Professional Documents
Culture Documents
Chest X
Uploaded by
Melissa KanggrianiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chest X
Uploaded by
Melissa KanggrianiCopyright:
Available Formats
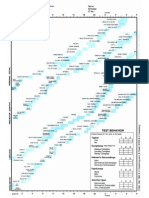
Chest X-Ray Findings that Can Suggest ACTIVE TB This category comprises all findings typically associated with
active pulmonary TB. An applicant with any of the following findings must submit sputum specimens for examination. 1. Infiltrate or consolidation - Opacification of airspaces within the lung parenchyma. Consolidation or infiltrate can be dense or patchy and might have irregular, ill-defined, or hazy borders. 2. Any cavitary lesion - Lucency (darkened area) within the lung parenchyma, with or without irregular margins that might be surrounded by an area of airspace consolidation or infiltrates, or by nodular or fibrotic (reticular) densities, or both. The walls surrounding the lucent area can be thick or thin. Calcification can exist around a cavity. 3. Nodule with poorly defined margins - Round density within the lung parenchyma, also called a tuberculoma. Nodules included in this category are those with margins that are indistinct or poorly defined. The surrounding haziness can be either subtle or readily apparent and suggests coexisting airspace consolidation. 4. Pleural effusion - Presence of a significant amount of fluid within the pleural space. This finding must be distinguished from blunting of the costophrenic angle, which may or may not represent a small amount of fluid within the pleural space (except in children when even minor blunting must be considered a finding that can suggest active TB). 5. Hilar or mediastinal lymphadenopathy (bihilar lymphadenopathy) - Enlargement of lymph nodes in one or both hila or within the mediastinum, with or without associated atelectasis or consolidation. 6. Linear, interstitial disease (in children only) - Prominence of linear, interstitial (septal) markings. 7. Other - Any other finding suggestive of active TB, such as miliary TB. Miliary findings are nodules of millet size (1 to 2 millimeters) distributed throughout the parenchyma.
Chest X-Ray Findings that Can Suggest INACTIVE TB This category includes findings that are suggestive of prior TB, that is inactive. It must be remembered that assessments of the activity of TB cannot be made accurately on the basis of a single radiograph alone. If there is any question of active TB, sputum smears must be obtained. Therefore, any applicant might have findings grouped in this category, but still have active TB as suggested by The presence of signs or symptoms of TB (Class B1). Sputum smears positive for AFB (Class A). 1. Discrete fibrotic scar or linear opacityDiscrete linear or reticular densities within the lung. The edges of these densities should be distinct and there should be no suggestion of airspace opacification or haziness between or surrounding these densities. Calcification can be present within the lesion and then the lesion is called a fibrocalcific scar. 2. Discrete nodule(s) without calcificationOne or more nodular densities with distinct borders and
without any surrounding airspace opacification. Nodules are generally round or have rounded edges. These features allow them to be distinguished from infiltrates or airspace opacities. To be included here, these nodules must be noncalcified. Nodules that are calcified are included in the category OTHER X-ray findings, No follow-up needed. 3. Discrete fibrotic scar with volume loss or retractionDiscrete linear densities with reduction in the space occupied by the upper lobe. Associated signs include upward deviation of the fissure or hilum on the corresponding side with asymmetry of the volumes of the two thoracic cavities. 4. Discrete nodule(s) with volume loss or retractionOne or more nodular densities with distinct borders and no surrounding airspace opacification with reduction in the space occupied by the upper lobe. Nodules are generally round or have rounded edges. 5. OtherAny other finding suggestive of prior TB, such as upper lobe bronchiectasis. Bronchiectasis is bronchial dilation with bronchial wall thickening.
You might also like
- Chest XDocument2 pagesChest XMelissa KanggrianiNo ratings yet
- Daily Multivitamins With Iron To Prevent Anemia in High-Risk Infants - MelDocument10 pagesDaily Multivitamins With Iron To Prevent Anemia in High-Risk Infants - MelMelissa KanggrianiNo ratings yet
- Jnma00288 0098Document3 pagesJnma00288 0098Melissa KanggrianiNo ratings yet
- Oral Cancer in Young Adults Report ofDocument4 pagesOral Cancer in Young Adults Report ofMelissa KanggrianiNo ratings yet
- CDC Chapter IIIDocument20 pagesCDC Chapter IIIMelissa KanggrianiNo ratings yet
- STABLE Program Module Objectives SummaryDocument2 pagesSTABLE Program Module Objectives SummaryMelissa Kanggriani100% (1)
- Fever in Child Apa Peds.2010-3852v1Document10 pagesFever in Child Apa Peds.2010-3852v1Ibrahim AlmoosaNo ratings yet
- CDC Chapter VDocument17 pagesCDC Chapter VMelissa KanggrianiNo ratings yet
- Formato Denver IIDocument1 pageFormato Denver IIMelly AnidaNo ratings yet
- Burning Mouth Syndrome-EtiologyDocument5 pagesBurning Mouth Syndrome-EtiologyMelissa KanggrianiNo ratings yet
- Diagnosis, Treatment, and Prevention of Typhoid Fever (WHO)Document48 pagesDiagnosis, Treatment, and Prevention of Typhoid Fever (WHO)Nina KharimaNo ratings yet
- Korti Ko SteroidDocument5 pagesKorti Ko SteroidMelissa KanggrianiNo ratings yet
- Faring It IsDocument34 pagesFaring It IsMelissa KanggrianiNo ratings yet
- Nephrotic Syndrome PDFDocument16 pagesNephrotic Syndrome PDFSulabh ShresthaNo ratings yet
- Rekomendasi TTG TLSDocument9 pagesRekomendasi TTG TLSMelissa KanggrianiNo ratings yet
- Nephrotic SyndromeDocument8 pagesNephrotic SyndromeAde Gustina SiahaanNo ratings yet
- The Host Response To Sepsis and Developmental ImpactDocument13 pagesThe Host Response To Sepsis and Developmental ImpactMelissa KanggrianiNo ratings yet
- Indian JOurnal of PediatricsDocument8 pagesIndian JOurnal of Pediatricsliska ramdanawatiNo ratings yet
- Sepsis Neonatorum NICE 2012Document40 pagesSepsis Neonatorum NICE 2012Melissa KanggrianiNo ratings yet
- Sepsis - Fanarof N AveryDocument56 pagesSepsis - Fanarof N AveryMelissa KanggrianiNo ratings yet
- Korti Ko SteroidDocument5 pagesKorti Ko SteroidMelissa KanggrianiNo ratings yet
- GI TRACT GabunganDocument7 pagesGI TRACT GabunganMelissa KanggrianiNo ratings yet
- HaematomasDocument6 pagesHaematomasMelissa KanggrianiNo ratings yet
- Kista GanglionDocument7 pagesKista GanglionMelissa KanggrianiNo ratings yet
- Urinary Incontinence in WomenDocument10 pagesUrinary Incontinence in WomenMelissa KanggrianiNo ratings yet
- Hipertensi Dan KehamilanDocument15 pagesHipertensi Dan KehamilanMelissa KanggrianiNo ratings yet
- PCI or PTCADocument30 pagesPCI or PTCAMelissa KanggrianiNo ratings yet
- Chronic Gastritis - Emedicine - 2 Des 2010Document15 pagesChronic Gastritis - Emedicine - 2 Des 2010Melissa KanggrianiNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5782)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Kelompok 1.4 PresentasiDocument13 pagesKelompok 1.4 PresentasiiqiqiqiqiqNo ratings yet
- Anatomy and Histology of The Normal Lung and AirwaysDocument20 pagesAnatomy and Histology of The Normal Lung and AirwaysFahd Abdullah Al-refaiNo ratings yet
- Case Study 1 COPDDocument5 pagesCase Study 1 COPDRenee RoSeNo ratings yet
- Neonatal and Pediatric Patient Assessment (Study Guide)Document17 pagesNeonatal and Pediatric Patient Assessment (Study Guide)Fatima Sherrisa SaliNo ratings yet
- Physiological Basis of Respiratory Disease (Qutayba Hamid, Joanne Shannon MD, James Martin)Document816 pagesPhysiological Basis of Respiratory Disease (Qutayba Hamid, Joanne Shannon MD, James Martin)RLibdehNo ratings yet
- Respiratory System (Anatomy and Physiology)Document71 pagesRespiratory System (Anatomy and Physiology)Butch Dumdum100% (11)
- IS-5216-Part-2 1982Document27 pagesIS-5216-Part-2 1982AEE 400KVNo ratings yet
- Questions Metabolic AcidosisDocument6 pagesQuestions Metabolic Acidosisyayooo2004No ratings yet
- Ineffective Breathing Pattern Pneumonia Nursing Care PlanDocument1 pageIneffective Breathing Pattern Pneumonia Nursing Care PlanJasonlee Baluyot100% (2)
- Topic 1 - Gas Exchange in Plants and AnimalsDocument14 pagesTopic 1 - Gas Exchange in Plants and AnimalsYara Jeah Ingay BaliliNo ratings yet
- Hypoxia and Oxygen TherapyDocument19 pagesHypoxia and Oxygen Therapynirilib86% (7)
- Pcap - PathophysiologyDocument4 pagesPcap - PathophysiologyAyla Mar100% (1)
- Pediatric Resucitation Pediatric Resucitation: Pgi Gasataya, Charisse Ann G Pgi Tabobo, Raymee TDocument30 pagesPediatric Resucitation Pediatric Resucitation: Pgi Gasataya, Charisse Ann G Pgi Tabobo, Raymee TCharisse Ann GasatayaNo ratings yet
- Recent Modes of Ventilation 103Document103 pagesRecent Modes of Ventilation 103medico_bhalla100% (2)
- Physiology of Body PositioningDocument95 pagesPhysiology of Body Positioningtanya dattNo ratings yet
- Day 9 - 11 - Human Body Systems - Respiratory and Circulatory SystemsDocument26 pagesDay 9 - 11 - Human Body Systems - Respiratory and Circulatory SystemsRichel Escalante MaglunsodNo ratings yet
- Acupressure Points For BronchitisDocument12 pagesAcupressure Points For BronchitisGopalsamy RamalingamNo ratings yet
- Iii. Lesson Proper: A. PreliminariesDocument3 pagesIii. Lesson Proper: A. PreliminariesMan Hee RaNo ratings yet
- Practice Examination For HESI ExitDocument76 pagesPractice Examination For HESI ExitGod_is_Good_294486% (43)
- Worksheet - Respiratory System PDFDocument3 pagesWorksheet - Respiratory System PDFDezta Fandity' VantycaNo ratings yet
- Review Questions For: Physiology II-1Document26 pagesReview Questions For: Physiology II-1ngphm70% (1)
- UntitledDocument68 pagesUntitledapi-233604231No ratings yet
- Foreign Bodies in ENTDocument18 pagesForeign Bodies in ENTSamsonNo ratings yet
- Grieco Et Al-2023-Intensive Care MedicineDocument4 pagesGrieco Et Al-2023-Intensive Care MedicineDr Vikas GuptaNo ratings yet
- 1 TM C Mcq-QuestionsDocument6 pages1 TM C Mcq-QuestionssaalimNo ratings yet
- 4 Basic Element For Normal MovementDocument17 pages4 Basic Element For Normal MovementKwai Fong ChanNo ratings yet
- Lecture PharynxDocument28 pagesLecture PharynxHoor AlnabhaniNo ratings yet
- 1.9.3,4 HandoutDocument3 pages1.9.3,4 HandoutfaezamushtaqNo ratings yet
- BIOLOGY CHAPTER 8 Form 4Document21 pagesBIOLOGY CHAPTER 8 Form 4husnäNo ratings yet