Professional Documents
Culture Documents
CHC-PC-0033: Procedure Number Version Nos
Uploaded by
Qari Ramadhan AminOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
CHC-PC-0033: Procedure Number Version Nos
Uploaded by
Qari Ramadhan AminCopyright:
Available Formats
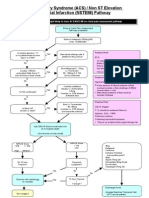
Guidelines for Management of Unstable Angina and NSTEMI 1.
Purpose
Procedure Number
Version Nos:
CHC-PC-0033
Unstable coronary lesions have a complex morphology because of ruptured plaque and superimposed thrombus. The use of antiplatelet agents and anticoagulants is aimed at stabilising these lesions. 2. Application These Guidelines is to be followed by all WCDHB clinical staff members. 3. Definitions Unstable Angina Change in pattern of angina New onset angina Pain at rest NSTEMI Elevated cardiac biomarkers (There may be other causes for this. Indicators that ischemia is the cause include typical history, ECG changes of ischaemia and regional wall abnormalities on ECHO) 4. Responsibilities 5. All WCDHB clinical staff must ensure that these Guidelines are followed correctly.
Clinical Guidelines 1.00 Risk Stratification All patients should be risk stratified. ECGs obtained during pain are particularly helpful. ST depression is more ominous than T wave changes Not only the presence of an elevated troponin, but also the magnitude of the troponin rise is an important prognostic indicator. Commonly used risk stratification tools are detailed on the following page.
Uncontrolled Document West Coast District Health Board
Guidelines for Management of Unstable Angina and NSTEMI
Procedure Number
Version Nos:
CHC-PC-0033
Short-Term Risk Of Death Or Nonfatal MI In Patients With Unstable Angina Feature High Risk (At least 1 of the following features must be present) Accelerating tempo of Ischaemic symptoms in preceding 48h Prolonged ongoing (>20 min) rest pain PCI last 6 months Prolonged (>20 min) rest angina, now resolved, with moderate or high likelihood of CAD. Pulmonary oedema, most likely related to ischaemia. New or worsening mitral regurgitation murmur S3 or new/worsening rates. Hypotension, bradycardia, tachycardia Age >75yrs Diabetes Associated syncope Associated haemodynamic instability (Systolic BP <90mmHg, cool peripheries, diaphoresis) Known poor LV function (EF <40%) Angina at rest with transient ST-segment changes >0.05mV Bundle-branch block, new or presumed new Sustained ventricular tachycardia Deep T wave inversion ( 3 min in 3 leads) Elevated troponins (e.g., TnT 0.03g/L) Intermediate Risk (No high-risk features but must have 1 of the following features) Prior MI, peripheral or cerebrovascular disease, or CABG; prior aspirin use Rest angina (<20 min or relieved with rest or sublingual nitro glycerine)
History
Character of pain
Clinical findings
Age >65-75yrs
ECG findings
T-wave inversions 0.2mV in 3 leads Pathological Q waves
Cardiac markers
2.00 TIMI Risk Score Factor Age >65 years >3 Risk Factors for IHD Prior coronary stenosis >50% >0.5mm ST deviation on ECG >2 anginal events in prior 7 days Aspirin use in prior 7 days Elevated cardiac markers Points 1 1 1 1 1 1 1
Uncontrolled Document West Coast District Health Board
Guidelines for Management of Unstable Angina and NSTEMI 3.00 Management
Procedure Number
Version Nos:
CHC-PC-0033
Management should be undertaken in consultation with DPH cardiologists. Patient should initially have continuous cardiac monitoring. Oxygen The role for routine O2 is much less clear than it was. O2 is a vasoconstrictor and as such may have detrimental effects Supplemental oxygen is indicated for patients who are hypoxic or at risk of hypoxia. For other patients a short period of O2 supplementation is reasonable during stabilisation. Aspirin Patients not on aspirin should receive 300mg of non enteric coated aspirin chewed. Continue indefinitely at 75-150 mg daily. (Patients post stenting probably should receive 300mg for the first 1/12) Morphine One study has suggested an increased mortality associated with morphine use in NSTEMI patients. There were significant problems with this trial and further study needed; in the meantime the use of morphine has been downgraded from a class 1 to a class 2a recommendation. ie. may be useful The use of IV morphine is reasonable for ongoing pain uncontrolled by anti-anginal medication. Nitrates Routinely used to control Pain, CHF and Hypertension. Initially sublingually and then topically, orally or intravenously if needed. IV nitrates should be started at 10 mcg / min (= 6ml/hr of 25mg GTN in 250ml dextrose) and titrated every 5 minutes according to symptoms and BP. Using ceiling dose is 600mcg/min (=120ml per hour). SBP should not be allowed to fall rapidly or below 100mmHg Change to an interrupted regime (oral/ topical) within 24 to 48 hrs if possible, in order to avoid tachyphylaxis. GTN should not be administered to patients who had received a phosphodiesterase inhibitor for erectile dysfunction within 24 hrs of Sildenafil or 48 hrs of Tadalafil use. The suitable time for the administration of nitrates after Vardenafil has not been determined. Beta Blockers Aggressive beta blockade is now less favoured than it was in the management of UA/NSTEMI patients. CHF/Poor LV fn is probably now a stronger indication for the use of beta blockers. It may be harmful to administer IV beta blockers to UA/NSTEMI patients who have contraindications to beta blockade, signs of HF or low-output state, or other risk factors for cardiogenic shock Usually started on admission if there are no contraindications (asthma, systolic BP <110 mmHg, heart rate <50 min or AV block.) The usual starting dose is short acting Metoprolol 25 mg tds, though 12.5mg tds may be more appropriate is there are concerns about tolerance.
Uncontrolled Document West Coast District Health Board 3
Guidelines for Management of Unstable Angina and NSTEMI
Procedure Number
Version Nos:
CHC-PC-0033
Aim for Metoprolol CR 95 mg daily by discharge but titrate slowly if there are concerns about haemodynamic stability or poor LV fn. IV Metoprolol may be reasonable for initially persistent pain that fails to settle with nitrates. Calcium Channel Blockers These are not usual first line therapy. They should be considered in patients who cannot tolerate beta blockers or in whom a combination of nitrates and beta blockers does not control symptoms. Diltiazem is the preferred agent. Initially 30mg tds then slow release preparations. Amlodipine or Felodipine may be considered especially if the patient has poor LV function. They are safer if used in combination with beta blockers (less likely to induce a tachycardia). Clopidogrel Clopidogrel should be considered for all patients who end up being admitted with UA or NSTEMI. All patients should be loaded with 300mg and continued on 75mg daily for 3 months A special authority application is needed. Heparin LMWH and in particular Enoxaparin is the preferred agent. Enoxaparin Unlike Clopidogrel the benefits of Enoxaparin are almost solely confined to patients who have or go on to have a positive troponin. Enoxaparin should be considered for all patients who have high risk features. These include ongoing pain, ECG changes and troponin leak. Standard dose is 1mg/kg SC every 12 hours. Some authorities suggest a loading dose of 30mg IV and this could be considered. Renal impairment: If the creat clearance is < 30ml/min the dosing interval should be increased to once every 24 hours. Current UA/NSTEMI guidelines do not call for a reduction in dose for the elderly. However local anecdotal evidence suggests there is a higher rate of bleeding complications in these patients and for the frail elderly it may be appropriate to reduce the dose to 0.75mg/kg. Enoxaparin should be continued for up to 8 days or the point of discharge, whichever occurs earlier. It is necessary to reverse the anticoagulant effect of Enoxaparin because of bleeding complication this may be partially achieved by the use of Protamine. (1mg of Protamine as a slow IV injection will neutralise 1mg of Enoxaparin). The response to Protamine cannot be assessed by APTT. Unfractionated Heparin The use of UFH may occasionally be preferred, usually in patients who have very severe renal impairment or who are at higher risk of bleeding and an agent that wears off quickly and can be fully reversed is preferred. Initial bolus of 60/U/kg (max 4000U) followed by infusion of 12U/kg/hr (max 1000U/hr). An APTT should be performed at 6hrs and then again once daily or 6hrs after any change in dose. Aim for an APTT of 60-80 sec. Continue the infusion for between 2 and 5 days. Hb and platelets should be monitored.
Uncontrolled Document West Coast District Health Board 4
Guidelines for Management of Unstable Angina and NSTEMI
Procedure Number
Version Nos:
CHC-PC-0033
Tirofiban Tirofiban is an intravenous platelet blocking agent (glycoprotein IIB/IIIA inhibitor) that is indicated in patient with high risk UA/NSTEMI. The drug should be used only on the advice of a Cardiologist. Tirofiban is usually reserved for high risk patients who have prolonged and recurrent symptoms despite being on all other appropriate agents, as they await angiography. As well as ongoing symptoms, features that should suggest the patient is at high risk and Tirofiban should be considered would include: Elevated troponin Large territory involved (eg wide spread ST/Twave changes across ant leads suggesting prox LAD lesion) ST depression, particularly fluctuating ST depression ST depression with hypotension and or pulmonary oedema Diabetics ACE Inhibitors (or ARB) All patients with UA/NSTEMI who have CHF, impaired LV function, hypertension or DM should be started on an ACE Inhibitor. Statins All patients with UA/NSTEMI should receive a Statin (Simvastatin 40mg) regardless of lipid levels. Target lipid levels for patients with known IHD are tol chol < 4 mmol/L and LDL < 2.0 mmol/L. Patients post CABG tot chol < 3.0 mmol/L and LDL < 2.0mmol/L. Hypertension Target BPs for UA/NSTEMI patients are 140/90 or 130/80 for those with diabetes or renal impairment. ACE Inhibitors, Beta Blockers and Thiazides are the most appropriate agents. NSAIDs NSAIDs should be stopped If it is essential to use an NSAID longer term then a non-selective agent (e.g. Naproxen) should be used. HRT HRT should be avoided. Warfarin In patients who are already on Warfarin for a pre existing condition (eg AF, mechanical valve, mural thrombus) the role of triple therapy with Aspirin, Clopidogrel and Warfarin is unclear. Judgement is required on a case by case basis. If the decision is made to use triple therapy the minimum doses for the minimum time should be used to reduce the risks of bleeding complications.
Uncontrolled Document West Coast District Health Board
Guidelines for Management of Unstable Angina and NSTEMI
Procedure Number
Version Nos:
CHC-PC-0033
Glycaemic Control / Diabetics The optimal treatment of elevated BSLs is uncertain. Unlike patients with STEMI clear guidelines do not exist. It may be appropriate to maintain BSLs less than 9 mmol/L for the first 3 days. Diabetics will gain greater benefits from the aggressive management (including revascularisation and Tirofiban) of UA/NSTEMI than non diabetics. 4.00 Invasive (PTCA) vs Conservative (medical management only) Strategies This decision should be made with the cardiologist on call. Most high risk patients (ECG changes, positive troponin, ongoing pain, diabetics) should be considered for transfer and PTCA. However there may be instances (including resource constraints) where it is reasonable to initially treat these patients conservatively. Patients with multiple co morbidities (e.g. advanced malignancy, intra cranial pathology, CAD know from previous angiography not to be amenable to revascularisation) should be considered for a conservative approach, particularly if they settle with medical management. A conservative strategy is appropriate for patients without any high risk features. Patients for whom a conservative approach is planned Patients who fail to settle should be considered for transfer and PTCA. Patients who settle should have an early ETT. This should be done prior to discharge (or failing this, within 3 to 7 days) Patients must be stable for 24 hrs before undertaking the ETT. Patients treated conservatively should be considered for an ECHO to assess LV function. Return to normal activities Appropriate advice will vary from patient to patient. Revascularised patients can return to activities sooner. Work normally 2 weeks Sexual activity normally 7-10/7 Air Travel normally 2 weeks Driving - normally 2 weeks post uncomplicated MI Lifestyle Modification / Discharge considerations Encourage smoking cessation. Aim for regular daily exercise of 30-60 min Yearly influenza vaccination Screen and treat for depression Referral to cardiac CNS for cardiac rehabilitation 6. References Non ST-Elevation Acute Coronary Syndromes: New Zealand management guidelines NZMJ 7 October 2005, Vol 118 No 1223 ACC Unstable Angina And Non-STEMI Guidelines. Executive summary. 2007;50:7:652-728 JACC
Guideline for Management of Acute Coronary Syndrome. Medical Journal of Australia Volume 184 Number 8 17 April 2006
Uncontrolled Document West Coast District Health Board 6
Guidelines for Management of Unstable Angina and NSTEMI 7. Related Documents There are no other documents related to these Guidelines Acknowledgement
Procedure Number
Version Nos:
CHC-PC-0033
These Guidelines are reproduced with the permission of Central Otago Health Services, who are the original authors of this document.
Version: Developed By:
Revision History
Authorised By: Date Authorised: Date Last Reviewed: Date Of Next Review:
1 Central Otago Health Services CQIT Committee August 2011 August 2011 August 2013
Uncontrolled Document West Coast District Health Board
You might also like
- Hypertension: DR Abdelmoniem Saeed Er SpecialistDocument41 pagesHypertension: DR Abdelmoniem Saeed Er SpecialistYousef Al-AmeenNo ratings yet
- Stroke by Dr. Amit RoyDocument32 pagesStroke by Dr. Amit RoyDr Sutanwi DasNo ratings yet
- Management of ArrhythmiasDocument4 pagesManagement of ArrhythmiasAray Al-AfiqahNo ratings yet
- Cardiology Pharmacist Guide to Acute Coronary SyndromeDocument38 pagesCardiology Pharmacist Guide to Acute Coronary SyndromeAnonymous100% (1)
- An Update Management of Acute Ischemic Stroke: SurotoDocument36 pagesAn Update Management of Acute Ischemic Stroke: SurotoShinta DianNo ratings yet
- CCU HandoverDocument9 pagesCCU Handoverapi-192342497No ratings yet
- Acute Coronary Syndromes 2015Document26 pagesAcute Coronary Syndromes 2015prototypeallhellNo ratings yet
- Fac Thrombolysis 2007Document36 pagesFac Thrombolysis 2007Tri Harjono0% (1)
- Mutt and JeffDocument8 pagesMutt and Jeffyoyo1rn100% (2)
- Hypertensive CrisisDocument7 pagesHypertensive Crisisalul847474No ratings yet
- Laporan Kasus: Myasthenia GravisDocument41 pagesLaporan Kasus: Myasthenia GravisTias DiahNo ratings yet
- TPA Protocol: Stroke in Carefully Selected PersonsDocument4 pagesTPA Protocol: Stroke in Carefully Selected PersonsJavier Gonzalez, M.D. DABEMNo ratings yet
- ThrombolyticsDocument14 pagesThrombolyticsJavier Gonzalez, M.D. DABEMNo ratings yet
- Acs 11 190524110746Document46 pagesAcs 11 190524110746Obakeng MandaNo ratings yet
- Cme Acs 2. Stemi (Izzah)Document36 pagesCme Acs 2. Stemi (Izzah)Hakimah K. SuhaimiNo ratings yet
- CHAPTER 56 - Unstable Angina and Non-ST ElevationDocument34 pagesCHAPTER 56 - Unstable Angina and Non-ST ElevationSatria WardanaNo ratings yet
- Drug Monograph XareltoDocument2 pagesDrug Monograph XareltoBenNo ratings yet
- ACS ManagementDocument24 pagesACS ManagementkalfNo ratings yet
- ACLS PharmacologyDocument6 pagesACLS PharmacologyEunice Angela Fulgueras80% (5)
- StrokeDocument22 pagesStrokeAlex GasnasNo ratings yet
- Anaesthesia For TURPDocument6 pagesAnaesthesia For TURPMutia FarinaNo ratings yet
- Advanced Cardiovascular Life Support (ACLS)Document73 pagesAdvanced Cardiovascular Life Support (ACLS)maya_fitrianaNo ratings yet
- Hypertensivecrisis: A Review of Pathophysiology and TreatmentDocument9 pagesHypertensivecrisis: A Review of Pathophysiology and Treatmentkelly johanna salas martinezNo ratings yet
- ACS-Karim AbdellatifDocument10 pagesACS-Karim AbdellatifKarim AbdellatifNo ratings yet
- Myocardial InfarctionDocument20 pagesMyocardial InfarctionRio Ramon HilarioNo ratings yet
- Ischemic Heart DiseaseDocument37 pagesIschemic Heart DiseaseAli100% (1)
- St-Segment Elevation Myocardial Infarction: PGI Barrantes, Lloyd DanielDocument28 pagesSt-Segment Elevation Myocardial Infarction: PGI Barrantes, Lloyd DanielLloyd Daniel BarrantesNo ratings yet
- Ws Ahf - Intro Apicd 2017 - EditedDocument18 pagesWs Ahf - Intro Apicd 2017 - Editedvkhen88No ratings yet
- Acute Coronary SyndromeDocument41 pagesAcute Coronary SyndromeAbdulhameed MohamedNo ratings yet
- Problem 2Document9 pagesProblem 2Chan Myae NaingNo ratings yet
- 6 - Fahad Class 6 Cardiac AnesthesiaDocument18 pages6 - Fahad Class 6 Cardiac AnesthesiaOne ClickNo ratings yet
- PENGGUNAAN OBAT PADA SISTEM CARDIOVASCULARDocument56 pagesPENGGUNAAN OBAT PADA SISTEM CARDIOVASCULARwidya vannesaNo ratings yet
- Cardiovascular Pharmacotherapy: Sutomo Tanzil Dept - of Pharmacology, Faculty of Medicine, Sriwijaya UniversityDocument44 pagesCardiovascular Pharmacotherapy: Sutomo Tanzil Dept - of Pharmacology, Faculty of Medicine, Sriwijaya UniversitydeviamufidazaharaNo ratings yet
- STEMI Case StudyDocument28 pagesSTEMI Case StudyAkbar IskandarNo ratings yet
- Main Stroke Protocol - Use For All Suspected Stroke-TIA PatientsDocument2 pagesMain Stroke Protocol - Use For All Suspected Stroke-TIA PatientsRivulet1No ratings yet
- Angina and MIDocument68 pagesAngina and MIAndrassy Twinkle AlineaNo ratings yet
- Dental care considerations for patients with heart diseaseDocument24 pagesDental care considerations for patients with heart diseaseAli ahmed0% (1)
- ACLS DrugsDocument16 pagesACLS Drugstostc100% (1)
- Acute Coronary SyndromesDocument15 pagesAcute Coronary SyndromesAnonymous noiextpGNo ratings yet
- Problems in Returned Travelers: DVT and ThromboembolismDocument14 pagesProblems in Returned Travelers: DVT and ThromboembolismMon Soe100% (1)
- Treatment of NSTE-ACSDocument4 pagesTreatment of NSTE-ACSAnuradha NanayakkaraNo ratings yet
- Management of The Patients WithDocument68 pagesManagement of The Patients WithДіна ШоріковаNo ratings yet
- ACLS MedicationsDocument31 pagesACLS MedicationsDrNorNo ratings yet
- Cardio BBDocument73 pagesCardio BBايات عبدالرحمنNo ratings yet
- ACS Final DraftDocument33 pagesACS Final Draftomcm17006No ratings yet
- Esc Acs GuidelinesDocument62 pagesEsc Acs GuidelineszakiyaNo ratings yet
- UntitledDocument62 pagesUntitledTGB LEGENDNo ratings yet
- Cardiovascular Diseases 2Document40 pagesCardiovascular Diseases 2Ali MuradNo ratings yet
- Nursing Module For Brain StrokeDocument27 pagesNursing Module For Brain StrokeziadabiakarNo ratings yet
- HUTTDocument25 pagesHUTTdrdj14No ratings yet
- QR HypertensionDocument8 pagesQR HypertensionHani NadiahNo ratings yet
- ACS NSTEMI Clinical PathwayDocument3 pagesACS NSTEMI Clinical PathwayXtiaRNo ratings yet
- No. 2 STEMI and NSTEMIDocument8 pagesNo. 2 STEMI and NSTEMIArkanelJ.ChingNo ratings yet
- Bradycardia and Tachycardia Treatment OptionsDocument31 pagesBradycardia and Tachycardia Treatment OptionscmirceaNo ratings yet
- Fast Facts for Patients: Thrombotic Thrombocytopenic Purpura: Prompt action saves livesFrom EverandFast Facts for Patients: Thrombotic Thrombocytopenic Purpura: Prompt action saves livesNo ratings yet
- Case-Based Device Therapy for Heart FailureFrom EverandCase-Based Device Therapy for Heart FailureUlrika Birgersdotter-GreenNo ratings yet
- Revascularization in Stable Coronary Artery Disease Review BMJDocument17 pagesRevascularization in Stable Coronary Artery Disease Review BMJucicardiocovid ocgnNo ratings yet
- Normal Adult 12-Lead ECGDocument2 pagesNormal Adult 12-Lead ECGIlonaNo ratings yet
- Peripheral Vascular System Anatomy Exam TechniquesDocument2 pagesPeripheral Vascular System Anatomy Exam TechniquesAngelica Mae Dela CruzNo ratings yet
- YeDocument39 pagesYeRhea RaveloNo ratings yet
- MEGACODEDocument6 pagesMEGACODESafety JNo ratings yet
- Obtaining and Interpreting EcgDocument8 pagesObtaining and Interpreting EcgAndra Elena PricopNo ratings yet
- ALS Cardiac Arrest GuideDocument1 pageALS Cardiac Arrest GuideLucian Alin DinuNo ratings yet
- Acute Chest PainDocument103 pagesAcute Chest PainYajjat GargNo ratings yet
- Isosorbide DinitrateDocument1 pageIsosorbide Dinitrate202110439No ratings yet
- Interpretasi EKGDocument81 pagesInterpretasi EKGGyna MarsianaNo ratings yet
- Aortic Valve DiseaseDocument63 pagesAortic Valve DiseaseFaridOrahaNo ratings yet
- DAFTAR PUSTAKA TENTANG PENYAKIT STROKEDocument5 pagesDAFTAR PUSTAKA TENTANG PENYAKIT STROKEWilliam WiryawanNo ratings yet
- Clinical Standards For Heart Disease 2010Document59 pagesClinical Standards For Heart Disease 2010Novita Dwi MardiningtyasNo ratings yet
- ArrhythmiaDocument21 pagesArrhythmiaBaix Furianto0% (1)
- Is The Cardiac Rehabilitation Programme Successful in Serdang Hospital: Patients' PerspectiveDocument3 pagesIs The Cardiac Rehabilitation Programme Successful in Serdang Hospital: Patients' PerspectiveAnanthankumar MunusamyNo ratings yet
- ACLS FullMapsDocument68 pagesACLS FullMapswong2689No ratings yet
- Pacemaker SyndromeDocument26 pagesPacemaker SyndromeOlga GoryachevaNo ratings yet
- Previous Question Paper 2 Cardiology PDFDocument6 pagesPrevious Question Paper 2 Cardiology PDFDeepthi D100% (1)
- Coronary Heart Disease in the Framingham StudyDocument21 pagesCoronary Heart Disease in the Framingham StudyYunlong LiuNo ratings yet
- Oral Contributions: JACC March 9, 2010 ABSTRACTS: Cardiac Arrhythmias A1Document217 pagesOral Contributions: JACC March 9, 2010 ABSTRACTS: Cardiac Arrhythmias A1Apner Calvin SuNo ratings yet
- 2020 AFIB 2020 - For WebDocument166 pages2020 AFIB 2020 - For WebHussein TfNo ratings yet
- T Wave / T TalasDocument14 pagesT Wave / T TalasLidianaBeka0% (1)
- Atrial Fibrillation CASE STUDYDocument2 pagesAtrial Fibrillation CASE STUDYChristianneMikeNo ratings yet
- Valvular Heart Disease: Mitral RegurgitationDocument33 pagesValvular Heart Disease: Mitral RegurgitationjihyooniNo ratings yet
- Susila Wahiddiyah, Alfi Ari Fahrul RizalDocument10 pagesSusila Wahiddiyah, Alfi Ari Fahrul RizalNandha PuspitaSariNo ratings yet
- Heart Sounds & Murmurs GuideDocument11 pagesHeart Sounds & Murmurs GuideTraceyNo ratings yet
- Herbesser IVDocument24 pagesHerbesser IVsuho exoNo ratings yet
- Sick Sinus SyndromeDocument12 pagesSick Sinus Syndromeb3djo_76100% (1)
- SPECIFIC OBJECTIVE: On Completion of The Class StudentsDocument15 pagesSPECIFIC OBJECTIVE: On Completion of The Class Studentsanimesh pandaNo ratings yet
- Heart Failure Diagnosis and ClassificationDocument12 pagesHeart Failure Diagnosis and ClassificationFreddy PanjaitanNo ratings yet