Professional Documents
Culture Documents
Jhe Asthma LT
Uploaded by
dinna_dinunOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Jhe Asthma LT
Uploaded by
dinna_dinunCopyright:
Available Formats
Journal of Health Economics 29 (2010) 377387
Contents lists available at ScienceDirect
Journal of Health Economics
journal homepage: www.elsevier.com/locate/econbase
Long term effects of childhood asthma on adult health
Jason M. Fletcher a, , Jeremy C. Green a , Matthew J. Neidell b
a b
Yale University, United States Columbia University, United States
a r t i c l e
i n f o
a b s t r a c t
Childhood asthma is a major chronic condition affecting millions of children in this country, yet little is known about its potential long term consequences. In this paper, we estimate the relationship between childhood asthma and several outcomes as a young adult. To overcome many of the methodological issues plaguing earlier research on this topic, we estimate sibling xed effect models that correct for measurement error using parental reports of asthma status. In our preferred specication, we nd substantial long term impacts of childhood asthma on general health status, obesity, and missed work and school days as a young adult. Broadly, our ndings contribute to the growing literature in social sciences on the impacts of early life health conditions on later life health and social outcomes and suggest early treatment of asthma may have long-run benets on young adult health and socioeconomic outcomes. 2010 Elsevier B.V. All rights reserved.
Article history: Received 19 May 2009 Received in revised form 15 September 2009 Accepted 8 March 2010 Available online 19 March 2010 JEL classication: I12 I24 Keywords: Asthma Sibling xed effects: Measurement error
1. Introduction Asthma is one of the most common chronic health conditions aficting children. Nearly one in ten children has asthma, and this has nearly doubled over the past 25 years (Akinbami, 2006). It is a leading cause of health care utilization and the leading cause of school absences in children (U.S. Environmental Protection Agency, 2006; Currie, 2008). Furthermore, asthma disproportionately impacts children from lower socioeconomic background, with rates as high as 3035 percent in poor, urban areas (Akinbami, 2006; Nicholas et al., 2005). With estimated indirect and directs costs from asthma of over $18 billion (Smith et al., 1997; Weiss and Sullivan, 2001), the debilitating impacts from this highly prevalent condition on childrens human capital acquisition are substantial. Despite the ubiquity of this illness, much less is known about the long term consequences of this condition. The plausibility of a lasting impact from asthma comes from a growing body of evidence documenting the impact of childhood health shocks on adult outcomes (e.g., Smith, 1999, 2007; Case et al., 2002, 2005; Almond, 2006; Black et al., 2007; Currie, 2008; Fletcher, in press). While this research has linked several early health conditions, such as ADHD, birth weight, or depression, to later outcomes, little attention has
Corresponding author at: Division of Health Policy and Administration, Yale University, 60 College Street, #303, New Haven, CT 06520, United States. Tel.: +1 203 785 5760. E-mail address: jason.etcher@yale.edu (J.M. Fletcher). 0167-6296/$ see front matter 2010 Elsevier B.V. All rights reserved. doi:10.1016/j.jhealeco.2010.03.007
focused on asthma, despite it being one of the most common conditions to strike children. And the existing papers that focus on asthma suffer from methodological limitations that may preclude causal interpretations (Currie, 2008). This paper contributes to the growing literature on early life health status and later outcomes by estimating the long term impacts of asthma on health and other social outcomes. Using data from the National Longitudinal Study of Adolescent Health (Add Health) (Harris, 2008), we examine the impact of childhood asthma on self-reported health status, obesity, and missed school and work days. To control for potential confounding we estimate sibling xed effect models and control for a wide range of variables that may be correlated with both asthma status and our outcomes of interest. Although xed effect models may help to control for confounding, they may exacerbate measurement error since asthma is self-reported, thus offsetting some of the potential benets. Therefore, we extend the xed effect models by using parents report of asthma status as an instrumental variable for the childs self-report of asthma status. Although differences in asthma status within families are unlikely to be random, we present several specication checks that support the validity of our approach. Having had asthma as a child is associated with a 14 percentage point decrease in the probability of being in excellent self-reported health, a 12 percentage point increase in being obese, and a 10 percentage point increase in missing school or work as a young adult. Results from this analysis suggest that the prevalence of asthma early in life may have important deleterious consequences for long term health and wellbeing.
378
J.M. Fletcher et al. / Journal of Health Economics 29 (2010) 377387
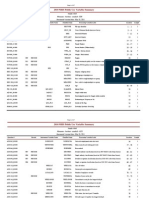
2. Background In general, research has shown that child health plays an important role in labor market outcomes and educational attainment for individuals as they grow older (Currie, 2008). To account for possible biases due to omitted factors at the environmental or family levels, several researchers have used sibling comparisons to link early health with later outcomes. Oreopoulos et al. (2008) found moderate effects of low birth weight children on education and labor market outcomes when compared to their normal weight siblings. Currie and Stabile (2006) found childhood ADHD to be linked with grade repetition, test score performance, and special education assignment.1 Fletcher and Wolfe (2009) present evidence that ADHD is linked with adult criminal activities. Fletcher (2008, in press) presents evidence that adolescent depression is associated with education outcomes in young adults, even between siblings. Smith (2007) found that better health in childhood is related to higher incomes, higher wealth, greater productivity, and a greater rate of income growth over the life course within each family. Focusing specically on asthma, long-run impacts may arise from several mechanisms. Asthma is often exacerbated by exercise because air is primarily inhaled through the mouth rather than nose, resulting in inhalation of colder and drier air that may trigger an attack (World Health Organization, 2008). Although this exercise-induced asthma can be controlled via proper medication, children wishing to reduce the likelihood of asthma attacks may decrease their amount of exercise. For example, of adults interviewed in the 19932000 surveys of the Behavioral Risk Factor Surveillance System, 70 percent who currently have asthma report any exercise in the past month, compared to 75 percent for those who do not currently have asthma.2 Even if children outgrow their asthma, exercise habits often form at early ages such that lasting impacts may persist (DiLorenzo et al., 1998). Given the strong evidence of an effect of exercise on obesity (Veerman et al., 2007), cardio-vascular disease (Li et al., 2006), and diabetes (e.g., Laaksonen et al., 2005), to name a few, this suggests the behavioral reaction to early diagnosis of asthma may have a lasting impact on physical health. Moreover, there may be direct biological alterations arising from the condition. During an asthma attack, the lining of the bronchial tubs swell, which causes the individuals airways to narrow and reduce the ow of air into and out of the lungs. These attacks can vary in severity and frequency, occurring several times a day in some children. Such chronic symptoms may damage long term lung function (Maddox and Schwartz, 2002). Additionally, since asthma treatment typically involves the use of both chronic and acute medication over a long period of time, the likelihood of adverse events is nontrivial in some populations (Boulet et al., 1999). Both of these suggest two channels whereby asthma during childhood could potentially reduce longer term health. While we are unaware of any studies that have examined the long term effects of asthma, several studies in various disciplines have examined the short-run consequences of asthma, summarized in Table 1. Typically, these studies estimate crosssectional associations between asthma and a variety of short-term, contemporaneous health and social outcomes, such as general health status, perceived wellbeing, life satisfaction, activity limi-
tations, missed school days, emotional problems, and behavioral problems.3 The studies generally found a negative correlation between asthma and these outcomes. While the previous literature is suggestive of negative consequences of asthma on health and socioeconomic outcomes, several limitations hinder statistical inference. Prominent among these is error in the measurement of asthma conditions, a focus on shortrun outcomes, and likelihood of environmental or family-level confounding in the estimated relationships. In this study, we overcome many of these limitations by using a longitudinal data set with information on the same individual at multiple points in time to explore longer run outcomes and estimating an instrumental variable/xed effects strategy that attempt to correct for both confounding and measurement error in self-reports of asthma. 3. Data In this paper, we use two data sources in our analysis. First, we use the 19972007 waves of the National Health Interview Survey (NHIS) in order to examine the typical age of onset of asthma in the US and the rate of asthma episodes by age, both of which provide supportive evidence that our main results represent long term effects of asthma. Second, we use the National Longitudinal Study of Adolescent Health (Add Health) to estimate regression models that relate asthma status to adult outcomes, where longitudinal data on adolescent siblings followed into adulthood is used to assess the health and socioeconomic effects of asthma. 3.1. NHIS The NHIS is an annual, cross-sectional household interview survey containing data on the health status and health care utilization of the civilian, non-institutionalized population. Each year of the NHIS contains approximately 35,000 households with a total of approximately 87,500 individual respondents (National Center for Health Statistics, 2009). The key variables of interest are selfreported asthma (Have you ever been told by a doctor or other health professional that you had asthma?) and asthma episodes (During the past 12 months, have you had an episode of asthma or asthma attack?), both available in all waves. Using both the child and young adults NHIS samples, we constructed asthma information by age for a synthetic panel of birth year cohorts so as to not confound age with cohort effects. Using the age of the individual and the survey year to dene cohorts, we focus on the 1987, 1994, and 2001 cohorts.4 We computed the mean rate for the ever asthma variable and prevalence of an asthma episode for each year of age within each cohort. 3.2. Add Health The Add Health is a school-based, longitudinal study of the health-related behaviors of adolescents and their outcomes in young adulthood. Beginning with an in-school questionnaire administered to a nationally representative sample of students in grades 7 through 12 in 199495 (Wave 1), the study follows up with a series of in-home interviews of students approximately one year (Wave 2) and then six years later (Wave 3). Other sources of data include questionnaires for parents, siblings, fellow students, and
1 Fletcher and Wolfe (2008) found evidence that the effects of ADHD on education outcomes may be short term and may not extend into adulthood education outcomes. 2 For more detailed information on the survey, see http://www.cdc.gov/brfss/index.htm. Comparable differences were also found for frequency and duration of exercise.
3 Although one study estimated sibling xed effect models, it focused on the impact of a specic asthma treatment on academic achievement, and found no evidence on an effect (Lindgren et al., 1992). 4 Unfortunately NHIS data is not available to dene a cohort similarly aged as the Add Health cohort.
Table 1 Literature on asthma, health, and social outcomes. Authors Ampon et al. (2005) Journal Thorax Year of publication 2005 Dataset and years 2001 Australia National Health Survey Study design Cross-sectional; logistic regression Outcome measures Life satisfaction, general health, psychological distress, reduced activity days ADHD, depression, behavioral disorders, learning disabilities, and missed school days Medical home score and its components Emotional and behavioral problems Activity limitations, missed school, disrupted sleep, etc.
Blackman and Gurka (2007)
Journal of Developmental and Behavioral Pediatrics Archives of Pediatric & Adolescent Medicine Archives of Pediatrics & Adolescent Medicine Annals of Allergy, Asthma, and Immunology Respiratory Medicine Medical Care
2007
2003 National Survey of Childrens Health 2003 National Survey of Childrens Health 1988 National Health Interview Survey 1995 and 2003 surveys of Seattle middle-school students (not same students) 2003 National Survey of Childrens Health & 19962003 Medical Expenditure Panel Survey 2000 Behavioral Risk Factor Surveillance System Survey of 3109 teenagers in Baltimore
Cross-sectional; logistic regression
J.M. Fletcher et al. / Journal of Health Economics 29 (2010) 377387
Brachlow et al. (2007) Bussing et al. (1995) Carter et al. (2005)
2007 1995 2005
Cross-sectional; logistic regression Cross-sectional; logistic regression Cross-sectional for each year, separately; entirely descriptive (no regressions) Literature Review Cross-sectional; negative binomial regressions Cross-sectional; logistic regression Cross-sectional; logistic regression
Chapman (2005) Chen and Escarce (2008)
2005 2008
Ford et al. (2003) Forrest et al. (1997)
Chest Pediatrics
2003 1997
Fowler et al. (1992) Gorman and Asaithambi (2008) Halterman et al. (2008) Lindgren et al. (1992)
Pediatrics Social Science Quarterly Ambulatory Pediatrics New England Journal of Medicine
1992 2008 2008 1992
1988 National Health Interview Survey 2003 National Asthma Survey 2003 National Survey of Childrens Health Primary data collection from siblings with and without asthma; test scores
Cross-sectional; logistic regression Cross-sectional; logistic regression Cross-sectional; logistic regression Cross-sectional; sibling comparisons (note: this study examined impact of a specic asthma treatment, rather than asthma itself) Pooled cross-sections (no synthetic panel) Cross-sectional; entirely descriptive (no regressions)
Treatment for asthma and asthma outcomes (independent variables are family structure) Physically and mentally unhealthy days, activity limitations Perceived wellbeing, physical and emotional symptoms, activity limitations, comorbidities, negative behaviors Grade failure, learning disabilities, suspension/expulsion, school absences Adult asthma prevalence (independent variables are family history measures) Health status and access to care Academic achievement
Scal et al. (2008) Taylor and Newacheck (1992)
Journal of Pediatrics Pediatrics
2008 1992
20002005 National Health Interview Survey 1988 National Health Interview Survey
Delays in access to care and other unmet needs Activity restrictions, medical care utilization, school absences
379
380
J.M. Fletcher et al. / Journal of Health Economics 29 (2010) 377387
school administrators. By design, the Add Health survey included a sample stratied by region, urbanicity, school type, ethnic mix, and size.5 Over 20,000 students completed the Wave 1 in-home survey in 199495, with over 14,000 followed longitudinally. We focus our baseline analysis around the approximately 13,000 respondents who were surveyed longitudinally and also reported their asthma status at Wave 3. The survey also collected information from over 5000 individuals who had a sibling or twin who was also surveyed at Wave 1. In our analysis that uses sibling comparisons, we focus on the approximately 3100 siblings who were followed longitudinally with their co-sibling and reported their asthma status at Wave 3. Using these data, we explore the impact of asthma on several outcome measures. First, we use a general measure of health status. In Wave 3 of Add Health, respondents are asked, In general, how is your health?, measured on a ve-point scale of poor, fair, good, very good, or excellent. Since this is a young population, we dene the dependent variable as a binary variable for being in excellent condition.6 Despite the subjectivity of this variable, research has shown it to be a strong predictor of objective measures, such as mortality and health care utilization (Miilunpalo et al., 1997). We also focus on obesity as an outcome, where the height and weight of respondents is measured in Wave 3. We classify individuals as obese if their body mass index exceeds 30, with remaining individuals classied as non-obese. Asthma may impact obesity by impacting lifestyle choices, namely exercise, which is an essential ingredient for maintaining a healthy body weight. Such effects may accumulate over time if lifestyle choices are habit-forming. Reverse causality is a potential concern with this outcome because obesity may increase the severity of asthma among those individuals who already have asthma (Vortmann and Eisner, 2008; Sutherland et al., 2008). To address this, as we discuss below in more detail, in several sensitivity analyses we focus on children who previously had asthma but do not currently have it, a situation where temporal precedence has been established. As a nal outcome, we focus on missed work and school days, using the measure from Add Health that asks respondents, In the past month, how often did a health problem cause you to miss a day of school or work? For inclusion in our models, this dependent variable is dened dichotomously, as an indicator for those individuals reporting having ever missed school or work days due to a health problem, as compared to those individuals who have never missed school or work days due to a health problem. Missed school and work days are an important outcome to study because a high percent of total asthma costs are indirect costs that include work and school loss that may be increasing over time (Smith et al., 1997; Weiss and Sullivan, 2001). Add Health contains several measures of asthma that we use in our analysis. In Wave 3, the young adult respondents were asked whether they have ever been diagnosed with asthma, which will serve as our primary measure of asthma. In the Wave 1 parental survey, each parent was asked whether their child currently has asthma. In Wave 3, young adults were asked Whether they have taken prescription medication in the past year for asthma. To control for potentially untreated asthma, we also use two measures for general unmet care: Has there been any time in the past 12 months when you thought you should get medical care, but you did not? and whether the respondent had been seen in an emergency room in the previous ve years where the main reason for the visit was an illness.
4. Methods To assess the lasting impacts of asthma, we begin with the following linear model:
3 3 1 Yifs = 0 + 1 Ever Asthma3 + 2 Xifs + 3 Xifs + ifs , ifs
(1)
where Yifs is the adult outcome of interest for individual i in family f from school s at Wave 3; ever asthma is the key independent variable, measured at Wave 3 (young adulthood); X w is a vector including controls for age, gender, race and ethnicity, birth order at Wave 3 and number of siblings, family income, mothers educational attainment, mothers marital status, mothers age, parental health, mother having asthma, and father having asthma at Wave 1. A concern with this model is possible omitted variables biascharacteristics of the childhood circumstances and environment may be related to health outcomes later in life (Case et al., 2005). We extend this specication by including school xed effects:
3 3 1 Yifs = 0 + 1 Ever Asthma3 + 2 Xifs + 3 Xifs + ifs s
+ ifs ,
(2)
where s is the vector of school xed effects that controls for attributes of schools and thus allows classmate comparisons. While school xed effects may overcome some of these concerns, it is possible that background characteristics vary considerably within schools, suggesting omitted variable bias remains a concern. In our preferred specications, we examine within-family differences by controlling for family xed effects:
3 3 1 Yifs = 0 + 1 Ever Asthma3 + 2 Xifs + 3 Xifs + ifs f
+ ifs .
(3)
By comparing siblings within the same family, we control for family and environmental background attributes that are shared between siblings and invariant over time. Although sibling xed effect models may correct for biases from omitted variables, it may exacerbate measurement error, thus attenuating our estimates and offsetting some of the benets from a more rigorous methodology (Card, 1996). Measurement error is a problem for survey research in general (Bound et al., 2000), especially in self-reported health measures (Butler et al., 1987; Chen et al., 2003). The prevalence of asthma is likely to be measured with error as clinical measures of asthma are known to lack sensitivity and specicity (Peat et al., 2000). There is also evidence that retrospective measures of self-reported asthma are most likely to capture cases of asthma with higher severity (Toren et al., 2006). In order to address this, we use the parental report of whether the adolescent had asthma in Wave 1 of this survey as an instrumental variable.7 This strategy purges our model of measurement error if parental reports are correlated with self-reports, which we demonstrate below, and if parental reports are uncorrelated with the measurement error in the childs report. Although we cannot test this assumption, we suspect it is a plausible one. As we report below, auxiliary analyses that examine the issue of non-classical measurement error suggest that our approach is biased by no more than 5 percent. Although sibling xed effects control for unobservable characteristics common to siblings, unobserved differences between siblings may be present (Bound and Solon, 1999). For example, a sibling with asthma may have a compromised immune system and thus be prone to additional health conditions that may impact later
See Udry (2003) for full description of the Add Health data set. We also nd comparable results dening the variable as being in excellent or very good health status or using the full ve point-scale.
6
7 This method is similar in spirit to that used by Ashenfelter and Krueger (1994), where one twins report of the others educational attainment was used as an instrument for the second twins self-reported educational attainment.
J.M. Fletcher et al. / Journal of Health Economics 29 (2010) 377387
381
outcomes. To limit the possibility of this concern, we separately add to our models controls for other health conditions that may arise from asthma comorbidities in this population and assess how this impacts our estimates.8 These controls include indicators for symptoms of childhood AD/HD,9 ever diagnosed with high cholesterol, epilepsy or diabetes by Wave 3, previous emergency room (ER) visit for an accident, injury, or other non-illness reasons in the ve years preceding Wave 3 of the survey, and learning disability, mental retardation, and having difculty with hands and feet at Wave 1.10 As we demonstrate below, our results are largely insensitive to these additional controls. While this IV/FE procedure likely reduces bias due to measurement error and confounding, we must also attempt to separate the impacts from asthma during childhood from the impacts from current asthma in order to focus on long term effects of the illness. That is, our key independent variable (ever asthma at Wave 3) could reect current asthma status, so our estimates would not reect the impact of past asthma experiences. While the impacts of asthma are typically more benign as children age, adult asthma may still have signicant impacts on other facets of life. To address this, we proceed with two approaches. First, we separately add to our model an indicator variable for whether the young adult is currently taking prescription medication for asthma. All asthma is not necessarily treated through medication, so we also include controls for whether the respondent has any unmet care for any medical need and whether the respondent reported an ER visit in the previous ve years for any illness. Since these two variables are not specic to asthma, this is a conservative approach for capturing uncontrolled asthma. After controlling for these variables, we can interpret the coefcient on ever asthma as the impact of ever having asthma conditional on not currently taking medications for asthma, not having unmet health care needs for asthma, and not having a recent ER visit for asthma. Thus, it reects the long-run impact from having asthma as a child. As a second, more conservative approach, instead of adding these three variables to our regressions, we eliminate from our analysis young adults who responded yes to any of the three variables. While we are likely dropping irrelevant observations, we again view this as a conservative approach for confronting this issue. With these two approaches, we hope to estimate effects for those individuals who were aficted by asthma as a child but not as a young adult. 5. Results 5.1. NHIS Results from the synthetic panel dataset constructed from the pooled cross-sections of the 19972007 waves of the NHIS are displayed in Figs. 1 and 2. Fig. 1 shows the time path of ever having asthma from the NHIS for the 2001, 1994, and 1987 birth year cohorts. Since each of these three birth year cohorts is included in only some years of the NHIS data, we examine separate age ranges that are available for each cohort but with several years of overlap between each cohort. This analysis provides a sense of the prevalence of asthma from the rst year of life through age 20.
Fig. 1. NHIS time path of ever asthma.
As this gure indicates, most of the onset of asthma occurs early in life. For the 2001 birth year cohort, the prevalence of ever having asthma during the rst year of life is approximately 2.9 percent, and increases steadily to 14.3 percent by age 6. The prevalence of ever having asthma was approximately 12.5 percent at age 6 for the 1994 birth year cohort. Following this cohort forward, the prevalence was 16.7 percent at age 13, and 16.1 percent at this same age for the 1987 birth year cohort. The last point for the 1987 birth year cohort shows that the prevalence of ever having asthma is approximately 16.9 percent at age 20. These results suggest that most of asthma onset occurs early in life, with little increase in the prevalence of ever having asthma beyond the age of 13. Appendix A presents the time path of ever having asthma for alternative cohorts the individuals born in the years 1997, 1987, and 1977 and shows that our conclusion that the onset of ever having asthma occurs almost entirely before the age of 13 is robust to the birth year cohorts used in the analysis. The time path of asthma attacks from the NHIS is displayed in Fig. 2. As with the prevalence of ever asthma, most asthma episodes occur early in life. For the 2001 birth year cohort, 60.9 percent of asthmatic children in their rst year of life had an asthma episode or attack during this year. At age 6, 47.8 percent of asthmatic individuals in this cohort had an asthma episode or attack. When the 1994 birth year cohort was six years old, 51.1 percent of asthmatic individuals in this cohort had an asthma episode or attack, and when the cohort was 13 years old, 30.6 percent of asthmatic individuals suffered from an asthma episode or attack. At age 13, 41.9 percent of asthmatic individuals in the 1987 birth year cohort had
8 Although parents may respond to the asthma status of their children by providing differential investments across siblings within a family, we do not consider this as a bias since it is a post-treatment response and may therefore reect a mechanism by which asthma has long run effects. 9 At wave 3, respondents retrospectively report eighteen symptoms of AD/HD during childhood. Following Fletcher and Wolfe (2009), we use DSM-IV related cutoffs from the list of symptoms in order to create our measure of AD/HD. 10 To preserve sample size, a separate indicator is included for missing data on these health variables.
Fig. 2. NHIS time path of asthma attacks.
382 Table 2 Add Health summary statistics. Variable
J.M. Fletcher et al. / Journal of Health Economics 29 (2010) 377387
Full sample Mean Std. Dev. 0.47 0.42 0.41 0.32 0.38 1.75 0.50 0.41 0.36 0.25 1.17 1.41 42.56 2.25 0.44 6.59 1.03 0.27 0.23 0.22 0.42 0.46 0.35 0.39 0.40 0.39 0.34 0.46 0.28 0.21 0.12 0.10 0.32 0.09 0.10 0.13 0.28
Sibling sample Mean 0.33 0.22 0.20 0.12 0.17 21.82 0.48 0.24 0.13 0.07 2.00 1.92 44.69 13.16 0.71 41.50 2.43 0.09 0.06 0.05 0.23 0.42 0.15 0.20 0.19 0.18 0.13 0.32 0.09 0.04 0.01 0.01 0.13 0.00 0.01 0.02 0.10 Std. Dev. 0.47 0.41 0.40 0.33 0.38 1.72 0.50 0.43 0.34 0.25 1.24 1.54 42.58 2.19 0.45 6.27 1.03 0.28 0.23 0.21 0.42 0.44 0.36 0.40 0.39 0.38 0.34 0.47 0.28 0.21 0.11 0.10 0.33 0.06 0.07 0.13 0.30
Excellent self-reported health status at Wave 3 Obese at Wave 3 Missed school or work days at Wave 3 Parental report of adolescent current asthma at Wave 1 Young adult self-report of ever having asthma at Wave 3 Age at Wave 3 Male Black Hispanic Other race Birth order Number of siblings at Wave 1 Family income at Wave 1 Mothers educational attainment at Wave 1 Married parents at Wave 1 Parent age at Wave 1 Parental health at Wave 1 Mother has asthma at Wave 1 Father has asthma at Wave 1 Medications for asthma at Wave 3 Received needed health care at Wave 3 Emergency room visit for illness at Wave 3 Grade = 8 at Wave 1 Grade = 9 at Wave 1 Grade = 10 at Wave 1 Grade = 11 at Wave 1 Grade = 12 at Wave 1 Missing parent information Ever AD/HD by Wave 3 Diagnosed with high cholesterol by Wave 3 Diagnosed with epilepsy by Wave 3 Diagnosed with diabetes by Wave 3 Learning disability at Wave 1 Mentally retarded at Wave 1 Difculty with hands at Wave 1 Difculty with feet at Wave 1 Missing health conditions information N = 13,048 in the full sample and 3129 in the sibling sample.
0.33 0.23 0.22 0.12 0.17 21.84 0.47 0.22 0.15 0.07 1.83 1.60 46.02 13.25 0.72 42.02 2.41 0.09 0.06 0.05 0.23 0.41 0.15 0.19 0.20 0.18 0.14 0.30 0.09 0.04 0.01 0.01 0.12 0.01 0.01 0.02 0.08
an asthma episode or attack, and approximately 24.6 of asthmatic individuals in this cohort had an asthma episode or attack at age 20. This gure suggests that the severity of asthma decreases as children age. To summarize the results from the NHIS, we nd that most asthma begins during early childhood and fades as children age. Because of this pattern, this suggests that our regression analysis is more likely to pick up long-run impacts from earlier asthma and not short-run impacts from contemporaneous asthma, something we also further probe and nd support for below. 5.2. Add Health Table 2 contains the descriptive statistics for the Add Health sample. In the full sample, approximately 12 percent of adolescents currently had asthma as measured by parental report in Wave 1. Of the 1828 year old individuals, 17 percent had ever had asthma by Wave 3 of the survey as measured by the individuals selfreport. Focusing on the subsample with siblings (used to produce the sibling xed effect estimates), the prevalence of asthma closely approximates the full sample, with parents reporting 12 percent of the adolescents currently having asthma at Wave 1 of the survey, and 17 percent of respondents self-reporting ever having asthma by the third wave of the study. These estimates are similar to the estimated prevalence of current and ever asthma for the equivalent ages and years of NHIS (current asthma was only included as of 2001). In this year of the survey, individuals between the ages of 11
and 19 had a mean prevalence of current asthma of 9.9 percent (95% condence interval: 8.112.2 percent). For years 2001 and 2002 of the NHIS, individuals between the ages of 18 and 26 had a mean prevalence of ever asthma of 14.3 percent (95% condence interval: 10.7, 17.7 percent). These descriptive statistics speak to the comparability of our NHIS and Add Health samples. Descriptive statistics for other variables are similar across the full Add Health sample and family Add Health subsample, with no meaningful differences in the distribution of gender, race, ethnicity, or grade levels in school. As a result, we can more credibly compare OLS results with sibling xed effects estimates in our empirical analyses. We present the results and robustness checks for our three outcomes (self-rated health status, obesity, and work/school absence) in separate tables. First, the estimated effects of ever asthma on excellent self-reported health status at Wave 3 are displayed in Table 3. The rst row of this table displays results from OLS and school xed effects estimates on the full sample and OLS and sibling xed effect estimates on the sibling sample, with limited individual level covariates and without instrumental variables. Column 1 presents the estimated coefcient on ever having asthma at Wave 3, showing a statistically signicant 7.7 percentage point reduction in excellent self-rated health status. In order to control for environmental inuences, school xed effects are added to the model in the second column of this table, but this does not change the coefcient noticeably. In column 3, the OLS results on the sibling sample are somewhat smaller than results for the full sample, but the difference is not statistically signicant. In column 4, when we control
J.M. Fletcher et al. / Journal of Health Economics 29 (2010) 377387 Table 3 Add Health results, long term effect of asthma on excellent health status. Specication: Sample: 1. Baseline model OLS Full 0.077*** (0.010) 12,729 0.719*** (0.011) 0.082*** (0.017) 12,729 0.078*** (0.017) 12,729 0.035 (0.022) 12,494 0.015 (0.031) 7437 School FE Full 0.075*** (0.009) 12,729 0.715*** (0.012) 0.079*** (0.017) 12,729 0.076*** (0.017) 12,729 0.032 (0.022) 12,494 0.010 (0.031) 7437 OLS Family 0.045** (0.019) 3027 0.725*** (0.022) 0.060 (0.037) 3010 0.053 (0.037) 3010 0.025 (0.045) 2962 0.042 (0.061) 1775
383
Sibling FE Family 0.104*** (0.031) 3027 0.731*** (0.030) 0.169*** (0.052) 3010 0.169*** (0.051) 3010 0.137** (0.062) 2962 0.150 (0.103) 1167
2. IV measurement error correction First stage results Second stage results
3. IV including controls for health conditions (second stage results only) 4. IV including controls for current asthmatics (second stage results only) 5. IV excluding current asthmatics (second stage results only)
Robust standard errors adjusted for clustering of individuals within schools and within families for the full and family samples respectively, are reported in parentheses. All models include controls for age, sex, race and ethnicity, birth order, number of siblings, family income, grade in school, mothers education, marital status, parental health, asthmatic mother, and asthmatic father. Health conditions are AD/HD, high cholesterol, epilepsy, diabetes, learning disability, mentally retarded, difculty with hands, difculty with feet, and previous emergency room visit for non-illness. Potential current asthma controls include asthma medications, emergency room visits in the past ve years for illness, and unmet health care needs. * Statistical signicance at the 10 percent level in a two-sided t-test. ** Statistical signicance at the 5 percent level in a two-sided t-test. *** Statistical signicance at the 1 percent level in a two-sided t-test.
for unobserved shared family environmental factors by including family xed effects, our estimates remain statistically signicant and increase slightly to 10 percentage points. As previously mentioned, self-reported asthma status may be reported with error, and any resulting bias may be a particular concern in xed effect models. In the second row of Table 3 we correct for potential measurement error in asthma status by instrumenting for the Wave 3 measure of ever having asthma with the Wave 1 parental report of currently having asthma. Results from the rst stage of the 2SLS estimation demonstrate the strength of our instrument, yielding t-statistics that range from 20 to 65. For the rst three columns, these instrumental variables estimates reveal a slightly larger long term effect of asthma on general health status than estimates without measurement error corrections, though these differences are not appreciable. For the sibling xed effect models, however, where measurement error concerns may be exacerbated, the coefcient on asthma increases considerably from the sibling xed effects estimate in the rst row of the table from 10.4 percentage points to 16.9 percentage points. Although the differences in these estimates are not statistically signicant according to a Hausman test, the differences are large in terms of economic signicance. This suggests that some of the increased impact by correcting for confounding by including family xed effects is lost to measurement error; this is only realized when we also instrument for asthma status. While family xed effects capture factors that are common to children within a family, a child with asthma may be different from his sibling in other important ways. More specically, a child who is asthmatic may be more prone to other health conditions, and these health conditions may be driving our results. In row 3, we add controls for several common health conditions, including AD/HD, but the results are nearly identical to those in row 2, suggesting the presence of comorbidities is unlikely to bias our estimates of the relationship between asthma and general health.
Although we have controlled for family factors, other illnesses, and corrected for measurement error, our estimates may reect a combination of childhood asthma and current asthma symptoms. That is, since the key dependent variable reects whether the young adult has ever had asthma, asthma may still be present so that our estimates reect the impact of current asthma on health. To address this, we control for current asthma symptoms by using three variables (1) an indicator for receiving a prescription for asthma medications in the previous year (2) an indicator for reporting unmet health care needs in the previous year, and (3) an indicator for reporting an emergency room visit in the previous ve years where the reason for the visit was an illness. If these variables capture current asthma status, we can interpret our estimates as the impact of ever having asthma conditional on not currently having asthma. While these variables will no doubt include individuals who have current asthma symptoms as well as other similar illnesses, this provides a conservative approach for controlling for current asthma. The results from adding these variables as covariates, shown in row 4, indicate a modest reduction in effects: the sibling xed effect coefcient is reduced from 16.9 percentage points to 13.7 percentage points. This slight reduction, while not statistically signicant, may be due in part from over-controlling for current asthma status. As a further test, we limit our sample to those without current asthma based on the three variables. Despite the over 60 percent reduction in sample size, we nd quite comparable estimates. The coefcient on the sibling FE model slightly rises from 0.137 to 0.150, though the considerable loss in sample size has pushed our estimate out of statistical signicance. The estimates suggest the impacts from asthma on health as a young adult are likely long term ones stemming from childhood asthma, a nding consistent with better asthma management as children age (as shown in Fig. 2). For the instrumented results, it is important to note that the binary nature of the potentially mismeasured variable (asthma)
384
J.M. Fletcher et al. / Journal of Health Economics 29 (2010) 377387
Table 4 Add Health results, long term effect of asthma on obesity. Specication: Sample: 1. Baseline model OLS Full 0.039*** (0.011) 12,068 0.719*** (0.011) 0.056*** (0.016) 12,068 0.053*** (0.016) 12,068 0.041** (0.021) 11,850 0.031 (0.025) 7047 School FE Full 0.043*** (0.011) 12,068 0.715*** (0.012) 0.059*** (0.017) 12,068 0.056*** (0.017) 12,067 0.044** (0.022) 11,850 0.041 (0.026) 7047 OLS Family 0.033 (0.024) 2797 0.723*** (0.023) 0.089** (0.036) 2783 0.085** (0.036) 2783 0.091** (0.045) 2741 0.077 (0.056) 1648 Sibling FE Family 0.009 (0.029) 2797 0.739*** (0.031) 0.078* (0.047) 2783 0.082* (0.047) 2783 0.122** (0.057) 2701 0.173* (0.091) 1087
2. IV measurement error correction First stage results Second stage results
3. IV including controls for health conditions (second stage results only) 4. IV including controls for current asthmatics (second stage results only) 5. IV excluding current asthmatics (second stage results only)
Robust standard errors adjusted for clustering of individuals within schools and within families for the full and family samples respectively, are reported in parentheses. All models include controls for age, sex, race and ethnicity, birth order, number of siblings, family income, grade in school, mothers education, marital status, parental health, asthmatic mother, and asthmatic father. Health conditions are AD/HD, high cholesterol, epilepsy, diabetes, learning disability, mentally retarded, difculty with hands, difculty with feet, and previous emergency room visit for non-illness. Potential current asthma controls include asthma medications, emergency room visits in the past ve years for illness, and unmet health care needs. * Statistical signicance at the 10 percent level in a two-sided t-test. ** Statistical signicance at the 5 percent level in a two-sided t-test. *** Statistical signicance at the 1 percent level in a two-sided t-test. Table 5 Add Health results, long term effect of asthma on missed school and work. Specication: Sample: 1. Baseline model OLS Full 0.057*** (0.011) 12,531 School FE Full 0.055*** (0.011) 12,531 OLS Family 0.065*** (0.019) 2967 Sibling FE Family 0.035 (0.029) 2967
2. IV measurement error correction First stage results Second stage results
0.719*** (0.011) 0.048*** (0.018) 12,531 0.047*** (0.018) 12,531 0.007 (0.022) 12,302 0.020 (0.026) 7329
0.715*** (0.012) 0.044** (0.018) 12,531 0.044** (0.018) 12,531 0.003 (0.022) 12,302 0.014 (0.026) 7329
0.721*** (0.022) 0.125*** (0.037) 2950 0.124*** (0.037) 2950 0.093** (0.045) 2903 0.132** (0.053) 1742
0.729*** (0.031) 0.134*** (0.052) 2950 0.134*** (0.052) 2950 0.106* (0.061) 2861 0.080 (0.095) 1146
3. IV including controls for health conditions (second stage results only) 4. IV including controls for current asthmatics (second stage results only) 5. IV excluding current asthmatics (second stage results only)
Robust standard errors adjusted for clustering of individuals within schools and within families for the full and family samples respectively, are reported in parentheses. All models include controls for age, sex, race and ethnicity, birth order, number of siblings, family income, grade in school, mothers education, marital status, parental health, asthmatic mother, and asthmatic father. Health conditions are AD/HD, high cholesterol, epilepsy, diabetes, learning disability, mentally retarded, difculty with hands, difculty with feet, and previous emergency room visit for non-illness. Potential current asthma controls include asthma medications, emergency room visits in the past ve years for illness, and unmet health care needs. * Statistical signicance at the 10 percent level in a two-sided t-test. ** Statistical signicance at the 5 percent level in a two-sided t-test. *** Statistical signicance at the 1 percent level in a two-sided t-test.
indicates that any measurement error would be non-classical. As a result, this leads to attenuation in our rst stage estimates, which inates our second stage estimates (Brachet, 2005). In order to examine the potential bias caused by misreporting, we follow recent parametric work in this area by Hausman et al. (1998) and Brachet (2005) to estimate the likely size
of the bias in our instrumental variable analysis due to nonclassical measurement error.11 Our analysis, described in more
11 See Brachet (2005) for additional discussion and application to measurement error in reports of prenatal smoking.
J.M. Fletcher et al. / Journal of Health Economics 29 (2010) 377387
385
detail in Appendix B, suggests that the bias is approximately 67 percent. Table 4 presents results of the estimated long term effects of asthma on obesity. Comparable to row 1 in the previous table, we nd statistically signicant estimates in OLS and school xed effect models of approximately 3.54 percentage points, but a smaller and statistically insignicant estimate in the sibling FE model. Correcting for measurement error by instrumenting also increases this estimate, making it statistically signicantly different from both zero and the non-IV estimate (according to a Hausman test). This suggests the confounding correction from using family xed effects is dwarfed by the resulting measurement error, pointing to the need to correct for measurement error. Including controls for other health conditions and current asthma status also has a minimal impact on our estimates; if anything our results are now larger in the sibling xed effects models. These robustness checks again support our interpretation of these estimates as long term effects. Results from estimating the long term effects of asthma on missed school and work days are presented in Table 5. Focusing again on the preferred sibling xed effect estimates, we do not nd a statistically signicant impact without instrumenting. Correcting for measurement error, however, reveals a statistically signicant 13 percentage point increase in missed school/work for those with asthma as a child that is also different from the FE model according to a Hausman test. The next three rows demonstrate that this result is again largely robust to inclusion of other health conditions and current asthma status. 6. Conclusion Childhood asthma is a major chronic condition affecting millions of children in this country in many ways. In this paper, we estimate the relationship between childhood asthma and several outcomes as a young adult. To overcome many of the methodological issues plaguing earlier research on this topic, we estimate sibling xed effect models that also correct for measurement error using parental reports of asthma status as an instrumental variable. Although we nd that using family xed effects to control for family background factors that may confound the relationship between asthma and adult outcomes generally increases the magnitude of our estimates, correcting for the measurement error from using family xed effects is an essential step. We nd substantial long term impacts of childhood asthma, including reductions in health status, increases in obesity, and increases in absenteeism by as much as 4050 percent by early adulthood. Since asthma is a condition that largely begins during childhood and persists for many years, the large estimated impacts likely reect the accumulation of effects over time. Furthermore, the magnitude of these effects is comparable to those from other studies on early illness and later health conditions. For example, Currie and Hyson (1999) report that low birth weight increases the likelihood of reporting poor health by 3050 percent at age 33. Almond and Mazumder (2005) estimate that in utero exposure to the 1918 u increased poor health reports for individuals over 60 by approximately 30 percent. Currie et al. (2008) show that childhood AD/HD can increase the likelihood of welfare receipt by 50 percent in early adulthood. Our ndings contribute to this growing body of evidence of signicant impacts from early life health conditions on later life health and social outcomes. Given the prevalence and persistence of asthma, our results speak to the potential reallocation of resources towards younger children. Treating poor adult health may be very costly because it often requires undoing the cumulative damage from a lifetime of negative shocks or low quality investments (see Heckman, 2007
for a general framework focusing on early investments), so that focusing on reducing the onset of asthma may be more efcient.12 Although the exact causes of asthma remain largely unknown, recent research suggests that exposure to common airborne allergens, such as cockroach and dust mites, in the presence of a weakened immune system caused by too clean of an environment (Institute of Medicine, 2000; Braun-Fahrlnder et al., 2002) may explain some of the recent rise in asthma. Therefore, our results suggest that efforts to minimize childhood exposure to these allergens and to strengthen the immune system may be an important component of current policy measures aimed at improving the health of adults. Acknowledgements Jeremy C. Green acknowledges support from a predoctoral traineeship from the Agency for Healthcare Research and Quality. This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Information on how to obtain the Add Health data les is available on the Add Health website (http://www.cpc.unc.edu/addhealth). No direct support was received from grant P01-HD31921 for this analysis. Appendix A. NHIS time path of asthma for alternative birth year cohorts
Appendix B. Non-classical measurement error with IV In order to estimate the potential bias in our IV results due to non-classical measurement error, we outline the parametric work of Hausman et al. (1998) and Brachet (2005), tailored to our variables. Omitting subscripts for ease of exposition, the equation of interest is Y = Asthma + X + . (A1)
12 Our data permits us to identify the impacts from having asthma as a child but not separately distinguish the impacts from the development of asthma versus exacerbation of asthma.
386
J.M. Fletcher et al. / Journal of Health Economics 29 (2010) 377387 von Mutius, E., 2002. Environmental exposure to endotoxin and its relation to asthma in school-age children. New England Journal of Medicine 347 (12), 869877. Bussing, R., et al., 1995. Prevalence of behavior problems in US children with asthma. Archives of Pediatrics & Adolescent Medicine 149 (5), 565572. Butler, J.S., Burkhauser, R.V., Mitchell, J.M., Pincus, T.P., 1987. Measurement error in self-reported health variables. The Review of Economics and Statistics 69 (4), 644650. Card, D., 1996. The effect of unions on the structure of wages: a longitudinal analysis. Econometrica 64 (4), 957979. Carter, E.R., Debley, J.S., Redding, G.J., 2005. Changes in asthma prevalence and impact on health and function in Seattle middle-school children: 1995 vs. 2003. Annals of Allergy, Asthma & Immunology 94 (6), 634639. Case, A., Fertig, A., Paxson, C., 2005. The lasting impact of childhood health and circumstance. Journal of Health Economics 24, 365389. Case, A., Lubotsky, D., Paxson, C., 2002. Economic status and health in childhood: the origins of the gradient. The American Economic Review 92 (5), 1308 1334. Chapman, K.R., 2005. Impact of mild asthma on health outcomes: ndings of a systematic search of the literature. Respiratory Medicine 99, 13501362. Chen, A.Y., Escarce, J.J., 2008. Family structure and the treatment of childhood asthma. Medical Care 46 (2), 174184. Chen, D., Krieder, B., Merwin, E., Stern, S., 2003. Diagnosis measurement error and corrected instrumental variables. In: Staff General Research Paper No. 10231. Iowa State University Department of Economics. Currie, J., 2008. Healthy, wealthy, and wise: socioeconomic status, poor health in childhood, and human capital development. In: NBER Working Paper No. 13987. Currie, J., Hyson, R., 1999. Is the impact of health shocks cushioned by socioeconomic status? The case of low birthweight. American Economic Review Papers and Proceedings 89 (2), 245250. Currie, J., Stabile, M., 2006. Child mental health and human capital accumulation: the case of ADHD. Journal of Health Economics 25 (6), 10941118. Currie, Stabile, J.M., Manivong, P., Roos, L., 2008. Child health and young adult outcomes. In: NBER Working Paper 14482. DiLorenzo, Thomas M., Renee, C. Stucky-Ropp, Vander Wal, Jillon S., Gotham, Heather J., 1998. Determinants of exercise among children II: a longitudinal analysis. Preventive Medicine 27 (3), 470477. Fletcher, J.M., 2008. Adolescent depression: diagnosis, treatment, and educational attainment. Health Economics 17, 12151235. Fletcher, J.M., in press. Adolescent depression and educational attainment: evidence from sibling xed effects. Health Economics. Fletcher, J.M., Wolfe, Barbara L., 2008. Child mental health and human capital accumulation: the case of ADHD revisited. Journal of Health Economics 27 (3), 794800. Fletcher, J.M., Wolfe, Barbara L., 2009. Long term consequences of childhood ADHD on criminal activities. Journal of Mental Health Policy and Economics 12 (3), 119138. Ford, E.S., et al., 2003. Self-reported asthma and health-related quality of life: ndings from the behavioral risk factor surveillance system. Chest 123, 119127. Forrest, C.B., et al., 1997. The impact of asthma on the health status of adolescents. Pediatrics 99 (2), E1. Fowler, M.G., Davenport, M.G., Garg, R., 1992. School functioning of US children with asthma. Pediatrics 90, 939944. Gorman, B.K., Asaithambi, R., 2008. Biology, social environment, and health: how family history and social conditions affect adult asthma. Social Science Quarterly 89 (3), 728750. Halterman, J.S., et al., 2008. The impact of health insurance gaps on access to care among children with asthma in the United States. Ambulatory Pediatrics 8, 4349. Harris, K.M., 2008. The National Longitudinal Study of Adolescent Health (Add Health), Waves I & II, 19941996; Wave III 20012002 [machine-readable data le and documentation]. Carolina Population Center, University of North Carolina at Chapel Hill, Chapel Hill, NC. Hausman, J., Abrevaya, J., Scott-Morton, F., 1998. Misclassication of the dependent variable in a discrete-response setting. Journal of Econometrics 87, 239269. Heckman, J.J., 2007. The economics, technology, and neuroscience of human capability formation. Proceedings of the National Academy of Sciences 104 (33), 1325013255. Institute of Medicine, 2000. Clearing the Air: Asthma and Indoor Air Exposures. National Academies Press, Washington, DC. Laaksonen, D.E., Lindstrom, J., Lakka, T.A., et al., 2005. Physical activity in the prevention of type 2 diabetes: the Finnish diabetes prevention study. Diabetes 54 (1), 158165. Li, T.Y., Rana, J.S., Manson, J.E., et al., 2006. Obesity as compared with physical activity in predicting risk of coronary heart disease in women. Circulation 113 (4), 499506. Lindgren, S., et al., 1992. Does asthma treatment with theophylline limit childrens academic performance? New England Journal of Medicine 327, 926930. Maddox, L., Schwartz, D.A., 2002. The pathophysiology of asthma. Annual Review of Medicine 53, 477498. Miilunpalo, Seppo, Vuori, Ilkka, Oja, Pekka, Pasanen, Matti, Urponen, Helka, 1997. Self-rated health status as a health measure: the predictive value of selfreported health status on the use of physician services and on mortality in the working-age population. Journal of Clinical Epidemiology 50 (5), 517 528.
The equation for reporting asthma status, the potential mismeasured variable, is assumed to be Asthma = 1(X + Z + > 0), (A2)
where Z is a vector of instruments not included in X. Parental reports of asthma status for the respondents serve as Z in our application. In this model, the omitted variable problem is captured by non-zero correlation between and . Without misclassication and assuming that is uniformly distributed, the two-stage least squares estimator is consistent for . In our case, Asthma is an imperfect measure of true asthmatic status, Asthma* and the probabilities of misclassication depend only on the respondents actual asthma status, but are otherwise independent of the covariates in the equations X and Z. Specically, write the misclassication probabilities as: a0 Pr(Asthma = 1|Asthma = 0) a1 Pr(Asthma = 0|Asthma = 1) , (A3)
These assumptions on the misclassication process are the binary variable analogs of the classical measurement error assumptions in the standard case of continuous variables. Next, derive the following equation for the conditional expectation of the observed dependent variable: E(Asthma|X, Z ) = Pr(Asthma = 1|X, Z ), E(Asthma|X, Z ) = a0 + (1 a0 a1 )F (X + Z ), (A4) (A5)
where F ( ) is the cdf of . Using Eq. (A5) and an assumption of the shape of F ( ), we can estimate the alphas using non-linear least squares; the model is identied entirely from the non-linearly of F . As shown in Brachet (2005), our IV estimate will overstate the magnitude of the actual effects of asthma on outcomes by a factor of 1/(1 a0 a1 ). Using either a normal or logistic density functions for F , we estimate this factor as 1.061.07, suggesting our IV estimates are inated by roughly 6 percent or 7 percent. References
Almond, D., 2006. Is the 1918 Inuenza Pandemic Over? Long-Term Effects of In Utero Inuenza Exposure in the Post-1940 U.S. Population. Journal of Political Economy 114 (4), 672712. Almond, D., Mazumder, B., 2005. The 1918 inuenza pandemic and subsequent health outcomes: an analysis of SIPP data. American Economic Review Papers and Proceedings 95 (2), 258262. Akinbami, L.J., 2006. State of childhood asthma, United States: 19802005. In: Advance Data from Vital and Health Statistics 381. CDC National Center for Health Statistics, December 12. Ampon, R.D., et al., 2005. Impact of asthma on self-reported health status and quality of life: a population based study of Australians Aged 1864. Thorax 60, 735739. Ashenfelter, O.A., Krueger, A.B., 1994. Estimates of the economic return to schooling from a new sample of twins. The American Economic Review 84, 11571173. Black, S., Devereux, P., Salvanes, Kjell, 2007. From the cradle to the labor market: the effect of birth weight on adult outcomes. The Quarterly Journal of Economics (February), 409439. Blackman, J.A., Gurka, M.J., 2007. Developmental and behavioral comorbidities of asthma in children. Journal of Developmental & Behavioral Pediatrics 28 (2), 9299. Boulet, Louis-Philippe, Becker, Allan, Berube, Denis, Beveridge, Robert, Pierre Ernst on behalf of the Canadian Asthma Consensus Group, 1999. Summary of recommendations from the Canadian asthma consensus report. Canadian Medial Association Journal 161 (Suppl. 11), S1S12. Bound, J., Brown, C.C., Mathiowetz, N.A., 2000. Measurement error in survey data. In: University of Michigan Population Studies Center Research Report No. 00-0450. Bound, J., Solon, G., 1999. Double trouble: on the value of twins-based estimation of the returns to schooling. Economics of Education Review 18, 169182. Brachet, T., 2005. Maternal smoking, misclassication, and infant health. In: University of Pennsylvania Working Paper. Brachlow, A.E., et al., 2007. Comparison of indicators for a primary care medical home between children with autism or asthma and other special health care needs. Archives of Pediatric & Adolescent Medicine 161 (4), 399405. Braun-Fahrlnder, C., Riedler, J., Herz, U., Eder, W., Waser, M., Grize, L., Maisch, S., Carr, D., Gerlach, F., Bufe, A., Lauener, R.P., Schierl, R., Renz, H., Nowak, D.,
J.M. Fletcher et al. / Journal of Health Economics 29 (2010) 377387 National Center for Health Statistics, 2009. National Health Interview Survey (NHIS) Description. Available from: http://www.cdc.gov/nchs/about/major/ nhis/hisdesc.htm (accessed 07.04.09). Nicholas, S.W., Jean-Louis, B., Ortiz, B., Northridge, M., Shoemaker, K., Vaughan, R., Rome, M., Canada, G., Hutchinson, V., 2005. Addressing the childhood asthma crisis in Harlem: the Harlem Childrens zone asthma initiative. American Journal of Public Health 95, 245249. Oreopoulos, Philip, Stabile, Mark, Walld, Randy, Roos, Leslie L., 2008. Short-, medium-, and long-term consequences of poor infant health: an analysis using siblings and twins. Journal of Human Resources 43 (1), 88138. Peat, J.K., Toelle, B.G., Mellis, C.M., 2000. Problems and possibilities in understanding the natural history of asthma. Journal of Allergy and Clinical Immunology 106 (3), 144152. Scal, P., et al., 2008. Transition into adulthood: delays and unmet needs among adolescents and young adults with asthma. Journal of Pediatrics 152, 471475. Smith, D.H., et al., 1997. A national estimate of the economic costs of asthma. American Journal of Respiratory and Critical Care Medicine 156 (3), 787793. Smith, J.P., 2007. The impact of socioeconomic status on health over the life-course. The Journal of Human Resources 42 (4), 739764. Smith, J.P., 1999. Healthy bodies and thick wallets: the dual relation between health and economic status. The Journal of Economic Perspectives 13 (2), 145166.
387
Sutherland, T.J.T, et al., 2008. The association between obesity and asthma: interactions between systemic and airway inammation. American Journal of Respiratory and Critical Care Medicine 178 (5), 469475. Taylor, W.R., Newacheck, P.W., 1992. Impact of childhood asthma on health. Pediatrics 90, 657662. Toren, K., Palmqvist, M., Lowhagen, O., Balder, B., Tunsater, A., 2006. Self-reported asthma was biased in relation to disease severity while reported year of asthma onset was accurate. Journal of Clinical Epidemiology 59, 9093. Udry JR. 2003. The National Longitudinal Study of Adolescent Health (Add Health), Waves I & II, 19941996; Wave III, 20012002 [machine-readable data le and documentation]. Chapel Hill, NC: Carolina Population Center, University of North Carolina at Chapel Hill. U.S. Environmental Protection Agency, 2006. Asthma facts. In: Indoor Environments Division, Ofce of Air and Radiation, EPA 402-F-04-019. Veerman, J.L., Barendregt, J.J., van Beeck, E.F., et al., 2007. Stemming the obesity epidemic: a tantalizing prospect. Obesity 15 (9), 23652370. Vortmann, M., Eisner, M.D., 2008. BMI and health status among adults with asthma. Obesity 16, 146152. Weiss, K.B., Sullivan, S.D., 2001. The health economics of asthma and rhinitis. I. Assessing the economic impact. Current Reviews of Allergy and Clinical Immunology 107, 38. World Health Organization, 2008. Asthma fact sheet. Available at: http://www. who.int/mediacentre/factsheets/fs307/en/print.html (accessed 29.08.09).
You might also like
- Ron Brookmeyer, Donna F. Stroup-Monitoring The Health of Populations - Statistical Principles and Methods For Public Health Surveillance (2003)Document389 pagesRon Brookmeyer, Donna F. Stroup-Monitoring The Health of Populations - Statistical Principles and Methods For Public Health Surveillance (2003)Medical_Doctor100% (1)
- Coping With Chronic Illness Childhood AdolescenceDocument27 pagesCoping With Chronic Illness Childhood AdolescenceLouisette AgapeNo ratings yet
- Prevalence of Asthma in Australian ChildrenDocument4 pagesPrevalence of Asthma in Australian Childrenoktha_pohanNo ratings yet
- Adverse Childhood Experiences and Coping Strategies: Identifying Pathways To Resiliency in AdulthoodDocument17 pagesAdverse Childhood Experiences and Coping Strategies: Identifying Pathways To Resiliency in AdulthoodAndreea PalNo ratings yet
- Demographic Research: Volume 32, Article 4, Pages 107 Published 9 January 2015Document42 pagesDemographic Research: Volume 32, Article 4, Pages 107 Published 9 January 2015paaztiiNo ratings yet
- Environmental Tobacco Smoke Exposure and Asthma in Adults: Uteii, 2Document5 pagesEnvironmental Tobacco Smoke Exposure and Asthma in Adults: Uteii, 2Tony Tukang TahuNo ratings yet
- Gastro Oesophageal RefluxDocument7 pagesGastro Oesophageal Refluxjustifieda13No ratings yet
- Effect of Low Birth Weight On Childhood Asthma: A Meta-AnalysisDocument8 pagesEffect of Low Birth Weight On Childhood Asthma: A Meta-Analysisnavali rahmaNo ratings yet
- The Dynamics of Health: Andrew M. Jones, Nigel Rice & Paul ContoyannisDocument21 pagesThe Dynamics of Health: Andrew M. Jones, Nigel Rice & Paul ContoyannisailmanetNo ratings yet
- Systematic Review and Meta-Analysis of Health Promotion Interventions For Children and Adolescents Using An Ecological FrameworkDocument14 pagesSystematic Review and Meta-Analysis of Health Promotion Interventions For Children and Adolescents Using An Ecological FrameworkFikran Ahmad Ahmad Al-HadiNo ratings yet
- Higher Education and Health Investments: Does More Schooling Affect Preventive Health Care Use?Document33 pagesHigher Education and Health Investments: Does More Schooling Affect Preventive Health Care Use?Sarmad AslamNo ratings yet
- Bài 2 - TaDocument12 pagesBài 2 - TaTRINH NGUYEN THI NGOCNo ratings yet
- The Effectiveness of Cigarette Regulations in Reducing Cases of Sudden Infant Death SyndromeDocument28 pagesThe Effectiveness of Cigarette Regulations in Reducing Cases of Sudden Infant Death SyndromeEugenio MartinezNo ratings yet
- The Scars of The Past? Childhood Health and Health Differentials in Later LifeDocument12 pagesThe Scars of The Past? Childhood Health and Health Differentials in Later LifeJefersson Romero BarreraNo ratings yet
- TC Record PDFDocument17 pagesTC Record PDFPeter MuennigNo ratings yet
- Discussion Paper Series: The Causal Effect of Education On Chronic Health ConditionsDocument27 pagesDiscussion Paper Series: The Causal Effect of Education On Chronic Health ConditionsMerna YasserNo ratings yet
- Bài 4 - TaDocument12 pagesBài 4 - TaTRINH NGUYEN THI NGOCNo ratings yet
- Bài 5 - TaDocument11 pagesBài 5 - TaTRINH NGUYEN THI NGOCNo ratings yet
- Parenting Stress Among Caregivers of Children With Chronic IllnessDocument21 pagesParenting Stress Among Caregivers of Children With Chronic IllnessZuluaga LlanedNo ratings yet
- Final Chapter 2 RRLDocument17 pagesFinal Chapter 2 RRLStephanie Joy EscalaNo ratings yet
- Beating and Insulting Children As A Risk For Adult Cancer, Cardiac Disease and AsthmaDocument9 pagesBeating and Insulting Children As A Risk For Adult Cancer, Cardiac Disease and AsthmaBadger6No ratings yet
- Jurnal 4Document11 pagesJurnal 4keperawatan fkNo ratings yet
- Review: Developing Asthma in Childhood From Exposure To Secondhand Tobacco Smoke: Insights From A Meta-RegressionDocument8 pagesReview: Developing Asthma in Childhood From Exposure To Secondhand Tobacco Smoke: Insights From A Meta-RegressionJules IuliaNo ratings yet
- Aging and The Environment A Research FrameworkDocument1 pageAging and The Environment A Research FrameworkPedro SanchezNo ratings yet
- Childhood - Adversity&early AgingDocument10 pagesChildhood - Adversity&early AgingMaudeNo ratings yet
- Work Family Conflict, Individual Factors and Metabolic Syndrome Risk Among Officers in Immigration Department MalaysiaDocument102 pagesWork Family Conflict, Individual Factors and Metabolic Syndrome Risk Among Officers in Immigration Department Malaysianur akhmarNo ratings yet
- The Determinants of The Health of The PeopleDocument19 pagesThe Determinants of The Health of The PeopleDina KaraNo ratings yet
- Iron Supplementation ExperimentDocument0 pagesIron Supplementation ExperimentGarrett PetersonNo ratings yet
- Safari - 16 Aug 2019 18.28Document1 pageSafari - 16 Aug 2019 18.28Yoan Caroline Saron KapressyNo ratings yet
- Humrep Des398 FullDocument9 pagesHumrep Des398 FullKinjal ShahNo ratings yet
- NCHS, 1998 NCHS, 1998 NCHS, 1998Document2 pagesNCHS, 1998 NCHS, 1998 NCHS, 1998seqNo ratings yet
- The Education-Health GradientDocument7 pagesThe Education-Health GradientatikfaizaNo ratings yet
- Health Consequences of Adverse Childhood Experiences: A Systematic ReviewDocument9 pagesHealth Consequences of Adverse Childhood Experiences: A Systematic ReviewCocia Podina Ioana RoxanaNo ratings yet
- Ni Hms 545265Document21 pagesNi Hms 545265Resti Zulvanita DeviNo ratings yet
- Asthma: A Growing EpidemicDocument16 pagesAsthma: A Growing Epidemicatc5049No ratings yet
- Control Del Asma Sorensen 2016Document3 pagesControl Del Asma Sorensen 2016José Luis GálvezNo ratings yet
- ACE Finished - Docx1234Document10 pagesACE Finished - Docx1234Nadia umwaliNo ratings yet
- Time Spent Outdoors, Activity Levels, and Chronic Disease Among American AdultsDocument10 pagesTime Spent Outdoors, Activity Levels, and Chronic Disease Among American AdultsSebastian Gonzalez MazoNo ratings yet
- Health Consequences of Adverse Childhood Experiences: A Systematic ReviewDocument9 pagesHealth Consequences of Adverse Childhood Experiences: A Systematic Reviewana raquelNo ratings yet
- Do Children Carry The Weight of DivorceDocument27 pagesDo Children Carry The Weight of DivorceCorina IoanaNo ratings yet
- Allergy - 2014 - Frey - Asthma and Obesity in Children Current Evidence and Potential Systems Biology Approaches PDFDocument15 pagesAllergy - 2014 - Frey - Asthma and Obesity in Children Current Evidence and Potential Systems Biology Approaches PDFHssan GhozlaneNo ratings yet
- Nihms 1531605Document23 pagesNihms 1531605Billis ParaschouNo ratings yet
- This Content Downloaded From 216.249.57.75 On Sun, 10 Dec 2023 23:39:07 +00:00Document52 pagesThis Content Downloaded From 216.249.57.75 On Sun, 10 Dec 2023 23:39:07 +00:00jathumathNo ratings yet
- Work, Health, and Nursing ResearchDocument2 pagesWork, Health, and Nursing ResearchVita EvelynNo ratings yet
- Associations Between Adult Attachment Ratings and Health ConditionsDocument8 pagesAssociations Between Adult Attachment Ratings and Health ConditionsAzzurra AntonelliNo ratings yet
- Obesity and Asthma: E. Rand Sutherland, MD, MPHDocument14 pagesObesity and Asthma: E. Rand Sutherland, MD, MPHAsep HrNo ratings yet
- Overweight and Obesity Associated With Higher Depression Prevalence in Adults: A Systematic Review and Meta-AnalysisDocument12 pagesOverweight and Obesity Associated With Higher Depression Prevalence in Adults: A Systematic Review and Meta-AnalysisLev FyodorNo ratings yet
- Asthma KendingDocument323 pagesAsthma KendingLaith AL-GurayfiiNo ratings yet
- NIH Public Access: Author ManuscriptDocument19 pagesNIH Public Access: Author ManuscriptMaríaA.SerranoNo ratings yet
- Obesity and The Risk of Newly Diagnosed Asthma in School-Age ChildrenDocument10 pagesObesity and The Risk of Newly Diagnosed Asthma in School-Age ChildrenMar LindaNo ratings yet
- Child Mortality in Rural IndiaDocument28 pagesChild Mortality in Rural IndiasrinuswNo ratings yet
- Williams 2008Document11 pagesWilliams 2008Jure ČudičNo ratings yet
- Artigo SobreDocument16 pagesArtigo SobreMarina HeinenNo ratings yet
- PAPER Nutrition in Early Life and The Programming of Adult Disease A Review Ene 2015Document14 pagesPAPER Nutrition in Early Life and The Programming of Adult Disease A Review Ene 2015Joanna Rudman AbzaradelNo ratings yet
- Hea 29 4 446Document8 pagesHea 29 4 446Sinyo TimiselaNo ratings yet
- BPH UnderstandingTheRelationshipDocument25 pagesBPH UnderstandingTheRelationshipXiiAhnChoiPenjahatKunukNo ratings yet
- Nicholson 2000Document13 pagesNicholson 2000Prayogi Dwina AnggaNo ratings yet
- BIology, SES and HealthDocument4 pagesBIology, SES and HealthBethy OreroNo ratings yet
- Methodological DescriptionDocument10 pagesMethodological DescriptionYoki VirgoNo ratings yet
- SSM - Population Health: ArticleDocument10 pagesSSM - Population Health: ArticlemahsusiyatiNo ratings yet
- Obesity and Lung Disease: A Guide to ManagementFrom EverandObesity and Lung Disease: A Guide to ManagementAnne E. DixonNo ratings yet
- Jurnal Kumis KucingDocument7 pagesJurnal Kumis Kucingdinna_dinunNo ratings yet
- Clin Infect Dis. 2001 Guerrant 331 51 DIAREDocument21 pagesClin Infect Dis. 2001 Guerrant 331 51 DIARELamanta JazeNo ratings yet
- Diana New - 2Document5 pagesDiana New - 2dinna_dinunNo ratings yet
- Editorial: Hypertension: A Behavioral Medicine PerspectiveDocument2 pagesEditorial: Hypertension: A Behavioral Medicine Perspectivedinna_dinunNo ratings yet
- TrimyristinDocument3 pagesTrimyristindinna_dinunNo ratings yet
- Prevalens Asma Pada Kelompok Siswa 13-14 Tahun Menggunakan Kuesioner ISAAC Dan Uji Provokasi Bronkus Di Jakarta PusatDocument9 pagesPrevalens Asma Pada Kelompok Siswa 13-14 Tahun Menggunakan Kuesioner ISAAC Dan Uji Provokasi Bronkus Di Jakarta Pusatdinna_dinunNo ratings yet
- Jurnal Aspergillus OryzaeDocument5 pagesJurnal Aspergillus Oryzaedinna_dinunNo ratings yet
- Chapter One - 050546Document5 pagesChapter One - 050546ADEOYE JAMESNo ratings yet
- Topic ProposalDocument11 pagesTopic ProposalXyra Mae PugongNo ratings yet
- Charii Attachment ReportDocument23 pagesCharii Attachment ReportSulemana HanifNo ratings yet
- Ujian Tengah Semester 2020 Mata Kuliah: Penyakit Akibat KerjaDocument21 pagesUjian Tengah Semester 2020 Mata Kuliah: Penyakit Akibat KerjaWidya AnggrainiNo ratings yet
- Intersecting The Academic Gender GapDocument99 pagesIntersecting The Academic Gender GapAlia RamosNo ratings yet
- Timed Up and Go TestDocument6 pagesTimed Up and Go TestcamilaNo ratings yet
- Measuring Population Health OutcomesDocument11 pagesMeasuring Population Health OutcomesRazaCreciaLastrillaMenesesNo ratings yet
- Hubungan Gerd Dengan DepresiDocument8 pagesHubungan Gerd Dengan DepresiDella Elvina RoeslandNo ratings yet
- 2010 NHIS Public Use Variable Summary: Filename - Section: Document Vers Ion DateDocument27 pages2010 NHIS Public Use Variable Summary: Filename - Section: Document Vers Ion DateJin SiclonNo ratings yet
- Informal Sector WorkersDocument16 pagesInformal Sector WorkersNawang WulanNo ratings yet
- Changes in Alcohol Consumption and Risk of DementiaDocument14 pagesChanges in Alcohol Consumption and Risk of DementiaAndrew BelgorodskyNo ratings yet
- Dawson-2000-Alcoholism - Clinical and Experimental ResearchDocument10 pagesDawson-2000-Alcoholism - Clinical and Experimental ResearchManas AuttaNo ratings yet
- MMWR - May 26 2022Document28 pagesMMWR - May 26 2022HNNNo ratings yet
- Housman y Dorman (2005) - The Alameda County StudyDocument7 pagesHousman y Dorman (2005) - The Alameda County StudyFrancesscaNo ratings yet
- Sesi 7c - Studi Kros Seksional 2011Document88 pagesSesi 7c - Studi Kros Seksional 2011rahimulyNo ratings yet
- 2, Sources of DataDocument38 pages2, Sources of DataCollinsNo ratings yet
- Revised Strain Index PDFDocument107 pagesRevised Strain Index PDFjacknewman870No ratings yet
- NHIS Variable SummaryDocument4 pagesNHIS Variable SummaryJin SiclonNo ratings yet
- Kipo2013MixedMethods32455 109334 2 PBDocument11 pagesKipo2013MixedMethods32455 109334 2 PBLaura RodriguesNo ratings yet
- Regression For MultivariateDocument78 pagesRegression For MultivariateNazmulNo ratings yet
- Andersen, R. M. (2008) - National Health Surveys and The Behavioral Model of Health Services Use. Medical Care, 46 (7), 6Document8 pagesAndersen, R. M. (2008) - National Health Surveys and The Behavioral Model of Health Services Use. Medical Care, 46 (7), 6Rifa FauziyyahNo ratings yet
- NHIS CompleteDocument68 pagesNHIS CompleteojogoddyNo ratings yet
- U.S. Filipino Adults' Patterns of CAM Use and Medical Pluralism Secondary Analysis of 2012 National Health Interview SurveyDocument12 pagesU.S. Filipino Adults' Patterns of CAM Use and Medical Pluralism Secondary Analysis of 2012 National Health Interview SurveyKaye Reyes-HapinNo ratings yet
- Mm6805a2 HDocument6 pagesMm6805a2 HAarohi BaviskarNo ratings yet
- Summary Health Statistics For U.S. Adults: National Health Interview Survey, 2012Document171 pagesSummary Health Statistics For U.S. Adults: National Health Interview Survey, 2012Zulfikar BasriNo ratings yet
- Health of Newly Arrived Immigrants in Canada and The United StatesDocument10 pagesHealth of Newly Arrived Immigrants in Canada and The United StatesRafael AlfradiqueNo ratings yet
- Keller Et Al., 2012 PDFDocument15 pagesKeller Et Al., 2012 PDFIonescu DanNo ratings yet
- More Than Ramps A Guide To Improving Health Care Quality and Access For People With DisabilitiesDocument385 pagesMore Than Ramps A Guide To Improving Health Care Quality and Access For People With Disabilitiesiarinadem2011100% (1)
- The Ecology of Medical Care Revisited. Green Etc. New England Journal of Medicine 2001Document5 pagesThe Ecology of Medical Care Revisited. Green Etc. New England Journal of Medicine 2001Jose Mauricio Carvalho LemosNo ratings yet