Professional Documents
Culture Documents
Nursing
Uploaded by
Annette Aquino GuevarraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nursing
Uploaded by
Annette Aquino GuevarraCopyright:
Available Formats
BIPOLAR DISORDER
DEFINITON Bipolar disorder sometimes called manic-depressive disorder is associated with mood swings that range from the lows of depression to the highs of mania. When you become depressed, you may feel sad or hopeless and lose interest or pleasure in most activities. When your mood shifts in the other direction, you may feel euphoric and full of energy. Mood shifts may occur only a few times a year, or as often as several times a day. In some cases, bipolar disorder causes symptoms of depression and mania at the same time.
Reference: http://www.mayoclinic.com/health/bipolar-disorder/DS00356
RISK FACTORS Factors that may increase the risk of developing bipolar disorder include:
Having blood relatives such as a parent or sibling with bipolar disorder Periods of high stress Drug or alcohol abuse Major life changes, such as the death of a loved one Being in your early 20s Conditions that commonly occur with bipolar disorder If you have bipolar disorder, you may also have another health condition that's diagnosed before or after your diagnosis of bipolar disorder. Such conditions need to
be diagnosed and treated because they may worsen existing bipolar disorder. They include:
Anxiety disorders. Examples include post-traumatic stress disorder (PTSD), social phobia and generalized anxiety disorder. Attention-deficit/hyperactivity disorder (ADHD). ADHD has symptoms that overlap with bipolar disorder. For this reason, bipolar disorder can be difficult to differentiate from ADHD. Sometimes one is mistaken for the other. In some cases, a person may be diagnosed with both conditions. Addiction or substance abuse. Many people with bipolar disorder also have alcohol, tobacco or drug problems. Drugs or alcohol may seem to ease symptoms, but they can actually trigger, prolong or worsen depression or mania. Physical health problems. People diagnosed with bipolar disorder are more likely to have certain other health problems, including heart disease, thyroid problems and obesity.
Reference: http://www.mayoclinic.com/health/bipolar-disorder/DS00356/DSECTION=risk-factors
CAUSES/ ETIOLOGY The exact cause of bipolar disorder is unknown, but several factors seem to be involved in causing and triggering bipolar episodes:
Biological differences. People with bipolar disorder appear to have physical changes in their brains. The significance of these changes is still uncertain but may eventually help pinpoint causes. Neurotransmitters. An imbalance in naturally occurring brain chemicals called neurotransmitters seems to play a significant role in bipolar disorder and other mood disorders. Hormones. Imbalanced hormones may be involved in causing or triggering bipolar disorder. Inherited traits. Bipolar disorder is more common in people who have a blood relative (such as a sibling or parent) with the condition. Researchers are trying to find genes that may be involved in causing bipolar disorder.
Environment. Stress, abuse, significant loss or other traumatic experiences may play a role in bipolar disorder.
Reference: http://www.mayoclinic.com/health/bipolar-disorder/DS00356/DSECTION=causes
PSYCHODYNAMICS
The pathophysiology of bipolar disorder has not been determined, and no objective biologic markers correspond definitively with the disease state. However, twin, family, and adoption studies all indicate that bipolar disorder has a genetic component. In fact, first-degree relatives of a person with bipolar disorder are approximately 7 times more likely to develop bipolar disorder than the rest of the population. The genetic component of bipolar disorder appears to be complex: the disorder is likely to be caused by multiple different common disease alleles, on the order of hundreds to thousands, each of which contributes a relatively low degree of risk on its own. Such disease genes can be difficult to find without very large sample sizes, on the order of thousands of subjects. The first series of genome-wide association studies (GWAS) for bipolar disorder were published in 2007 and 2008, and a collaborative analysis of the last 3 studies gave combined support for 2 particular genes, ANK3 (ankyrin G) andCACNA1C (alpha 1C subunit of the L-type voltage-gated calcium channel) in a sample of 4,387 cases and 6,209 controls. ANK3 is an adaptor protein found at axon initial segments that regulates the assembly of voltage-gated sodium channels. Both ANK3 and subunits of the calcium channel are down-regulated in mouse brain in response to lithium, which indicates a possible therapeutic mechanism of action of 1 of the most effective treatments for bipolar disorder. Further evidence for association of bipolar disorder to CACNA1C was reported in 2011 in an ever-growing sample (now numbering 11,974 bipolar disorder cases and 51,792 controls), providing overwhelming support for this gene as a bipolar susceptibility locus. CACNA1C, on chromosome 12, encodes the alpha subunit of the L-type voltage-gated calcium ion channel found in the brain. L-type calcium channel blockers have been used to treat bipolar disorder, and there has been speculation that at least some mood stabilizers may mediate their effects via modulating calcium channel signaling in bipolar illness. A joint analysis of the bipolar GWAS data was carried out, including GWAS data from another large-scale study of schizophrenia published in the same issue. Again, both ANK3 and CACNA1C came up positive in the combined data set, suggesting a shared genetic basis for these disorders. A previous National Institutes of Health (NIH) report on recent genome-wide association studies also underscored that bipolar disorder and schizophrenia could indeed share common susceptibility genes
on chromosome 6. These data herald future revision of theDiagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) according to an etiologic rather than descriptive basis. The first GWAS of bipolar disorder used a much smaller sample size than subsequent attempts , including an initial sample of 461 patients with bipolar disorder from the National Institute of Mental Health (NIMH) consortium and a follow-up sample of 563 patients collected in Germany. This gene was not highlighted in the most recent and largest bipolar GWAS published by Sklar et al 2011. Nevertheless, this study remains of interest, in that the strongest association signals were detected in genes also involved in biochemical pathways regulated by lithium. The strongest hit was at a marker within the first intron of diacylglycerol kinase eta (DGKH) gene. DGKH is a key protein in the lithium-sensitive phosphatidyl inositol pathway. Three of the other associated genes in this study also interact with the Wnt signaling pathway upstream and downstream of glycogen synthase kinase 3-beta (GSK3). Lithium-mediated inhibition of GSK3 is thought to result in downregulation of molecules involved in cell death and upregulation of neuroprotective factors. Additionally, GSK3 is a central regulator of the circadian clock, and lithiummediated modulation of circadian periodicity is thought to be a critical component of lithiums therapeutic effect. In fact, another major coup for bipolar disorder research has been the finding that a dominant-negative mutation in the CLOCKgene normally contributing to circadian periodicity in humans results in maniclike behavior in mice. Manic behavior in CLOCK mutant mice includes hyperactivity, decreased sleep, reduced anxiety, and an increased response to cocaine. The latter finding also provides a shared biologic basis for the high rate of substance abuse observed in clinical populations of subjects with bipolar disorder. Furthermore, the experimenters were able to abolish the manic behaviors by rescuing expression of normal CLOCK specifically in the ventral tegmental area of the mouse brain. This area is rich in D2 receptors. Joseph Coyle hypothesizes in his commentary in the paper on the same issue that the efficacy of atypical antipsychotics in acute mania might, in part, be achieved by their ability to lower activity in neurons specifically within the ventral tegmental area. Although large-scale association studies of bipolar disorder are beginning to yield results, one of the greatest obstacles to finding genes for such complex behavior is the imprecision inherent in diagnosis of the disorder itself; objective criteria are lacking. Therefore, some of the most exciting recent research is focused on defining heritable, quantitative diagnostic measures that capture specific features of bipolar disorder (termed endophenotypes) to refine the search for responsible genes. Such promising measures for bipolar disorder include structural brain phenotypes, sleep and activity measures, neurocognitive measures, and gene expression studies. Gene expression studies, one way of measuring the relative activity or inactivity of genes, have already been proven useful for illuminating the pathophysiology of psychiatric disorders, including bipolar disorder. For instance,
studies comparing specific regions of postmortem brain tissue from persons with bipolar disorder with tissue from control subjects have consistently shown that levels of expression of oligodendrocyte-myelinrelated genes appear to be decreased in brain tissue from persons with bipolar disorder. As with genetic studies, gene expression profiling studies require very large sample sizes to produce replicable data. Furthermore, they must focus on the correct brain region(s) thought to be functioning differently in bipolar disorder, a point still under some debate. Therefore, research in this area is ongoing and frequently subject to update. Oligodendrocytes produce myelin membranes that wrap around and insulate axons to permit the efficient conduction of nerve impulses in the brain. Therefore, loss of myelin is thought to disrupt communication between neurons, leading to some of the thought disturbances observed in bipolar disorder and related illnesses. Brain imaging studies of persons with bipolar disorder also show abnormal myelination in several brain regions associated with this illness. A meta-analysis by Houenou et al found decreased activation and diminution of gray matter in a cortical-cognitive brain network, which has been associated with the regulation of emotions in patients with bipolar disorder. An increased activation in ventral limbic brain regions that mediate the experience of emotions and generation of emotional responses was also discovered. This provides evidence for functional and anatomical alterations in bipolar disorder in brain networks associated with the experience and regulation of emotions. Interestingly, gene expression and neuroimaging studies of persons with schizophrenia and major depression also demonstrate similar findings, indicating that mood disorders and schizophrenia may share some biologic underpinnings, possibly related to psychosis. These types of data may also lead to the future revision of psychiatric diagnostic manuals based on a new understanding of the etiology of these disorders. Another approach to delineating the pathophysiology of bipolar disorder involves studying changes in gene expression induced in rodent brains after administration of pharmacologic agents used to treat bipolar disorder. For example, investigators have demonstrated that 2 chemically unrelated drugs (lithium and valproate) used to treat bipolar disorder both up-regulate the expression of the cytoprotective protein Bcl-2 in the frontal cortex and the hippocampus of rat brains. These types of studies are also performed on human tissue by exposing cultured monocytes from peripheral blood to lithium and other factors. A postmortem study by Konradi et al of the hippocampus in both patients with bipolar disorder and healthy persons found that the 2 groups did not differ in the total number of hippocampal neurons. However, patients with bipolar disorder had reduced volume of nonpyramidal cell layers, a reduced number of somatostatin-positive and parvalbumin positive neurons, a reduced somal volume in cornu ammonis sector 2/3, and reduced messenger RNA levels for somatostatin, parvalbumin, and glutamic acid decarboxylase 1. These findings suggest alteration of hippocampal interneurons in patients with bipolar disorder that might lead to hippocampal dysfunction.
Neuroimaging studies of individuals with bipolar disorder or other mood disorders also suggest evidence of cell loss or atrophy in these same brain regions. Thus, another suggested cause of bipolar disorder is damage to cells in the critical brain circuitry that regulates emotion. According to this hypothesis, mood stabilizers and antidepressants are thought to alter mood by stimulating cell survival pathways and increasing levels of neurotrophic factors to improve cellular resiliency. In 2008, Mathew et al published a review of novel drugs and therapeutic targets for severe mood disorders that focus on increasing neuroplasticity and cellular resiliency. Post et al proposed a mechanism involving electrophysiologic kindling and behavioral sensitization processes, which resonates with the neuronal injury hypothesis. They asserted that a person who is susceptible to bipolar disorder experiences an increasing number of minor neurologic insultsfrom drugs of abuse, stress-related excessive glucocorticoid stimulation, or other factorsthat eventually result in mania. Sufficient brain damage might persist to cause mania to recur even with no or minor environmental or behavioral stressors. This type of formulation helps explain the effective role of anticonvulsant medications (eg, carbamazepine and valproate) in the prevention of the highs and lows of bipolar disorder. It also supports clinical observations that the more episodes a person experiences, the more he or she will have in the future, underscoring the need for long-term treatment.
MEDICAL/NURSING MANAGEMENT
Treatment of bipolar disorder is usually involves medication. A combination of mood stabilizing agents with antidepressants, antipsychotics, and anticonvulsants is used to regulate manic and depressive episodes. Mood stabilizing agents such as lithium, carbamazepine, and valproate are prescribed to regulate the manic highs and lows of bipolar disorder. Lithium (Cibalith-S, Eskalith, Lithane, Lithobid, Lithonate, Lithotabs) is one of the oldest and most frequently prescribed drugs available for the treatment of bipolar mania and depression. Because the drug takes 40 days to reach a therapeutic level in the bloodstream, it is sometimes prescribed in conjunction with neuroleptics and/or benzodiazepines to provide more immediate relief of a manic episode. Lithium has also been shown to be effective in regulating bipolar depression, but is not
recommended for mixed mania. Lithium may not be an effective longterm treatment option for rapid cyclers, who typically develop a tolerance for it, or may not respond to it. Possible side effects of the drug include weight gain, thirst, nausea, and hand tremors. Prolonged lithium use may also cause hyperthyroidism (a disease of the thryoid that is marked by heart palpitations, nervousness, the presence of goiter, sweating, and a wide array of other symptoms.) Carbamazepine (Tegretol, Atretol) is an anticonvulsant drug usually prescribed in conjunction with other mood stabilizing agents. The drug is often used to treat bipolar patients who have not responded well to lithium therapy. Blurred vision and abnormal eye movement are two possible side effects of carbamazepine therapy. As of early 1998, carbamazepine did not have an FDA-approved indication for mania. Valproate (divalproex sodium or Depakote; valproic acid or Depakene) is one of the few drugs available that has been proven effective in treating rapid cycling bipolar and mixed states patients. Valproate is prescribed alone or in combination with carbamazepine and/or lithium. Stomachcramps, indigestion, diarrhea, hair loss, appetite loss, nausea, and unusual weight loss or gain are some of the common side effects of valproate. Note: valproate is also approved for the treatment of mania. Because antidepressants may stimulate manic episodes in some bipolar patients, their use is typically short-term. Selective serotonin reuptake inhibitors (SSRIs) or, less often, monoamine oxidase inhibitors (MAO inhibitors) are prescribed for episodes of bipolar depression. Tricyclic antidepressants used to treat unipolar depression may trigger rapid cycling in bipolar patients and are, therefore, not a preferred treatment option for bipolar depression. SSRIs, such as fluoxetine (Prozac), sertraline (Zoloft), and paroxetine (Paxil), treat depression by regulating levels of serotonin, a neurotransmitter. Anxiety, diarrhea, drowsiness, headache, sweating,
nausea, sexual problems, and insomnia are all possible side effects of SSRIs. MAOIs, such as tranylcypromine (Parnate) and phenelzine (Nardil), block the action of monoamine oxidase (MAO), an enzyme in the central nervous system. Patients taking MAOIs must cut foods high in tyramine (found in aged cheeses and meats) out of their diet to avoid hypotensive side effects. Bupropion (Wellbutrin) is a heterocyclic antidepressant. The exact neurochemical mechanism of the drug is not known, but it has been effective in regulating bipolar depression in some patients. Side effects of bupropion include agitation, anxiety, confusion, tremor, dry mouth, fast or irregular heartbeat, headache, and insomnia. ECT, or electroconvulsive therapy, has a high success rate for treating both unipolar and bipolar depression, and mania. However, because of the convenience of drug treatment and the stigma sometimes attached to ECT therapy, ECT is usually employed after all pharmaceutical treatment options have been explored. ECT is given under anesthesia and patients are given a muscle relaxant medication to prevent convulsions. The treatment consists of a series of electrical pulses that move into thebrain through electrodes on the patient's head. Although the exact mechanisms behind the success of ECT therapy are not known, it is believed that this electrical current alters the electrochemical processes of the brain, consequently relieving depression. Headaches, muscle soreness, nausea, and confusion are possible side effects immediately following an ECT procedure. Temporary memory loss has also been reported in ECT patients. In bipolar patients, ECT is often used in conjunction with drug therapy. Adjunct treatments are used in conjunction with a long-term pharmaceutical treatment plan. Long-acting benzodiazepines such as clonazepam (Klonapin) and alprazolam (Xanax) are used for rapid treatment of manic symptoms to calm and sedate patients until mania or hypomania have waned and mood stabilizing agents can take effect.
Sedation is a common effect, and clumsiness, lightheadedness, and slurred speech are other possible side effects of benzodiazepines. Neuroleptics such as chlorpromazine (Thorazine) and haloperidol (Haldol) are also used to control mania while a mood stabilizer such as lithium or valproate takes effect. Because neuroleptic side effects can be severe (difficulty in speaking or swallowing, paralysis of the eyes, loss of balance control, muscle spasms, severe restlessness, stiffness of arms and legs, tremors in fingers and hands, twisting movements of body, and weakness of arms and legs), benzodiazepines are generally preferred over neuroleptics. Because bipolar disorder is thought to be biological in nature, therapy is recommended as a companion to, but not a substitute for, pharmaceutical treatment of the disease. Psychotherapy, such as cognitive-behavioral therapy, can be a useful tool in helping patients and their families adjust to the disorder, in encouraging compliance to a medication regimen, and in reducing the risk of suicide. Also, educative counseling is recommended for the patient and family. Calcium channel blockers (nimodipine or Nimotop), typically used to treat angina and hypotension, have been found effective in a few small studies for treating rapid cyclers. Calcium channel blockers stop the excess calcium build up in cells that is thought to be a cause of bipolar disorder. They are usually used in conjunction with other drug therapies such as carbamazepine or lithium. Clozapine (Clozaril) is an atypical antipsychotic medication used to control manic episodes in patients who have not responded to typical mood stabilizing agents. The drug has also been a useful prophylactic, or preventative treatment, in some bipolar patients. Common side effects of clozapine include tachycardia (rapid heart rate), hypotension, constipation, and weight gain. Agranulocytosis, a potentially serious but reversible condition in which the white blood cells that typically fightinfection in the body are destroyed, is a possible side effect of
clozapine. Patients treated with the drug should undergo weekly blood tests to monitor white blood cell counts. Risperidone (Risperdal) is another atypical antipsychotic medication that has been successful in controlling mania in several clinical trials when low doses were administered. The side effects of risperidone are mild compared to many other antipsychotics (constipation, coughing, diarrhea, dry mouth, headache, heartburn, increased length of sleep and dream activity, nausea, runny nose, sore throat, fatigue, and weight gain). Lamotrigine (Lamictal, or LTG), an anticonvulsant medication, was found to alleviate manic symptoms in a 1997 trial of 75 bipolar patients. The drug was used in conjunction with divalproex (divalproate) and/or lithium. Possible side effects of lamotrigine include skin rash, dizziness, drowsiness, headache, nausea, and vomiting. rTMS, or repeated transcranial magnetic stimulation is a new and still experimental treatment for the depressive phase of bipolar disorder. In rTMS, a large magnet is placed on the patient's head and magnetic fields of different frequency are generated to stimulate the left front cortex of the brain. Unlike ECT, rTMS requires no anesthesia and does not induce seizures.
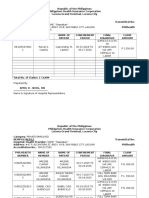
POSSIBLE NURSING DIAGNOSIS
You might also like
- Annex B Doh 2Document3 pagesAnnex B Doh 2Annette Aquino GuevarraNo ratings yet
- First Page 2Document3 pagesFirst Page 2Annette Aquino GuevarraNo ratings yet
- Infectious Waste: Referred PatientDocument1 pageInfectious Waste: Referred PatientAnnette Aquino GuevarraNo ratings yet
- Infectious Waste: Referred PatientDocument1 pageInfectious Waste: Referred PatientAnnette Aquino GuevarraNo ratings yet
- Transmittal PhilhealthDocument7 pagesTransmittal PhilhealthAnnette Aquino GuevarraNo ratings yet
- Fdar Samples PresentationDocument29 pagesFdar Samples PresentationAnnette Aquino Guevarra100% (2)
- Affidavit of LigationDocument2 pagesAffidavit of LigationAnnette Aquino GuevarraNo ratings yet
- GarbageDocument1 pageGarbageAnnette Aquino GuevarraNo ratings yet
- Immediate Essential New Born CareDocument2 pagesImmediate Essential New Born CareAnnette Aquino GuevarraNo ratings yet
- Immediate Essential New Born CareDocument2 pagesImmediate Essential New Born CareAnnette Aquino GuevarraNo ratings yet
- Transmittal PhilhealthDocument7 pagesTransmittal PhilhealthAnnette Aquino GuevarraNo ratings yet
- Transmittal PhilhealthDocument7 pagesTransmittal PhilhealthAnnette Aquino GuevarraNo ratings yet
- Project in ScienceDocument6 pagesProject in ScienceAnnette Aquino GuevarraNo ratings yet
- List of ClientsDocument1 pageList of ClientsAnnette Aquino GuevarraNo ratings yet
- (Open 24 Hours) (Open 24 Hours)Document2 pages(Open 24 Hours) (Open 24 Hours)Annette Aquino GuevarraNo ratings yet
- SummaryDocument1 pageSummaryAnnette Aquino GuevarraNo ratings yet
- Skills Checklist - Ob GyneDocument3 pagesSkills Checklist - Ob GyneAnnette Aquino GuevarraNo ratings yet
- Certificate of Employment for Private Nurse Criezl AridaDocument1 pageCertificate of Employment for Private Nurse Criezl AridaAnnette Aquino Guevarra70% (10)
- Drug NameDocument6 pagesDrug NameAnnette Aquino GuevarraNo ratings yet
- Psychiatric NursingDocument10 pagesPsychiatric NursingAnnette Aquino GuevarraNo ratings yet
- LetterDocument1 pageLetterAnnette Aquino GuevarraNo ratings yet
- BookDocument7 pagesBookAnnette Aquino GuevarraNo ratings yet
- NewspaperDocument4 pagesNewspaperAnnette Aquino GuevarraNo ratings yet
- StaffDocument1 pageStaffAnnette Aquino GuevarraNo ratings yet
- DLSPDocument3 pagesDLSPAnnette Aquino GuevarraNo ratings yet
- SummaryDocument1 pageSummaryAnnette Aquino GuevarraNo ratings yet
- Course DescriptionDocument6 pagesCourse DescriptionAnnette Aquino GuevarraNo ratings yet
- Narrative (Dec 07 2012)Document3 pagesNarrative (Dec 07 2012)Annette Aquino GuevarraNo ratings yet
- CBCDocument4 pagesCBCAnnette Aquino GuevarraNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- DOC461 Rev C-Laparoscopic UrologyDocument12 pagesDOC461 Rev C-Laparoscopic UrologyMI Kol EuanNo ratings yet
- Banana - Recommendations For Maintaining Postharvest Quality - Postharvest Technology Center - UC Davis PDFDocument3 pagesBanana - Recommendations For Maintaining Postharvest Quality - Postharvest Technology Center - UC Davis PDFFernando SanchezNo ratings yet
- Instructions For Use of Weight Watchers Body Fat Analysis Bathroom ScalesDocument2 pagesInstructions For Use of Weight Watchers Body Fat Analysis Bathroom Scalesjbloggs20070% (1)
- Psychiatric Nursing ProcessDocument24 pagesPsychiatric Nursing ProcessJoric MagusaraNo ratings yet
- Ankle Dislocations Health Conference 2010Document16 pagesAnkle Dislocations Health Conference 2010Aswan IsmailNo ratings yet
- DNC 2Document6 pagesDNC 2Maria VisitacionNo ratings yet
- Pulmonary Function TestsDocument24 pagesPulmonary Function TestsSachin KonkaniNo ratings yet
- Macular Degeneration TreatmentDocument2 pagesMacular Degeneration Treatmentsanjeevan netralayaNo ratings yet
- Assessment of The Visual and Radiographic Changes in Teeth Subjected To High Temperatures: A Forensic StudyDocument6 pagesAssessment of The Visual and Radiographic Changes in Teeth Subjected To High Temperatures: A Forensic StudyInternational Journal of Innovative Science and Research Technology100% (1)
- Individual Assignment A1 Engineering Technologist in Society Clb40002Document13 pagesIndividual Assignment A1 Engineering Technologist in Society Clb40002Anonymous T7vjZG4otNo ratings yet
- Community Acquired Pneumonia Case StudyDocument14 pagesCommunity Acquired Pneumonia Case StudycenakatokNo ratings yet
- Oral Cavity Malignancy-SurgeryDocument62 pagesOral Cavity Malignancy-SurgeryAsif AbbasNo ratings yet
- Drug Price List Updated May 2016Document636 pagesDrug Price List Updated May 2016shajbabyNo ratings yet
- Hazardous Waste Generator Online RegistrationDocument12 pagesHazardous Waste Generator Online RegistrationTricia LacuestaNo ratings yet
- Case Report OA HipDocument38 pagesCase Report OA HipDian RasitawatiNo ratings yet
- Soil AnalysisDocument12 pagesSoil AnalysisSunit Hazarika100% (1)
- Fpsyt 13 1049476Document12 pagesFpsyt 13 1049476putriNo ratings yet
- Endoscopic Evaluation of Post-Fundoplication Anatomy: Esophagus (J Clarke and N Ahuja, Section Editors)Document8 pagesEndoscopic Evaluation of Post-Fundoplication Anatomy: Esophagus (J Clarke and N Ahuja, Section Editors)Josseph EscobarNo ratings yet
- Mental Status Exam findingsDocument1 pageMental Status Exam findingsjkfloresNo ratings yet
- HijamaDocument10 pagesHijamaGendale Am-isNo ratings yet
- Zomeo Mobile AppDocument23 pagesZomeo Mobile AppdrsunilarrakhNo ratings yet
- Sepsis Guidelines: The Work of The Society of Critical Care MedicineDocument3 pagesSepsis Guidelines: The Work of The Society of Critical Care MedicineRomina Zucco ZúñigaNo ratings yet
- Ota Field Placement Evaluation Form - 2022-2023Document9 pagesOta Field Placement Evaluation Form - 2022-2023api-584383908No ratings yet
- Goldfish: Starting Out WithDocument16 pagesGoldfish: Starting Out WithGogo PNo ratings yet
- Family-Fasciolidae Genus: Fasciola: F. Hepatica, F. GiganticaDocument3 pagesFamily-Fasciolidae Genus: Fasciola: F. Hepatica, F. GiganticaSumit Sharma PoudelNo ratings yet
- International Medical Guide For Ships (Quantification Addendum) Third EditionDocument58 pagesInternational Medical Guide For Ships (Quantification Addendum) Third EditionΔΗΜΗΤΡΗΣΧΑΛΑΤΣΗΣ100% (1)
- Narrative TherapyDocument11 pagesNarrative TherapyCamila Orellana100% (1)
- The Difference Between Healthy and Obsessive Love ExplainedDocument4 pagesThe Difference Between Healthy and Obsessive Love Explainedmary grace banaNo ratings yet
- Myocardial Infarction Causes, Symptoms, TreatmentDocument23 pagesMyocardial Infarction Causes, Symptoms, TreatmentAnelle Umali50% (2)
- Mur Form 20v220 - FinalDocument2 pagesMur Form 20v220 - FinalShafiq MohamedtaqiNo ratings yet