Professional Documents
Culture Documents
Airway, Drips and ECG
Uploaded by
drsamnCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Airway, Drips and ECG
Uploaded by
drsamnCopyright:
Available Formats
PRACTICAL ASPECTS OF ANAESTHESIA: AIRWAY, DRIPS AND ELECTROCARDIOGRAM
Maintenance of the Airway
Introduction Maintenance of a clear airway is of crucial importance during anaesthesia and intensive care. Respiratory obstruction, usually due to the tongue falling back onto the pharynx, is the major cause of morbidity and mortality during general anaesthesia particularly in the recovery phase. The principles employed to avoid this problem in the perioperative period are applicable in other emergency situations such as following drug overdose, airway trauma and cardiac arrest. Recognition of Airway Obstruction Airway obstruction in the conscious patient is easily recognised as it leads to strenuous efforts on the part of the patient to overcome it. However, the unconscious patient may not exhibit classical compensatory signs when obstructed. One sees paradoxical chest movement, where the upper abdomen and chest see-saw during attempted inspiration, the chest retracting and the abdomen sticking out. Lack of air entry and exit means that air movement cannot be detected by listening at the mouth, and obviously the patient will eventually become cyanosed. Application of a bag and mask (e.g. Waters circuit) and observation of bag movement provides conclusive proof.
Sites and Treatment of Airway Obstruction
Nasal passages Although the nasal passages are the 'normal' portal for air from atmosphere to lungs, obstruction does not usually cause problems as air may equally well pass via the buccal cavity. However, neonates are inveterate 'nose breathers' and do not adopt mouth breathing easily, even when the nasal airway is totally obstructed, e.g. from choanal atresia. Insertion of an oral airway and placement of the infant in the prone position may allow temporary respite, but often surgical relief of the obstruction is necessary as an emergency. Buccal cavity By far the commonest cause of obstruction in the mouth is relaxation of the jaw muscles due to anaesthesia or
any central nervous system depressant (e.g. head injury, alcohol, benzodiazepines). The tongue falls back onto the posterior wall of the pharynx thus preventing air passage. (Figure 1).
Figure 1: Airway obstruction: (a) The normal upper airway: anatomical sites of obstruction. (b) Obstruction due to tongue falling back in the unconscious patient Luckily this is also the easiest form of obstruction to treat. In the anaesthetised patient, the lower jaw is mechanically lifted forwards taking the tongue with it and thus clearing the airway. This manoeuvre may be combined with insertion of an oral airway that mechanically interposes itself between the pharynx and the tongue (Figure 2).
Figure 2: Re-establishment of patent airway by insertion of oral (Guedel) airway
The patient who is unconscious from other causes or has a full stomach, should be turned on to the side with a head down tilt. Not only does this usually 'automatically' clear the airway by allowing the tongue to fall away from the pharynx, but should vomiting occur, it is much less likely to be aspirated. All unconscious patients should be recovered on their sides. Other causes of airway obstruction in the mouth are much less common. In the neonate, maldevelopment of the upper jaw with a large tongue pushing back against the pharynx (e.g. Pierre Robin syndrome) causes respiratory obstruction that may need urgent treatment. The tongue is stitched and pulled forward, and the baby nursed prone. Trauma to the buccal cavity may lead to mechanical obstruction, e.g. by teeth, dentures or oedema of the tongue and pharynx which prevents free passage of air. Apart from the general measurements mentioned above, endotracheal intubation may be required. Infectious causes in the mouth and pharynx, e.g. Ludwig's angina and retropharyngeal abscess, cause obstruction by swelling. Foreign bodies, especially vomitus, should always be sought for and cleared manually in suspect cases. Epiglottis, larynx and trachea Sudden obstruction is commonly due to infection (acute epiglottitis) trauma or foreign body aspiration, especially particulate matter in vomitus. If this cannot be removed manually or by instrumentation through the mouth, cricothyrotomy or tracheostomy may be necessary to bypass the obstruction. Below the level of the trachea, blockage of air passages does not produce complete obstruction so is not dealt with further here.
Special Techniques
Endotracheal intubation (ETI)
Relief of airway obstruction by the methods outlined above may only provide temporary relief prior to definitive ETI. To accomplish this skilfully and atraumatically requires considerable practical experience. The practice of some 200 endotracheal intubations is the minimum that most anaesthetists in training need to feel reasonably confident. This is usually accomplished in the first six months of training. There is great variability in the anatomy of the region, so unexpected difficulties arising in this manoeuvre are not uncommon. As a life-saving measure, non-anaesthetists have a better chance of effectively providing respiratory support with a bag and mask (and airway if needed), than unsuccessfully attempting to place an endotracheal tube. Turning the patient on the side and head down, with careful observation and frequent suction of the oropharynx, is usually adequate to prevent gross inhalation of stomach contents. Whilst preparations are made, it is important that the airway is maintained by other means as outlined above, and the patient fully oxygenated. Equipment required (Figure 3) 1. A pressurised source of oxygen and gas delivery system; a self-inflating bag is also suitable 2. Mask and airway of suitable size (a mask size of 3 or 4 with a size 2 Guedel airway is suitable for female adults, with one size bigger for males) 3. A cuffed endotracheal tube (ETT) for oral use (these are numbered according to their internal diameter in mm. A size 8 is suitable for females and 9 for males. In the emergency situation smaller sized tubes should be available) 4. A laryngoscope of appropriate size (a Macintosh size 3 or 4 for adults) 5. A syringe and clamp for cuff inflation, tube ties, etc 6. Intubating forceps (Magill) for guiding the ETT and also for removing foreign bodies 7. Drugs (such as i.v. anaesthetics and sedatives, neuromuscular blockers and atropine) 8. A good suction apparatus
Figure 3: Endotracheal intubation trolley
Technique The patient is turned onto the back and a pillow placed underneath the head. This flexes the neck so that the chin is directed towards the chest. Pulling back on the chin towards the operator then extends the head. This 'sniffing the morning air' position is designed to align the planes of the mouth with that of the larynx. Separating the lips and pulling on the upper jaw and lip with the index finger opens the mouth. The laryngoscope is held in the left hand, and enters the mouth with the blade directed towards the right tonsil. On reaching this level, the blade is swept to the midline, keeping the tongue on the left, and out of sight. At this point the epiglottis comes into view (Figure 4).
Figure 4: Principles of visualisation of the larynx with laryngoscope prior to endotracheal intubation. (a) Shows the patient in the incorrect position prior to attempted intubation. The greater the angle of a the greater the difficulty in visualising the larynx. (b) Shows the position with the neck flexed on a pillow and the head extended ("sniffing the morning air"). Angle a is now minimised, especially if gentle traction is exerted on the laryngoscope in the direction shown in A (i.e. up towards the ceiling, NOT rotated) and gentle pressure applied just below the cricoid cartilage (B). It is easy to see that the visual and laryngeal planes are now more closely aligned. The blade is gently advanced until it reaches the vallecula, i.e. the angle between the base of the tongue and epiglottis. It is important to get the earliest view of the epiglottis and not lose sight of it, so as to avoid going too far and misinterpreting the oesophagus for the larynx. At this stage the whole laryngoscope is lifted upwards and away from the operator so that the larynx comes into view. This may also require pressure on the trachea just below the cricoid ring to produce optimal alignment (Figure 4). The ETT is taken in the right hand with the inner curve of the tube facing the right side of the mouth so as to minimally impede the view of the larynx as the tube is inserted. If possible, observe the tube entering the larynx and push it in only until the cuffed portion disappears beyond the cords. This avoids inadvertent endobronchial intubation. The cuff is inflated to provide an airtight seal and the bag squeezed to ascertain correct placement of the tube by listening to both sides of the chest with a stethoscope.
Laryngeal mask airway (LMA) The introduction of the laryngeal mask airway markedly facilitated the management of the airway during anaesthesia. In the vast majority of adult patients it provides a reliable airway, suitable for 'gentle' positive pressure ventilation but providing limited protection against aspiration of regurgitated gastric contents. It is technically much easier to insert a laryngeal mask airway than an endotracheal tube. The procedure does not require a laryngoscope and the successful insertion is less dependent on anatomical variations from patient to patient. For these reasons it is easier to acquire the skill of inserting the laryngeal mask airway than an endotracheal tube; in the future, the device may well find its place in resuscitation kits as an alternative to the endotracheal tube or when intubation proves difficult. The device is illustrated in Fig. 9.5; the external appearance of the airway, once inserted, is identical to that of an endotracheal tube. A large pear-shaped cuff is designed to fit in the oropharynx and once inflated with approximately 40 ml of air, it pushes the base of the tongue forwards. In its original 1981 design (by Dr Archie Brain, then at the London Hospital in London), the laryngeal mask airway was constructed from a cut endotracheal tube joined to a cuff from a Goldman dental nasal mask. The masks available now are made of silicon rubber and can withstand many autoclave sterilisations. The device must be well lubricated before insertion and the patient's head positioned as if for endotracheal intubation. The insertion is facilitated by pulling the jaw forwards and by the insertion of two gloved fingers in the mouth drawing the tongue downwards and forwards as shown in Figure 5.
Figure 5 Laryngeal Mask (a) the mask (b) in correct position
Care of Unconscious Patients : Other Aspects Regardless of the cause, unconsciousness also means that the protective reactions to pain and discomfort are absent. Circumstances permitting, the patient should be put on the side with a slight head down tilt (e.g. following a grand mal convulsion). The cornea of the eye may dry and suffer irreversible damage due to absence of tears and blinking; so, eyes should be taped closed during unconsciousness. Shoulder and hip joints should be protected from pulling and excessive passive movement to prevent dislocation. Peripheral nerves may suffer prolonged compression or stretching, so watch out for hard, sharp edges pressing on the lateral surface of the leg (superficial peroneal nerve) or the side of the face (facial nerve). The brachial plexus is perhaps the most vulnerable to stretching and compression due to over-extension of the arm or by keeping the patient in the lateral position without additional support of the rib cage. Maintenance of body temperature is important. Wet garments must be replaced soon after surgery and the patient kept well covered with blankets if ambient temperature is below 24 deg. C. During prolonged major surgery a warming blanket should be used. Finally, remember that the unconscious patient should be turned in bed or trolley at regular intervals of 30 minutes to relieve effects of pressure on the skin, and great care must be exercised not to drop the unconscious patient on the floor on transferring to or from bed!
Setting up an Intravenous Infusion
Introduction This is best learnt initially by doing it in the skills laboratory. Beginners should practice the whole sequence many times over, starting with unwrapping the giving set, the bag of intravenous fluid and the cannula (Figure 6).
Figure 6: Essential equipment needed to set up a drip. (a) Bag of fluid (checked for content and expiry date) for infusion. (b) Infusion set for giving blood (two chamber with ball float. Squeezing lower chamber causes the ball to rise up and prevent back flow during rapid infusion requirements (c) Intravenous cannula showing various components. The proper practice of connecting the three parts without contamination and the presence of air bubbles can only be learnt by watching an experienced person first and then doing it under supervision. The practice of some 50 cannulations is perhaps the minimum required to feel some confidence with the technique (or to give it up!). Only short-term cannulation will be discussed. An experienced person best does long-term cannulation (weeks rather than days) through a large deep vein (subclavian or internal jugular), with rigorous aseptic conditions.
Venous cannulation is best-practised initially in anaesthetised patients. In awake patients any cannula bigger than 22 G should not be inserted without anaesthetising the skin to be punctured with a small amount of 1% lignocaine through a 25 G needle. In children and very nervous adults, a topical local anaesthetic such as amethocaine gel or EMLA cream can be applied to the area for 30 minutes prior to cannulation. Choice of vein The first important step is to choose the appropriate vein for the purpose. Except in very special circumstances, only the superficial veins of forearm and hand should be used. The areas of the wrist and elbow should be avoided because this requires splinting of the joint and there is increased likelihood of the cannula becoming dislodged or the vein thrombosed. A 'Y' junction in the forearm is probably the best choice for beginners, because the entry into the vein is more obvious. Choice of cannula There is no evidence that different makes of cannula has any influence upon the success of peripheral vein cannulation. Of the presently available models perhaps only cost should be considered in the choice (Figure 7).
Figure 7: Types of cannula
Depending upon the objective in mind, the appropriate size of cannula should be chosen. Types of i.v. cannula for specific requirements The following table gives an idea of the size of cannula you might need for different clinical situations Application Continuous infusion of drugs (pumped) Normal daily fluid replacement Slow blood transfusion or intraoperative fluids Rapid blood transfusion SWG - Standard wire gauge. Internal Gauge diameter in mm 0.8-1.0 1.2 1.7 2.0-2.4 SWG 22-20 18 16 14-12 Max flow rate ml min-1 25-50 65 150 200-300
Preparation of insertion site A tourniquet, blood pressure cuff or a helpers hand must be placed proximal to the puncture site to distend the vein. The pressure applied round the arm must be such that blood flow in the arteries is not compromised (check for radial pulse if in doubt). If vein distension is insufficient, gently tapping it at a rate of 3-4 s-1 for 1 minute, or application of a warm towel for 2-3 minutes, usually produces a rewarding improvement. The operator must wash his hands and put on gloves before starting the procedure, but the value and techniques of disinfecting the site of puncture are much debated. If a disinfectant is used (alcohol, chlorhexidene or iodine-based preparations) at least 1 minute should be allowed for it to take effect prior to puncture. Shaving of the skin produces small abrasions which alter the skin flora, and should be done only to facilitate the application of adhesive tape. Technique of insertion The left hand of the operator holds the patient's arm (or hand) steady, the thumb pulling the skin taut, distally to the puncture site, without collapsing the vein. With the bevel of the needle facing upwards, the cannula/needle assembly is advanced through the skin a few mm from the vein, using a quick jabbing action, at an angle of approximately 20 degrees to the surface of the skin. Note that the assembly must be held by the
hub of the needle and not by the hub of the cannula. The cannula is then further advanced until it enters the vein with a feel of a 'click' followed by flash-back of blood into the hub. It is then advanced some 3-5 mm inside the vein, the needle pulled out some 10 mm and the whole assembly advanced until the cannula is fully inserted (Figure 8).
Figure 8: Insertion of cannula into vein. Arrows indicate direction of pull
Fxation of the cannula and maintenance of flow There is an infinite variety of methods of securing the cannula to the skin. Good common sense is the most important factor. Even the most perfect way of taping the cannula in situ is easily defeated by a moist or greasy skin. If the drip is to be used in the awake patient over a few days, it is worth spending a bit more time in devising a firm way of securing the cannula in place (Figure 9).
Figure 9: Technique of securing cannula and drip set in the arm. (a) Arrows indicate direction of forces which may act to pull cannula out (1) and to keep cannula in place (2). Tape place directly over the injection site should be sterile. When secured as in (a), a loop is made in the giving set and then the whole drip is secured with 3 inch tape as indicated. If the cannula has an integral injection port then this must be kept free of tape. Alternatively a short extension with three way tap can be used if injection of drugs is required. The important aspects of the technique preventing accidental removal of the cannula are: 1. The tensile strength of the tape (depends on width) 2. The adhesiveness of the tape (depends on type) 3. The area of adhesive surface in contact with dry skin and with the cannula 4. The direction of the tape applied on the skin with respect to the cannula 5. Presence of hair 6. Shielding of the giving set from potential sources of pulling The important factors in preserving the patency of the drip are those that prevent thrombosis and infection. The longer the length of cannula inside the vein the higher the incidence of thrombosis; cannulae placed at the wrist or elbow tend to cause thrombosis more rapidly due to trauma to vein wall. Injection of drugs through the drip increases the chances of thrombophlebitis; the irritant action of drugs and hypertonic or acidic solutions has the same effect. Daily dressing of the puncture site and the use of local antiseptic agents is mandatory. In some hospitals in other European countries (but not the US) the routine practice of inserting a new cannula in a different site every 24 hours (also changing the giving set and fluid container) has been found to be cost effective. At the first signs of local inflammation the cannula must be removed and replaced elsewhere, preferably in the other arm.
Monitoring the ECG during anaesthesia
Introduction It is only in the last 30 years that ECG monitoring during anaesthesia has become routine, even for minor operations in healthy patients. Patients with pre-existing cardiac disease and ECG changes obviously benefit from ECG monitoring, but what changes and abnormalities can be detected from its use in the previously fit patient? First, it is necessary to consider apparatus and lead placement (Figure 10).
Figure 10: ECG monitoring during anaesthesia and Intensive Care (a) the CM5 lead placement. (b) Common types of rhythm disturbance during anaesthesia.
Apparatus and lead placement The conventional 12 lead ECG is obtained using an electrocardiograph from which a printed record is obtained for analysis. For 'real time' monitoring during anaesthesia and in the intensive care unit (ICU) an oscilloscope is used on which the electrical signal from the heart is directly displayed. Most units also employ 'memory' devices which enable abnormalities to be stored and separately displayed using a 'freeze' and 'cascade' facility. For permanent records, a separate printer is necessary, although these are not routinely available in theatre. It would obviously be inconvenient to place electrodes on every anaesthetised patient to allow a full 12 lead record to be obtained. Indeed, most theatre monitors are only equipped for 'bipolar' electrodes (3 lead systems) and not those necessary for the augmented or chest leads obtainable from the 12 lead ECG. There is also often no provision for lead selection. In addition, frequent movement and contact with the patient by the surgical and anaesthetic team has necessitated the use of 'filters' which cut out spurious noise and movement artefact, even including diathermy suppression in the more sophisticated units. Although the signal obtained is clearer, there is an unfortunate tendency for it to be degraded, and as a result, the ECG, particularly the ST segment changes (indicative of ischaemia, see below) are more difficult to interpret. Switching the filters off is possible in some units by changing from the 'monitoring' to the 'diagnostic' mode.
With only three leads available, it is important that lead placement is optimised to produce the most useful information. The bipolar leads involve measurement and display of the difference in electrical potential (from the heart) between two points on the body surface. Conventionally, the three limb leads are utilised, I, II and III. 'I' measures the difference in potential between right arm and left arm, 'II' right arm and left leg, 'III' left arm and left leg. The 3 leads include two that are 'active', and one that is 'inactive' (earth). The former two may be placed to record leads I, II or III, the inactive lead being placed anywhere on the body surface. However, the information which primarily needs to be obtained relates to dysrhythmia and ischaemia detection. Whilst lead II is useful for the diagnosis of supraventricular dysrhythmias, none of the three bipolar leads is really suitable for detection of ischaemia. With regard to the conventional 12 lead ECG, it has been found that about 90% of detectable ischaemic changes are present in lead V5. Although this cannot be measured directly with a 3 lead ECG, a modified V5 (CM5) system can be employed. This involves placing the red active lead (usually designated 'right arm') on an electrode over the upper right of the sternum, and the other ('left arm') yellow electrode placed in the usual V5 position (5th intercostal space under the left nipple.) The inactive green lead is usually placed on the left shoulder. This CM5 configuration not only produces a modified V5 record for ischaemia detection, but also is excellent for dysrhythmia monitoring as it is aligned in the same direction as lead II. One also notes, in practice, that the amplitude of the signal is greater in this position (as one electrode is over the left ventricle), allowing for the gain (and also the noise) of the ECG amplifier to be reduced. Dysrhythmia detection Supraventricular dysrhythmias These occur frequently in normal anaesthetised subjects, but are rarely dangerous. The sino-atrial (SA) node is particularly susceptible to shielding or suppression by halothane, especially if the arterial carbon dioxide tension (PaCO2) is also low. This results in a junctional rhythm with absent or abnormal P waves. Sinus bradycardia frequently follows vagal stimulation (such as from pulling on the mesentery or intraocular manipulations), and may be prevented or treated with atropine. Atrial premature contractions (APCs) are commonly caused by stimulation under too light anaesthesia (particularly dental extraction). In the latter case, treatment with a beta blocker may be necessary. Ventricular dysrhythmias
These occur for a variety of reasons. Dental extraction is a common cause of multi-focal ectopics occurring in the otherwise normal patient. In rare circumstances this may lead to ventricular tachycardia or even fibrillation. Again, treatment with beta blockers or lignocaine usually reduces their frequency and severity. If the sinus rate slows excessively (see above), 'opportunist' ectopics may occur, but these are usually easily overridden by simply increasing the heart rate with atropine. A common accompaniment of halothane anaesthesia is ventricular bigeminus, particularly if there is an element of CO2 retention during spontaneous respiration. This is not usually serious, but can be alleviated by reduction of halothane concentration and/or lowering the PaCO2 by ventilatory assistance for a short period. In more resistant cases, halothane may have to be discontinued and substituted by other inhalational agents less likely to cause dysrhythmias such as enflurane, isoflurane, sevoflurane or desflurane. The concurrent administration of adrenaline (during local anaesthetic infiltration) often precipitated serious ventricular dysrhythmias in association with high concentrations of halothane particularly if associated with CO2 retention. Halothane is now rarely used and happily dysrhythmias are much less common with agents such as isoflurane, sevoflurane and desflurane. Even so, the dose of adrenaline should be limited to about 0.15 ml Kg-1 of a 1:100 000 mixture (10 ug ml-1) over a 10 minute period, and hypoxia and hypercarbia avoided. Ischaemia detection During anaesthesia, the principal method of ischaemia detection involves the ST segment. Provided the machine is correctly calibrated (1 mV for 1 cm upward deflection) and the filters switched off, ST segment depression of more than 1 mm signifies impending subendocardial ischaemia. This usually indicates that the oxygen supply/demand ratio of the heart has been adversely affected, e.g. oxygen demand is excessive, as in tachycardia and hypertension in the patient with pre-existing ischaemic myocardium, or supply is reduced as in excessive hypotension. Correction of these factors should return the ST segment to normality. ST segment elevation is less common, but may signify full thickness myocardial ischaemia with impending infarction. If possible surgery should be completed expeditiously and anaesthesia discontinued, as it is extremely likely to lead to a 'full blown' myocardial infarction. Conclusion Even in the 'normal' patient, ECG monitoring gives extremely useful information which can be appropriately acted upon with benefit to the patient, as indicated above. However, a normal ECG has no absolute correlation with blood pressure and perfusion, it simply reflects the electrical (and not mechanical) activity of the heart.
You might also like
- Articles PracticalDocument4 pagesArticles PracticaldrsamnNo ratings yet
- IELTS Speaking Criteria Public Version PDFDocument1 pageIELTS Speaking Criteria Public Version PDFDiana Laura Durán Chablé100% (1)
- Approaches To Management of Acute Pain 1Document22 pagesApproaches To Management of Acute Pain 1drsamnNo ratings yet
- Oxygen Therapy and Oxygen ToxicityDocument8 pagesOxygen Therapy and Oxygen ToxicitydrsamnNo ratings yet
- Simple EmergenciesDocument177 pagesSimple Emergenciesharsh89100% (1)
- Arterial Blood Gases and Acid Base BalanceDocument12 pagesArterial Blood Gases and Acid Base BalancedrsamnNo ratings yet
- Common Antibiotic Questions and TopicsDocument2 pagesCommon Antibiotic Questions and TopicsdrsamnNo ratings yet
- Public Writing Band DescriptorsDocument2 pagesPublic Writing Band DescriptorsKaveh JalaliNo ratings yet
- Heart FailureDocument10 pagesHeart FailuredrsamnNo ratings yet
- Clinical Trials, 6 Principles: N.B. Patients Must Now Give Written Consent Before Entering A Clinical TrialDocument2 pagesClinical Trials, 6 Principles: N.B. Patients Must Now Give Written Consent Before Entering A Clinical TrialdrsamnNo ratings yet
- Head and NeckDocument11 pagesHead and NeckdrsamnNo ratings yet
- r4f Pastest MnemonicsDocument23 pagesr4f Pastest MnemonicsplayuhzNo ratings yet
- Acute Respiratory FailureDocument8 pagesAcute Respiratory FailureCayunk NorlianaNo ratings yet
- Layers of Abdominal Wall When Performing An AppendicectomyDocument2 pagesLayers of Abdominal Wall When Performing An AppendicectomydrsamnNo ratings yet
- Skin As An Organizing Model: What Is It? (Anatomy)Document11 pagesSkin As An Organizing Model: What Is It? (Anatomy)Chemist Mary MouresNo ratings yet
- Science 2009-03-13Document112 pagesScience 2009-03-13drsamnNo ratings yet
- Lab FaqsDocument384 pagesLab FaqsPriyanka SinghNo ratings yet
- Science 2009-01-30Document96 pagesScience 2009-01-30drsamnNo ratings yet
- Biology Under Construction - in Vitro Reconstitution of Cellular FunctionDocument8 pagesBiology Under Construction - in Vitro Reconstitution of Cellular FunctiondrsamnNo ratings yet
- MRCS1 2brochureDocument12 pagesMRCS1 2brochuredrsamn100% (2)
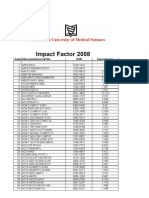
- Impact Factor 2008Document119 pagesImpact Factor 2008abood127No ratings yet
- Wound Repair and RegenerationDocument8 pagesWound Repair and RegenerationdrsamnNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Surgical Instruments 3Document110 pagesSurgical Instruments 3Gerald Resubal OriñaNo ratings yet
- MinitrephDocument8 pagesMinitrephdisk_la_poduNo ratings yet
- IV Cannulation OET ReadingDocument20 pagesIV Cannulation OET ReadingKush Gurung70% (10)
- Tear Trough Filler Techniques Utilizing Hyaluronic Acid A Systematic Review - Rao, 2022Document9 pagesTear Trough Filler Techniques Utilizing Hyaluronic Acid A Systematic Review - Rao, 2022Rafael Autran Cavalcante AraújoNo ratings yet
- Prymax Healthcare LLPDocument24 pagesPrymax Healthcare LLPrythmdipenNo ratings yet
- PLS Sistem BroşürDocument12 pagesPLS Sistem BroşürAnar MaharramovNo ratings yet
- Introcan Safety Deep Access: Cannulation Under UltrasoundDocument1 pageIntrocan Safety Deep Access: Cannulation Under UltrasoundsantoniloyNo ratings yet
- Implanon Insertion Revised ChecklistDocument2 pagesImplanon Insertion Revised ChecklistDerese GosaNo ratings yet
- A 10-Point Plan For Avoiding Hyaluronic Acid Dermal Filler-Related Complications During Facial Aesthetic Procedures and Algorithms For ManagementDocument9 pagesA 10-Point Plan For Avoiding Hyaluronic Acid Dermal Filler-Related Complications During Facial Aesthetic Procedures and Algorithms For Managementleenatalia93100% (1)
- Iridex Endo ProbesDocument8 pagesIridex Endo ProbeslatentheatNo ratings yet
- Livanova - Bi-Flow CannulaDocument3 pagesLivanova - Bi-Flow CannulaAhmadNo ratings yet
- Demonstration On Iv CannulationDocument54 pagesDemonstration On Iv CannulationAnusha100% (1)
- Choose From Our Extensive Inventory of Biopsy and Breast Lesion DevicesDocument32 pagesChoose From Our Extensive Inventory of Biopsy and Breast Lesion DevicesjackxrdNo ratings yet
- Classic Techniques in Medicine: Methods of Obtaining Peripheral Venous Access in Di Ycult SituationsDocument4 pagesClassic Techniques in Medicine: Methods of Obtaining Peripheral Venous Access in Di Ycult SituationsClarissa GuifayaNo ratings yet
- Eopa Arterial Cannulae: IdealDocument2 pagesEopa Arterial Cannulae: IdealHeart SurgeryNo ratings yet
- Bone Grafting HCP Spine Marrow Cellution Bma Surgical Technique Guide Pmd018207Document16 pagesBone Grafting HCP Spine Marrow Cellution Bma Surgical Technique Guide Pmd018207Satyam PatelNo ratings yet
- COMPLICATII TARDIVE DUPA INJECTAREA DE ACID HIALURONIC IN SCOP ESTETIC SI MANAGEMENTUL LOR Ro 399Document21 pagesCOMPLICATII TARDIVE DUPA INJECTAREA DE ACID HIALURONIC IN SCOP ESTETIC SI MANAGEMENTUL LOR Ro 399tzupel4No ratings yet
- Tissue Augmentation in Clinical PracticeDocument402 pagesTissue Augmentation in Clinical PracticeFabiola Camberos Ruíz100% (8)
- Guideline of ExtravasationDocument35 pagesGuideline of ExtravasationAura Lorena Rivas Zambrano100% (1)
- PML-PC/4000/11-09 - Touching Life with Care: POLYMED's Medical Device CatalogDocument60 pagesPML-PC/4000/11-09 - Touching Life with Care: POLYMED's Medical Device CatalogsbosNo ratings yet
- AIIMS Delhi Nursing Officer Exam 2019 Memory Based Question Paper SummaryDocument40 pagesAIIMS Delhi Nursing Officer Exam 2019 Memory Based Question Paper Summaryrejin rejinrNo ratings yet
- Techniques of Blood Collection in Laboratory Animals by Neelam RajDocument6 pagesTechniques of Blood Collection in Laboratory Animals by Neelam RajNeelam Raj ThakurNo ratings yet
- Shiley Tracheostomy SpecificationsDocument2 pagesShiley Tracheostomy Specificationsmomirc1No ratings yet
- BD Hypo Catalog PDFDocument10 pagesBD Hypo Catalog PDFChaitra Kshathriya MNo ratings yet
- Medical Supplies Philippine Heart Center 2015Document146 pagesMedical Supplies Philippine Heart Center 2015Emmeline Roy DoblaNo ratings yet
- NCM112 Skills Lab: Oxygen Therapy via Nasal CannulaDocument4 pagesNCM112 Skills Lab: Oxygen Therapy via Nasal CannulaMark Zedrix MediarioNo ratings yet
- MedicalDocument3 pagesMedicalmandible removerNo ratings yet
- Biopsy NeedlesDocument26 pagesBiopsy NeedlesMahdi Saleh AishanNo ratings yet
- The Pocket Book of Small Animal Tips For VetsDocument52 pagesThe Pocket Book of Small Animal Tips For VetsYudith Novida100% (1)
- Med Price RequestDocument6 pagesMed Price RequestJohann CostalesNo ratings yet