Professional Documents
Culture Documents
Effects of Exercise Training On Inflammatory Markers in Patients With Heart Failure
Uploaded by
Matheus BarbosaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Effects of Exercise Training On Inflammatory Markers in Patients With Heart Failure
Uploaded by
Matheus BarbosaCopyright:
Available Formats
Heart Fail Rev (2008) 13:3949 DOI 10.
1007/s10741-007-9050-1
Effects of exercise training on inammatory markers in patients with heart failure
Josef Niebauer
Published online: 6 October 2007 Springer Science+Business Media, LLC 2007
Abstract Cardiologists now recognize that the cardiocentric model of heart failure does not sufciently explain the entire traits particular to chronic heart failure. Evidence accumulates, that many features of the syndrome can be explained by the known biological effects of inammatory mediators. Indeed, when expressed in experimental models at concentrations commonly observed in heart failure, inammatory mediators such as tumor necrosis factor-a, interleukin-6, and nitric oxide can produce effects that mimic features of heart failure, including (but not limited to) progressive left-ventricular dysfunction, pulmonary edema, left-ventricular remodeling, and cardiomyopathy. As we witness anti-cytokine therapies and other strategies to avoid an increase in cytokines we have been shown that acute bouts of exercise are associated with an increase in pro-inammatory cytokines and markers of oxidative stress. As a consequence we have been warned exercise may thus even further contribute to the deterioration of heart failure. However, there are several randomized trials which unanimously document that chronicas opposed to acute bouts ofexercise does not only lead to a reduction of cytokines and oxidative stress, but that patients dramatically benet by the increase in maximal oxygen consumption, exercise capacity, quality of life, reduction in hospitalization, morbidity, and mortality. Over the past two decades it has become evident that cytokine research has come to stay and that we will continue to see anti-cytokine treatment strategies for our patients. It is the aim of this
review to shed some more light on the most commonly investigated and most relevant cytokines. Keywords Cytokines Interleukin Tumor necrosis factor alpha Oxidative stress
Introduction Chronic heart failure does not have one underlying cause; it is rather that numerous diseases can eventually lead to the same clinical syndrome of ventricular dysfunction associated with the cardinal symptoms of exercise intolerance, breathlessness, and fatigue. Among the causes of chronic heart failure, the most frequent etiologies include previous myocardial infarction secondary to coronary artery disease, hypertension, and various types of cardiomyopathies like hypertrophic, restrictive, and idiopathic cardiomyopathies, as well as general causes such as arrhythmias, valve diseases, and pericardial and congenital heart diseases. Over the past two decades, it has been recognized that chronic heart failure is no longer seen as merely a failure of the heart to provide adequate cardiac output, it is rather a multisystem syndrome, which not only affects the cardiovascular system but also effects on the humoral, neuroendocrine, renal, and musculoskeletal systems. The former cardiovascular model could not fully explain the various symptoms patients experience or the peripheral manifestations of this disease. Indeed, morbidity and mortality are poorly correlated with changes in hemodynamics [1], and exercise intolerance shows only little correlation with left ventricular ejection fraction, pulmonary capillary wedge pressure or cardiac index [2]. In contrast, however, muscle bulk characteristics have been shown to better predict exercise capacity [3], which
J. Niebauer (&) University Institute of Sports Medicine, Prevention and Rehabilitation Paracelsus Medical University, Institute of Sports Medicine of the State of Salzburg, Lindhofstr. 20, 5020 Salzburg, Austria e-mail: j.niebauer@salk.at
123
40
Heart Fail Rev (2008) 13:3949
underlines the signicance of peripheral factors in symptom generation in chronic heart failure and illustrates the multisystem nature of this disorder [4]. Chronic heart failure is very disabling and a leading cause of morbidity and mortality worldwide with a prognosis comparable to many highly malignant tumors [5]. Hospital admissions are rising despite the evidence that angiotensin converting enzyme inhibitors, angiotensin-2antagonist, aldosterone antagonists, and -blockers improve morbidity and mortality in clinical trials. In fact, the incidence and prevalence rates continuously rise due to a higher life expectancy in the general population, improved medical therapy that leads to prolonged survival after myocardial infarction and enhanced diagnostics that have led to a better detection of heart failure. Despite all this progress, there is no evidence that the prognosis of patients with heart failure has improved. It is the failure of our current medical therapies but also the lack of implementation of current guidelines [6] as well as the modest patient compliance with prescriptions that drives the search for underlying pathomechanisms and intelligent therapies. Chronic heart failure and inammation It has become clear over the past two decades that many features of the syndrome of chronic heart failure can be explained by the known biological effects of inammatory mediators. There has been a considerable increase in research in this area and it continues to remain a widely recognized and discussed eld. Indeed, when expressed in experimental models at the concentrations that are observed in heart failure, inammatory mediators such as tumor necrosis factor-a and nitric oxide can produce effects that mimic some clinical features of heart failure, including (but not limited to) progressive left-ventricular dysfunction, pulmonary edema, left-ventricular remodeling, and cardiomyopathy [7, 8]. Thus, the elaboration of cytokines may be responsible, in part, for disease progression in patients with chronic heart failure [7, 9, 10]. Cytokines The term cytokine refers to a group of protein molecules with relatively small molecular weights (*1530 kDa) that are secreted by cells in response to a variety of different inducing stimuli. As opposed to cytokines, polypeptide hormones are generally produced by a specic cell type in a specic organ and tend to act at short distances in a juxtacrine, paracrine, and autocrine fashion. Cytokines have been shown to play a major role in the pathogenesis of various diseases, including chronic heart failure.
Nevertheless, it has been postulated that when cytokines are expressed at sufciently high concentrations, as this has been shown to occur during heart failure, these molecules may spill over into the circulation, where they may exert endocrine effects [8]. In general, cytokines are thought to exert their effects by binding to specic receptors on the surface of the cell, although cytokines may in some instances have direct membrane effects [11]. Two of the cytokines that have been associated with chronic heart failure include TNF-a and interleukin (IL-) 6 [12]. Both cytokines are low molecular weight proteins, which are secreted by several different cell types and have a variety of immune and/or inammatory actions.
Tumor necrosis factor-a In 1975, tumor necrosis factor-a (TNF-a) was discovered in the search for an anti-cancer treatment [13]. While studying hemorrhagic necrosis of tumors produced by endotoxin, it was found that the serum of bacillus CalmetteGuerin (BCG)infected mice treated with endotoxin contained a substance, then termed tumor necrosis factor, which mimicked the tumor necrotic action of endotoxin itself. A variety of tests indicated that TNF-a was not residual endotoxin, but a factor released from host cells that the authors speculated would probably be macrophages, by endotoxin. In 1985, cachectin, a hormone that suppresses the expression of lipoprotein lipase and other anabolic enzymes in fat, was puried. It was identied as a protein with an isoelectric point of 4.7 and a subunit molecular weight of 17,000. After the purication of cachectin, the complementary DNAs and genes encoding each protein were cloned almost immediately and were shown to be identical [14]. TNF-a exerts its effects via the ubiquitous receptors, i.e., TNF-R55 (TNF receptor 1; TNFR-1) and TNF-R75 (TNF receptor 2; TNFR-2). However, the phenotypic expression of these receptors is markedly different. Whereas TNFR-1 is regarded the most important receptor, giving rise to the intracellular effects of TNF-a including the regulation of nitric oxide synthase (NOS) activity and cytotoxicity, the more abundant TNFR-2 is involved in regulating TNF-a levels. In addition, the extracellular domain fragments of both receptors shed from cell surfaces can be detected as soluble forms (sTNFR-1 and -2). Although there is a strong correlation between elevated sTNFRs and increased mortality in chronic heart failure [15], the role of sTNFRs remains rather controversial. Ferrari et al. [16] have shown that at physiological concentrations, sTNFRs may be able to stabilize the TNF-a molecule, thereby potentiating its long-term actions. However, at higher concentrations sTNFRs inhibit the activity of TNF-a. Therefore, it has
123
Heart Fail Rev (2008) 13:3949
41
been proposed that sTNFRs may regulate TNF-a activity in chronic heart failure. Elevated levels of the pro-inammatory cytokine TNF have been documented in patients with chronic heart failure, and this has been found to correlate with the severity of heart failure [17]. Increased expression of tumor necrosis factor (TNF) has been found in cardiac tissue of patients with chronic heart failure undergoing heart transplantation and the failing heart has been suggested as the cause of immune activation [8]. The original suggestion was that these molecules were produced secondary to the immune activation that occurred in response to tissue injury. This concept was subsequently challenged by the observation from several laboratories that TNF and nitric oxide synthase were expressed by the failing human heart in the absence of a demonstrable inammatory inltrate, which suggested that the heart was a potential site of production of inammatory mediators [18, 19]. It has also been propagated that generalized hypoxia due to low cardiac output, as typically encountered during chronic heart failure, may be the stimulus for increased TNF production. Although the failing myocardium has been reported to be capable of producing TNF, it remains to be seen whether this can explain high systemic TNF levels. Nevertheless, there is good evidence that TNF levels produced by myocytes do have a negative inotropic effect on the myocardium itself [18], and furthermore not only promote left ventricular remodeling [20], but also induce dilated cardiomyopathy in humans [21]. An increased challenge could be the cause of inammatory cytokine activation in chronic heart failure with a resultant increase in TNF-a production. In a previous study, it was demonstrated that patients with high sCD14 levels, which are indicative of endotoxincell interaction and shedding of CD14 from the cell membrane, have markedly increased levels of TNF-a, sTNFR-1, -2, and intercellular adhesion molecule-1 (ICAM-1) [22], supporting the hypothesis of increased endotoxin levels. Indeed, we could demonstrate that endotoxin concentrations and proinammatory cytokines are elevated in patients with heart failure who have peripheral edema. Raised endotoxin concentrations were normalized by lengthened diuretic treatment. Endotoxemia in these patients was not associated with a strong acute-phase response that would have led to an increased hepatic LBP synthesis and subsequent blocking of lipopolysaccharide effects [23]. These results lend credence to the hypothesis that bacterial endotoxin may be an important stimulus of immune activation in patients with chronic heart failure. These ndings were in keeping with the hypothesis [22] that acute venous congestion could lead to altered gut permeability for bacteria, endotoxin, or both, and to translocation of these materials into the circulation. To
further test this hypothesis, we set out to invasively assess endotoxin levels in hepatic veins and left ventricles of patients with acute onset of decompensated heart failure [24]. It was found that levels of endotoxin were systemically elevated during acute heart failure and signicantly higher in hepatic veins than the left ventricles. As a result of clinical recompensation endotoxin levels were not different between sites anymore. Thus we concluded that higher levels of endotoxin in hepatic veins as compared to the left ventricles during acute heart failure are suggestive of bacterial or endotoxin translocation from the bowel into the blood stream. Most recently, there have been two reports on improved levels of TNF-a, one after improving heart function through intensied heart failure therapy [25], and one study reported that therapy with the phosphodiesterase inhibitor pentoxyphilline given to patients with chronic heart failure for 6 months led to signicant reduction in TNF-a levels and improved left ventricular ejection fraction [26]. Despite these pioneering reports, no link between a pathogenic process and cytokine activation has been documented in human beings with heart failure or in animal models. The cause of increased cytokine production in patients with heart failure remains unknown. Indeed, the transition from bench to bedside would not be easy. Specically, large scale clinical trials (RENAISSANCE and RECOVER) using the soluble TNF-receptor fusion protein etanerceptthat worked so well in cell culture, animal experiments, and human pilot studies [27 29]were stopped, once it became obvious that superiority over placebo would not be achieved [30, 31]. Nevertheless, in our effort to nd better treatments for heart failure and cardiac cachexia, trials like these are vital, since they may show effectiveness in subgroups and furthermore help us to both design better drugs and studies.
Interleukin-6 Interleukin-6 is a pro-inammatory cytokine, which has been shown to be elevated in patients with chronic heart failure [32], and it is associated with severe symptoms of heart failure as demonstrated by a higher incidence of New York Heart Association (NYHA) functional class III and IV, worse left ventricular function, and a poorer prognosis [8, 33]. In one study, it was demonstrated that plasma IL-6 levels not only increased signicantly from the femoral artery to the femoral vein in normal subjects and in patients with chronic heart failure, but that there was also a signicant arteriovenous IL-6 spill over in the leg which increased with the severity of chronic heart failure. Furthermore, treatment with beta-adrenergic blocking agents
123
42
Heart Fail Rev (2008) 13:3949
showed an independent and signicant negative relation with plasma IL-6 levels indicative of an activation of the sympathetic nervous system [33]. The mechanism by which IL-6 exerts its deleterious effects remains to be elucidated. However, there is initial evidence that suggests that IL-6 is involved in the development of ventricular hypertrophy via stimulation of a glycoprotein 130 receptor subunit expressed on cardiac myocytes [34].
Exercise training: a poly-pill Although the known benecial effects of exercise training are increasingly recognized, it is only with great delay that it is becoming part of the routine management of chronic heart failure [35]. While denitive data on the effects of training on prognosis are not yet available, many of the variables associated with a poor prognosis, such as exercise performance, [36] sympathetic [37] and neurohormonal activation [3840] peripheral hypoxia [41], and endothelial function [42] improve with exercise training. Also the cardinal symptom of heart failure, i.e., shortness of breath on exertion and the resulting impaired exercise capacity measured as peak VO2 improves by up to 20% [43, 44]. Training regimes have generally shown an improvement in endothelial function in normal subjects [45] and patients with heart failure [46]. Furthermore, a recent meta-analysis supports the notion that training may even improve prognosis [47].
Exercise and cytokines It is well known that acute bouts of exercise lead to increases in markers of endothelial damage such as VCAM and p-selectin, pro-inammatory cytokines including TNFa and interleukin 6, peripheral hypoxia and may induce free radical formation [48]. It is indeed ndings like these that raised fears that exercise training might be rather deleterious than helpful in patients with chronic heart failure. In order to shed further light on the effects of chronic exercise training as opposed to acute bouts of exercise, several randomized trials have been carried out [36, 39, 41, 43, 4956] to investigate the relation between an exercise training regime for heart failure patients and markers of pro-inammatory cytokine activation and endothelial damage. Out of a panoply of markers which we identied in current literature to be of relevance we chose e-selectin, since it is expressed on inammed endothelial cells in response to treatment with inammatory cytokines and is involved in the process of binding white cells to the
endothelium; sICAM, which is elevated in inammatory states, including atheroma and heart failure [57], and mediates the binding of inammatory cells to vascular endothelium [58]; and CD14, which is the principal receptor for the complex of endotoxin and its binding protein, endotoxin [59] which results in the up-regulation of cell surface molecules, including adhesion molecules. Our results showed that while there were higher baseline levels of circulating TNF, its soluble receptors TNF-R1 and -R2, IL-6, e-selectin, sICAM, and CD14, a training regime sufcient to induce a systemic training effect in heart failure patients did not cause an increase in these cytokines and endothelial factors that might be associated with an adverse outcome. Other studies, however, did not only report the lack of an exercise-induced cytokine activation but also found a decrease in at least some cytokines or their soluble receptors [39, 51, 60, 61]. Since these studies did not uniformly report improved levels of TNF-a, interleukin 6, and other cytokines, it remains unclear what causes such a heterogeneous response to exercise training. Taken all trials together, it may be speculated that a training period of only 8 weeks as chosen in our study may not be long enough to induce changes in cytokines, since most studies were carried out 1226 weeks. Also, our patients only showed mildly impaired oxygen consumption and exercise intolerance. It may be speculated that despite pronounced pathological ndings in the echocardiogram, the stimulus for cytokine activation at baseline was not strong enough to induce a state of cytokine activation that would be more amenable to an exercise-based intervention. This hypothesis nds support by several other studies that could neither detect a decrease in serum cytokine levels after chronic exercise training [50, 51, 60]. Like in our study, their patients presented with rather mild CHF, well comparable with NYHA class II, and only had mildly elevated cytokine levels at baseline.
Anabolic/catabolic imbalance Role of cytokines Chronic heart failure has a poor outcome [62] and in some patients it can even deteriorate further to cardiac cachexia, a wasting syndrome, which is associated with a particularly poor prognosis [63]. Also in these patients TNF levels have been reported to be elevated [17, 64], and they have been found to be the strongest predictor of the degree of previous weight loss. This is in keeping with animal experiments in which skeletal muscle wasting and apoptosis could be induced by TNF [65, 66], thus providing an explanation for the correlation observed in humans. Indeed, an association
123
Heart Fail Rev (2008) 13:3949
43
between increased levels of serum TNF levels and subjective [67] (NYHA class) as well as objective parameters of exercise in tolerance [12] (quadriceps muscle strength) have been reported. Further alterations that have been described in the musculature of patients with chronic heart failure comprise muscle atrophy, increased ber type switching from oxidative type I to glycolytic type IIb bers, decreases in myosin heavy-chain type I bers, decreases in mitochondrial enzymes involved in oxidation of fatty acids, as well as decreases in cytochrome c oxidase and mitochondrial volume density [68, 69]. Some of these alterations are amenable to exercise training. Ennezat et al. reported that exercise training induced a nearly two-fold increase in Cu/Zn superoxide dismutase and glutathione peroxidase in skeletal muscle biopsies [70]. Furthermore, in the skeletal musculature of patients with chronic heart failure, there is an increase in iNOS expression, TNF, IL-1-beta, and IL-6 that can all be benecially modied by exercise training, which remains the most useful intervention to correct these alterations [51, 54, 71]. Cytokines may affect muscle metabolism and strength by direct effects such as the expression of the sarcoplasmic reticulum Ca++ adenosine triphosphatase and phospholamdan [72] or by the inducible isoform of nitric oxide synthase (iNOS), which has been shown to be stimulated by IL-1 beta and TNF-alpha via activation of nuclear factor-kappa-B [73]. The elevated expression of iNOS was conrmed in skeletal muscle biopsies from patients with CHF [54, 74] and it has been proposed that excessive intracellular levels of nitric oxide produced by iNOS may inhibit key aerobic enzymes like cytochrome C oxidase (COX) and reduce peak oxygen uptake [54]. Skeletal muscle biopsies from patients with moderate CHF (NYHA class II) show increased expression of TNFalpha, IL-1-beta, and IL-6 independent from serum cytokine levels and in the absence of pro-inammatory monocytes/macrophages, which indicates that skeletal myocytes may produce cytokines in a parakrine/autokrine fashion in quantities large enough to induce iNOS expression [51]. In the same study, the expression of iNOS was conrmed in skeletal muscle biopsies and was reduced by exercise training, which was paralleled by a decrease in nitrotyrosine levels. It may be speculated that hypoperfusion and oxidative stress might be the initial proinammatory stimuli.
Growth hormoneInsulin-like growth factor 1 axis In cardiac cachexia, there is an imbalance between catabolic and anabolic steroid metabolism and cytokine
activation both of which appear to be related to the loss of muscle bulk and the development of cachexia in chronic heart failure. Furthermore, there is some evidence for the existence of a catabolic state within skeletal muscle in this syndrome. Abnormalities of the growth hormoneinsulinlike growth factor I (IGF-I) axis have been described in CHF. These include raised levels of growth hormone coexistent with inappropriately normal levels of IGF-I being associated with the presence of cachexia [12, 75]. This growth hormone resistant state is not only found in cachexia but also in some patients with untreated heart failure. We have previously shown that low IGF-I levels characterize a subgroup of patients with chronic heart failure in whom body composition is unfavorably altered, which coincides with cytokine and neurohormonal activation [12]. Loss of muscle bulk happens early in the course of chronic heart failure and the development of cachexia is an adverse prognostic feature [63]. The origin of the weight loss is not clear, but recent studies have drawn attention to the potential importance of neurohormonal and immune activation. Tumor necrosis factor-a is elevated in chronic heart failure, there is an increase in the ratio between circulating levels of catabolic and anabolic steroids and an insulin-resistant state develops [76]. Also, the resting metabolic rate of patients with heart failure is increased and resting leg oxygen consumption has been shown to be increased. We have previously reported that patients with low IGF-1 levels have reduced muscle strength even after correction for muscle bulk, and there was a direct relationship between the degree of growth hormone sensitivity, as represented by the IGF-1:GH ratio, and body mass index [12]. Further, although leg cross sectional area was unchanged in the low IGF-1 group, there was a reduction in muscle cross-sectional area and an increase in the ratio of fat to muscle in the leg. These ndings suggest a possible role for growth hormone resistance in the development of muscle loss in chronic heart failure. Thus, for future growth hormone trials greater care has to be taken to select patients without acquired growth hormone resistance, which could be done on the basis of patients baseline growth hormone binding protein levels, or their rst-dose IGF-I response to a test dose of growth hormone [76]. Muscle loss can also be explained by a decrease in the number of IGF-1 receptors. This has been shown to be associated with massive apoptosis in some tumor models, and overexpression of IGF-1 protects cells from apoptosis [77]. Antibodies against the IGF-1 receptor [78] or the induction of IGF-1 receptor mutant [79] also inhibit tumor growth. The frequency with which apoptosis is seen in tissue samples is increased in chronic heart failure [80]. It may be that in heart failure, as IGF-I levels decline, a protective factor is removed permitting apoptosis of skeletal muscle cells. Interestingly, exercise training has been
123
44
Heart Fail Rev (2008) 13:3949
shown useful to improve local IGF-I expression without signicant changes of systemic parameters of the GH/IGF-I axis. This illustrates the therapeutic potential of exercise training to attenuate peripheral skeletal muscle alterations, which includes local IGF-I expression [49]. In addition, we found TNF levels to be signicantly higher in patients with low IGF-1 levels than in those with normal to high levels, and TNF levels were inversely correlated with muscle bulk [12]. It has previously been published that TNF-induced cell killing is prevented by IGF-1 alone [81]. Therefore, there may be a link between low IGF-1 levels and reduced muscle bulk in patients with congestive heart failure. Additionally, there may also be a direct link between IGF-1 deciency and raised TNF-a levels. It has repeatedly been shown in animal studies that administration of IGF-1 reduces mucosal atrophy and improves gut barrier function, thereby reducing bacterial translocation [82, 83]. It could be speculated that lower IGF-1 levels favor bacterial translocation in CHF patients, which could explain increased TNF-a levels as observed in our study, which signicantly correlate with soluble CD14 and endotoxin [23].
Role of endothelial function Mechanisms that lead to increased levels of cytokines in the musculature include hypperfusion as a result of increased vascular resistance in the periphery. This can be the result of endothelial dysfunction [55, 84], but also an increased sympathetic tone that may result in an impaired local vasodilatory response with subsequent hypoperfusion, tissue ischemia and generation of reactive oxygen species (ROS) [85, 86]. Both have been shown to be amenable to shear stress or exercise training by attenuating NO release [55, 84], or by upregulating central antioxidative and suppressing central pro-oxidant mechanisms which may contribute to the exercise training-induced benecial effects on autonomic activity [85], of which the latter will not be discussed in this review. Exercise intolerance may in part be related to impaired ow-dependent vasodilation in conductance vessels as compared with normal subjects, which suggests that there is vascular endothelial dysfunction of large conduit vessels. Altered endothelial function might thus contribute to impaired tissue perfusion in heart failure. Exercise training programs produce an increase in exercise capacity and at the same time an improvement in endothelial function [55, 84]. The cause of the impaired endothelial function has not yet been fully elucidated. It may be related to abnormalities of the vasodilator nitric oxide (NO), although there are conicting reports concerning the effects of heart failure on NO in the literature. Oxidative stress secondary to increased
free radical formation is reported to be common in chronic heart failure, and has an adverse effect on cardiac function and outcome [5]. Free radicals can inactivate NO and its biological activity. Indeed, improved endothelial function and lower total peripheral resistance after training may reduce skeletal muscle ischemia during exercise. Since nitric oxide acts as a free radical scavenger, nitric oxide might directly reduce local oxidative stress. It also augments vascular endothelial cell superoxide dismutase expression in vascular smooth muscle cells [87]. In fact, Linke et al. demonstrated an antioxidative effect of exercise training in skeletal muscle of patients with chronic heart failure [50]. Superoxide dismutase (SOD), catalase (Cat), and glutathione peroxidase (GPX) activity was reduced whereas nitrotyrosin formation was increased. Exercise training augmented GPX and Cat activity in skeletal musculature and decreased nitrotyrosine production. In their study, the reduced activity of major antioxidative enzymes in the skeletal musculature of CHF patients was associated with increased local oxidative stress. Basal release of nitric oxide in patients with chronic heart failure has been variously reported to be decreased, normal or elevated. In patients with mild heart failure (NYHA class II), we found that patients without oral nitrates showed signicantly lower levels of NO than healthy controls. This is in keeping with previously reported diminished endothelial function in patients with heart failure [55, 84], which is due to a functional imbalance between vasodilation and vasoconstriction in favor of constricting agents. It has repeatedly been shown that endothelial function can be improved by exercise training in normal subjects, and patients with heart failure [55, 84]. The mechanism of benet might be due to a shear stress induced release of both the vasodilators nitric oxide and prostacyclin and an inhibition of the release of the vasoconstrictor endothelin-1 [88]. Furthermore, when exercise training is performed chronically it is not associated with a deleterious increase in markers of pro-inammatory cytokines and endothelial damage [41]. In our study, however, levels of NO remained unaltered by exercise training. This does not come as a surprise, since exercise training does not necessarily lead to a detectable increase in systemic nitric oxide levels, whereas it does increase local expression of mRNA for nitric oxide synthase, augment nitric oxide activity, and enhance endothelium-dependent vasodilation at the site of increased shear stress [8991]. There is thus an increased sensitivity of the endothelium and vascular smooth muscle cells to vasodilatory stimuli. The lack of an increase in systemic levels of NO might even be benecial, since patients with heart failure have increased inducible NO synthase activity, and local overproduction of NO in cardiac tissue [92] is known to exert a negative
123
Heart Fail Rev (2008) 13:3949
45
inotropic effect. Furthermore, to date it is not clear whether increased levels of NO secondary to the application of oral nitrates have any benecial effects on patients quality of life, progression of the disease or prognosis. There is an ongoing debate about what type, frequency, and intensity of exercise should be prescribed in order to optimize its effects on endothelial function. A practical approach is being illustrated in Fig. 1. Nevertheless, this question has not fully been answered even though it has been recently addressed again by Wisloff et al. [93] who compared moderate continuous training with aerobic interval training. They found superior effects in the aerobic interval group which included reverse LV remodeling, decline in LV end-diastolic and end-systolic volumes, decrease in pro-brain natriuretic peptide, improvement in brachial artery ow-mediated dilation, an increase in LV ejection fraction, improved mitochondrial function in lateral vastus muscle, decreased levels of reactive oxygen species, and improved NO-mediated endothelial function, providing evidence that aerobic interval training might be the preferred mode of exercise training in these patients (Tables 1, 2).
hydrogen peroxide and superoxide. Production of reactive oxygen species by xanthine oxidase has been implicated in the reoxygenation injury resulting from ischemia and reperfusion [95]. However, it has also been shown that the increased formation of purine substrates for xanthine oxidase can become more important for generating reactive oxygen species than is a major conversion of xanthine dehydrogenase to xanthine oxidase [96]. During exercise ATP is converted to ADP and AMP to supply energy for muscular contraction. When ATP breakdown exceeds re-synthesis, accumulation of ADP and AMP then activates the purine nucleotide cycle and a degradation cascade producing inosine monophosphate, hypoxanthine, and in some tissues, xanthine, and uric acid [97]. Venous hypoxanthine levels are higher in CHF patients than in healthy subjects, and increase in both in response to acute exercise [98]. In a previous study, we assessed levels of hypoxanthine at baseline as well as after a program of unsupervised, home-based exercise training. At baseline, levels were raised suggesting that heart failure patients are in a state of hypoxia. Exercise training was able to reduce levels of this pro-oxidant substrate and potentially oxidative stress.
Purine pathway Conclusion CHF is associated with increased oxidative stress, as indicated by reduced antioxidants, a depressed oxidationreduction (redox) state and increased lipid peroxidation. Oxidative stress can cause contractile dysfunction [94], which may contribute to the progression of heart failure. Xanthine oxidase is formed from xanthine dehydrogenase under conditions of both hypoxia and hyperoxia. The oxidase form of the enzyme utilizes molecular oxygen as a cofactor for the conversion of hypoxanthine and xanthine to uric acid, and this process results in production of both
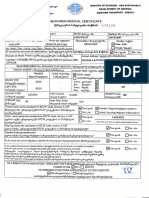
Fig. 1 Hemodynamic effects of chronic exercise training
R e s p i r at o r y s y s t e m : Inspiratory muscle strength Nervous System: Sympathetic Parasympathetic
Despite the growing number of therapeutic options the number of patients with chronic heart failure continues to rise. Exercise training has been shown to be associated with decreased cytokine activation both locally and systemically. It exerts a panoply of positive changes not only to the myocardium but also systemically, and is associated with a marked increase in maximal oxygen uptake, quality of life, reduced rate of hospitalization, and mortality, so it can safely be considered a poly-pill. In the age of
M u s c u la t u r e : Oxid ativ e ca pac it y O xi d a t iv e s t r es s P r o -i n f l a m m a t o r y c yt ok i n e s Neuro-endocrine system: Aldosterone Angiotensin release Ox id at i v e str e ss P r o - i n f l a m m a to ry cy t o k i n e s / Vasculature: Endothelial function O x i d a t i ve st r e s s
Venous Return
Heart Rat e Vascular Resistance
Va s c u l a r r e m o d e l i n g Vascular Resistance
Cardiac and vascular remodeling Vascular Resistance
Le f t ve n tr i c u la r f ill ing
E je ct io n f r a ct i o n
123
46 Table 1 Common exercise prescription according to clinical status NYHA VO2 max Frequency of sessions per week I II III IIIb [25 2025 \20 \15 37 35 35 3 duration 3060 20 10 \10 Intensity Watts/kg [1 [1 [1 \1
Heart Fail Rev (2008) 13:3949
Strength training beats/min 7080 60 60 5060 Optional Optional Endurance Interval
Table 2 Effects of exercise training on selected proinammatory cytokines
Variables TN F-a :
Negative effects/associations Negative inotrop Higher NYHA class Decompensation Poorer prognosis
Chronic exercise training l;
IL-6 :
Negative inotrop Higher NYHA class Poorer prognosis
l;
IGF-1 ;
Apoptosis Loss of muscle mass/strength Poor prognosis
Local IGF (muscle) : Systemic l ;
iNOS :
Inhibit aerobic enzymes Apoptosis Reduce peak oxygen uptake
evidencebased medicine state-of-the-art therapy is not complete if exercise training is not included. Efforts on all ends have to be intensied in order to offer exercise training to as many of our patients as possible.
References
1. Cohn JN, Archibald DG, Ziesche S, Franciosa JA, Harston WE, Tristani FE, Dunkman WB, Jacobs W, Francis GS, Flohr KH (1986) Effect of vasodilator therapy on mortality in chronic congestive heart failure Results of a Veterans Administration Cooperative Study. N Engl J Med 314:15471552 2. Franciosa JA, Park M, Levine TB (1981) Lack of correlation between exercise capacity and indexes of resting left ventricular performance in heart failure. Am J Cardiol 47:3339 3. Volterrani M, Clark A, Ludman P, Swan J, Adamopoulos S, Piepoli M, Coats A (1994) Determinants of exercise capacity in chronic heart failure. Eur Heart J 15:801809 4. Clark A, Poole-Wilson P, Coats A (1996) Exercise limitation in chronic heart failure: the central role of the periphery. J Am Coll Cardiol 28:10921102 5. Stewart S (2003) Prognosis of patients with heart failure compared with that of common types of cancer. Heart Fail Monit 3:8794 6. Drechsler K, Dietz R, Klein H, Wollert KC, Storp D, Molling J, Zeymer U, Niebauer J (2005) Euro heart failure survey. Medical treatment not in line with current guidelines. Z Kardiol 94:510 515
7. Seta Y, Shan K, Bozkurt B, Oral H, Mann DL (1996) Basic mechanisms in heart failure: the cytokine hypothesis. J Card Fail 2:243249 8. Torre-Amione G, Kapadia S, Lee J, Durand JB, Bies RD, Young JB, Mann DL (1996) Tumor necrosis factor-alpha and tumor necrosis factor receptors in the failing human heart. Circulation 93:704711 9. Gullestad L, Aukrust P (2001) The cytokine network in heart failure: pathogenic importance and potential therapeutic targets. Heart Fail Monit 2:813 10. Paulus WJ (2000) Cytokines in heart failure. Heart Fail Monit 1:5056 11. Kagan BL, Baldwin RL, Munoz D, Wisnieski BJ (1992) Formation of ion-permeable channels by tumor necrosis factor-alpha. Science 255:14271430 12. Niebauer J, Paum CD, Clark AL, Strasburger CJ, Hooper J, Poole-Wilson PA, Coats AJ, Anker SD (1998) Decient insulinlike growth factor I in chronic heart failure predicts altered body composition, anabolic deciency, cytokine and neurohormonal activation. J Am Coll Cardiol 32:393397 13. Carswell EA, Old LJ, Kassel RL, Green S, Fiore N, Williamson B (1975) An endotoxin-induced serum factor that causes necrosis of tumors. Proc Natl Acad Sci U S A 72:36663670 14. Beutler B, Greenwald D, Hulmes JD, Chang M, Pan YC, Mathison J, Ulevitch R, Cerami A (1985) Identity of tumour necrosis factor and the macrophage-secreted factor cachectin. Nature 316:552554 15. Rauchhaus M, Doehner W, Francis DP, Davos C, Kemp M, Liebenthal C, Niebauer J, Hooper J, Volk HD, Coats AJ, Anker SD (2000) Plasma cytokine parameters and mortality in patients with chronic heart failure. Circulation 102:30603067
123
Heart Fail Rev (2008) 13:3949 16. Ferrari R, Bachetti T, Confortini R, Opasich C, Febo O, Corti A, Cassani G, Visioli O (1995) Tumor necrosis factor soluble receptors in patients with various degrees of congestive heart failure [see comments]. Circulation 92:14791486 17. Anker S, Clark A, Kemp M, Salsbury C, Teixeira M, Hellewell P, Coats AJS (1997) Tumour necrosis factor and steroid metabolism in chronic heart failure: possible relation to muscle wasting. J Am Coll Cardiol 30:9971001 18. Torre-Amione G, Kapadia S, Lee J, Bies RD, Lebovitz R, Mann DL (1995) Expression and functional signicance of tumor necrosis factor receptors in human myocardium. Circulation 92:14871493 19. Habib FM, Springall DR, Davies GJ, Oakley CM, Yacoub MH, Polak JM (1996) Tumour necrosis factor and inducible nitric oxide synthase in dilated cardiomyopathy [see comments]. Lancet 347:11511155 20. Suffredini AF, Fromm RE, Parker MM, Brenner M, Kovacs JA, Wesley RA, Parrillo JE (1989) The cardiovascular response of normal humans to the administration of endotoxin [see comments]. N Engl J Med 321:280287 21. Hegewisch S, Weh HJ, Hossfeld DK (1990) TNF-induced cardiomyopathy. Lancet 335:294295 22. Anker S, Egerer K, Volk H-D, Kox W, Poole-Wilson P, Coats AJS (1997) Elevated soluble CD14 receptors and altered cytokines in chronic heart failure. Am J Cardiol 79:14261430 23. Niebauer J, Volk HD, Kemp M, Dominguez M, Schumann RR, Rauchhaus M, Poole-Wilson PA, Coats AJS, Anker SD (1999) Endotoxin and immune activation in chronic heart failure: a prospective cohort study. Lancet 353:18381842 nauer M, Thiele H, Anker SD, Schuler G, 24. Peschel T, Scho Niebauer J (2003) Invasive assessment of bacterial endotoxin and inammatory cytokines in patients with acute heart failure. Eur J Heart Fail 5:609614 25. Liu L, Zhao SP (1999) The changes of circulating tumor necrosis factor levels in patients with congestive heart failure inuenced by therapy. Int J Cardiol 69:7782 26. Sliwa K, Skudicky D, Candy G, Wisenbaugh T, Sareli P (1998) Randomised investigation of effects of pentoxifylline on leftventricular performance in idiopathic dilated cardiomyopathy. Lancet 351:10911093 27. Bozkurt B, Torre-Amione G, Warren MS, Whitmore J, Soran OZ, Feldman AM, Mann DL (2001) Results of targeted anti-tumor necrosis factor therapy with etanercept (ENBREL) in patients with advanced heart failure. Circulation 103:10441047 28. Deswal A, Bozkurt B, Seta Y, Parilti-Eiswirth S, Hayes FA, Blosch C, Mann DL (1999) Safety and efcacy of a soluble P75 tumor necrosis factor receptor (Enbrel, etanercept) in patients with advanced heart failure [see comments]. Circulation 99:32243226 29. Kalra D, Bozkurt B, Deswal A, Torre-Amione G, Mann DL (2001) Experimental options in the treatment of heart failure: the role of cytokine antagonism. Heart Fail Monit 1:114121 30. Mann DL, McMurray JJ, Packer M, Swedberg K, Borer JS, Colucci WS, Djian J, Drexler H, Feldman A, Kober L, Krum H, Liu P, Nieminen M, Tavazzi L, van Veldhuisen DJ, Waldenstrom A, Warren M, Westheim A, Zannad F, Fleming T (2004) Targeted anticytokine therapy in patients with chronic heart failure: results of the Randomized Etanercept Worldwide Evaluation (RENEWAL). Circulation 109:15941602 31. Aukrust P, Yndestad A, Ueland T, Damas JK, Gullestad L (2006) Anti-inammatory trials in chronic heart failure. Heart Fail Monit 5:29 32. Aukrust P, Ueland T, Lien E, Bendtzen K, Muller F, Andreassen AK, Nordoy I, Aass H, Espevik T, Simonsen S, Froland SS, Gullestad L (1999) Cytokine network in congestive heart failure secondary to ischemic or idiopathic dilated cardiomyopathy. Am J Cardiol 83:376382
47 33. Tsutamoto T, Hisanaga T, Wada A, Maeda K, Ohnishi M, Fukai D, Mabuchi N, Sawaki M, Kinoshita M (1998) Interleukin6 spillover in the peripheral circulation increases with the severity of heart failure, and the high plasma level of interleukin- 6 is an important prognostic predictor in patients with congestive heart failure. J Am Coll Cardiol 31:391398 34. Kunisada K, Hirota H, Fujio Y, Matsui H, Tani Y, YamauchiTakihara K, Kishimoto T (1996) Activation of JAK-STAT and MAP kinases by leukemia inhibitory factor through gp130 in cardiac myocytes [see comments] [published erratum appears in Circulation 1997 Apr 1;95(7):1975]. Circulation 94:26262632 35. Niederseer D, Thaler C, Niebauer J (2007) The failing heart. N Engl J Med 356:2545 36. Coats AJ, Adamopoulos S, Meyer TE, Conway J, Sleight P (1990) Effects of physical training in chronic heart failure. Lancet 335:6366 37. Gordon A, Tyni-Lenne R, Jansson E, Kaijser L, TheodorssonNorheim E, Sylven C (1997) Improved ventilation and decreased sympathetic stress in chronic heart failure patients following local endurance training with leg muscles. J Card Fail 3:312 veri H, Leinonen H, Ha rko nen M (1999) The 38. Kiilavuori K, Na effect of physical training on hormonal status and exertional hormonal response in patients with chronic congestive heart failure. Eur Heart J 20:456464 39. Adamopoulos S, Parissis J, Kroupis C, Georgiadis M, Karatzas D, Karavolias G, Koniavitou K, Coats AJ, Kremastinos DT (2001) Physical training reduces peripheral markers of inammation in patients with chronic heart failure. Eur Heart J 22:791797 40. Braith RW, Welsch MA, Feigenbaum MS, Kluess HA, Pepine CJ (1999) Neuroendocrine activation in heart failure is modied by endurance exercise training. J Am Coll Cardiol 34:11701175 41. Niebauer J, Clark AL, Webb-Peploe KM, Boger R, Coats AJ (2005) Home-based exercise training modulates pro-oxidant substrates in patients with chronic heart failure. Eur J Heart Fail 7:183188 42. Hambrecht R, Wolf A, Gielen S, Linke A, Hofer J, Erbs S, Schoene N, Schuler G (2000) Effect of exercise on coronary endothelial function in patients with coronary artery disease. N Engl J Med 342:454460 43. Niebauer J, Clark AL, Webb-Peploe KM, Coats AJ (2005) Exercise training in chronic heart failure: effects on proinammatory markers. Eur J Heart Fail 7:189193 44. Keteyian SJ, Levine AB, Brawner CA, Kataoka T, Rogers FJ, Schairer JR, Stein PD, Levine TB, Goldstein S (1996) Exercise training in patients with heart failure. A randomized, controlled trial. Ann Intern Med 124:10511057 45. Goto C, Higashi Y, Kimura M, Noma K, Hara K, Nakagawa K, Kawamura M, Chayama K, Yoshizumi M, Nara I (2003) Effect of different intensities of exercise on endothelium-dependent vasodilation in humans: role of endothelium-dependent nitric oxide and oxidative stress. Circulation 108:530535 46. Kobayashi N, Tsuruya Y, Iwasawa T, Ikeda N, Hashimoto S, Yasu T, Ueba H, Kubo N, Fujii M, Kawakami M, Saito M (2003) Exercise training in patients with chronic heart failure improves endothelial function predominantly in the trained extremities. Circ J 67:505510 47. Piepoli MF, Davos C, Francis DP, Coats AJ, ExTraMATCH Collaborative (2004) Exercise training meta-analysis of trials in patients with chronic heart failure (ExTraMATCH). Br Med J 328:189 48. Jenkins RR (1988) Free radical chemistry: relationship to exercise. Sports Med 5:156170 49. Hambrecht R, Schulze PC, Gielen S, Linke A, Mobius-Winkler S, Erbs S, Kratzsch J, Schubert A, Adams V, Schuler G (2005) Effects of exercise training on insulin-like growth factor-I
123
48 expression in the skeletal muscle of non-cachectic patients with chronic heart failure. Eur J Cardiovasc Prev Rehabil 12:401406 Linke A, Adams V, Schulze PC, Erbs S, Gielen S, Fiehn E, Mobius-Winkler S, Schubert A, Schuler G, Hambrecht R (2005) Antioxidative effects of exercise training in patients with chronic heart failure: increase in radical scavenger enzyme activity in skeletal muscle. Circulation 111:17631770 bius-Winkler S, Linke A, Erbs S, Yu J, Gielen S, Adams V, Mo Kempf W, Schubert A, Schuler G, Hambrecht R (2003) Antiinammatory effects of exercise training in the skeletal muscle of patients with chronic heart failure. J Am Coll Cardiol 42:861868 Adams V, Jiang H, Yu J, Mobius-Winkler S, Fiehn E, Linke A, Weigl C, Schuler G, Hambrecht R (1999) Apoptosis in skeletal myocytes of patients with chronic heart failure is associated with exercise intolerance. J Am Coll Cardiol 33:959965 Hambrecht R, Niebauer J, Fiehn E, Kalberer B, Offner B, bler W, Schuler G (1995) Hauer K, Riede U, Schlierf G, Ku Physical training in patients with stable chronic heart failure: effects on cardiorespiratory tness and ultrastructural abnormalities of leg muscles. J Am Coll Cardiol 25:12391249 Hambrecht R, Adams V, Gielen S, Linke A, Mobius-Winkler S, Yu J, Niebauer J, Jiang H, Fiehn E, Schuler G (1999) Exercise intolerance in patients with chronic heart failure and increased expression of inducible nitric oxide synthase in the skeletal muscle. J Am Coll Cardiol 33:174179 Hambrecht R, Fiehn E, Weigl C, Gielen S, Hamann C, Kaiser R, Yu J, Adams V, Niebauer J, Schuler G (1998) Regular physical exercise corrects endothelial dysfunction and improves exercise capacity in patients with chronic heart failure. Circulation 98:27092715 Hambrecht R, Fiehn E, Yu J, Niebauer J, Weigl C, Hilbrich L, Adams V, Riede U, Schuler G (1997) Effects of endurance training on mitochondrial ultrastructure and ber type distribution in skeletal muscle of patients with stable chronic heart failure. J Am Coll Cardiol 29:10671073 Devaux B, Scholz D, Hirche A, Klovekorn WP, Schaper J (1997) Upregulation of cell adhesion molecules and the presence of low grade inammation in human chronic heart failure. Eur Heart J 18:470479 Takahashi M, Ikeda U, Masuyama J, Kitagawa S, Kasahara T, Saito M, Kano S, Shimada K (1994) Involvement of adhesion molecules in human monocyte adhesion to and transmigration through endothelial cells in vitro. Atherosclerosis 108:7381 Hailman E, Lichenstein HS, Wurfel MM, Miller DS, Johnson DA, Kelley M, Busse LA, Zukowski MM, Wright SD (1994) Lipopolysaccharide (LPS)-binding protein accelerates the binding of LPS to CD14. J Exp Med 179:269277 Conraads VM, Beckers P, Bosmans J, De Clerck LS, Stevens WJ, Vrints CJ, Brutsaert DL (2002) Combined endurance/resistance training reduces plasma TNF-a receptor levels in patients with chronic heart failure and coronary artery disease. Eur Heart J 23:18541860 LeMaitre JP, Harris S, Fox KAA, Denvir M (2004) Change in circulating cytokines after 2 forms of exercise training in chronic stable heat failure. Am Heart J 147:100105 Niebauer J, Clark AL, Anker SD, Coats AJS (1999) Three year mortality in heart failure patients with very low left ventricular ejection fractions. Int J Cardiol 70:245247 Anker S, Ponikowski P, Varney S, Chua T, Clark A, WebbPeploe K, Harrington D, Kox W, Poole-Wilson P, Coats A (1997) Wasting as an independent risk factor for mortality in chronic heart failure. Lancet 349:10501053 Levine B, Kalman J, Mayer L, Fillit HM, Packer M (1990) Elevated circulating levels of tumor necrosis factor in severe chronic heart failure. N Engl J Med 323:23641
Heart Fail Rev (2008) 13:3949 65. Krown KA, Page MT, Nguyen C, Zechner D, Gutierrez V, Comstock KL, Glembotski CC, Quintana PJ, Sabbadini RA (1996) Tumor necrosis factor alpha-induced apoptosis in cardiac myocytes Involvement of the sphingolipid signaling cascade in cardiac cell death. J Clin Invest 98:28542865 66. Tracey K, Morgello S, Koplin B, Fahey T, Fox K, Aledo A (1990) Metabolic effects of cachectin/tumor necrosis factor are modied by site of production: Cachectin/tumor necrosis factorsecreting tumor in skeletal muscle induces chronic cachexia, while implantation in brain induces predominantely acute cachexia. J Clin Invest 86:20142024 67. Torre-Amione G, Kapadia SR, Benedict C, Oral H, Young JB Mann DL (1996) Proinammatory cytokine levels in patients with depressed left ventricular ejection fraction: a report from the studies of left ventricular dysfunction (SOLVD). J Am Coll Cardiol 27:12011206 68. Pina IL, Apstein CS, Balady GJ, Belardinelli R, Chaitman BR, Duscha BD, Fletcher BJ, Fleg JL, Myers JN, Sullivan MJ (2003) Exercise and heart failure: a statement from the American heart association vommittee on exercise, rehabilitation, and prevention. Circulation 107:12101225 nig H, Funke E, Just H (1992) nzel T, Ko 69. Drexler H, Riede U, Mu Alterations of skeletal muscle in chronic heart failure. Circulation 85:17511759 70. Ennezat PV, Malendowicz SL, Testa M, Colombo PC, Cohen-Solal A, Evans T, LeJemtel TH (2001) Physical training in patients with chronic heart failure enhances the expression of genes antioxidative enzymes. J Am Coll Cardiol 38:194198 71. Adams V, Yu J, Mobius-Winkler S, Linke A, Weigl C, Hilbrich L, Schuler G, Hambrecht R (1997) Increased inducible nitric oxide synthase in skeletal muscle biopsies from patients with chronic heart failure. Biochem Mol Med 61:152160 72. McTiernan CF, Lemster BH, Frye C, Brooks S, Combes A, Feldman AM (1997) Interleukin-1-beta inhibits phospholamban gene expression in cultured cardiomyocytes. Circ Res 81:493503 73. Li N, Karin M (1999) Is NF-kB the senosr of oxidative stress? FASEB J 13:11371143 rstermann U, Drexler H (1998) Inducible nitric oxide 74. Riede U, Fo synthase in skeletal muscle of patients with chronic heart failure. J Am Coll Cardiol 32:964969 75. Anker SD, Chua TP, Ponikowski P, Harrington D, Swan JW, Kox WJ, Poole-Wilson PA, Coats AJ (1997) Hormonal changes and catabolic/anabolic imbalance in chronic heart failure and their importance for cardiac cachexia. Circulation 96:526534 76. Anker SD, Volterrani M, Paum CD, Strasburger CJ, Osterziel KJ, Doehner W, Ranke MB, Poole-Wilson PA, Giustina A, Dietz R, Coats AJ (2001) Acquired growth hormone resistance in patients with chronic heart failure: implications for therapy with growth hormone. J Am Coll Cardiol 38:443452 77. Resnicoff M, Burgaud J, Rotman H, Abraham D, Baserga R (1995) Correlation between apoptosis, tumorigenesis, and levels of insulin-factor I receptors. Cancer Res 55:37393741 78. Arteaga CL, Osborne CK (1989) Growth inhibition of human breast cancer cells in vitro with an antibody against the type I somatomedin receptor. Cancer Res 49:62376241 79. Prager D, Li H, Asa S, Melmed S (1994) Dominant negative inhibition of tumorgenesis in vivo by human insulin-like growth factor-I receptor mutant. Proc Natl Acad Sci 91:21812185 80. Olivetti G, Abbi R, Quaini F, Kajstura J, Cheng W, Nitahara J, Quaini E, Di Loreto C, Beltrami C, Krajewski S, Reed J, Anversa P (1997) Apoptosis in the failing human heart. N Engl J Med 336:11311141 81. Wu Y, Tewari M, Cui S, Rubin R (1996) Activation of the insulin-like growth factor-I receptor inhibits tumor necrosis factor-induced cell death. J Cell Physiol 168:499509
50.
51.
52.
53.
54.
55.
56.
57.
58.
59.
60.
61.
62.
63.
64.
123
Heart Fail Rev (2008) 13:3949 82. Sugiura T, Tashiro T, Yamamori H, Morishima Y, Otsubo Y, Hayashi N, Furukawa K, Nitta H, Nakajima N, Ishizuka T, Tatibana M, Ino H, Ito I (1997) Effects of insulin-like growth factor-1 on endotoxin translocation in burned rats receiving total parenteral nutrition. Nutrition 13:783787 83. Huang K, Chung D, Herndon D (1993) Insulinlike growth factor 1 (IGF-1) reduces gut atrophy and bacterial translocation after severe burn injury. Arch Surg 128:4753 84. Hornig B, Maier V, Drexler H (1996) Physical training improves endothelial function in patients with chronic heart failure. Circulation 93:210214 85. Gao L, Wang W, Dongmei L, Zucker IH (2007) Exercise training normalizes sympathetic outow by central antioxidant mechanisms in rabbits with pacing-induced chronic heart failure. Circulation 115:30953102 86. Zucker IH, Pliquett RU (2002) Novel mechanisms of sympathoexcitation in chronic heart failure. Heart Fail Monit 3:27 87. Fukai T, Siegfried MR, Ushio-Fukai M, Cheng Y, Kojda G, Harrison DG (2000) Regulation of the vascular extracellular superoxide dismutase by nitric oxide and exercise training. J Clin Invest 105:16311639 88. Niebauer J, Dulak J, Chan JR, Tsao PS, Cooke JP (1999) Gene transfer of nitric oxide synthase: effects on endothelial biology. J Am Coll Cardiol 34:12011207 89. Niebauer J, Cooke JP (1996) Cardiovascular effects of exercise: role of endothelial shear stress. J Am Coll Cardiol 28:16521660 90. Niebauer J, Maxwell AJ, Lin PS, Tsao PS, Kosek J, Bernstein D, Cooke JP (1999) Impaired aerobic capacity in hypercholesterolemic mice: partial reversal by exercise training. Am J Physiol 276:H1346H1354
49 91. Niebauer J, Maxwell AJ, Lin PS, Wang D, Tsao PS, Cooke JP (2003) NOS inhibition accelerates atherogenesis: Reversal by exercise. Am J Physiol 91:148153 92. Haywood GA, Tsao PS, von der Leyen HE, Mann MJ, Keeling PJ, Trindade PT, Lewis NP, Byrne CD, Rickenbacher PR, Bishopric NH, Cooke JP, McKenna WJ, Fowler MB (1996) Expression of inducible nitric oxide synthase in human heart failure. Circulation 93:10871094 93. Wisloff U, Stoylen A, Loennechen JP, Bruvold M, Rognmo O, Haram PM, Tjonna AE, Helgerud J, Slordahl SA, Lee SJ, Videm V, Bye A, Smith GL, Njjar SM, Ellingsen L, Skjaerpe T (2007) Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation 115:30863094 94. Ferrari R, Ceconi C, Curello S, Guarnieri C, Caldarera CM, Albertini A, Visioli O (1985) Oxygen-mediated myocardial damage during ischaemia and reperfusion: role of the cellular defences against oxygen toxicity. J Mol Cell Cardiol 17:937945 95. Parks DA, Granger DN (1986) Xanthine oxidase: biochemistry, distribution and physiology. Acta Physiol Scand Suppl 548:8799 96. Xia Y, Zweier JL (1995) Substrate control of free radical generation from xanthine oxidase in the post ischemic heart. J Biol Chem 270:1879718803 97. Ketai LH, Simon RH, Kreit JW, Grum CM (1987) Plasma hypoxanthine and exercise. Am Rev Respir Dis 136:98101 98. Fox IH, Palella TD, Kelley WN (1987) Hyperuricemia: a marker for cell energy crisis. N Engl J Med 317:111112
123
You might also like
- Progressive Resistance Training in Breast Cancer - A SystematicDocument18 pagesProgressive Resistance Training in Breast Cancer - A SystematicMatheus BarbosaNo ratings yet
- The Effects of An IndividualizedDocument7 pagesThe Effects of An IndividualizedMatheus BarbosaNo ratings yet
- Resistance Exercise in Men Receiving Androgen DeprivationDocument7 pagesResistance Exercise in Men Receiving Androgen DeprivationMatheus BarbosaNo ratings yet
- The Anti-Inflammatory Effect of ExerciseDocument10 pagesThe Anti-Inflammatory Effect of ExerciseMatheus BarbosaNo ratings yet
- Resistance Exercise and SupraphysiologicDocument10 pagesResistance Exercise and SupraphysiologicMatheus BarbosaNo ratings yet
- The Benefits of Exercise Training For Quality of Life in HIVDocument13 pagesThe Benefits of Exercise Training For Quality of Life in HIVMatheus BarbosaNo ratings yet
- Immune Response To A 30-Minute WalkDocument7 pagesImmune Response To A 30-Minute WalkMatheus BarbosaNo ratings yet
- Percentis Bmi 2-20 CDC FemDocument1 pagePercentis Bmi 2-20 CDC FemMatheus BarbosaNo ratings yet
- Physical Activity and Hormonal Regulation of Appetite Sex Differences and Weight ControlDocument6 pagesPhysical Activity and Hormonal Regulation of Appetite Sex Differences and Weight ControlMatheus BarbosaNo ratings yet
- Kinetics of Lactate Metabolism After Submaximal ErgometricDocument6 pagesKinetics of Lactate Metabolism After Submaximal ErgometricMatheus BarbosaNo ratings yet
- Lymphocyte and Cytokines After Short Periods of ExerciseDocument5 pagesLymphocyte and Cytokines After Short Periods of ExerciseMatheus BarbosaNo ratings yet
- Effects of A Supervised Home-Based Aerobic andDocument7 pagesEffects of A Supervised Home-Based Aerobic andMatheus BarbosaNo ratings yet
- Bmi For Age, Boys 2-20 YoDocument1 pageBmi For Age, Boys 2-20 YoLeny Karlina HakimNo ratings yet
- Implications of Chronic Heart Failure On Peripheral Vasculature and Skeletal Muscle Before and After Exercise TrainingDocument17 pagesImplications of Chronic Heart Failure On Peripheral Vasculature and Skeletal Muscle Before and After Exercise TrainingMatheus BarbosaNo ratings yet
- Effects of High-Intensity Endurance and Resistance Exercise On HIV Metabolic AbnormalitiesDocument10 pagesEffects of High-Intensity Endurance and Resistance Exercise On HIV Metabolic AbnormalitiesMatheus BarbosaNo ratings yet
- Exercise Training in HIV-1-InfectedDocument8 pagesExercise Training in HIV-1-InfectedMatheus BarbosaNo ratings yet
- Hodgkin's Lymphorna in An Elite Endurance AthleteDocument5 pagesHodgkin's Lymphorna in An Elite Endurance AthleteMatheus BarbosaNo ratings yet
- Effects of Testosterone and Progressive Resistance Training inDocument8 pagesEffects of Testosterone and Progressive Resistance Training inMatheus BarbosaNo ratings yet
- Effects of Exercise Training and Metformin On Body.13Document9 pagesEffects of Exercise Training and Metformin On Body.13Matheus BarbosaNo ratings yet
- Evidence For Prescribing Exercise As Therapy in Chronic DiseaseDocument61 pagesEvidence For Prescribing Exercise As Therapy in Chronic DiseaseMatheus BarbosaNo ratings yet
- Effects of Detraining On The Functional CapacityDocument8 pagesEffects of Detraining On The Functional CapacityMatheus BarbosaNo ratings yet
- Effects of An Intrahospital Exercise Program Intervention For Children With LeukemiaDocument10 pagesEffects of An Intrahospital Exercise Program Intervention For Children With LeukemiaMatheus BarbosaNo ratings yet
- Effects of Pharmacological Doses of NandroloneDocument10 pagesEffects of Pharmacological Doses of NandroloneMatheus BarbosaNo ratings yet
- Exercise and The Nitric Oxide Vasodilator SystemDocument23 pagesExercise and The Nitric Oxide Vasodilator SystemMatheus BarbosaNo ratings yet
- Effectiveness of Aerobic Exercise in AdultsDocument9 pagesEffectiveness of Aerobic Exercise in AdultsMatheus BarbosaNo ratings yet
- Dynamics of Fat Cell Turnover in HumansDocument5 pagesDynamics of Fat Cell Turnover in HumansMatheus BarbosaNo ratings yet
- Deleterious Effects of Short-Term, High-IntensityDocument6 pagesDeleterious Effects of Short-Term, High-IntensityMatheus BarbosaNo ratings yet
- Beta-Blockers, Exercise, and The Immune System in Men With Coronary Artery DiseaseDocument6 pagesBeta-Blockers, Exercise, and The Immune System in Men With Coronary Artery DiseaseMatheus BarbosaNo ratings yet
- Cortisol - Essential Adaptation Hormone in ExerciseDocument4 pagesCortisol - Essential Adaptation Hormone in ExerciseMatheus BarbosaNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Konsep Filosofi, Konsep Holistik GadarDocument30 pagesKonsep Filosofi, Konsep Holistik GadarWinda GanggurNo ratings yet
- Rizal's Visit To The United States (1888Document23 pagesRizal's Visit To The United States (1888Dandy Lastimosa Velasquez57% (7)
- Health Economics: Which of The Following Is Not A Reason For Increased Health Spending?Document8 pagesHealth Economics: Which of The Following Is Not A Reason For Increased Health Spending?Arjun Aryal100% (1)
- 20190305190022636Document94 pages20190305190022636Subhi MohamadNo ratings yet
- Genny Suwandi - DVIDocument18 pagesGenny Suwandi - DVIgennysuwandiNo ratings yet
- Defluoridation of Ground WaterDocument12 pagesDefluoridation of Ground WaterNikitha PerumallaNo ratings yet
- Employees' State Insurance Corporation E-Pehchan Card: Insured Person: Insurance No.: Date of RegistrationDocument3 pagesEmployees' State Insurance Corporation E-Pehchan Card: Insured Person: Insurance No.: Date of RegistrationSaikatNo ratings yet
- PLLDocument24 pagesPLLjagannnathdNo ratings yet
- Tuskegee ExperimentDocument2 pagesTuskegee ExperimentAniya LewisNo ratings yet
- Liquidation Report: To Liquidate The MOOE Cash Advanced Made by Kibao Elementary School Per Check # 298152dated 9/16/16Document3 pagesLiquidation Report: To Liquidate The MOOE Cash Advanced Made by Kibao Elementary School Per Check # 298152dated 9/16/16December Cool50% (2)
- Cancer-Relatedfatiguein Cancersurvivorship: Chidinma C. Ebede,, Yongchang Jang,, Carmen P. EscalanteDocument13 pagesCancer-Relatedfatiguein Cancersurvivorship: Chidinma C. Ebede,, Yongchang Jang,, Carmen P. EscalanteMahdhun ShiddiqNo ratings yet
- Intracranial Pressure: Current Perspectives On Physiology and MonitoringDocument11 pagesIntracranial Pressure: Current Perspectives On Physiology and MonitoringWander ValentimNo ratings yet
- ADHERENCE and INVASION ASSAYS A092Document2 pagesADHERENCE and INVASION ASSAYS A092Samrah Anwar0% (2)
- The Intentional Application of Humor With CKD PatientsDocument8 pagesThe Intentional Application of Humor With CKD PatientsKaryn BuxmanNo ratings yet
- Malaysia School ImmunizationDocument41 pagesMalaysia School ImmunizationKalai ArikaranNo ratings yet
- Water Pollution Is The Contamination ofDocument36 pagesWater Pollution Is The Contamination ofsuradotNo ratings yet
- Seafarer Medical CertificateDocument2 pagesSeafarer Medical CertificateKoki ToNo ratings yet
- Ambroxol PDFDocument2 pagesAmbroxol PDFmina zayNo ratings yet
- CPT CODING Power PointDocument24 pagesCPT CODING Power PointJack100% (1)
- Bulletin 201215 (HTML Edition)Document128 pagesBulletin 201215 (HTML Edition)DonnieNo ratings yet
- Details Received From Collectorate - Excellent Dedicated Work - During Pandemic COVID - 19Document2 pagesDetails Received From Collectorate - Excellent Dedicated Work - During Pandemic COVID - 19Vimal kumarNo ratings yet
- Centaur CortisolDocument12 pagesCentaur CortisolMohamed AliNo ratings yet
- Microbiome Labs Total Gut RestorationDocument2 pagesMicrobiome Labs Total Gut RestorationKrishna DasNo ratings yet
- Medicine List With DosageDocument9 pagesMedicine List With DosageonovNo ratings yet
- Altitude Diving PhysiologyDocument12 pagesAltitude Diving PhysiologyKarin Gandeswari100% (1)
- Basic Maternity ConceptsDocument14 pagesBasic Maternity ConceptsDivine Grace Arreglo AbingNo ratings yet
- Cannistra 2007Document4 pagesCannistra 2007amdreyNo ratings yet
- Mh25 Borderline Personality GuidelineDocument182 pagesMh25 Borderline Personality GuidelineAbdul Hakim Abdul KadirNo ratings yet
- Ansdell G Elefant C. Pavlicevic M. Stige B. (2010) - Where Music Helps CommunityDocument4 pagesAnsdell G Elefant C. Pavlicevic M. Stige B. (2010) - Where Music Helps CommunityNati de la BarraNo ratings yet
- 1111 - USP Micro Limit Test For Non SterileDocument2 pages1111 - USP Micro Limit Test For Non SterileSpectre SpectreNo ratings yet