Professional Documents
Culture Documents
Progesterone
Uploaded by
Violeta NitaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Progesterone
Uploaded by
Violeta NitaCopyright:
Available Formats
Progesterone also known as P4 (pregn-4-ene-3,20-dione) is a C-21 steroid hormone involved in the female menstrual cycle, pregnancy (supports gestation)
and embryogenesis of humans and other species. Progesterone belongs to a class of hormones called progestogens, and is the major naturally occurring human progestogen. Progesterone is commonly manufactured from the yam family, Dioscorea. Dioscorea produces large amounts of a steroid called diosgenin, which can be converted into progesterone in the laboratory. Chemistry Progesterone was independently discovered by four research groups.[1][2][3][4] Willard Myron Allen co-discovered progesterone with his anatomy professor George Washington Corner at the University of Rochester Medical School in 1933. Allen first determined its melting point, molecular weight, and partial molecular structure. He also gave it the name Progesterone derived from Progestational Steroidal ketone.[5] Like other steroids, progesterone consists of four interconnected cyclic hydrocarbons. Progesterone contains ketone and oxygenated functional groups, as well as two methyl branches. Like all steroid hormones, it is hydrophobic. [edit] Sources [edit] Animal Progesterone is produced in the ovaries (specifically after ovulation in the corpus luteum), the adrenal glands (near the kidney), and, during pregnancy, in the placenta. Progesterone is also stored in adipose (fat) tissue. In humans, increasing amounts of progesterone are produced during pregnancy:
Initially, the source is the corpus luteum that has been "rescued" by the presence of human chorionic gonadotropins (hCG) from the conceptus. However, after the 8th week production of progesterone shifts to the placenta. The placenta utilizes maternal cholesterol as the initial substrate, and most of the produced progesterone enters the maternal circulation, but some is picked up by the fetal circulation and used as substrate for fetal corticosteroids. At term the placenta produces about 250 mg progesterone per day. An additional source of progesterone is milk products. They contain much progesterone because on dairy farms cows are milked during pregnancy, when the progesterone content of the milk is high. After consumption of milk products the level of bioavailable progesterone goes up.[6]
[edit] Plants
In at least one plant, Juglans regia, progesterone has been detected.[7] In addition, progesteronelike steroids are found in Dioscorea mexicana. Dioscorea mexicana is a plant that is part of the yam family native to Mexico.[8] It contains a steroid called diosgenin that is taken from the plant and is converted into progesterone.[9] Diosgenin and progesterone are found in other Dioscorea species as well. Another plant that contains substances readily convertible to progesterone is Dioscorea pseudojaponica native to Taiwan. Research has shown that the Taiwanese yam contains saponins steroids that can be converted to diosgenin and thence to progesterone.[10] Many other Dioscorea species of the yam family contain steroidal substances from which progesterone can be produced. Among the more notable of these are Dioscorea villosa and Dioscorea polygonoides. One study showed that the Dioscorea villosa contains 3.5% diosgenin. [11] Dioscorea polygonoides has been found to contain 2.64% diosgenin as shown by gas chromatography-mass spectrometry.[12] Many of the Dioscorea species that originate from the yam family grow in countries that have tropical and subtropical climates.[13] [edit] Synthesis [edit] Biosynthesis
Top: Conversion of cholesterol (1) into pregnenolone (3) to progesterone (6). Bottom: Progesterone is important for aldosterone (mineralocorticoid) synthesis, as 17hydroxyprogesterone is for cortisol (glucocorticoid), and androstenedione for sex steroids. In mammals, progesterone (6), like all other steroid hormones, is synthesized from pregnenolone (3), which in turn is derived from cholesterol (1) (see the upper half of the figure to the right).
Cholesterol (1) undergoes double oxidation to produce 20,22-dihydroxycholesterol (2). This vicinal diol is then further oxidized with loss of the side chain starting at position C-22 to produce pregnenolone (3). Biologically, this reaction is catalyzed by cytochrome P450scc. The conversion of pregnenolone to progesterone takes place in two steps. First, the 3-hydroxyl group is oxidized to a keto group (4) and second, the double bond is moved to C-4, from C-5 through a keto/enol tautomerization reaction.[14] This reaction is catalyzed by 3beta-hydroxysteroid dehydrogenase/delta(5)-delta(4)isomerase. Progesterone in turn (see lower half of figure to the right) is the precursor of the mineralocorticoid aldosterone, and after conversion to 17-hydroxyprogesterone (another natural progestogen) of cortisol and androstenedione. Androstenedione can be converted to testosterone, estrone and estradiol. Pregenolone and progesterone can also be synthesized by yeast.[15] a Levels
Progesterone levels (black line) during the menstrual cycle In women, progesterone levels are relatively low during the preovulatory phase of the menstrual cycle, rise after ovulation, and are elevated during the luteal phase. Progesterone levels tend to be < 2 ng/ml prior to ovulation, and > 5 ng/ml after ovulation. If pregnancy occurs, progesterone levels are initially maintained at luteal levels. With the onset of the luteal-placental shift in progesterone support of the pregnancy, levels start to rise further and may reach 100-200 ng/ml at term. Whether a decrease in progesterone levels is critical for the initiation of labor has been argued and may be species-specific. After delivery of the placenta and during lactation, progesterone levels are very low. Progesterone levels are relatively low in children and postmenopausal women.[19] Adult males have levels similar to those in women during the follicular phase of the menstrual cycle. Effects
Micrograph showing changes to the endometrium due to progesterone (decidualization) H&E stain. Progesterone exerts its primary action through the intracellular progesterone receptor although a distinct, membrane bound progesterone receptor has also been postulated.[20][21] Additionally, progesterone is a highly potent antagonist of the mineralocorticoid receptor (MR, the receptor for aldosterone and other mineralocorticosteroids). It prevents MR activation by binding to this receptor with an affinity exceeding even those of aldosterone and other corticosteroids such as cortisol and corticosterone.[22] Progesterone has a number of physiological effects which are amplified in the presence of estrogen. Estrogen through estrogen receptors upregulates the expression of progesterone
receptors.[23] Also, elevated levels of progesterone potently reduce the sodium-retaining activity of aldosterone, resulting in natriuresis and a reduction in extracellular fluid volume. Progesterone withdrawal, on the other hand, is associated with a temporary increase in sodium retention (reduced natriuresis, with an increase in extracellular fluid volume) due to the compensatory increase in aldosterone production which combats the blockade of the mineralocorticoid receptor by the previously elevated level of progesterone.[24] Reproductive system Progesterone is sometimes called the "hormone of pregnancy",[25] and it has many roles relating to the development of the fetus:
Progesterone converts the endometrium to its secretory stage to prepare the uterus for implantation. At the same time progesterone affects the vaginal epithelium and cervical mucus, making it thick and impermeable to sperm. If pregnancy does not occur, progesterone levels will decrease, leading, in the human, to menstruation. Normal menstrual bleeding is progesterone-withdrawal bleeding. During implantation and gestation, progesterone appears to decrease the maternal immune response to allow for the acceptance of the pregnancy. Progesterone decreases contractility of the uterine smooth muscle.[25] In addition progesterone inhibits lactation during pregnancy. The fall in progesterone levels following delivery is one of the triggers for milk production. A drop in progesterone levels is possibly one step that facilitates the onset of labor.
The fetus metabolizes placental progesterone in the production of adrenal steroids. Nervous system Progesterone, like pregnenolone and dehydroepiandrosterone, belongs to the group of neurosteroids. It can be synthesized within the central nervous system and also serves as a precursor to another major neurosteroid, allopregnanolone. Neurosteroids affect synaptic functioning, are neuroprotective, and affect myelination.[26] They are investigated for their potential to improve memory and cognitive ability. Progesterone affects regulation of apoptotic genes. Its effect as a neurosteroid works predominantly through the GSK-3 beta pathway, as an inhibitor. (Other GSK-3 beta inhibitors include bipolar mood stabilizers, lithium and valproic acid.) Other systems
It raises epidermal growth factor-1 levels, a factor often used to induce proliferation, and used to sustain cultures, of stem cells.
It increases core temperature (thermogenic function) during ovulation.[27] It reduces spasm and relaxes smooth muscle. Bronchi are widened and mucus regulated. (Progesterone receptors are widely present in submucosal tissue.) It acts as an antiinflammatory agent and regulates the immune response. It reduces gall-bladder activity.[28] It normalizes blood clotting and vascular tone, zinc and copper levels, cell oxygen levels, and use of fat stores for energy. It may affect gum health, increasing risk of gingivitis (gum inflammation) and tooth decay. It appears to prevent endometrial cancer (involving the uterine lining) by regulating the effects of estrogen.
Adverse effects Progesterone can cause increased fluid retention which may result in epilepsy, migraine, asthma, cardiac or renal dysfunction. Blood clots may develop which can result in strokes and heart attacks which may lead to death or long-term disability; pulmonary embolus or breast cancer can also develop as a result of progesterone therapy. Progesterone is associated with an increased risk of thrombotic disorders such as thrombophlebitis, cerebrovascular disorders, pulmonary embolism, and retinal thrombosis.[29] Common adverse effects include; cramps, abdominal pain, skeletal pain, perineal pain, headache, arthralgia, constipation, dyspareunia, nocturia, diarrhea, nausea, vomiting, joint pain, flatulence, hot flushes, decreased libido, thirst, increased appetite, nervousness, drowsiness, excessive urination at night. Psychiatric effects including depression, mood swings, emotional instability, aggression, abnormal crying, insomnia, forgetfulness, sleep disorders.[29] Less frequent adverse effects which may occur include; allergy, anemia, bloating, cramps, fatigue, tremor, urticaria, pain, conjunctivitis, dizziness, vomiting, myalgia, back pain, breast pain, difficult or painful intercourse, genital itching, genital yeast infection, upper respiratory tract infection, cystitis, dysuria, asthenia, xerophthalmia, syncope, dysmenorrhea, genital pruitis, premenstrual tension, gastritis, urinary tract infection, urinary tract infection, vaginal discharge, pharyngitis, sweating, hyperventilation, vaginal dryness, dyspnea, fever, edema, flu-like symptoms, gastrointestinal discomfort, gas, abdominal swelling, dry mouth, rhinitis, back pain, pruritis, rash, leg pain, skin discoloration, skin disorders, seborrhea, sinusitis, upper respiratory tract infection, asthma, acne, itching, painful or difficult urination, frequent urination.[29] Medical applications The use of progesterone and its analogues have many medical applicationsboth to address acute situations, and to address the long-term decline of natural progesterone levels. Because of the poor bioavailability of progesterone when taken orally, many synthetic progestins have been
designed. However, the roles of progesterone may not be fulfilled by the synthetic progestins which in some cases were designed solely to mimic progesterone's uterine effects. [edit] Bioavailability Progesterone is poorly absorbed by oral ingestion unless micronised and in oil, or with fatty foods; it does not dissolve in water. Products such as Prometrium, Utrogestan, Minagest and Microgest are therefore capsules containing micronised progesterone in oil - in all three mentioned the oil is peanut oil, which may cause serious allergic reactions in some people, but compounding pharmacies, which have the facilities and licenses to make their own products, can use alternatives. Vaginal and rectal application is also effective, with products such as ENDOMETRIN (progesterone) Vaginal Insert 100 mg, approved by the FDA in June 2007 to support embryo implantation and early pregnancy. Other products are CRINONE and PROCHIEVE bioadhesive progesterone vaginal gels (the first progesterone products FDAapproved for use in infertility and during pregnancy) and Cyclogest, which is progesterone in cocoa butter in the form of pessaries. Progesterone can be given by injection, but because it has a short half-life they need to be daily. Marketing of progesterone phamaceutical products, country to country, varies considerably, with many countries having no oral progesterone products marketed, but they can usually be specially imported by pharmacies through international wholesalers. Progesterone can be absorbed through the skin when administered as a skin cream, thus avoiding the breakdown by the liver that occurs when it is ingested.[30] "Natural progesterone" products derived from yams, do not require a prescription. Wild yams contain a plant steroid called diosgenin, however there is no evidence that the human body can metabolize diosgenin into progesterone.[31][32] Diosgenin can however be chemically converted into progesterone in the lab.[16] [edit] Specific uses
Progesterone is used to support pregnancy in Assisted Reproductive Technology (ART) cycles such as In-vitro Fertilization (IVF). While daily intramuscular injections of progesterone-in-oil (PIO) have been the standard route of administration, PIO injections are not FDA-approved for use in pregnancy. A recent meta-analysis showed that the intravaginal route with an appropriate dose and dosing frequency is equivalent to daily intramuscular injections.[33] In addition, a recent case-matched study comparing vaginal progesterone with PIO injections showed that live birth rates were nearly identical with both methods.[34] Progesterone is used to control anovulatory bleeding. It is also used to prepare uterine lining in infertility therapy and to support early pregnancy. Patients with recurrent pregnancy loss due to inadequate progesterone production may receive progesterone. Progesterone is being investigated as potentially beneficial in treating multiple sclerosis, since the characteristic deterioration of nerve myelin insulation halts during pregnancy, when progesterone levels are raised; deterioration commences again when the levels drop.
Vaginally dosed progesterone is being investigated as potentially beneficial in preventing preterm birth in women at risk for preterm birth. The initial study by Fonseca suggested that vaginal progesterone could prevent preterm birth in women with a history of preterm birth.[35]
A subsequent and larger study showed that vaginal progesterone was no better than placebo in preventing recurrent preterm birth in women with a history of a previous preterm birth,[36] but a planned secondary analysis of the data in this trial showed that women with a short cervix at baseline in the trial had benefit in two ways: a reduction in births less than 32 weeks and a reduction in both the frequency and the time their babies were in intensive care.[37] In another trial, vaginal progesterone was shown to be better than placebo in reducing preterm birth prior to 34 weeks in women with an extremely short cervix at baseline.[38] An editorial by Roberto Romero discusses the role of sonographic cervical length in identifying patients who may benefit from progesterone treatment.[39]
Progesterone is used in hormone therapy for transsexual women and other women with intersex conditions - especially when synthetic progestins have been ineffective or caused side-effects - since normal breast tissue cannot develop except in the presence of both progestogen and estrogen. Mammary glandular tissue is otherwise fibrotic, the breast shape conical and the areola immature. Progesterone can correct those even after years of inadequate hormonal treatment. Research usually cited against such value was conducted using Provera, a synthetic progestin. Progesterone also has a role in skin elasticity and bone strength, in respiration, in nerve tissue and in female sexuality, and the presence of progesterone receptors in certain muscle and fat tissue may hint at a role in sexuallydimorphic proportions of those. Progesterone receptor antagonists, or selective progesterone receptor modulators (SPRM)s, such as RU-486 (Mifepristone), can be used to prevent conception or induce medical abortions.
Note that methods of hormonal contraception do not contain progesterone but a progestin. Progesterone may affect male behavior.[40] Progesterone is starting to be used in the treatment of the skin condition hidradenitis suppurativa.
[citation needed]
[edit] Aging Since most progesterone in males is created during testicular production of testosterone, and most in females by the ovaries, the shutting down (whether by natural or chemical means), or removal, of those inevitably causes a considerable reduction in progesterone levels. Previous concentration upon the role of progestagens (progesterone and molecules with similar effects) in female reproduction, when progesterone was simply considered a "female hormone", obscured the significance of progesterone elsewhere in both sexes. The tendency for progesterone to have a regulatory effect, the presence of progesterone receptors in many types of body tissue, and the pattern of deterioration (or tumor formation) in many of those increasing in later years when progesterone levels have dropped, is prompting widespread research into the potential value of maintaining progesterone levels in both males and females.
[edit] Brain damage Previous studies have shown that progesterone supports the normal development of neurons in the brain, and that the hormone has a protective effect on damaged brain tissue. It has been observed in animal models that females have reduced susceptibility to traumatic brain injury and this protective effect has been hypothesized to be caused by increased circulating levels of estrogen and progesterone in females.[41] A number of additional animal studies have confirmed that progesterone has neuroprotective effects when administered shortly after traumatic brain injury.[42] Encouraging results have also been reported in human clinical trials.[43][44] The mechanism of progesterone protective effects may be the reduction of inflammation which follows brain trauma.[45]
You might also like
- Progesterone in Orthomolecular Medicine by Ray PeatDocument66 pagesProgesterone in Orthomolecular Medicine by Ray PeatJulian MiñoNo ratings yet
- Estrus SynchronizationDocument27 pagesEstrus SynchronizationMuhammad NaeemNo ratings yet
- Development Team: Zoology Animal Physiology Reproductive HormoneDocument26 pagesDevelopment Team: Zoology Animal Physiology Reproductive HormoneIrfan Pathan KakarNo ratings yet
- Hormon ReproDocument36 pagesHormon Reproalvinrinaldi1101No ratings yet
- EstrogensDocument15 pagesEstrogensАнна ВарданянNo ratings yet
- Peran Progesterone Pada KehamilanDocument17 pagesPeran Progesterone Pada KehamilanPraja Putra AdnyanaNo ratings yet
- INFERTILITAS HormonDocument64 pagesINFERTILITAS HormonJulie Carnetion DNo ratings yet
- Endocrinology of PregnancyDocument68 pagesEndocrinology of PregnancySht SristiNo ratings yet
- Types and Examples: Estrogen, or Oestrogen, Is The PrimaryDocument8 pagesTypes and Examples: Estrogen, or Oestrogen, Is The PrimaryBeniamin BorotaNo ratings yet
- Hormone of Reproductive System (Synthesis and Mechanism of Action)Document38 pagesHormone of Reproductive System (Synthesis and Mechanism of Action)pwfNo ratings yet
- Progesterone in Orthomolecular MedicineDocument68 pagesProgesterone in Orthomolecular Medicineederbernadino92No ratings yet
- Gonadal Hormones, Their Inhibitors and Fertility and Antifertility AgentsDocument29 pagesGonadal Hormones, Their Inhibitors and Fertility and Antifertility AgentsGopal Prasad DahalNo ratings yet
- Sex HarmoneDocument22 pagesSex Harmonesuyash jainNo ratings yet
- A&P Assignment.Document17 pagesA&P Assignment.Tinke WinkeNo ratings yet
- Animal Hormones and Their Functions: Balete, Berida, BorromeoDocument88 pagesAnimal Hormones and Their Functions: Balete, Berida, BorromeoRessabela Juniper FayneNo ratings yet
- Gonadal HormonesDocument40 pagesGonadal HormonesJoyce VillanuevaNo ratings yet
- New Estrogen and ProgesteroneDocument56 pagesNew Estrogen and ProgesteroneHBrNo ratings yet
- Hormones of The GonadsDocument17 pagesHormones of The GonadsSophia AgenyiNo ratings yet
- Sex HormonesDocument58 pagesSex Hormonesbug4444not100% (1)
- Reproductive Hormones and Their FunctionsDocument6 pagesReproductive Hormones and Their FunctionsOwolabi PetersNo ratings yet
- Endocrine System (Vertebrate) : HomeostasisDocument7 pagesEndocrine System (Vertebrate) : HomeostasisKaleem UllahNo ratings yet
- EstrDocument2 pagesEstraviraaworldNo ratings yet
- P4 Fisiologia, AccionDocument9 pagesP4 Fisiologia, AccionCinthia DarceNo ratings yet
- 2015 - Physiology Production and Action of ProgesteroneDocument9 pages2015 - Physiology Production and Action of ProgesteroneCinantya Meyta SariNo ratings yet
- ContraceptivesDocument8 pagesContraceptivesRadowan AhmadNo ratings yet
- EndocrinologyDocument7 pagesEndocrinologyVijith.V.kumarNo ratings yet
- 3 EndocrinologyDocument4 pages3 EndocrinologyJessa MayNo ratings yet
- Lab Act Fisiologi - FBS6Document29 pagesLab Act Fisiologi - FBS6Ayi Abdul BasithNo ratings yet
- Mechanism Term and PretermDocument10 pagesMechanism Term and PretermRian AmertaNo ratings yet
- Induction of Puberty and Synchronization of Estrus in CattleDocument24 pagesInduction of Puberty and Synchronization of Estrus in CattleMayuri VohraNo ratings yet
- Drugs Affecting The FemaleDocument32 pagesDrugs Affecting The FemaleLule Allan PhillipNo ratings yet
- Drugs Affecting Reproduction: DR - R - PrameelaDocument76 pagesDrugs Affecting Reproduction: DR - R - PrameelaRamadi PrameelaNo ratings yet
- Sex Hormones and Their FunctionsDocument11 pagesSex Hormones and Their Functionsashutosh choudharyNo ratings yet
- Clinical Use of Progestins in Bitches and Queens - A Review - IVISDocument35 pagesClinical Use of Progestins in Bitches and Queens - A Review - IVISDai AnaNo ratings yet
- Gonadal Hormones 1-13Document66 pagesGonadal Hormones 1-13abstabsNo ratings yet
- Neuroendocrinology of Female Reproductive Organs Part IIDocument49 pagesNeuroendocrinology of Female Reproductive Organs Part IIShikha GautamNo ratings yet
- KIMED1Document9 pagesKIMED1Yolita Satya Gitya UtamiNo ratings yet
- Pharma - Reproductive SystemDocument4 pagesPharma - Reproductive SystemJordann de GuzmanNo ratings yet
- Female Sex HormonesDocument28 pagesFemale Sex HormonesAbdimalik AliNo ratings yet
- The Long-Term Effects of Metoclopramide-Induced HyperprolactinemiaDocument7 pagesThe Long-Term Effects of Metoclopramide-Induced Hyperprolactinemiaapi-282416840No ratings yet
- Nutr Influences EstrogenDocument8 pagesNutr Influences EstrogenPortiaI100% (1)
- Female HormoneDocument24 pagesFemale HormoneZuha HundalNo ratings yet
- The Eicosanoids: Prostaglandins, Thromboxanes, Leukotrienes, & Related Compounds& Nitric Oxide and Drugs For AsthmaDocument60 pagesThe Eicosanoids: Prostaglandins, Thromboxanes, Leukotrienes, & Related Compounds& Nitric Oxide and Drugs For AsthmaMer CiNo ratings yet
- Anaphy Overt DMDocument7 pagesAnaphy Overt DMVal FielNo ratings yet
- Estrogen and ProgesteroneDocument45 pagesEstrogen and Progesteronevinay0717No ratings yet
- بحث دبوانDocument12 pagesبحث دبوانNezar AlnasserNo ratings yet
- Progesterone in A NutshellDocument14 pagesProgesterone in A NutshellkiyannNo ratings yet
- Progesterone Review of Safety For Clinical StudiesDocument19 pagesProgesterone Review of Safety For Clinical StudiesCatrinescu OanaNo ratings yet
- Gynecomastia and Premature ThelarcheDocument14 pagesGynecomastia and Premature ThelarchexanderaleNo ratings yet
- The Role of Hormone in ParturitionDocument36 pagesThe Role of Hormone in ParturitionDiana HayatiNo ratings yet
- Steroids JenniferKettelDocument25 pagesSteroids JenniferKettelvinay0717No ratings yet
- Reproductive Disorders in The Dog and Bitch With Genetic ConcernsDocument5 pagesReproductive Disorders in The Dog and Bitch With Genetic ConcernsLuis WolfNo ratings yet
- EndocrinologyDocument21 pagesEndocrinologySANCHAYEETANo ratings yet
- Lecture 2 - Reprod - HormonesDocument5 pagesLecture 2 - Reprod - Hormoneskushal NeupaneNo ratings yet
- PCOS HealingDocument36 pagesPCOS HealingKheyrne Danu100% (1)
- How Estrogen Protects BonesDocument7 pagesHow Estrogen Protects BonesAndreas Pratama NugrahaNo ratings yet
- Female Sex HormonesDocument30 pagesFemale Sex HormonesMagdy El-GammalNo ratings yet
- A Ver Si EsteDocument13 pagesA Ver Si EsteVictor Hugo Rojas MuñozNo ratings yet
- Fkumj Physiology of Hormone 2012Document84 pagesFkumj Physiology of Hormone 2012sakelengelNo ratings yet
- Hormones and Embryonic Development: Advances in the BiosciencesFrom EverandHormones and Embryonic Development: Advances in the BiosciencesG. RaspéNo ratings yet
- Misty Williams How Are You Wired To Sleep UpdatedDocument21 pagesMisty Williams How Are You Wired To Sleep UpdatedCarolyn McClendonNo ratings yet
- Chap2 Lesson 1-4Document43 pagesChap2 Lesson 1-4Renalf Ezra BarbietoNo ratings yet
- Menopause: Prepared By: Kriti Banstola B.Sc. NursingDocument42 pagesMenopause: Prepared By: Kriti Banstola B.Sc. NursingKriti BanstolaNo ratings yet
- 1000 Ques & Ans File 2Document54 pages1000 Ques & Ans File 2bibin joyNo ratings yet
- Kathrine O Neal PP PDFDocument92 pagesKathrine O Neal PP PDFrezqNo ratings yet
- PF Vol 28 44 IndexDocument250 pagesPF Vol 28 44 Indexoliver reyNo ratings yet
- Unitive and Procreative Health Procreation, Creation and EvolutionDocument9 pagesUnitive and Procreative Health Procreation, Creation and EvolutionJustJ ThingsNo ratings yet
- D e M o GR Ap Hy, Fa Mi Ly PL An Ni N G An D C o NTDocument11 pagesD e M o GR Ap Hy, Fa Mi Ly PL An Ni N G An D C o NTDr-Sanjay SinghaniaNo ratings yet
- Utro Vs Microgest MKTDocument2 pagesUtro Vs Microgest MKTDedi SetiawanNo ratings yet
- Micronised Progesterone Soft Gelatin Capsules 100 MG / 200 MG / 400 MGDocument2 pagesMicronised Progesterone Soft Gelatin Capsules 100 MG / 200 MG / 400 MGSnehal AskandNo ratings yet
- Endometrin Corvera Drug-StudyDocument3 pagesEndometrin Corvera Drug-Studykkd nyleNo ratings yet
- Sex HormonesDocument442 pagesSex Hormonesuilifteng100% (1)
- Pharmacy Daily For Wed 05 Oct 2016 - WA Pharmacy Vax Success, End Med Review Cap Call, NSAID Heart Risk Link, Health AMPERSAND Beauty and Much MoreDocument4 pagesPharmacy Daily For Wed 05 Oct 2016 - WA Pharmacy Vax Success, End Med Review Cap Call, NSAID Heart Risk Link, Health AMPERSAND Beauty and Much MorepharmacydailyNo ratings yet
- Fogsi Position Statement On The Use of ProgestogensDocument9 pagesFogsi Position Statement On The Use of ProgestogensRaviraj TirukeNo ratings yet
- Clinical Findings: ACOG - Cervical Insufficiency As "Document5 pagesClinical Findings: ACOG - Cervical Insufficiency As "lllNo ratings yet
- ACOG Practice Bulletin Prevencion PPDocument10 pagesACOG Practice Bulletin Prevencion PPFelipe LlanosNo ratings yet
- Combine PDFDocument44 pagesCombine PDFruang belajar farmasiNo ratings yet
- Clinical Practice Guidelines On Miscarriage ManagementDocument44 pagesClinical Practice Guidelines On Miscarriage ManagementEvelyn LimNo ratings yet
- Oripro®: What Is in This LeafletDocument3 pagesOripro®: What Is in This LeafletKirubakaranNo ratings yet
- Vaginal Progesterone Prophylaxis For Preterm Birth (The OPPTIMUM Study) : A Multicentre, Randomised, Double-Blind TrialDocument11 pagesVaginal Progesterone Prophylaxis For Preterm Birth (The OPPTIMUM Study) : A Multicentre, Randomised, Double-Blind TrialFideVegaNo ratings yet
- App 2021 AcogDocument26 pagesApp 2021 AcogFernanda Copete Yolianis100% (1)
- PPR - LISTS - Registered Medicine Price List - 20221127 BahrainDocument318 pagesPPR - LISTS - Registered Medicine Price List - 20221127 BahrainvdvedNo ratings yet
- Mock Test 1 Part A Summer 2006Document53 pagesMock Test 1 Part A Summer 2006Alida Rautenbach0% (1)
- HRT Dosing GuideDocument5 pagesHRT Dosing GuideBAMNo ratings yet
- AMS Guide To Equivalent MHT-HRT Doses 1020 V1Document2 pagesAMS Guide To Equivalent MHT-HRT Doses 1020 V1송필용No ratings yet
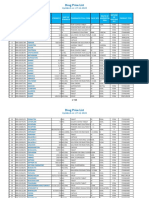
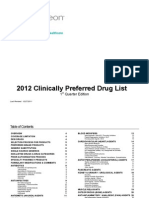
- Clinically Preferred FormularyDocument42 pagesClinically Preferred FormularyrajendickNo ratings yet
- Clinical Practice Guidelines On MenopauseDocument57 pagesClinical Practice Guidelines On Menopauseshivangini sahayNo ratings yet
- A Short Cervical Length in PregnancyDocument10 pagesA Short Cervical Length in Pregnancydinda_zaidiNo ratings yet
- Hormone Replacement TherapyDocument9 pagesHormone Replacement TherapyAgung SentosaNo ratings yet
- Australian Product Information - Oripro (Progesterone) Pessaries 1 Name of The Medicine 2 Qualitative and Quantitative CompositionDocument14 pagesAustralian Product Information - Oripro (Progesterone) Pessaries 1 Name of The Medicine 2 Qualitative and Quantitative CompositionKirubakaranNo ratings yet