Professional Documents
Culture Documents
5 - Prenatal Diagnosis'' PDF
Uploaded by
ALNAKIOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
5 - Prenatal Diagnosis'' PDF
Uploaded by
ALNAKICopyright:
Available Formats
Prenatal diagnosis Prenatal diagnosis for populations at risk of genetic disorders has been established within antenatal care,
with the aim of confirming a normal pregnancy. Populations at risk for having an abnormal baby include women aged 35 or more, carriers for X- linked inherited disorders such as Duchenne muscle dystrophy and Fragile-X syndrome, parents who are carriers for chromosomal abnormalities, and many other family histories of genetic disorders. Prenatal diagnosis is helpful for:
Managing the remaining weeks of the pregnancy Determining the outcome of the pregnancy Planning for possible complications with the birth process Planning for problems that may occur in the newborn infant Deciding whether to continue the pregnancy Finding conditions that may affect future pregnancies
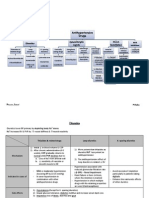
Variable screening tests have been used to investigate the high-risk pregnancy, where some tests are invasive while others are non-invasive. Non-invasive tests Biochemical markers Isolation of Foetal cells from maternal circulation Ultrasound Amniocentesis Chorionic villus sampling Foetal blood sampling Foetal tissue sampling / foetoscopy
Invasive tests
1- Non-invasive methods: These tests together with maternal age are used as screening rather than diagnostic tests. These will limit the invasive tests to those considered high risk pregnancies and includes the following:
1.1- Maternal serum or blood tests A- The triple test, is routinely used in the second trimester to investigate women at risk of having a Down syndrome (DS) foetus, and includes maternal serum alpha feto-protein (MSAFP), human chorionic gonadotrophin (hCG) and unconjugated estriol (uE3). AFP can be measured at 15-18 weeks of gestation. MSAFP testing is based on the fact that the DS foetus tends to be small, have a smaller placenta, and thus releases less AFP into the serum of the pregnant woman. This is not a definitive test. If the MSAFP test is low it suggests the risk of a DS foetus especially in woman with high risk (age 35 or more). If MSAFP alone is tested, 20 % of DS foetuses will be identified. If MSAFP and human chorionic gonadotrophin (HCG) are determined, 50 - 60 % of DS foetuses will be identified. If MSAFP, HCG and estradiol (E2) are tested, 60 -70 % of DS foetuses will be identified. A positive screening test suggests only that the risk of DS is increased, and the definitive testing of karyotyping via amniocentesis is indicated.
On the other hand, quadruple test [triple test with the fourth indicator inhibin-A (INHA)] is highly effective in identifying several foetal anomalies other than Down syndrome such as trisomies 18 and 16, Turner syndrome, triploidy and foetal death.
The first trimester screening of free beta-human-chorionic gonadotropin and pregnancy associated plasma protein-A (PAPPA) is a highly indicative test for a risk of DS especially when associated with the first trimester ultrasound finding of foetal nuchal translucency (NT).
1.2- Isolation of foetal nucleated cells from maternal circulation is a promising noninvasive prenatal test enabling investigation of foetal chromosomes in early pregnancy. Several studies have successfully isolated nucleated foetal cells (NFCs) from maternal
circulation. Yet, NCFs are not used routinely not only due to the scarcity of these cells in maternal circulation but also due to the need to confirm their foetal origin. Therefore by improving the techniques of isolation and identification of NFCs. We have used NFCs to investigate chromosomal aneuploidy with a relative low false positive rate. And used FISH on non-dividing interphase nuclei to investigate the numerical but not structural chromosome anomalies. In addition, foetal DNA has been identified, especially that for male foetus, in maternal serum and plasma during pregnancy. Several studies have used foetal DNA to screen paternally inherited single-gene disorders or mutated genes that can be distinguished from maternal components. Studies have successfully investigated several disorders such as Duchenne muscle dystrophy, foetal RhD blood type, sickle cell anaemia and beta-thalassemia in heterozygous carriers.
1.3- Genetic Sonogram: Ultrasonographers can determine several congenital anomalies suggestive of chromosomal and non-chromosomal defects. First trimester sonographic assessment of foetal anomalies is an important test for prenatal diagnosis. It requires understanding of embryonic development as some normal second trimester findings would be considered abnormal first trimester findings. The optimal time for scanning is around 12-week of gestation as most of organs can be visualized. Increased nuchal fold thickness detected in the first trimester is a good indicator not only for chromosomal anomalies (aneuoploidy) but also for skeletal and cardiovascular disorders. The second trimester ultrasound findings (18- 20 weeks) assess the foetal measurements and can assess foetal age to support risk estimation based on maternal serum biochemical markers. Foetal abnormalities including changes in the head circumstances; heart, nuchal thickness, foetal and limbs size are indicators of several disorders. DS foetuses for example, have a relatively thickened nuchal fold, short femur, short humerus, and echogenic intracardiac
focus. Trisomy 18 (Edward syndrome) foetuses usually show marked growth retardation and several congenital anomalies that can detected in ~90% of cases. Also trisomy 13 (Patau syndrome) foetuses have distinctive features and anomalies that can be diagnosed in the second trimester in 90-100% of cases. On the other hand, triploidy is usually lost early in pregnancy, but can occasionally be seen in the second trimester and frequently has specific ultrasonographic features. Generally sonographic markers may not be able to distinguish normal variation from specific disorders, such as growth retardation due to placental insufficiency; and other confirmative tests should be performed.
2- Invasive techniques: Invasive techniques, procedures used to obtain foetal cells, fluids or tissue samples for accurate diagnosis. The diagnostic value of these tests has to be balanced against the risk of causing foetal loss.
2.1- Chorionic villus sampling (CVS) can be done at about 11 weeks, either transvaginally or transabdominally. Earlier testing (before 11 weeks) is thought to be associated with a small risk of foetal hazards (such as limb reduction). The CVS test is done earlier, and is usually faster than amniocentesis. There is a small chance of maternal cell contamination and a 1-4% risk of miscarriage, infection, placental trauma, or foetomaternal haemorrhage after the procedure dependent on obstetric experience.
2.2- Amniocentesis, a sampling of the amniotic fluid (AF) surrounding the foetus, is routinely done transabdominally at 16- 18 weeks gestation, but can be performed from 11 weeks. A 10- 20 ml sample is withdrawn that contains fluid (for biochemical tests) and cells, mainly amniotic fluid cells (65%), fibroblast cells (10%) and epithelial cells (25%). Other foetal and maternal cell types, mainly blood cells, are frequently seen in the sample but do not usually divide in culture. Miscarriage, intrauterine infection, persistent amniotic
fluid leak, foeto-maternal haemorrhage, foetal injuries are less frequent complications after the procedure. Amniocentesis testing for chromosome disorders is 99.8 % reliable for detecting numerical chromosome abnormality.
2.3- Foetal blood sampling (FBS) is usually done for rapid assessment of foetal chromosomal anomalies, haemoglobinopathies, coagulopathies, infection and
immunodeficiency later in pregnancy. Blood is taken from the umbilical vein at the placental insertion under the ultrasound guidance. Foetal loss rate after the procedure is variable from 0-24%, with 12% losses for growth retarded foetuses.
2.4- Foetal tissue sampling (FTS): Diagnosis of certain foetal anomalies depends on histological and ultrastructure studies, based on foetal biopsy. For example foetal skin biopsy in the second trimester is used for prenatal diagnosis of epidermolysis bullosa lethalis. Foetal loss after these invasive procedures under ultrasound guidance is as high as 1%.
3- Cytogenetics / molecular genetics and prenatal diagnosis Development and accuracy of obstetric procedures for collecting samples (CVS, AF, FBS) and the reliability of chromosomal and/or DNA analysis have increased the demand for prenatal diagnosis. Despite advances in DNA technology, chromosomal karyotyping is still the core service of prenatal diagnosis. AF cells require about 1-2 weeks to give sufficient dividing cells for karyortyping. On the other hand, CVS contains cytotrophoblast cells that are actively dividing and provide sufficient metaphases in short-term cultures (24 hours) for rapid low resolution karyotyping. CVS mesenchymal core cells are also cultured and karyotyped after 1-2 weeks to confirm and support the result of the short-term cultures. Foetal blood contains lymphocytes that grow well in culture. Complications of
5
culture failure and maternal contamination are infrequent and represent ~1%. CVS sometimes shows chromosomal mosaicism, in particular with cytotrophoblast short-term cultures and represents confined placental mosaicism, but this is less frequent in the mesenchymal core cultures. Foetal chromosomal anomalies can be classified into numerical, mosaic and structural, where viable chromosomal aneuploidy of autosomal and/or sex chromosomes mainly chromosomes 13, 18, 21, X and Y chromosome is a particular focus of prenatal testing. Rapid interphase FISH screening of amniocytes has been used successfully in most prenatal diagnostic units for chromosomes 13, 18, 21, X and Y, to give rapid diagnosis of numerical chromosome anomalies with a high degree of concordance with karyotyping. Chromosome specific FISH probes or/ and subtelomeric FISH probes have been used prenatally to identify, some structural chromosome anomalies. DNA based techniques using polymerase chain reaction (PCR) tests are employed in prenatal diagnostic tests, such as multiplex fluorescence PCR (QF-PCR) tests for identifying chromosomal aneuploidy using DNA samples extracted from different foetal tissues (CVS, AF, FB, FTS). Also mutated genes that cause inherited genetic disorders such as Fra-X syndrome, and Duchenne muscle dystrophy have been detected prenatally by using PCR based tests.
Maternal Age 15 - 19 20 - 24 25 - 29 30 - 34 35 - 39 40 - 44 45 - 49
Trisomy 21 1:1600 1:1400 1:1100 1:700 1:240 1:70 1:20
Trisomy 18 1:17000 1:14000 1:11000 1:7100 1:2400 1:700 1:650
Trisomy 13 1:33000 1:25000 1:20000 1:14000 1:4800 1:1600 1:1500
Some of the more common chromosomal abnormalities that can occur. The descriptions are for the completely abnormal condition in which all fetal cells contain the abnormal karyotype.
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- VITMINS High Yield Pharmacology 3 PDF 13Document1 pageVITMINS High Yield Pharmacology 3 PDF 13ALNAKI0% (1)
- Netter S Illustrated Pharmacology, 2004-4Document7 pagesNetter S Illustrated Pharmacology, 2004-4ALNAKINo ratings yet
- JB Drugs ToolbookDocument272 pagesJB Drugs ToolbookOrion JohnNo ratings yet
- الأدوية اثناء الحملDocument9 pagesالأدوية اثناء الحملALNAKINo ratings yet
- أدوية الطوارىءDocument162 pagesأدوية الطوارىءManar22No ratings yet
- ReferenceBooks ProvincialRequriements 2012Document1 pageReferenceBooks ProvincialRequriements 2012ALNAKINo ratings yet
- Liver Function (II)Document20 pagesLiver Function (II)ALNAKINo ratings yet
- Nausea and Vomiting Highlights:: When To Refer To A PhysicianDocument2 pagesNausea and Vomiting Highlights:: When To Refer To A PhysicianALNAKINo ratings yet
- 3alam El-Teb: Edited byDocument17 pages3alam El-Teb: Edited byALNAKINo ratings yet
- Pharmacology SummaryDocument16 pagesPharmacology Summarysechzhen96% (46)
- CNS Stimulants: Pentetrazol CaffeineDocument1 pageCNS Stimulants: Pentetrazol CaffeineALNAKINo ratings yet
- أدوية الطوارىءDocument162 pagesأدوية الطوارىءManar22No ratings yet
- Antihypertensive DrugsDocument7 pagesAntihypertensive Drugshamadadodo7No ratings yet
- ( ) هام للغايةHERB DRUG-INTERACTION-CHARTDocument5 pages( ) هام للغايةHERB DRUG-INTERACTION-CHARTALNAKINo ratings yet
- Phl211 Sns 14th Lecture SFDocument10 pagesPhl211 Sns 14th Lecture SFALNAKINo ratings yet
- Phl211 Sns 13th Lecture SFDocument10 pagesPhl211 Sns 13th Lecture SFALNAKINo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Control and Prevention of MRSA in Hospitals and in The CommunityDocument41 pagesThe Control and Prevention of MRSA in Hospitals and in The CommunityDimas RfNo ratings yet
- Standard Case DefinitionsDocument10 pagesStandard Case DefinitionsMohammed AbdillahiNo ratings yet
- Hiv Trends Pir RHWC DavaoDocument57 pagesHiv Trends Pir RHWC DavaoIsfahan MasulotNo ratings yet
- Albendazole - Drug Information PDFDocument7 pagesAlbendazole - Drug Information PDFjjjkkNo ratings yet
- Psychological Changes of A Pregnant WomanDocument4 pagesPsychological Changes of A Pregnant WomanEuna Patricia AguilarNo ratings yet
- Fdar Cabg 3nesurgicalDocument5 pagesFdar Cabg 3nesurgicalMary Margareth GonzalesNo ratings yet
- Nursing Practice I.Document32 pagesNursing Practice I.beautifulme031690No ratings yet
- HBP MCQsDocument67 pagesHBP MCQsNessreen JamalNo ratings yet
- Sesi 15-Making Your Hospital Baby FriendlyDocument47 pagesSesi 15-Making Your Hospital Baby FriendlySiti HajarNo ratings yet
- Immunofluorescence Techniques: Ian D. Odell and Deborah CookDocument4 pagesImmunofluorescence Techniques: Ian D. Odell and Deborah CookbalamurugantNo ratings yet
- Jemds Title PDocument1 pageJemds Title PKriti KumariNo ratings yet
- Perinatology Clinics 2008, Vol.35, Issues 4, Neuroprotection in The NewbornDocument210 pagesPerinatology Clinics 2008, Vol.35, Issues 4, Neuroprotection in The NewbornJhonny MarquezNo ratings yet
- Tehnica Injectiei IM Vast Lateral Si DeltoidDocument6 pagesTehnica Injectiei IM Vast Lateral Si DeltoidAnca NeaguNo ratings yet
- Asthma and COPDDocument47 pagesAsthma and COPDSamuelVilbrunNo ratings yet
- Clinic Accomplishment ReportDocument9 pagesClinic Accomplishment ReportJen Apinado100% (6)
- Essential Intrapartum and Newborn Care: Health Science Department Southway College of TechnologyDocument3 pagesEssential Intrapartum and Newborn Care: Health Science Department Southway College of TechnologyRowena AngelesNo ratings yet
- Complications Following Dental Extractions in A Mobile Dental ClinicDocument4 pagesComplications Following Dental Extractions in A Mobile Dental ClinicdamingeniusNo ratings yet
- Kurva LubchencoDocument3 pagesKurva LubchencoDanil Armand67% (3)
- Inservice Surgical Hand Scrub Protocol UpdatesDocument20 pagesInservice Surgical Hand Scrub Protocol Updatescamicam_121No ratings yet
- Mckenzie Exercises: Exercise OneDocument6 pagesMckenzie Exercises: Exercise OneJansen ChNo ratings yet
- MEAL (Psychiatric Nursing 2)Document4 pagesMEAL (Psychiatric Nursing 2)Yucef Bahian-AbangNo ratings yet
- Facial TicsDocument2 pagesFacial TicsNdhe PoetryNo ratings yet
- Bsped Dka Guidelines 2020Document23 pagesBsped Dka Guidelines 2020drsaleemNo ratings yet
- Common Breast DiseasesDocument64 pagesCommon Breast Diseasesamirahmei100% (1)
- Geriatrics RehabDocument30 pagesGeriatrics RehabNasroon BhambhaniNo ratings yet
- PathogenesisDocument14 pagesPathogenesisIdreesNo ratings yet
- Viral Skin InfectionsDocument28 pagesViral Skin Infectionstolesadereje73No ratings yet
- Cycles and Cycle Safety: Pegasus PharmaceuticalsDocument25 pagesCycles and Cycle Safety: Pegasus PharmaceuticalsMahmoud El Mohamdy100% (2)
- Procedure: Inserting A Nasogastric/ Nasointestinal Tube: BUENO, Jessa Mae D 3-8 February 28, 2024Document15 pagesProcedure: Inserting A Nasogastric/ Nasointestinal Tube: BUENO, Jessa Mae D 3-8 February 28, 2024Jessa BuenoNo ratings yet
- Ajnr Benign Enhancing Lesion of Foramen MagnumDocument5 pagesAjnr Benign Enhancing Lesion of Foramen Magnumapi-288086961No ratings yet