Professional Documents
Culture Documents
HTP Final
Uploaded by
Sj 斗力上Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
HTP Final
Uploaded by
Sj 斗力上Copyright:
Available Formats
Learning Objectives
Learning Content
Rationale
Method / Strategy
Rationale
Time / Venue / Resources
Evaluation
After 8 hours of Nurse-PatientSignificant others interaction. The patient-significant others will be able to acquire nowledge, skills and attitude in the care of patient with : Chronic Obstructive Pulmonary Disease Specific Objectives After 2 hour of nursepatient-significant others interaction, the patient-significant others will be able to: 1. Define : Chronic Obstructive Pulmonary Disease
After 1 hour of nurse-patientsignificant others interaction, the patient-significant others will be able to: Also known as, chronic obstructive lung disease (COLD), chronic obstructive airway disease (COAD), chronic airflow limitation (CAL) and chronic obstructive respiratory disease (CORD), is the occurrence of chronic bronchitis or emphysema, a pair Definition of COPD is very important as to not misconcept COPD with other diseases Informal discussion Cooperative learning Visual aids Manila paper Starting an informal discussion will help build rapport. 10 mins At PICU Manila Paper Pentel Pen
Define Chronic Obstructive Pulmonary Disease
of commonly co-existing diseases of the lungs in which the airways become narrowed
2. Identify the risk factors of Chronic Obstructive Pulmonary Disease
Exposure to tobacco smoke Occupational exposure to dusts and chemicals Age. Genetics Oxidative stress Environment Nutrition Socio-economic status
It is an important part of the lecture to be able to identify what caused COPD in the client.
Lecture Visual aids Images
For easy understanding of the subject.
15 mins At PICU Pictures
Identify the risk factorrs of Chronic Obstructive Pulmonary Disease
3. Enumerate the signs and symptoms of Chronic Obstructive Pulmonary Disease
tachypnea, a rapid breathing rate wheezing sounds or crackles in the lungs heard through a stethoscope breathing out taking a longer time than breathing in enlargement of the chest, particularly the front-toback distance (hyperaeration) active use of muscles in the neck to help with breathing breathing through pursed
For supplemental knowledge.
Formal discussion In this phase of Powerpoint teaching we will need a more serious interaction. To gain full attention of the patient and the SO
20 mins. AT PICU Manila Paper Images
Enumerate the signs and symptoms of Chronic Obstructive Pulmonary Disease
lips increased anteroposterior to lateral ratio of the chest (i.e. barrel chest). 4. Show awareness of the disease condition Management Bronchodilators Bronchodilators are medicines that relax smooth muscle around the airways, increasing the calibre of the airways and improving air flow. They can reduce the symptoms of shortness of breath, wheeze and exercise limitation, resulting in an improved quality of life for people with COPD.[49] They do not slow down the rate of progression of the underlying disease.[4] Bronchodilators are usually administered with an inhaler or via a nebulizer. Anticholinergics Anticholinergic drugs cause airway smooth muscles to relax by blocking stimulation from cholinergic nerves. Ipratrop ium provides short-acting rapid relief of COPD symptoms. Tiotropium is a longacting anticholinergic whose regular use is associated with Since the patient already acquired COPD. We prioritize management than prevention. Formal Discussions Powerpoint Quiz Pharmacological : Health Teaching Management of COPD is a very important knowledge. For it will be done wrong, the patient might die. 30 mins. At PICU Laptop Yellow Paper Ballpen Shows awareness of the disease condition
improvements in airflow, exercise capacity, and quality of life. Ipratropium is associated with increased cardiovascularmorbidity.[52] While tiotropium in pill form reduces the risk of all cause mortality, cardiovascular mortality and cardiovascular events[53] that in mist form increases mortality.[54 Corticosteroids Corticosteroids are used in tablet or inhaled form to treat and prevent acute exacerbations of COPD. Well-inhaled corticosteroids (ICS) have not been shown to be of benefit for people with mild COPD, however, they have been shown to decrease acute exacerbations in those with either moderate or severe COPD.[55] They however have no effect on overall oneyear mortality and are associated with increased rates of pneumonia.[43] Other medication Antibiotics (specifically macrolid es such as azithromycin reduce
the number of exacerbations in those who have two or more a year.[56] Supplemental oxygen Supplemental oxygen or oxygen therapy can improve oxygen saturation levels, allowing patients with COPD or low oxygen levels to maintain their mobility and increase their ability to complete activities of daily living (ADL), such as exercise, household chores, shopping, etc. Long-term oxygen therapy for at least 16 hours a day can improve the quality of life and survival for people with COPD and arterial hypoxemia or with complications of hypoxemia such as pulmonary hypertension, cor pulmonale, or secondary erythrocytosis.[57] Hig h concentrations of supplemental oxygen can lead to the accumulation of carbon dioxide andrespiratory acidosis for some people with severe COPD; lower oxygen flow rates are generally safer for these individuals. Another safety issue concerning the use of oxygen for patients with COPD is smoking, because oxygen can act as an oxidizing
agent. Other measures Pulmonary rehabilitation is a program of exercise, disease management and counselling coordinated to benefit the individual.[58] Pulmonary rehabilitation has been shown to improve shortness of breath and exercise capacity. It has also been shown to improve the sense of control a patient has over their disease as well as their emotions Prevention Annual influenza vaccinations and pneumococcal vaccinations. Smoking cessation Occupational Health Air pollution 5. Express his feeling for the plan of care Help the patient and SO to This will express their feelings towards the help us plan of care evaluate if the patient and SO will cooperate in the plan of care and if Informal Discussion For the patient and SO, to be able to express their feelings more. 10 mins. At PICU Express his feelings for the plan of care?
there would be some modification s needed.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Family Medicine Shelf Review - PPTX (Read-Only)Document142 pagesFamily Medicine Shelf Review - PPTX (Read-Only)Alejandro Bocanegra Osuna58% (19)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Anatomy and Physiology CopdDocument15 pagesAnatomy and Physiology CopdAssenav May100% (3)
- Asthma Case StudyDocument4 pagesAsthma Case StudyEver Green100% (2)
- COPD Case PresentationDocument66 pagesCOPD Case PresentationAzima Abdelrhaman100% (4)
- NCP AsthmaDocument2 pagesNCP Asthmaissaiahnicolle0% (1)
- Pulmonary Function TestDocument9 pagesPulmonary Function TestMarivic DianoNo ratings yet
- Prob PrioDocument2 pagesProb PrioSj 斗力上No ratings yet
- Self Care DeficitDocument2 pagesSelf Care DeficitSj 斗力上75% (4)
- NCP & Prio!!!Document45 pagesNCP & Prio!!!Sj 斗力上100% (1)
- Ecologic Model COPDDocument2 pagesEcologic Model COPDSj 斗力上No ratings yet
- Health Teaching Plan - NasoDocument7 pagesHealth Teaching Plan - NasoSj 斗力上No ratings yet
- Decreased Urine OutputDocument3 pagesDecreased Urine OutputSj 斗力上No ratings yet
- NCP Acute PainDocument4 pagesNCP Acute PainSj 斗力上No ratings yet
- MomDocument11 pagesMomSj 斗力上No ratings yet
- EPISTAXIS-bleeding From The Nose (Most Common) Etiology (Cause)Document34 pagesEPISTAXIS-bleeding From The Nose (Most Common) Etiology (Cause)Julliza Joy PandiNo ratings yet
- Flixotide Nebules Pi 006 ApprovedDocument10 pagesFlixotide Nebules Pi 006 ApprovedTampan BeraniNo ratings yet
- Art. - Qual - of Life AsthmaDocument6 pagesArt. - Qual - of Life AsthmaMaria MariaNo ratings yet
- Cough Triggers and Their Pathophysiology in Patients With Prolonged or Chronic CoughDocument10 pagesCough Triggers and Their Pathophysiology in Patients With Prolonged or Chronic CoughZetian QinNo ratings yet
- 7081 - PHARMA - AnnualReport - 2001-12-31 - Pharma-OpsActivities-Achievements (795KB) - 583228015Document35 pages7081 - PHARMA - AnnualReport - 2001-12-31 - Pharma-OpsActivities-Achievements (795KB) - 583228015surayaNo ratings yet
- Dr. Elly Nurus Sakinah 2010Document23 pagesDr. Elly Nurus Sakinah 2010udunk adhinkNo ratings yet
- Invasive Mechanical Ventilation in COPD and Asthma: ReviewDocument11 pagesInvasive Mechanical Ventilation in COPD and Asthma: ReviewHerbertNo ratings yet
- Drug Study LCPDocument3 pagesDrug Study LCPalleen_viaNo ratings yet
- Anti-Asthmatic Agents: Visit: For More Ppt'sDocument38 pagesAnti-Asthmatic Agents: Visit: For More Ppt'sGANESH KUMAR JELLANo ratings yet
- Drugs Affecting The Respiratory SystemDocument4 pagesDrugs Affecting The Respiratory SystemJerica Jaz F. Vergara100% (1)
- UTS - Small Volume Nebulizer Aerosol TreatmentsDocument5 pagesUTS - Small Volume Nebulizer Aerosol TreatmentsQumairy LutfiyahNo ratings yet
- Chronic Obstructive Pulmonary Disease: A Case Presentation OnDocument95 pagesChronic Obstructive Pulmonary Disease: A Case Presentation OnJunery Bagunas100% (2)
- Full Download Daviss Drug Guide For Nurses 16th Edition Vallerand Test BankDocument32 pagesFull Download Daviss Drug Guide For Nurses 16th Edition Vallerand Test Bankjaydejakabfx100% (32)
- Therapeutic Index FinalDocument432 pagesTherapeutic Index FinalhossainctgNo ratings yet
- Tribute TrialDocument9 pagesTribute TrialMr. LNo ratings yet
- Unit V Pulmonary NursingDocument22 pagesUnit V Pulmonary Nursingtamtamtamtama0No ratings yet
- Summary of Product Characteristics, Labelling and Package LeafletDocument44 pagesSummary of Product Characteristics, Labelling and Package LeafletamineNo ratings yet
- 04 Chapter Respiratory SystemDocument18 pages04 Chapter Respiratory SystemMSKCNo ratings yet
- GOLD 2019 Slide SetDocument135 pagesGOLD 2019 Slide SetIhsan KNo ratings yet
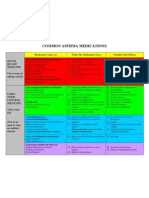
- Common Asthma MedicationsDocument1 pageCommon Asthma MedicationsHeart of the Valley, Pediatric CardiologyNo ratings yet
- Management of Asthma: Alsalman A. Anam Gullas College of MedicineDocument16 pagesManagement of Asthma: Alsalman A. Anam Gullas College of MedicineAlsalman AnamNo ratings yet
- SFP-Vol392 30MCQs PDFDocument4 pagesSFP-Vol392 30MCQs PDFdeepanshi vashishthaNo ratings yet
- Bronchial Asthma and ManagementDocument43 pagesBronchial Asthma and ManagementMarius-Sorin CionteaNo ratings yet
- Asthma COPD DrugsDocument63 pagesAsthma COPD DrugsSimbarashe KanyeraNo ratings yet