Professional Documents
Culture Documents
Use of Cardiovascular Magnetic Resonance For Risk Stratification in Heart Failure
Uploaded by
PUIGCOZAROriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Use of Cardiovascular Magnetic Resonance For Risk Stratification in Heart Failure
Uploaded by
PUIGCOZARCopyright:
Available Formats
Downloaded from heart.bmj.com on October 31, 2011 - Published by group.bmj.
com
Cardiomyopathy
Use of cardiovascular magnetic resonance for risk stratication in chronic heart failure: prognostic value of late gadolinium enhancement in patients with non-ischaemic dilated cardiomyopathy
Stephanie Lehrke, Dirk Lossnitzer, Michael Schob, Henning Steen, Constanze Merten, Helmut Kemmling, Regina Pribe, Philipp Ehlermann, Christian Zugck, Grigorios Korosoglou, Evangelos Giannitsis, Hugo A Katus
< Additional tables are
published online only. To view these les please visit the journal online (http://heart.bmj. com). Abteilung Innere Medizin III, Medizinische Klinik, Universitatsklinikum Heidelberg, Heidelberg, Germany Correspondence to Dr Stephanie Lehrke, Abteilung Innere Medizin III, Universitatsklinikum Heidelberg, Im Neuenheimer Feld 410, 69120 Heidelberg, Germany; stephanie.lehrke@med. uni-heidelberg.de Accepted 5 October 2010 Published Online First 20 November 2010
ABSTRACT Objective Owing to its variable clinical course, risk stratication is of paramount importance in nonischaemic dilated cardiomyopathy (DCM). The goal of this study was to investigate the long-term prognostic signicance of late gadolinium enhancement (LGE) as detected by contrast-enhanced cardiovascular magnetic resonance (CE-CMR) in patients with DCM. Design Observational cohort study. Setting University hospital. Patients 184 consecutive patients with DCM. Measurements CE-CMR was performed on a 1.5 T clinical scanner. Presence, extent and patterns of LGE were determined by two independent observers. Outcome measures Patients were followed for the composite end point of cardiac death, hospitalisation for decompensated heart failure, or appropriate implantable cardioverter debrillator discharge for a mean6SEM of 685630 days. Results LGE was detected in 72/184 patients (39%) and was associated with a lower left ventricular (LV) ejection fraction (31% (20.9e42.2%) vs 44% (33.1e50.9%), p<0.001), higher LV end-diastolic volume index (133 (116e161) ml/m2 vs 109 (92.7e137.6) ml/m2, p<0.001) and higher LV mass (80 (67.1e94.8) g/m2 vs 65.8 (55.2e82.9) g/m2, p<0.001). Patients in whom LGE was present were more likely to experience the composite end point (15/72 vs 6/112, p0.002). Receiver operating characteristic curve analysis revealed a LGE of >4.4% of LV mass as optimal discriminator for the composite end point. When entered into multivariate Cox regression analysis, LGE retained its independent predictive value, yielding an associated HR of 3.4 (95% CI 1.26 to 9). Conclusion The presence of LGE in this large DCM patient cohort is associated with pronounced LV remodelling, functional impairment and an adverse outcome. Further research is necessary to determine whether these ndings will aid the clinical management of DCM patients.
sudden cardiac death. Despite the identication of a series of factors that are associated with an adverse prognosis, such as age,4 male gender,2 degree of systolic dysfunction,5 QRS duration6 and cardiac biomarkers such as natriuretic peptides and troponins,7 risk stratication remains challenging, and better tools are necessary to identify highest risk patients, who are most likely to benet from early aggressive interventions such as the implantation of implantable cardioverter debrillators (ICDs). Cardiac MRI has become the gold standard for the assessment of cardiac function and mass.8 In addition, the administration of gadolinium contrast agents allows the detection of areas of late gadolinium enhancement (LGE). Originally used for the detection of myocardial infarction and viability assessment, different patterns of LGE have been found in a large number of cardiac diseases, including cardiomyopathies. McCrohon et al were the rst to report the presence of a mid-wall enhancement in patients with DCM, which was distinct from the LGE pattern seen in ischaemic cardiomyopathy.9 Subsequent studies reported the presence of LGE in up to 42% of patients with DCM.10 In addition to its diagnostic value, contrast-enhanced cardiovascular magnetic resonance (CE-CMR) has recently shown promising results in risk assessment in patients with cardiomyopathies. The presence of LGE has been shown to be associated with an increased risk of adverse events and to add independent information to established risk factors in patients with DCM,8 10 11 and more recently in patients with hypertrophic cardiomyopathies.12 13 Owing to the major impact this nding might potentially have with regard to the clinical management of DCM patients and in light of the limited number of patients included in the aforementioned studies, our goal was to assess the prognostic signicance of LGE in a larger population of clinically stable patients with DCM.
Non-ischaemic dilated cardiomyopathy (DCM) accounts for a substantial proportion of cardiovascular morbidity and mortality in developed countries.1e3 Despite the overall serious prognosis, with a 10-year mortality of over 40%,4 the individual clinical course is highly heterogeneous, ranging from asymptomatic patients to those suffering from severe congestive heart failure and
Heart 2011;97:727e732. doi:10.1136/hrt.2010.205542
METHODS Study population
The study population consisted of 184 consecutive patients with DCM who were referred to the Cardiomyopathy Center at the University Hospital Heidelberg between May 2005 and April 2008. CE-CMR was performed in these patients as part of the standard clinical evaluation for patients with
727
Downloaded from heart.bmj.com on October 31, 2011 - Published by group.bmj.com
Cardiomyopathy
cardiomyopathy at our institution unless one of the following contraindications to MR was present: cardiac pacemaker/ICD; other metallic implants not MR compatible; lack of patient informed consent; severe claustrophobia; severe obesity preventing the patient from entering the scanner bore; pregnancy; lactation. Chronic renal failure with an estimated glomerular ltration rate <30 ml/min/1.73 m2 was added as an exclusion criterion in July 2007 as a consequence of the advisory of the European Medical Board regarding nephrogenic systemic brosis following the administration of gadolinium contrast media. The diagnosis of DCM was based on the 1995 WHO/International Society and Federation of Cardiology criteria.14 Patients had to exhibit depressed systolic function (left ventricular ejection fraction (LV-EF) <50%) on a non-CMR study in the absence of signicant coronary artery disease (dened as $50% luminal stenosis on coronary angiography and/or a history of coronary revascularisation or myocardial infarction), valvular disease, hypertensive heart disease and congenital abnormalities. All patients had chronic heart failure of at least 12 months duration and were examined in a clinically stable condition (New York Heart Association (NYHA) functional class #III). No patient showed signs or symptoms of ongoing myocarditis. Patients initially diagnosed as having DCM displaying a subendocardial or transmural pattern of late enhancement suggestive of myocardial infarction were excluded from the nal analysis. Patients with a normal LV-EF on CMR (>55%) were also excluded. All patients were followed by either direct communication (follow-up visit or telephone interview) for the occurrence of (cardiac) death, ICD implantation, ICD discharge, hospitalisation for decompensated congestive heart failure, or heart transplantation. Mean6SEM follow-up duration was 658630 days. For outcome analysis, the end point was dened as a composite of cardiac death, appropriate ICD discharge for ventricular brillation/tachycardia, and hospitalisation for heart failure. If patients underwent heart transplantation, the follow-up data were censored at the time of transplantation. All patients gave their informed consent. The study protocol was approved by the institutional ethics committee. semi-automated software for volumetric analysis. Results for ventricular volumes, ejection fraction and LV myocardial mass were derived from short-axis slices after manual tracing of epicardial and endocardial borders, excluding papillary muscles from the myocardium. The presence and extent of late enhancement were evaluated by two independent observers experienced in CE-CMR (SL and HS), who were blinded to clinical data and outcome. To exclude artefact, LGE was deemed present only if visible in two orthogonal views. The pattern of LGE was characterised as mid-wall, epicardial, patchy/foci, or diffuse. For quantication of brosis, LGE was dened as areas with a signal intensity >2 SD above the mean signal intensity of remote myocardium in the same short-axis slice.11 Areas were measured by manual planimetry and expressed as percentage of myocardial mass.
Statistical analysis
Continuous variables were expressed as mean6SEM or as median with IQR for non-parametric variables. Differences between two groups were compared using the Student t test or ManneWhitney U test. In cases of more than two groups, differences were compared using analysis of variance or the KruskaleWallis test. Categorical variables were expressed as counts and percentages and compared by c2 test or Fisher exact test, respectively. Survival curves were estimated by the KaplaneMeier method and compared by the log-rank test. Univariate and multivariate Cox proportional hazards regression analysis was performed to calculate HRs and 95% CIs. For all analyses, p<0.05 was regarded as signicant. All statistical analyses were carried out using SPSS V.14.0.
RESULTS
Baseline patient demographics are displayed in table 1. The majority of patients were in symptomatic heart failure (NYHA Table 1 Patient demographics according to presence or absence of late gadolinium enhancement (LGE)
All patients (n[184) Age (years) BMI (kg/m2) Males Familial DCM Arterial hypertension Diabetes Atrial brillation 51.5561.1 25.6460.28 138 (75) 27 (14.7) 71 (38.6) 22 (12) 23 (12.5) LGEpos (n[72) 53.361.7 25.560.4 58 (81) 8 (1) 28 (39) 11 (15) 8 (1) LGEneg (n[112) 5061.5 25.760.4 80 (71) 19 (1.7) 43 (38.4) 11 (1) 15 (13.4) p Value* ns ns ns ns ns ns ns
CMR scan protocol
CMR was performed on a 1.5 T clinical scanner (Achieva Intera; Philips Healthcare, Best, The Netherlands) equipped with a veelement cardiac phased-array receiver coil. Cine images were obtained using a breath-hold segmented-k-space balanced fasteld echo sequence (SSFP) employing retrospective ECG gating in long-axis planes (two-chamber, four-chamber and threechamber views) as well as in contiguous short-axis slices (gap 2 mm) covering the whole ventricles from the annulus of the atrioventricular valves to the apex. Typical imaging parameters were: eld of view 3503350 mm2; repetition time/echo time 2.8/1.4 ms; acquired voxel size 2.232.238 mm3; ip angle 608; reconstructed voxel size 1.331.238 mm3. Delayed contrastenhanced images were acquired 10 min after the intravenous administration of gadolinium diethylenetriaminepenta-acetate (Magnevist; Bayer Schering Pharma, Berlin, Germany; 0.2 mmol/ kg) using a three-dimensional inversion-recovery gradient echo pulse sequence in sequential short-axis slices covering the whole ventricle as well as two-chamber and four-chamber views. Inversion time was adjusted to null normal myocardium and was typically 180e240 ms.
NYHA functional class I 42 (22.8) II 88 (47.8) III 54 (29.4) Heart failure medication ACEI 149 (81) ATRB 35 (19) b\ blockers 159 (86.4) Spironolactone 78 (42.4) Other diuretic 87 (47.3) Digoxin 34 (18.5) NT-proBNP (pg/ml) 255 (114e1488)
13 (18) 30 (41.7) 29 (40.2)
29 (25.9) 58 (51.8) 25 (22.3)
ns ns 0.03
60 (83.3) 17 (23.6) 66 (91.7) 39 (58.3) 42 (58.3) 16 (22.2) 491 (228.5e2932)
89 (79.5) 18 (16) 93 (83) 39 (34.8) 45 (40.2) 18 (16.1) 254 (92e800)
ns ns ns 0.01 0.02 ns 0.001
CMR analysis
All analyses were performed on a commercially available workstation (Viewforum; Philips Healthcare) equipped with
728
Values are mean6SEM, number (%) or median (IQR). *LGEpos vs LGEneg. ACEI, angiotensin-converting enzyme inhibitor; ATRB, angiotensin receptor blocker; BMI, body mass index; DCM, dilated cardiomyopathy; NT-proBNP, N-terminal pro-brain natriuretic peptide; NYHA, New York Heart Association.
Heart 2011;97:727e732. doi:10.1136/hrt.2010.205542
Downloaded from heart.bmj.com on October 31, 2011 - Published by group.bmj.com
Cardiomyopathy
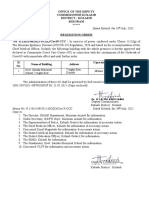
Figure 1 Presence and patterns of late gadolinium enhancement (LGE). LGE was present in 72/184 (39%) of patients with dilated cardiomyopathy. Representative short-axis slices illustrate the different patterns of LGE that were detected. In addition to the classic mid-wall enhancement, three distinct patterns of non-mid-wall LGE were found. Arrowheads indicate areas of LGE.
total study cohort ( n=184)
LGE neg (n=112)
LGE pos (n= 72)
45 non-midwall LGE (n= 45)
midwall LGE (n= 27)
epicardial ( n= 21)
patchy foci (n= 16)
diffuse (n= 8)
class II and III). In adherence with current treatment guidelines, almost all patients received b blockers and ACE inhibitors or angiotensin receptor blockers, respectively (table 1).
Late gadolinium enhancement
LGE was present in 72/184 (39%) patients (LGEpos). Of these, 27 exhibited a septal mid-wall enhancement, while 45 showed a nonmid-wall enhancement pattern (gure 1). With regard to the dichotomous presence of LGE, there was agreement between the two observers in all but one patient. This patient was assigned to the LGE-negative group (LGEneg) after a reading by a third blinded observer (DL). Compared with patients without any late enhancement, LGEpos patients showed more severe clinical heart failure, as reected in a higher prevalence of patients in NYHA functional class III and, consequently, the more frequent use of diuretics and spironolactone. In addition, the presence of LGE was associated with higher serum levels of NT-proBNP (table 1). No signicant differences were noted between patients with different enhancement patterns (online supplementary table 1A). With regard to quantication of LGE, linear regression analysis showed good interobserver and intraobserver reliability (R20.92 and R20.98, respectively). Among LGEpos patients, the median extent of brosis was 2.9% of LV mass (range 0.3e35.5%). Percentage of LGE was not related to gender, age, NYHA functional class or any other clinical baseline characteristic.
While a trend towards higher cardiac mortality among LGEpos patients could be observed, this failed to reach statistical signicance in light of the small total numbers (4/72 LGEpos patients vs 1/112 LGEneg patients, p0.08). However, the presence of LGE was associated with a markedly higher risk for the predened composite end point (15/72 LGEpos patients vs 6/112 LGEneg patients, p0.002). KaplaneMeier analysis revealed a signicantly worse event-free survival rate during long-term follow-up among LGEpos patients (gure 2A). Interestingly, when patients were further stratied according to degree of systolic dysfunction, the prognostic value of LGE was limited to those patients with a severely impaired LV function (LV-EF <30%) (gure 2B). The incidence of adverse cardiac events was not associated with specic LGE pattern (online supplementary table 3A). With an associated HR of 3.5, the presence of LGE was among the strongest univariate predictors for the combined end point, surpassed only by age $70 years. The multivariate model contained all univariate predictors in addition to NYHA class and male gender. LGE remained an independent predictor in addition to age and LV end-diastolic volume index (table 4). Among LGEpos patients, a strong association between the extent of LGE and the incidence of the combined end point could be noted (5.6% (2.7e11.4%) vs 2.6% (1.4e4.4%), p0.01). Table 2 Cardiovascular magnetic resonance data according to presence or absence of late gadolinium enhancement (LGE)
LGEpos (n[72) LV-EF (%) LV-EDV (ml) LV-EDVI (ml/m2) LV-ESV (ml) LV-SV (ml) CI (ml/min/m2) LV-mass (g) LV-mass/BSA (g/m2) RV-EF (%) RV-EDV (ml) RV-EDVI (ml/m2) RV-ESV (ml) RV-SV (ml) 31 265 133 181.3 76.7 2.9 158 80 41 195 103.25 113 73 (20.9e42.2) (228e325) (116e161) (128e255) (60e103) (2.3e3.5) (128e193) (67.1e94.8) (30e49.5) (162.5e195) (82.1e123) (91.5e157.5) (54.5e90) LGEneg (n[112) 44 215 109 117.5 86.2 2.9 129.4 65.8 40 224 111 132 82 (33.1e50.9) (175.2e272) (92.7e137.6) (89.3e173.3) (71e102) (2.5e3.4) (104.6e169.3) (55.2e82.9) (36e44) (201e258) (98.7e119) (119e162) (71.5e105) p Value <0.001 <0.001 <0.001 <0.001 ns ns <0.001 <0.001 ns ns ns ns 0.02
CMR parameters
Functional and volumetric CMR analysis revealed an association between the presence of LGE, more pronounced LV remodelling, and a higher degree of systolic dysfunction. As depicted in table 2, LGEpos patients exhibited larger LV volumes, a higher LV mass index and a lower LV-EF than patients in whom LGE was absent. Interestingly, no signicant differences could be found with regard to right ventricular analysis. Again, CMR parameters were comparable between patients with different enhancement patterns, with the exception of cardiac index (online supplementary table 2A). Among LGEpos patients, no signicant correlations between the extent of LGE and any of the functional CMR parameters could be established.
Outcome
During the follow-up period, ve patients suffered cardiac death; no non-cardiac deaths were recorded. The composite end point occurred in 21 patients (table 3).
Heart 2011;97:727e732. doi:10.1136/hrt.2010.205542
Values are median (IQR). BSA, body surface area; CI cardiac index; EDV, end-diastolic volume; EDVI, end-diastolic volume index; EF, ejection fraction; ESV, end-systolic volume; LV, left ventricular; RV, right ventricular; SV, stroke volume.
729
Downloaded from heart.bmj.com on October 31, 2011 - Published by group.bmj.com
Cardiomyopathy
Table 3 Incidence of cardiac events during follow-up
All patients (n[184) Cardiac death ICD discharge for VF/VT Hospitalisation for CHF Composite end point ICD implantation Cardiac transplantation 5 8 9 21 31 3 (2.7) (4.3) (4.9) (11.4)* (16.8) (1.6) LGEpos (n[72) 4 (5.6) 6 (8.3) 6 (8.3) 15* (20.8) 18 (25) 3 (4.2) LGEneg (n[112) 1 (0.9) 2 (1.8) 3 (2.7) 6 (5.4) 13 (11.6) 0 (0) p Valuey 0.08 0.06 0.16 0.002 0.03 0.06
A
event-free survival [%]
100 90 80 70 60 0
LGE neg [n=112] LGE pos [n=72]
log rank 7.63 p= 0.006
Values are number (%). *One patient was admitted for CHF and suffered sudden cardiac death at a later time point. yLGEpos vs LGEneg. CHF, congestive heart failure; ICD, implantable cardioverter debrillator; LGE, late gadolinium enhancement; VF, ventricular brillation; VT, ventricular tachycardia.
200
400
600
800 1000 1200 1400 1600
follow-up [days]
B
event-free survival [%]
Receiver operating characteristic curve analysis revealed a LGE percentage of 4.4 as optimal discriminator (area under the curve 0.7160.08, p0.01) for the occurrence of the combined end point with an associated HR of 5.28 (95% CI 1.8 to 15.5). Notably, when patients were divided into three groups according to (1) absence of LGE, (2) LGE #4.4% of LV mass and (3) LGE >4.4% of LV mass, KaplaneMeier analysis revealed a difference of event-free survival only for the third group (gure 2C).
100 90 80 70 60 50 40 0
EF>30%, LGE neg [n=89] EF<30%, LGE neg [n=23] EF>30%, LGE pos [n=36] EF<30%, LGE pos[n=36]
log rank 19.8 p = 0.0002
DISCUSSION
The ndings of this study support the use of CMR as a riskstratication tool in chronic heart failure. In this largest cohort of patients with DCM so far studied, the presence of LGE was associated with pronounced LV remodelling and constituted an independent predictor for adverse cardiac outcome. Fibrotic changes in hearts of patients with DCM have been recognised in histopathology for decades15 16 and can be classied into either diffuse (interstitial) or segmental (replacement) brosis.17 18 The mechanisms believed to contribute to the development of myocardial brosis are multiple and include inammation, neurohumoral changes and microvascular ischaemia.19 While its limited spatial resolution does not permit the visualisation of interstitial brosis, macroscopic areas of replacement brosis can reliably be detected by CE-CMR in patients with DCM. In the present cohort, LGE was found in 39% of patients, which is comparable to previous studies reporting incidences between 26% and 42%,6 10 and in line with ndings from explanted hearts of patients with DCM in whom segmental brosis can be detected in 33%.17 The process of adverse cardiac remodellingdthat is, the increase in ventricular volumes and myocardial mass and the change in chamber geometrydis central to the current pathophysiological understanding of chronic heart failure. On a cellular level, the remodelling process is characterised by several changes, including cardiomyocyte hypertrophy and broblast proliferation.19 20 In the present study, LGE was associated with marked increases in ventricular volumes and myocardial mass as well as severely impaired systolic function, providing further evidence for the close relationship between myocardial brosis and adverse remodelling, which has been observed in both animal and human myocardium.21 22 Despite the close association between presence of LGE and unfavourable ventricular function and geometry, it retained an independent prognostic value with an associated HR of 3.4 for the composite end point. Of note, the extent of brosis appears to be a critical factor for an adverse outcome. Among the LGEpos patients in our study population, only those with brosis extending to 4.4% of LV mass had an unfavourable prognosis, supporting earlier results from Assomull et al.11
730
200
400
600
800
1000 1200 1400 1600
C
event-free survival [%]
100 90 80 70 60 50 40 0 0
follow-up [days]
log rank 26.1 p < 0.0001
LGEneg LGEpos < 4.4%[n=48] LGEpos > 4.4%[n=24]
200
400
600
800 1000 1200 1400 1600
follow-up [days]
Figure 2 Event-free survival according to presence and extent of late gadolinium enhancement (LGE) and late ventricular ejection fraction (LV-EF). KaplaneMeier analysis illustrates the worse long-term outcome in LGEpos patients with regard to incidence of the composite end point of cardiac death, appropriate implantable cardioverter debrillator discharge, and hospitalisation for decompensated heart failure (A). The prognostic value of LGE strongly depends on underlying systolic dysfunction and appears to be conned to patients with a LV-EF < 30% (B). When LGEpos are further stratied into those with an area of LGE above or below the receiver operating characteristic curve specied discriminator of 4.4% LGE of LV mass, it becomes evident that those with only mild LGE have a prognosis comparable to those in whom LGE is absent (C). Why is the presence of LGE an independent predictor for adverse clinical outcome? Among others, one likely explanation is the promotion of re-entry mechanisms by focal brosis, causing malignant arrhythmias. Areas of brosis detected by CMR have been identied as substrates for inducible ventricular tachycardia in patients with ischaemic heart disease23 and, more recently, in patients with DCM.24 These ndings are supported by data from DCM patients undergoing ICD implantation.10 In addition to the impact on the electrophysiological properties of the heart, increasing amounts of brosis also lead to elastomechanical alterations, with a loss of ventricular compliance25
Heart 2011;97:727e732. doi:10.1136/hrt.2010.205542
Downloaded from heart.bmj.com on October 31, 2011 - Published by group.bmj.com
Cardiomyopathy
Table 4 Proportional hazard regression analysis for incidence of the composite end point
HR (95% CI) Univariate Male gender Age $70 years NYHA functional class LV-EF #30% EDVI (per 10 ml/m2 increase) LGE present LV-mass/BSA (per g/m2 increase) RV-EF #30% Multivariate* Age $70 years EDVI (per 10 ml/m2 increase) LGE present 0.78 (0.26 to 2.31) 4.91 (1.98 to 12.17) 1.84 (0.98 to 3.46) 3.38 (1.4 to 8.14) 1.09 (1.02 to 1.16) 3.5 (1.36 to 9.02) 1.001 (1 to 1.006) 2.71 (0.61 to 12.1) p Value 0.65 0.001 0.06 0.007 0.01 0.01 0.78 0.19
7.68 (2.92 to 20.23) 1.09 (1.01 to 1.18) 3.37 (1.26 to 9)
<0.001 0.025 0.015
*The nal model included all univariate predictors, male gender and NYHA functional class. BSA, body surface area; EDVI, end-diastolic volume index; EF, ejection fraction; LGE, late gadolinium enhancement; LV, left ventricular; NT-proBNP, N-terminal pro-brain natriuretic peptide; NYHA, New York Heart Association; RV, right ventricular.
on CMR alone correlates only poorly with the collagen volume fraction calculated from endomyocardial biopsies.18 One promising approach for the evaluation of microscopic brosis is the implementation of post-contrast T1 mapping sequences, which use the concept that gadolinium accumulation in interstitial brosis leads to shortening of T1 relaxation times.28e30 Endomyocardial biopsies were not routinely performed for the diagnosis of DCM in this patient cohort, in conformation with current guidelines. None of the patients had signs or symptoms of ongoing myocarditis; however, it is very likely that a subset of the patients in this study had myocarditis which developed into DCM. Previous studies reported that myocarditis is the cause of brosis in w10% of patients with DCM.4 A general limitation of the use of CE-CMR as a risk-stratication tool in patients with DCM is the current restrictions on application of gadolinium contrast agents in patients with chronic renal insufciency because of the risk of nephrogenic systemic brosis. It is known, however, that patients with chronic renal failure together with heart failure are at high risk.31
CONCLUSIONS
and subsequent increases in lling pressure, promoting the development of pulmonary and peripheral oedema. One important observation of this study is that the prognostic signicance of LGE is dependent on the degree of underlying LV dysfunction. Subgroup analysis revealed that the presence of brosis is associated with an unfavourable outcome only in patients with severely impaired LV function, which may reect greater vulnerability to the above effects of brotic changes on electrophysiological and mechanical properties. Conversely, patients with a LV-EF <30% and no evidence of brosis on CMR had a fairly benign outcome, supporting the additive prognostic impact of LGE. The patterns of LGE observed in patients with DCM are distinct from that seen in myocardial infarction, making CE-CMR a valuable tool for determining the aetiology of impaired systolic function.9 Interestingly, whereas some groups have reported the presence of only mid-wall enhancement in patients with DCM,9 11 others, including us, have found a variety of enhancement patterns, including not only mid-wall but also epicardial, diffuse and focal patterns.6 10 The reasons for this discrepancy are not yet clear. Histopathological examination of explanted hearts of patients with DCM shows patterns of brosis that conform with all of the observed LGE characteristics.15 16 20 At this point, it is not clear whether the various brotic patterns have different underlying causes or even represent different aetiologies of DCM. Although mid-wall enhancement is often observed in patients with myocarditis26 and may persist in patients who develop DCM, it is not specic to myocarditis, but can also be observed as a characteristic nding in certain familial DCM forms such as lamin mutations.27 Furthermore, epicardial and patchy patterns have also been described in DCM as well as myocarditis. In the present study, there is no evidence that the prognostic signicance of LGE is limited to certain patterns, which is in line with the ndings of Wu et al.10 However, these analyses need to be interpreted with caution because of the small number of patients and events. The use of CE-CMR for risk stratication of patients with CCM has produced promising data in single-centre studies. Results seem to be especially encouraging with regard to the identication of patients at high risk of developing malignant arrhythmias. However, there is a need for larger, multi-centre trials to conrm these ndings and to determine whether they will aid therapeutic decisions.
Acknowledgements We thank Birgit Horig and Angela Stocker-Wochele for excellent technical assistance with acquisitions of all MR scans. Competing interests None. Ethics approval This study was conducted with the approval of the ethics committee of the University of Heidelberg. Provenance and peer review Not commissioned; externally peer reviewed.
REFERENCES
1. Maron BJ, Towbin JA, Thiene G, et al. Contemporary denitions and classication of the cardiomyopathies. An American Heart Association scientic statement from the council on clinical cardiology, heart failure and transplantation committee; quality of care and outcomes research and functional genomics and translational biology interdisciplinary working groups; and council on epidemiology and prevention. Circulation 2006;113:1807e16. Coughlin SS, Neaton JD, Sengupta A, et al. Predictors of mortality from idiopathic dilated cardiomyopathy in 356,222 men screened for the multiple risk factor intervention trial. Am J Epidemiol 1994;139:166e72. Adams KF, Dunlap SH, Sueta CA, et al. Relation between gender, etiology and survival in patients with symptomatic heart failure. J Am Coll Cardiol 1996;28:1781e8. Felker GM, Thompson RE, Hare JM, et al. Underlying causes and long-term survival in patients with initially unexplained cardiomyopathy. N Engl J Med 2000;342:1077e84. Michels VV, Driscoll DJ, Miller FA, et al. Progression of familial and non-familial dilated cardiomyopathy: long-term follow-up. Heart 2003;89:757e61. Hombach V, Merkle N, Torzewski J, et al. Electrocardiographic and cardiac magnetic resonance imaging parameters as predictors of a worse outcome in patients with idiopathic dilated cardiomyopathy. Eur Heart J 2009;30:2011e18. Miller WL, Hartman KA, Burritt MF, et al. Troponin, B-type natriuretic peptides and outcomes in severe heart failure: differences between ischemic and dilated cardiomyopathies. Clin Cardiol 2007;30:245e50. Pennell D. Cardiovascular magnetic resonance. Heart 2001;85:581e9. McCrohon JA, Moon JCC, Prasad SK, et al. Differentiation of heart failure related to dilated cardiomyopathy and coronary artery disease using gadolinium- enhanced magnetic resonance. Circulation 2003;108:54e9. Wu KC, Weiss RG, Thiemann DR, et al. Late gadolinium enhancement by cardiovascular magnetic resonance heralds an adverse prognosis in nonischemic cardiomyopathy. Circulation 2003;108:54e9 Assomull RG, Prasad SK, Lyne J, et al. Cardiovascular magnetic resonance, brosis, and prognosis in dilated cardiomyopathy. J Am Coll Cardiol 2006;48:1977e85. OHanlon R, Grasso A, Roughton M, et al. Prognostic signicance of myocardial brosis in hypertrophic cardiomyopathy. J Am Coll Cardiol 2010;56:867e74.
2. 3. 4. 5. 6. 7. 8. 9. 10.
LIMITATIONS
Although CE-CMR is a valuable tool for detecting segmental brosis in patients with DCM, its limited spatial resolution does not allow the evaluation of diffuse brosis. The presence of LGE
Heart 2011;97:727e732. doi:10.1136/hrt.2010.205542
11. 12.
731
Downloaded from heart.bmj.com on October 31, 2011 - Published by group.bmj.com
Cardiomyopathy
13. 14. 15. 16. Bruder O, Wagner A, Jensen CJ, et al. Myocardial scar visualized by cardiovascular magnetic resonance imaging predicts major adverse events in patients with hypertrophic cardiomyopathy. J Am Coll Cardiol 2010;56:875e87. Richardson P, McKenna W, Bristow M, et al. Report of the 1995 World Health Organization/International Society and Federation of Cardiology Task Force on the denition and classication of cardiomyopathies. Circulation 1996;93:841e2. Unverferth DV, Baker PB, Swift SE, et al. Extent of myocardial brosis and cellular hypertrophy in dilated cardiomyopathy. Am J Cardiol 1986;57:816e20. Waller TA, Hiser WL, Capehart JE, et al. Comparison of clinical and morphologic cardiac ndings in patients having cardiac transplantation for ischemic cardiomyopathy, idiopathic dilated cardiomyopathy and dilated hypertrophic cardiomyopathy. Am J Cardiol 1998;81:884e94. Baig MK, Mahon N, McKenna WJ, et al. The pathophysiology of advanced heart failure. Am Heart J 1998;135:216e30. De Leeuw N, Ruiter DJ, Balk AHMM, et al. Histopathologic ndings in explanted heart tissue from patients with end-stage idiopathic dilated cardiomyopathy. Transpl Int 2001;14:299e306. Schalla S, Bekkers SC, Dennert R, et al. Replacement and reactive myocardial brosis in idiopathic dilated cardiomyopathy: comparison of magnetic resonance imaging with right ventricular biopsy. Eur J Heart Fail 2010;12:227e31. Beltrami CA, Finato N, Rocco M, et al. The cellular basis of dilated cardiomyopathy in humans. J Mol Cell Cardiol 1995;27:291e305. Ryoke T, Gu Y, Mao L, et al. Progressive cardiac dysfunction and brosis in the cardiomyopathic hamster and effects of growth hormone and angiotensindconverting enzyme inhibition. Circulation 1999;100:1734e43. Heling A, Zimmermann R, Kostin S, et al. Increased expression of cytoskeletal, linkage and extracellular proteins in failing human myocardium. Circ Res 2000;86:846e53. 23. 24. 25. 26. 27. 28. 29. Bello D, Fieno DS, Kim RJ, et al. Infarct morphology identies patients with substrate for sustained ventricular tachycardia. J Am Coll Cardiol 2005;45:1104e8. Nazarian S, Bluemke DA, Lardo AC, et al. Magnetic resonance assessement of the substrate for inducible ventricular tachycardia in nonischemic cardiomyopathy. Circulation 2005;112:2821e5. Choi EY, Choi BW, Kim SA, et al. Patterns of late gadolinium enhancement are associated with ventricular stiffness in patients with advanced non-ischaemic dilated cardiomyopathy. Eur J Heart Fail 2009;11:573e80. Mahrholdt H, Wagner A, Deluigi CC, et al. Presentation, patterns of myocardial damage and clinical course of viral myocarditis. Circulation 2006;114:1581e90. Raman SV, Sparks EA, Baker PM, et al. Mid-myocardial brosis by cardiac magnetic resonance in patients with lamin A/C cardiomyopathy: possible substrate for diastolic dysfunction. J Cardiovasc Magn Reson 2007;9:907e13. Messroghli DR, Plein S, Higgins DM, et al. Human myocardium: single-breath-hold MR T1 mapping with high spatial resolution- reproducibility study. Radiology 2005;238:1004e12. Jerosch- Herold M, Sheridan DC, Kushner JD, et al. Cardiac magnetic resonance imaging of myocardial contrast uptake and blood ow in patients affected with idiopathic or familial dilated cardiomyopathy. Am J Physiol Heart Circ Physiol 2008;295:1234e42. Iles L, Puger H, Phrommintikul A, et al. Evaluation of diffuse myocardial brosis in heart failure with cardiac magnetic resonance contrast-enhanced T1 mapping. J Am Coll Cardiol 2008;52:1574e80. Hillege HL, Nitsch D, Pfeffer MA, et al. Renal function as a predictor of outcome in a broad spectrum of patients with heart failure. Circulation 2006;113:671e78.
17. 18. 19. 20. 21. 22.
30. 31.
Information in a hurry...
If you need the latest information in emergency care then you need the Emergency Medicine Journal. Packed with research, educational papers and debate of all aspects of emergence medicine, the journal will make sure you know everything you need to.
FOR MORE DETAILS OR TO SUBSCRIBE, VISIT THE WEBSITE TODAY
emj.bmj.com
732
Heart 2011;97:727e732. doi:10.1136/hrt.2010.205542
Downloaded from heart.bmj.com on October 31, 2011 - Published by group.bmj.com
Use of cardiovascular magnetic resonance for risk stratification in chronic heart failure: prognostic value of late gadolinium enhancement in patients with non-ischaemic dilated cardiomyopathy
Stephanie Lehrke, Dirk Lossnitzer, Michael Schb, et al. Heart 2011 97: 727-732 originally published online November 20, 2010
doi: 10.1136/hrt.2010.205542
Updated information and services can be found at:
http://heart.bmj.com/content/97/9/727.full.html
These include:
Data Supplement References
"Web Only Data"
http://heart.bmj.com/content/suppl/2011/08/01/hrt.2010.205542.DC1.html
This article cites 31 articles, 21 of which can be accessed free at:
http://heart.bmj.com/content/97/9/727.full.html#ref-list-1
Article cited in:
http://heart.bmj.com/content/97/9/727.full.html#related-urls
Email alerting service
Receive free email alerts when new articles cite this article. Sign up in the box at the top right corner of the online article.
Topic Collections
Articles on similar topics can be found in the following collections Drugs: cardiovascular system (5364 articles) Dilated cardiomyopathy (207 articles) Heart failure (411 articles) Epidemiology (2189 articles)
Notes
To request permissions go to:
http://group.bmj.com/group/rights-licensing/permissions
To order reprints go to:
http://journals.bmj.com/cgi/reprintform
To subscribe to BMJ go to:
http://group.bmj.com/subscribe/
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- STEINER LECTURE Vaccination Caused The 1918 Deadly Flu EpidemicDocument3 pagesSTEINER LECTURE Vaccination Caused The 1918 Deadly Flu EpidemicSoror Babalon60% (5)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Bee Propolis PresentationDocument23 pagesBee Propolis PresentationPERRYAMNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Indoor Air Quality AnalysisDocument21 pagesIndoor Air Quality AnalysisAshmit DubeyNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Disaster Prevention and MitigationDocument36 pagesDisaster Prevention and MitigationCarlo HafallaNo ratings yet
- Ophthalmology Explorer 1st EditionDocument373 pagesOphthalmology Explorer 1st EditionAaron French100% (3)
- Vet MedicinesDocument36 pagesVet MedicinesSadam Irshad100% (3)
- Plasma Frequencies: Group One Group TwoDocument9 pagesPlasma Frequencies: Group One Group TwoMihnea ColtanelNo ratings yet
- ReportViewer 2Document4 pagesReportViewer 2Syed Husnain100% (1)
- Haematologica 2014Document7 pagesHaematologica 2014PUIGCOZARNo ratings yet
- EncefalitisDocument3 pagesEncefalitisPUIGCOZARNo ratings yet
- Amyloid and FDG-PET Study of Logopenic Primary ProgressiveDocument10 pagesAmyloid and FDG-PET Study of Logopenic Primary ProgressivePUIGCOZARNo ratings yet
- Movement DisordersDocument10 pagesMovement DisordersPUIGCOZARNo ratings yet
- J Nucl Med-2009 From RECIST To PercistDocument30 pagesJ Nucl Med-2009 From RECIST To PercistPUIGCOZARNo ratings yet
- Colina SNM 2013Document8 pagesColina SNM 2013PUIGCOZARNo ratings yet
- PET AmiloideDocument4 pagesPET AmiloidePUIGCOZARNo ratings yet
- EwingDocument8 pagesEwingPUIGCOZARNo ratings yet
- Guia para NueroendocrinosDocument17 pagesGuia para NueroendocrinosPUIGCOZARNo ratings yet
- Journal of Affective Disorders Volume 142 Issue 1 2012 [Doi 10.1016_j.jad.2012.05.001] Nery-Fernandes, Fabiana_ Rocha, Marlos v._ Jackowski, Andrea_ La -- Reduced Posterior Corpus Callosum Area in Suicidal and Non-suDocument6 pagesJournal of Affective Disorders Volume 142 Issue 1 2012 [Doi 10.1016_j.jad.2012.05.001] Nery-Fernandes, Fabiana_ Rocha, Marlos v._ Jackowski, Andrea_ La -- Reduced Posterior Corpus Callosum Area in Suicidal and Non-suPUIGCOZARNo ratings yet
- Florbetaben SNM 2013Document9 pagesFlorbetaben SNM 2013PUIGCOZARNo ratings yet
- Gidelines Infeccion InflamacionDocument2 pagesGidelines Infeccion InflamacionPUIGCOZARNo ratings yet
- 124 I PetDocument8 pages124 I PetPUIGCOZARNo ratings yet
- 11C MetioninaDocument8 pages11C MetioninaPUIGCOZARNo ratings yet
- 124 I PetDocument8 pages124 I PetPUIGCOZARNo ratings yet
- Prognostic Importance of Late Gadoliniumheartjnl-2011-300814.FullDocument6 pagesPrognostic Importance of Late Gadoliniumheartjnl-2011-300814.FullPUIGCOZARNo ratings yet
- Curva Tiempo ActividadDocument7 pagesCurva Tiempo ActividadPUIGCOZARNo ratings yet
- Anticuerpos MarcadosDocument9 pagesAnticuerpos MarcadosPUIGCOZARNo ratings yet
- Ralacion Adreview y Potenciales VentricularesDocument9 pagesRalacion Adreview y Potenciales VentricularesPUIGCOZARNo ratings yet
- Electrocardiographic and Cardiac MagneticDocument8 pagesElectrocardiographic and Cardiac MagneticPUIGCOZARNo ratings yet
- Prevalence of Scarred and DysfunctionalDocument11 pagesPrevalence of Scarred and DysfunctionalPUIGCOZARNo ratings yet
- GuidelinesDocument11 pagesGuidelinesPUIGCOZARNo ratings yet
- Myocardial Iodine-123 Meta-Iodobenzylguanidine Imaging and Cardiac Events in Heart FailureDocument10 pagesMyocardial Iodine-123 Meta-Iodobenzylguanidine Imaging and Cardiac Events in Heart FailurePUIGCOZARNo ratings yet
- CMR in Heart FailureDocument11 pagesCMR in Heart FailurePUIGCOZARNo ratings yet
- J Am Coll 2003Document10 pagesJ Am Coll 2003PUIGCOZARNo ratings yet
- Impact oDocument7 pagesImpact oPUIGCOZARNo ratings yet
- Seminars 2011Document14 pagesSeminars 2011PUIGCOZARNo ratings yet
- Heart Fail Rev Octubre 2010Document13 pagesHeart Fail Rev Octubre 2010PUIGCOZARNo ratings yet
- GuidelinesDocument11 pagesGuidelinesPUIGCOZARNo ratings yet
- Prebiotics and Probiotics (1Document20 pagesPrebiotics and Probiotics (1Mudassir Ali QazalbashNo ratings yet
- Agustin, Aileen - CMV UL 16Document10 pagesAgustin, Aileen - CMV UL 16Concepcion R. AquinoNo ratings yet
- Notes: Adrenal HypofunctionDocument4 pagesNotes: Adrenal HypofunctionWiyosa RusdiNo ratings yet
- Acute Osteomyelitis in Children - JurdingDocument25 pagesAcute Osteomyelitis in Children - JurdingTimoty MarioNo ratings yet
- Influenza 1918.0910Document19 pagesInfluenza 1918.0910RafaelNo ratings yet
- Journal Reading ParuDocument53 pagesJournal Reading ParuDaniel IvanNo ratings yet
- CKD Flyer PHEPRO - Org Sri LankaDocument19 pagesCKD Flyer PHEPRO - Org Sri LankalankaCnewsNo ratings yet
- National Guinea Worm Eradication ProgrammeDocument38 pagesNational Guinea Worm Eradication ProgrammeDeepan0507No ratings yet
- Maritime Declaration of Health 3Document1 pageMaritime Declaration of Health 3Geoffrey AchasNo ratings yet
- Atrial FlutterDocument2 pagesAtrial FlutterDhiaNo ratings yet
- At The End of The Lesson, The Learners Should Be Able ToDocument4 pagesAt The End of The Lesson, The Learners Should Be Able ToHarold Nalla HusayanNo ratings yet
- The Digestive SystemDocument10 pagesThe Digestive Systemapi-272920130No ratings yet
- WuchereriozaDocument37 pagesWuchereriozaSteames EaNo ratings yet
- Mrs Jenny obstetric historyDocument3 pagesMrs Jenny obstetric historyDwi AnggoroNo ratings yet
- Definition of PneumoniaDocument4 pagesDefinition of PneumoniaEmylia Ananda PutriNo ratings yet
- Feu-Nrmf (Drug Study)Document7 pagesFeu-Nrmf (Drug Study)Kaye LaraganNo ratings yet
- New Covid Care Center DesignatedDocument3 pagesNew Covid Care Center DesignatedPascal ChhakchhuakNo ratings yet
- Fowl Cholera Guide: Causes, Signs, Treatment & PreventionDocument34 pagesFowl Cholera Guide: Causes, Signs, Treatment & Preventionmazher aliNo ratings yet
- ISR Project - Water Scarcity in MaharashtraDocument38 pagesISR Project - Water Scarcity in MaharashtraSuraj0% (2)
- Republic Act No 11332Document6 pagesRepublic Act No 11332AnnyleneMauricioNo ratings yet
- Th1 - Th2 Dominance SymptomsListDocument3 pagesTh1 - Th2 Dominance SymptomsListikuus123No ratings yet
- Anti TBDocument68 pagesAnti TBGunjan YadavNo ratings yet


























































![Journal of Affective Disorders Volume 142 Issue 1 2012 [Doi 10.1016_j.jad.2012.05.001] Nery-Fernandes, Fabiana_ Rocha, Marlos v._ Jackowski, Andrea_ La -- Reduced Posterior Corpus Callosum Area in Suicidal and Non-su](https://imgv2-1-f.scribdassets.com/img/document/286583930/149x198/dca688bf78/1445582757?v=1)