally elongated shaped RBC. An autosomal recessive inherited disorder on the beta chain of hemoglobin Sickling of RBC that halts blood flow to the tissue distal to the blockage. Asymptomatic to newborn. Chorionic villi sampling or biopsy and amniocentesis means of diagnosing prenatally. Child Assessment Hemoglobin electrophoresis is used to diagnose sickle-anemia at birth from the few red cells that have already converted to their adult form.
After six months child begin to show signs of fever and anemia, stasis of blood and infarction in any body part, leading to local disease. Some infants swelling in the hands and feet due to aseptic infarction. Slight build children with long arms and legs. Protruding abdomen in children Prone to infection. Adult Assessment: In adults spleen size may reduced. Pnuemoccocal meningitis, and salmonella-induced osteomyelitis becomes frequent illness, cirrhosis, kidney function decreased. The sclereae are generally. Priapism Sickle Cell Crisis: Sudden severe onset of sickling. Vaso-occlusive crisis - Occur when a child has an illness causing dehydration or a respiratory infection that results in lowered oxygen exchange and lowered arterial oxygen level, or after strenuous exercise. Symptoms are sudden, severe, and painful. Aseptic necrosis of the head of the femur or humerus with increased joint pain may occur. Laboratory reports Hgb level below 6 to 8 g/100ml WBC is elevated to 12,000 to 20,000/mm3 Bilirubin and reticulocytes levels are increased CVA and renal involvement. Acute Chest syndrome leading to death Sequestration Crisis Spleenic Sequestration of RBCs Hyperhemolytic Crisis Increased destruction of RBC Megaloblastic Crisis Folic acid and Vitamin B deficiency Aplastic Crisis Severe sudden decrease in RBC Therapeutic Management Three primary needs: Pain relief, adequate hydration, and oxygenation Hydroxyurea, an antineoplastic agent that has the potential to increase the production of hemoglobin F. Drug may cause anorexia. Nursing Diagnosis Ineffective tissue perfusion related to generalized infarcts due to sickling. Outcome Evaluation Normal RR ABG at acceptable level Normal O2 saturation (O2 cannula) Urine output greater than 1mL/kg/h Nursing Management O2 via nasal cannula Monitor the flow rate carefully Use pulse oximetry to evaluate oxygen saturation levels. Encourage bed rest Relieve the pain and reduce oxygen expenditure. It is important to maintain accurate intake and output. Monitor urine specific gravity and hematuria. Nursing Diagnosis
Ineffective health maintenance related to lack of knowledge regarding long-term needs of child with sickle-cell anemia.
Outcome Evaluation Parent accurately describes disease process and identifies special precautions necessary to prevent sickle-cell crisis. In children, episodes of sickling grow less severe as a child reaches adolescence. Children who receive blood transfusion should not be given supplementary iron or iron fortified formula or vitamins or they may receive too much iron; high levels or excess iron are deposited in the body tissues (Hemochromatosis) Need to be followed at regular health care visits. Receive childhood immunization THALASSEMIAS Autosomal recessive anemias associated with abnormalities of the beta chain of adult hemoglobin. Most common in Mediterranean population. Thalassemia is a quantitative problem of too few globins synthesized. THALASSEMIA MINOR (HETEROZYGOUS BETA-THALASSEMIA) A mild form of this anemia, produce both defective beta hemoglobin and normal hemoglobin. RBC count is normal but the hemoglobin concentration will be decreased 2 -3 g/100mL below normal levels. The blood cells are moderately hypochromic and microcytic because of the poor hemoglobin formation. Children may have no symptoms other than pallor. No treatment , and life expectancy is normal. They should not receive a routine iron supplement because their inability to incorporate it well into hemoglobin may cause them to accumulate too much iron. THALASSEMIA MAJOR (HOMOZYGOUS BETA-THALASSEMIA) Also called Cooleys anemia or Mediterranean anemia Is a beta chain hemoglobin defect, symptoms do not become apparent until the childs fetal hemoglobin has largely been replaced by adult hemoglobin during the second half of the first year of life. Effects of thalassemia major on body are the following: Over stimulation of bone marrow leads to increased facial-mandibular growth Bronze-colored from hemosiderosis and jaundice Splenomegaly Cirrhosis and cholelithiasis Destruction of islet cells and diabetes mellitus Failure from circulatory overload THALASSEMIAS THALASSEMIA MAJOR (HOMOZYGOUS BETA-THALASSEMIA) Assessment: To maintain a functional level of hemoglobin, the bone marrow hypertrophies in an attempt to produce more RBCs. This may cause pain. As bone marrow become hyperactive, this characteristic change in the shape of the skull (parietal and frontal bossing) and protrussion of the upper teeth, with marked malocclusion. The base of the nose may be broad and flattened The eye may be slanted with an epicanthal fold as in Trisomy 21. THALASSEMIAS THALASSEMIA MAJOR (HOMOZYGOUS BETA-THALASSEMIA) Assessment:
An xray of bone shows marked osteoporotic tissue, possibly resulting to fracture. Hepatosplenomegaly due to excessive iron deposits and fibrotic scarring in the liver and the spleens increased attempts to destroy defective RBCs. Abdominal pressure form the enlarged spleen may cause anorexia and vomiting. Epistaxis is common, as is diabetes mellitus due to pancreatic hemosiderosis and cardiac dilatation with an accompanying murmur. Arrhythmias and heart failure are frequent causes of death.
THALASSEMIAS THALASSEMIA MAJOR (HOMOZYGOUS BETA-THALASSEMIA) Therapeutic Management: Digitalis, diuretics and a low-sodium diet may be prescribed to prevent hearth failure, and myocardial fibrosis. Transfusion of PRBCs every 2 -4 weeks to maintain hemoglobin level. Splenectomy may become necessary to reduce discomfort and also to reduce the rate of RBC hemolysis and the number of transfusion needed. Bone marrow transplantation can offer a cure. With treatment the over all prognosis is improving but still grave. THALASSEMIAS AUTOIMMUNE ACQUIRED HEMOLYTIC ANEMIA Occurs when antibodies directed against the person's own red blood cells (RBCs) cause the RBCs to burst (lyse), leading to insufficient plasma concentration. Occur at any age with idiopathic origin. Although the disorder may be associated with malignancy, viral infections, or collagen diseases. Child may recently have had an upper respiratory infection, measles, or varicella virus infection. THALASSEMIAS Assessment: Onset is insidious. Low grade fever, anorexia, lethargy, pallor, and icterus from release of indirect bilirubin form the hemolyzed cells. Stools and urine appear dark because excess bilirubin is being excreted. Some children the illness begins abruptly with high fever, hemoglobinuria, marked jaundice, and pallor. Liver and spleen may be enlarged. THALASSEMIAS Laboratory findings reveals: RBCs are extremely small and round (spherocytosis), reticulocytes count is increased, direct coombs test is positive, indicating the presence of antibodies attached to red cells. Hemoglobin levels may fall as low as 6g/100mL. THALASSEMIAS Therapeutic Management: In some children, the disease process runs a limited course and no treatment is necessary. In others, a single blood transfusion may correct the disturbance. For this children, it is difficult to cross-match blood for transfusion because the red cell antibody tends to clump or agglutinate all blood tested. If crossmatching is impossible, the child may be given type O Rh-negative blood. THALASSEMIAS If the anemia is persistent, corticosteriod therapy to reduce the immune response is generally effective, increasing the RBC count and hemoglobin count. For some children stronger immunosuppressive agents (cyclophosphamide [Cytoxan] or azathioprine [imuran]) are necessary to reduce anti body formation. If these are non effective, splenectomy may be necessary. POLYCYTHEMIA
Is an increase in number of RBCs. The condition results from increased erythropoiesis, which occurs as a compensatory response to insufficient oxygenation of the blood in order to help supply more oxygen to body cells. Chronic pulmonary disease and congenital heart disease are the major reasons for Polycythemia in children. It may also occur form lower oxygen level maintained during intrauterine life in newborns or with transfusion at birth (one twin receives excess blood and while a second twin is anemic). Plethora - marked reddened appearance of the skin. RBC are macrocytic and hemoglobin content is high. Treatment of Polycythemia involves treatment of the underlying cause. Because of the high blood viscosity from so many crowded blood cells. CVA or emboli may occur. The risk increase particularly if the child becomes dehydrated, such as with fever or during surgery. Exchange transfusion to reduce the RBC count may be necessary. Neutropenia Reduced number of white blood cells Neutrophilia Increased number of circulating white blood cells, primarily neutrophils. Leukemia Uncontrolled proliferation of white blood cells Eosinophilia Increased number of eosinophils Lymphocytosis Increased number of lympocytes
DISORDER OF THE BLOOD COAGULATION PLATELETS In irregularly shaped disk like cytoplasmic fragment of a megakaryocyte that is shed in the marrow sinus and subsequently found in the peripheral blood where it functions in clotting. A platelet contains granules in the central part (granulomere) and, peripherally, clear protoplasm (hyalomere), but no definite nucleus; is about one-third to one-half the size of an erythrocyte. PURPURAS Refers to a hemorrhagic rash or small hemorrhages in the superficial layer of the skin. Types Idiophatic Thrombocytopenic Purpura Henoch-Schonlein Syndrome Idiophatic Thrombocytopenic Purpura Is the condition of having an abnormally low platelet count of no known cause. ITP appear to be related to the production of antibodies against platelets or splenic macrophages. Multiple bleeding . Fatal complication: Subarachoid or intracerebral hemorrhage Lower gastrointestinal bleeding Treatment: Oral prednisone Platelet infusion Anti-D Nursing precutions Avoid salicylates or ibuprofen. Vaccination against viral disease of childhood to prevent rubella, rubeola, varicella. DISORDER OF THE BLOOD COAGULATION
Nursing Diagnosis Health-seeking behaviors related to injury-prevention measures. Outcome evaluation. Parents state precautions they will take to reduce possibility of bleeding. Repeat correct dose and timing of medication therapy Child skin is free from ecchymotic areas. Plate count increase to normal values. DISORDER OF THE BLOOD COAGULATION Nursing Diagnosis Risk for compromised family coping related to diagnosis of childs illness Outcome evaluation. Parents state they understand the nature of their childs illness Identified ways to carry out daily activities despite the ill.
Henoch-Schonlein Syndrome Also called anaphylactoid purpura Caused by increased vessel permeability No definite allergic correlation can be identified, it is generally considered to be a hypersensitivity reaction to an invading allergen. Frequent in children between 2-8 years old. Assessment Purpura on the buttocks, posterior thighs, and extensor surface of the arms and legs. Tip of the ear Joints are tender and swollen GIT symptoms Hematuria Therapeutic Management: Oral corticosteroid Mild analgesics Nose and throat cultures should be rule out. Urine should be assessed for protein and glucose Disease runs a course of 4-6 weeks. Complication: Chronic nephritis DISORDER OF THE BLOOD COAGULATION DISSEMINATED INTRAVASCULAR COAGULATION Is an acquired disorder of blood clotting that results from excessive trauma or some similar underlying stimulus. DIC leads to the formation of small blood clots inside the blood vessels throughout the body. Common in the critically ill patient. DISORDER OF THE BLOOD COAGULATION Assessment: Uncontrolled bleeding Ecchymoses and petechiae Toes and fingers are pale Cyanotic Mottled and feel cold Laboratory Test: Thrombocytopenia Large platelets on blood smear Prolonged prothrombin and partial thromboplastin times Low serum fibrinogen levels (Less than 100mg/100ml) Elevated fibrin split products Therapeutic Management: IV heparin
Blood transfusion (Fresh frozen plasma, platelets, or fibrinogen may be administered.) With adequate therapy, the results of blood coagulation studies will return to normal. If renal and brain cells were damaged from occluded capillaries, permanent injury to these areas may result. Nursing Diagnosis: Deficient knowledge about clotting disorder related to its paradoxical nature. Outcome Evaluation: Client or parents state nature of illness and proposed therapy State sign and symptoms of disease Verbalized understanding of treatments The parents understand the administration of heparin. HEMOPHILIAS Is an inherited interference with blood coagulation. There are numerous hemophilia types, each involving deficiency of a different blood coagulation factor. Haemophilia A (clotting factor VIII deficiency) is the most common form of the disorder, occurring at about 1 in 5,00010,000 male births. Signs and symptoms Characteristic symptoms vary with severity. In general symptoms are internal or external bleeding episodes, which are called "bleeds Complications Deep internal bleeding Joint damage Transfusion transmitted infection Intracranial haemorrhage NURSING DIAGNOSIS: Parental health-seeking behaviors related to strategies for protecting the child from injury OUTCOME EVALUATION: Free from ecchymosis area Epistaxis is absent Blood pressure is within age appropriate parameters. Swelling or warmth at joints is absent. NURSING DIAGNOSIS: Pain related to joint infiltration by blood OUTCOME EVALUATION: Child state that the pain is at a tolerable level. Immobilization of the affected joint helps to decrease bleeding and also provides relief. (As soon as acute episode has halted perform Passive range of motion as ordered to maintain function. NURSING DIAGNOSIS: Risk for interrupted family processes related to fears regarding childs prognosis and long term nature of illness. OUTCOME EVALUATION: Family members voice their fear regarding illness State that they can cope despite stress level Demonstrate positive coping response.
You might also like
- Diagnosing Anemia in Neonates An Evidence-Based ApproachDocument13 pagesDiagnosing Anemia in Neonates An Evidence-Based Approacharmando salvador100% (1)
- 2-step ABG interpretationDocument3 pages2-step ABG interpretationbarbaraNo ratings yet
- Ams 11Document702 pagesAms 11CrazyNo ratings yet
- Chapter 39 - Fluid, Electrolyte, and Acid-Base BalanceDocument41 pagesChapter 39 - Fluid, Electrolyte, and Acid-Base BalanceMary Singleton100% (1)
- 353 Med Terminology PDFDocument5 pages353 Med Terminology PDFNicole NicholsonNo ratings yet
- Medical Terminology Worksheet 1Document3 pagesMedical Terminology Worksheet 1Mayflor MansayonNo ratings yet
- Gastrointestinal Anatomy and Physiology: The EssentialsFrom EverandGastrointestinal Anatomy and Physiology: The EssentialsJohn F. ReinusNo ratings yet
- Essentialism Core CurriculumDocument8 pagesEssentialism Core CurriculumfLOR_ZIANE_MAENo ratings yet
- Sample Chapter 8.1Document25 pagesSample Chapter 8.1Adel Hassan100% (1)
- RBC morphology and associated cell types, pathologies, and parametersDocument2 pagesRBC morphology and associated cell types, pathologies, and parametersMiaoNo ratings yet
- Ives ScrapbookDocument84 pagesIves Scrapbookniknab@gmail.comNo ratings yet
- Immune Response: Cell Biology and Its Application BI-1202Document35 pagesImmune Response: Cell Biology and Its Application BI-1202Eriani Wulandari100% (1)
- AP Bio animal defensesDocument5 pagesAP Bio animal defensesancientblackdragon0% (1)
- NEURO2 1.02C Hemorrhagic Stroke - Dr. HiyadanDocument2 pagesNEURO2 1.02C Hemorrhagic Stroke - Dr. HiyadanAra Diocos100% (1)
- EYE PATHOLOGIES REVEALEDDocument11 pagesEYE PATHOLOGIES REVEALEDDranreb Berylle MasangkayNo ratings yet
- Circulatory SystemDocument2 pagesCirculatory SystemcatchivanNo ratings yet
- Disorders of Acid Base BalanceDocument1 pageDisorders of Acid Base BalanceLyn Domingo EllaquezNo ratings yet
- Perioperative Nursing Core ConceptsDocument67 pagesPerioperative Nursing Core ConceptsYucef Bahian-AbangNo ratings yet
- Pediatric Ulcerative Colitis: Diagnosis and Management ChallengesDocument2 pagesPediatric Ulcerative Colitis: Diagnosis and Management ChallengesicoanamareNo ratings yet
- ThrombocytopeniaDocument1 pageThrombocytopeniaanum786110No ratings yet
- 6.3 Defence Against Infectious DiseaseDocument43 pages6.3 Defence Against Infectious DiseaseAlacrity Xenoion SpadesNo ratings yet
- IMMUNE SYSTEM Notes MidtermsDocument5 pagesIMMUNE SYSTEM Notes MidtermsAdiel Calsa100% (1)
- Ap Cell Tour 1 ProteinDocument28 pagesAp Cell Tour 1 Proteinapi-235744933100% (1)
- Immunology & Oncology Review 2Document99 pagesImmunology & Oncology Review 2Melchor Felipe SalvosaNo ratings yet
- MS Final 46 Blood or Lymphatic DisorderDocument4 pagesMS Final 46 Blood or Lymphatic DisorderZachary T Hall0% (1)
- Family Medicine M3 Clerkship: Hypertensive Disorders GuideDocument35 pagesFamily Medicine M3 Clerkship: Hypertensive Disorders GuideJT ThomasNo ratings yet
- 4.2 ImmunodeficiencyDocument11 pages4.2 ImmunodeficiencyJohn Anthony de GùzmanNo ratings yet
- Rayneilda Eleana Siew MLT U29 Unit Makmal Patologi Hospital Nukleus WP LabuanDocument17 pagesRayneilda Eleana Siew MLT U29 Unit Makmal Patologi Hospital Nukleus WP LabuanValentine Brokenz Saintz100% (1)
- QuizzesDocument328 pagesQuizzesDaisyrie Manuel Barro100% (2)
- Medical Surgicl NursingDocument107 pagesMedical Surgicl NursingRitamariaNo ratings yet
- Acute Leukemias: Clinical Pharmacy Iv Bachelor of PharmacyDocument43 pagesAcute Leukemias: Clinical Pharmacy Iv Bachelor of PharmacyMuhammad Reza100% (2)
- Ebook ReviewerDocument203 pagesEbook ReviewerSheryl Nishmae Bernardo SantosNo ratings yet
- Urinalysis PDFDocument56 pagesUrinalysis PDFTio AjhaNo ratings yet
- Increased Intracranial Pressure and Monitoring Site PDFDocument21 pagesIncreased Intracranial Pressure and Monitoring Site PDFSari RakhmawatiNo ratings yet
- Blood Flashcards - QuizletDocument12 pagesBlood Flashcards - QuizletJay Leheri100% (1)
- Bacterial Flash Cards (Part 1 of 4)Document25 pagesBacterial Flash Cards (Part 1 of 4)Nafis Shamsid-DeenNo ratings yet
- CH 18 Endo F 2017Document152 pagesCH 18 Endo F 2017JuliaNo ratings yet
- Drug Calculations 2015Document35 pagesDrug Calculations 2015Anonymous DWMeAjhD1cNo ratings yet
- Anti - Infectives AgentsDocument83 pagesAnti - Infectives AgentsRhien Yrah P. CabalongaNo ratings yet
- EndocrineDocument23 pagesEndocrinensvickneswaranNo ratings yet
- NR304 Neurological Study GuideDocument10 pagesNR304 Neurological Study GuideStephanieNo ratings yet
- The Six Step Method of Interpreting EcgsDocument3 pagesThe Six Step Method of Interpreting EcgsSivakumar Gounden100% (1)
- Pharmacology Quick HitsDocument6 pagesPharmacology Quick HitsHuma Hameed DogarNo ratings yet
- Hematology summary guideDocument91 pagesHematology summary guidePeter Shirima100% (1)
- Diabetes Mellitus: Dr. Sajid Abbas JaffriDocument37 pagesDiabetes Mellitus: Dr. Sajid Abbas JaffriMaham ZarrinNo ratings yet
- Vitamins Table with Functions and Deficiency SymptomsDocument3 pagesVitamins Table with Functions and Deficiency SymptomsthomasqilNo ratings yet
- HeartMurmursExplained SystolicDiastolicManeuversDocument41 pagesHeartMurmursExplained SystolicDiastolicManeuversurtikikeNo ratings yet
- CH 39 Acid-Base ElectrolyteDocument16 pagesCH 39 Acid-Base ElectrolyteJonathan EdieNo ratings yet
- Hepatobiliary Disorders: Katrina Saludar Jimenez, R. NDocument42 pagesHepatobiliary Disorders: Katrina Saludar Jimenez, R. NKatrinaJimenezNo ratings yet
- Medical MneumonicsDocument139 pagesMedical MneumonicsdrtpkNo ratings yet
- Man Meets Microbes: An Introduction to Medical MicrobiologyFrom EverandMan Meets Microbes: An Introduction to Medical MicrobiologyNo ratings yet
- Anaerobic Infections in HumansFrom EverandAnaerobic Infections in HumansSydney FinegoldRating: 5 out of 5 stars5/5 (1)
- Microcirculation as Related to ShockFrom EverandMicrocirculation as Related to ShockDavid SheproNo ratings yet
- Ion Channels in Health and DiseaseFrom EverandIon Channels in Health and DiseaseGeoffrey S. PittNo ratings yet
- Coughing, A Simple Guide to The Condition, Treatment and Related ConditionsFrom EverandCoughing, A Simple Guide to The Condition, Treatment and Related ConditionsNo ratings yet
- Coping Mechanisms of The Third Year and Fourth Year Student Nurses of Bukidnon State UniversityDocument51 pagesCoping Mechanisms of The Third Year and Fourth Year Student Nurses of Bukidnon State UniversityfLOR_ZIANE_MAENo ratings yet
- ChapDocument57 pagesChapfLOR_ZIANE_MAENo ratings yet
- Patient Comfort Assessment GuideDocument6 pagesPatient Comfort Assessment GuidefLOR_ZIANE_MAENo ratings yet
- CHF Patient Education Book PDFDocument29 pagesCHF Patient Education Book PDFfLOR_ZIANE_MAENo ratings yet
- First To Third Year LevelsDocument7 pagesFirst To Third Year LevelsfLOR_ZIANE_MAENo ratings yet
- Health Teachings On CHFDocument6 pagesHealth Teachings On CHFfLOR_ZIANE_MAENo ratings yet
- Top Performing Medical Schools in The PhilippinesDocument2 pagesTop Performing Medical Schools in The PhilippinesfLOR_ZIANE_MAENo ratings yet
- Nurse ArticleDocument1 pageNurse ArticlefLOR_ZIANE_MAENo ratings yet
- Top Performing Medical Schools in The PhilippinesDocument2 pagesTop Performing Medical Schools in The PhilippinesfLOR_ZIANE_MAENo ratings yet
- Teaching Learning GuideDocument3 pagesTeaching Learning GuidefLOR_ZIANE_MAENo ratings yet
- Pain AssessmentDocument1 pagePain AssessmentfLOR_ZIANE_MAENo ratings yet
- Upper Respiratory Infection OverviewDocument4 pagesUpper Respiratory Infection OverviewfLOR_ZIANE_MAENo ratings yet
- What Are OrganophosphatesDocument8 pagesWhat Are OrganophosphatesfLOR_ZIANE_MAENo ratings yet
- Tri AGEDocument10 pagesTri AGEfLOR_ZIANE_MAENo ratings yet
- Map of Emotional Intelligence in Brain Regions CompletedDocument10 pagesMap of Emotional Intelligence in Brain Regions CompletedfLOR_ZIANE_MAENo ratings yet
- Bronchial Asthma - Patient Expectations and The Role in Asthma CareDocument2 pagesBronchial Asthma - Patient Expectations and The Role in Asthma CarefLOR_ZIANE_MAENo ratings yet
- Anatomy of The Eye EYE: Extaocular StructuresDocument5 pagesAnatomy of The Eye EYE: Extaocular StructuresfLOR_ZIANE_MAENo ratings yet
- Nystatin DrugstudyDocument2 pagesNystatin DrugstudyfLOR_ZIANE_MAENo ratings yet
- Alterations in Ocular MovementsDocument3 pagesAlterations in Ocular MovementsfLOR_ZIANE_MAENo ratings yet
- Mild PreecDocument4 pagesMild PreecfLOR_ZIANE_MAENo ratings yet
- Pathophysiology of Enteric FeverDocument4 pagesPathophysiology of Enteric FeverfLOR_ZIANE_MAENo ratings yet
- Tawa TawaDocument5 pagesTawa TawafLOR_ZIANE_MAENo ratings yet
- BSU-CON Case Study on Breast Cancer Stage IIIBDocument106 pagesBSU-CON Case Study on Breast Cancer Stage IIIBfLOR_ZIANE_MAENo ratings yet
- Tawa TawaDocument5 pagesTawa TawafLOR_ZIANE_MAENo ratings yet
- Age and PcapDocument2 pagesAge and PcapfLOR_ZIANE_MAENo ratings yet
- Congestive Heart Failure OverviewDocument15 pagesCongestive Heart Failure OverviewfLOR_ZIANE_MAENo ratings yet
- Penetrating Abdominal TraumaDocument1 pagePenetrating Abdominal TraumafLOR_ZIANE_MAENo ratings yet
- Etiology and Pa Tho PhysiologyDocument3 pagesEtiology and Pa Tho PhysiologyfLOR_ZIANE_MAENo ratings yet
- S U3 Z L0 V 0 NPMqazusy O8 XFP 48 LG 1 FKM 9 B20170320080333827Document8 pagesS U3 Z L0 V 0 NPMqazusy O8 XFP 48 LG 1 FKM 9 B20170320080333827VisaNathanNo ratings yet
- Case Studies: Case 1 Feline 8 Month Old Intact Male DSHDocument34 pagesCase Studies: Case 1 Feline 8 Month Old Intact Male DSHGuilherme Oliveira BjjNo ratings yet
- Abdon MelodyDocument4 pagesAbdon MelodyChirs Nicole CaguitlaNo ratings yet
- Chapter - 077 Hematologic DisordersDocument13 pagesChapter - 077 Hematologic DisordersClaudina CariasoNo ratings yet
- Blood Cell MorphologyDocument5 pagesBlood Cell MorphologyKIPRUTO DENNISNo ratings yet
- RBC PathologyDocument7 pagesRBC PathologyKent CruzNo ratings yet
- MCQ On Disorder of RBCS: Group (4) PresentsDocument6 pagesMCQ On Disorder of RBCS: Group (4) PresentsIrekton GGNo ratings yet
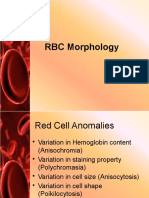
- RBC Anomalies: I. Variation in Hemoglobin ContentDocument6 pagesRBC Anomalies: I. Variation in Hemoglobin ContentMARIE NELLIE MOSTRADONo ratings yet
- Therapeutics Lilienthal PDFDocument724 pagesTherapeutics Lilienthal PDFtohnas50% (2)
- Atlas of Pediatric Peripheral Blood Smears PDFDocument52 pagesAtlas of Pediatric Peripheral Blood Smears PDFSuzy_89100% (2)
- Hematology Part 1 NotesDocument23 pagesHematology Part 1 NotesDr. Benson BenjaminNo ratings yet
- Acid Remedies in HomeopathyDocument8 pagesAcid Remedies in Homeopathyantonio andresNo ratings yet
- Currens Math For Meds Dosages and Solutions 11th Edition Curren Test BankDocument36 pagesCurrens Math For Meds Dosages and Solutions 11th Edition Curren Test Banksynechia.goblinqrs4v100% (28)
- Red blood cell abnormalities revealedDocument39 pagesRed blood cell abnormalities revealedShishir AhmedNo ratings yet
- RBC, PCV, ESR, Blood Indices ExplainedDocument5 pagesRBC, PCV, ESR, Blood Indices ExplainedUjjwal Kumar MauryaNo ratings yet
- Evaluating Cell Morphology and PlateletsDocument24 pagesEvaluating Cell Morphology and PlateletsEllya Latifah IlyasNo ratings yet
- Anemia Pathophysiology by Francis Oliveros, BSN 4Document2 pagesAnemia Pathophysiology by Francis Oliveros, BSN 4francis00090100% (1)
- FMGE DEC - 2019 (WWW - Medmutant.xyz)Document46 pagesFMGE DEC - 2019 (WWW - Medmutant.xyz)aditya jyothisNo ratings yet
- 0001 5866aDocument830 pages0001 5866aZllison Mae Teodoro MangabatNo ratings yet
- 782Document20 pages782Aarathi raoNo ratings yet
- Approach To The Adult With Anemia - UpToDate PDFDocument66 pagesApproach To The Adult With Anemia - UpToDate PDFJuliana Salerno100% (1)
- Result Reporting: Subjectively Graded As Few, Moderate, ManyDocument5 pagesResult Reporting: Subjectively Graded As Few, Moderate, ManyMemory MahwendaNo ratings yet
- (Lesson 6) RBC MorphologyDocument34 pages(Lesson 6) RBC MorphologyYfhps LnmNo ratings yet
- Prevalence of Hypochromic Microcytic Anemia in The Hematology-Oncology Department of The Donka National HospitalDocument4 pagesPrevalence of Hypochromic Microcytic Anemia in The Hematology-Oncology Department of The Donka National HospitalPremier PublishersNo ratings yet
- Pica 1992Document15 pagesPica 1992muiNo ratings yet
- Anemia: Signs and SymptomsDocument6 pagesAnemia: Signs and SymptomsHarisree SNo ratings yet