Professional Documents
Culture Documents
1 Jihvaagat Rog
Uploaded by
Knr GannuCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
1 Jihvaagat Rog
Uploaded by
Knr GannuCopyright:
Available Formats
Vaataj
Chapped lips or Cracked lips is a condition whereby the lips become dry and possibly cracked. It may be caused by the evaporation of moisture. Often the lips become dry because the layer of oil that is naturally produced by the body to coat the lips is removed or is lacking. Causes vary, but the most common cause of chapped lips is due to cold weather conditions. Symptoms Symptoms of chapped lips may include the lips being dry, burning, red and swollen, small cracks, and peeling of the skin on the lips. If the skin on chapped lips becomes extremely dry, stretching of the lips may cause large cracks, which may be painful and/or bleed. Cause
Chapped lips
The main cause of this problem is the absence of moisture from the lips, which can make them dry out very quickly, leaving them chapped. This happens often in the winter season when the air is dry. Lips normally have a very thin oily film on their surface that provides natural protection against moisture loss. However, in some cases, this film is removed, sometimes due to excessive licking habits, and this causes the lips to become chapped Treatments Adequate hydration is the first line of defense against chapped lips. Lip balm can provide temporary relief. It is often believed that petroleum jelly can heal chapped lips; however, it only aids in preventing moisture loss, but does not repair or penetrate the lips. Medical grade (USP) lanolin accelerates repair of lips [2] and is used in some lip repair products. Certain enzymes present in saliva (normally used for digestion) irritate the lips, and the evaporation of the water in saliva saps moisture from them. [3] For these reasons, licking one's lips should be avoided. Nasal sebum may also be used as a remedy.[4] Paitik
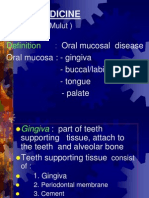
An aphthous ulcer (pron.: /fs/ AF-ths), also known as a canker sore, is a type of mouth ulcer that presents as a painful open sore inside the mouth[1] or upper throat characterized by a break in the mucous membrane. Its cause is unknown, but they are not contagious. [2] The condition is also known as aphthous stomatitis (stomatitis is inflammation of the mucous lining), and alternatively as Sutton's Disease, especially in the case of major, multiple, or recurring ulcers.[3] The term aphtha means ulcer; it has been used for many years to describe areas of ulceration on mucous membranes Recurrent aphthous stomatitis (RAS) can be distinguished from other diseases with similar-appearing oral lesions, such as certain oral bacteria or herpes simplex, by their tendency to recur, and their multiplicity and chronicity. Recurrent aphthous stomatitis is one of the most common oral conditions. At least 10% of the population has it, and women are more often affected than men. About 3040% of patients with recurrent aphthae report a family history Classification(wiki) Minor ulceration Minor aphthous ulcers indicate that the lesion size is between 310 mm (0.10.4 in). They are most common aphthous ulcers. The appearance of the lesion is that of an erythematous halo with yellowish or grayish color+pain Major ulcerations Major aphthous ulcers have the same appearance as minor ulcerations, but are greater than 10 mm in diameter and are painful. They usually take more than a month to heal, and frequently leave a scar. These typically develop after puberty with frequent recurrences Herpetiform ulcerations This is the most severe form. It occurs more frequently in females, and onset is often in adulthood. It is characterized by small, numerous, 13 mm lesions that form clusters. They typically heal in less than a month without scarring
Signs and symptoms Most commonly aphthous ulcers are seen on the lining of cheeks, tongue, lips and roof of mouth. Aphthous ulcers usually begin with a tingling or burning sensation at the site of the future aphthous ulcer. In a few days, they often progress to form a red spot or bump, followed by an open ulcer. The aphthous ulcer appears as a white or yellow oval with an inflamed red border. Sometimes a white circle or halo around the lesion can be observed. The gray, white, or yellow area within the red boundary is due to the formation of layers of fibrin, a protein involved in the clotting of blood. The ulcer, which itself is often painful, especially when agitated, may be accompanied by a painful swelling of the lymph nodes below the jaw; another symptom is fever. A sore on the gums may be accompanied by discomfort or pain in the teeth. Canker sores are very sensitive to spicy foods, and, if secondary infection occurs in canker sores, then antibiotics may also be required to treat it. Prevention Oral measures Regular use of non-alcoholic mouthwash may help prevent or reduce the frequency of sores. Informal studies suggest that mouthwash may help to temporarily relieve pain. [28] A study from 2011 found that using mouthwash containing Rosa damascena extract was more effective than the placebo in the treatment of recurrent aphthous stomatitis. [29] In some cases, aphthous ulcers may be minimized by avoiding toothpastes containing sodium dodecyl sulfate (sometimes called sodium lauryl sulfate, or with the acronyms SLS or SDS), a detergent found in most toothpastes. Using toothpaste free of this compound has been found in several studies to help reduce the amount, size, and recurrence of ulcers.[30][31][32] Dental braces are a common physical trauma that can lead to aphthous ulcers and the dental bracket can be covered with wax to reduce abrasion of the mucosa. Avoidance of other types of physical and chemical trauma will prevent some ulcers, but, since such trauma is usually accidental, this type of prevention is not usually practical. Nutrition Zinc deficiency has been reported in people with recurrent aphthous ulcers. [33] The few small studies looking into the role of zinc supplementation have reported mostly positive results, in particular for those people with zinc deficiency, [34] although some research has found no therapeutic effect. [35] Treatment A number of treatments for apthous ulcers exist, including analgesics, anesthetics agents, antiseptics, anti-inflammatory agents, steroids, sucralfate, tetracycline suspension, Debacterol, and silver nitrate.[36]. Suggestions to reduce the pain caused by an ulcer include avoiding spicy food, rinsing with salt water or over-the-counter mouthwashes, proper oral hygiene, and non-prescription local anesthetics. Active ingredients in the latter generally include benzocaine,[37] benzydamine or choline salicylate,[38] and phenol.[39] Anesthetic mouthwashes containing benzydamine hydrochloride have not been shown to reduce the number of new ulcers or significantly reduce pain,[40] and evidence supporting the use of other topical anesthetics is very limited, though some individuals may find them effective.[41] In general, their role is limited; their duration of effectiveness is, in general, short and does not provide pain control throughout the day. Such medications may cause complications in children.[42] Evidence is limited for the use of antimicrobial mouthwashes but suggests that they may reduce the painfulness and duration of ulcers and increase the number of days between ulcerations, without reducing the number of new ulcers. [43] Corticosteroid preparations containing hydrocortisone hemisuccinate or triamcinolone acetonide to control symptoms are effective in treating aphthous ulcers (Triamcinolone Acetonide was used in the product 'Adcortyl in Orabase' which was well known amongst ulcer sufferers but discontinued in the UK during 2009). [41][44][45] The application of silver nitrate will cauterize the sore; a single treatment decreases pain but does not affect healing time[46] though in children it can cause tooth discoloration if the teeth are still developing.[47] The use of tetracycline is controversial, as is treatment with levamisole, colchicine, gamma-globulin, dapsone, estrogen replacement and monoamine oxidase inhibitors.[37] While commonly used, magic mouthwash, a combination of a number of ingredients including viscous lidocaine, benzocaine, milk of magnesia, kaolin-pectate, chlorhexidine, or diphenhydramine, has little evidence to support its use
Paitik and shleshmaj
Herpes labialis, or orolabial herpes,[1]:368 is an infection of the lip by herpes simplex virus (HSV-1). An outbreak typically causes small painful blisters or sores on or around the mouth commonly known as cold sores or fever blisters. The sores typically heal within 23 weeks, but the herpes virus remains dormant in the facial nerves, following orofacial infection, periodically reactivating (in symptomatic people) to create sores in the same area of the mouth or face at the site of the original infection. The virus is transmitted from cold sores and also when there are no symptoms, as it can make copies of itself on the skin in the absence of a blister Symptoms Herpes infections usually show no symptoms; [6] when symptoms do appear they typically resolve within two weeks.[7] The main symptom of oral infection is inflammation of the mucosa of the cheek and gumsknown as acute herpetic gingivostomatitiswhich occurs within 510 days of infection. Other symptoms may also develop, including headache, nausea, dizziness and painful ulcerssometimes confused with canker soresfever, and sore throat. The first episode may be mild or severe. It usually occurs in children between 1 and 5 years old. First symptoms usually appear within 1 or 2 weeks, and as long as 3 weeks, after contact with the virus. Sore throat and fever that can last up to 5 days may occur before the blisters appear. There may also be swollen glands in the neck. First episode may last 2 to 3 weeks. The lesions may be on the gums, in the mouth and throat, or on the face. It may hurt to swallow. Later episodes are usually milder. May be triggered by menstruation, sun exposure, fever, stress, or various other unknown causes. Warning symptoms of itching, burning, increased sensitivity, or tingling sensation may occur about 2 days before lesions appear. An outbreak usually involves: Skin lesions or rash around the lips, mouth, and gums Small blisters (vesicles) filled with clear yellowish fluid o Blisters on a raised, red, painful skin area o Blisters that form, break, and ooze o Yellow crusts that slough to reveal pink, healing skin o Several smaller blisters that merge to form a larger blister Exams and Tests Diagnosis is made on the basis of the appearance or culture of the lesion. Examination may also show enlargement of lymph nodes in the neck or groin. Viral culture, viral DNA test, or Tzanck test of the skin lesion may reveal the herpes simplex virus. Treatment Untreated, the symptoms will generally go away in 1 to 2 weeks. Antiviral medications taken by mouth may help the symptoms go away sooner and decrease pain. Acyclovir, famciclovir, and valacyclovir are the three oral treatments currently available. Herpes sores often come back again and again. The antiviral medicines work best if you take them when the virus is just starting to come back -- before you see any sores. If the virus returns frequently, your doctor may recommend that you take the medicines all the time. Topical (rubbed onto the skin) antiviral cream (penciclovir andaacyclovir) may be used, but must be applied every 2 hours while you're awake. They are expensive and often only shorten the outbreak by a few hours to a day. Wash blisters gently with soap and water to reduce the spread of the virus to other areas of skin. An antiseptic soap may be recommended. Applying ice or warmth to the area may reduce pain.
Tips to prevent future outbreaks include applying a sunblock or lip balm containing zinc oxide to the lips when you're outdoors. A moisturizing balm to prevent the lips from becoming too dry may also help. Docosanol, a saturated fatty alcohol, is a safe and effective topical application that has been approved by the United States Food and Drug Administration for herpes labialis in adults with properly functioning immune systems. It is comparable in effectiveness to prescription topical antiviral agents. Due to its mechanism of action, there is little risk of drug resistance. [11] The duration of symptoms can be reduced by a small amount if an antiviral, anaesthetic or non-treatment cream (such as zinc oxide or zinc sulfate) is applied promptly.[12] Effective antiviral medications include acyclovir[13] and penciclovir, which can speed healing by as much as 10%.[14] Famciclovir or valaciclovir, taken in pill form, can be effective using a single day, high-dose application and is more cost effective and convenient than the traditional treatment of lower doses for 57 days. [15] Lysine has been suggested as a treatment for herpes labialis based on in vitro studies, but the evidence is inconclusive in humans Prevention Avoid direct contact with herpes sores. Minimize the risk of indirect spread by thoroughly washing items such as towels in hot (preferably boiling) water before reuse. Do not share items with an infected person, especially when they have herpes lesions. Avoid triggers (especially sun exposure) if you are prone to oral herpes. Avoid performing oral sex when you have active herpes lesions on or near your mouth and avoid receiving oral sex from someone who has oral or genital herpes lesions. Condoms can help reduce, but do not entirely eliminate, the risk of catching herpes from oral or genital sex with an infected person. Both oral and genital herpes viruses can sometimes be transmitted even when the person does not have active lesions.
Sannipatik
Lip cancer is a malignancy, occurring due to an autonomous and uncontrolled multiplication of cells in the lips. Lip cancer is a comparatively rare form of malignancy, and a greater part of the cases of lip cancer are due to squamous cell carcinoma. Lip Cancer Symptoms The following are the commonest lip cancer symptoms: Initial stages of lip cancer may be asymptomatic, i.e. there, may not be any clinical manifestations at all. Over a period of time, a sore or a lesion develops. Importantly, it fails to heal; and bleeds easily. There may be a thickening or a lump on the lips. Ulcer An ulcer or a sore on the lip that does not heal is the first symptom of a lip cancer. Nine out of 10 cancers are seen on the lower lip. It usually appears as a non-healing ulcer at the junction of middle and outer third of the lower lip, according to the American Oral Cancer Clinic. According to Merck's Manual, this cancer often feels rock hard and is attached to the underlying tissues. Lump on the Lip Lip cancer is often seen as a lump or thickening on the lips, according to the National Cancer Institute. Your lip will appear thickened and swollen. Pain and Bleeding With a cancer of the lip, you may have pain that makes it difficult to eat food. Pain can also occur in the lymph node of the affected part of the lip. This indicates that the cancer has spread beyond the lip to the lymph nodes, according to American Cancer Society. Additionally, an ulcer on the lip bleeds easily and can cause your lip to bleed. Numbness Loss of sensation in the lip indicates the cancer has spread and erodes the nerves, according to Baylor College of Medicine experts. When the cancer has spread to the nerves or compresses on the nerves, your lips will feel numb. Swollen Neck Glands The cancer can spread beyond the lip to the lymph glands of the neck. Your doctor will find swollen lymph nodes when he examines your neck. Consult your doctor if the above symptoms occur. Risk factors for Lip Cancer
Individuals who consume excessive alcohol and those who smoke a lot are at grave risk. Chewing tobacco is also an important risk factor for lip cancer. Sun exposure increases the risk for lip cancer as well.Another major risk factor is HPV infection. Diagnosing the Lip Cancer Symptoms A detailed physical examination of the lips and mouth helps determine the exact cause. The lymph nodes in the neck are also examined for swelling. A biopsy needs to be done to find out the exact condition and type of malignancy. Occasionally, lip cancer symptoms tend to go unnoticed, for the reason that they are similar to symptoms of other conditions. Besides, infrequently, some people do not demonstrate any symptoms during the initial stages. Hence, it is very crucial that you have regular physical and dental check ups, follow good dental hygiene, steer clear of the risk factors and prevent HPV infection through safe sex practices. Lip Cancer Symptoms Treatment Treatment for lip cancer depends on when the diagnosis is made, the type of cancer, the stage of the disease, the degree of spread, patient's age and his overall health status. The condition is most treatable if diagnosed in the early stages. A special health care team is required in order to manage lip cancer; it comprises of: medical oncologists, dentists, radiation oncologists, and registered nurses specializing in cancer care. Together, these experts help mange the case effectively. Surgical intervention: excision of the tumor mass from the lip is done. Also, during the excision, some amount of surrounding healthy tissue, and adjacent lymph nodes and other tissues are removed to avert recurrences and spread. Radiation therapy: is necessary to destroy all the cancer cells. Chemotherapy: The treatment regimen integrates chemotherapy drugs as well. For people in whom the cancer has progressed to an advanced stage and the condition is terminal, the intention of the treatment changes. Management of these cases modifies from treating to concentrating up on means to diminish the intensity of symptoms, alleviate / palliate the pain and make the patient comfortable. Treatment may need to be given via a hospice program.
Raktaj
Erythema multiformeErythema multiforme is a skin disorder due to an allergic reaction or infection. Causes Erythema multiforme is a type of hypsersensitivity reaction that occurs in response to medications, infections, or illness. Medications include: Barbiturates Penicillins Phenytoin Sulfonamides Infections include: Herpes simplex Mycoplasma The exact cause is unknown. The disorder is believed to involve damage to the blood vessels of the skin, followed by damage to skin tissues. Some forms of this condition are more severe than others. Erythema multiforme minor is not very serious. Most erythema multiforme is caused by herpes simplex or mycoplasma infections. Erythema multiforme major is more severe, and is known as Stevens-Johnson syndrome. The more severe form is usually caused by reactions to medications, rather than infections. Erythema multiforme occurs primarily in children and young adults.
Symptoms Fever, General ill feeling, Itching of the skin, Joint aches Multiple skin lesions: o Start quickly and may return o May spread o May appear as a nodule, papule, or macule and may look like hives o Central sore surrounded by pale red rings, also called a "target", "iris", or "bulls-eye" o May have vesicles and blisters of various sizes (bullae) o Located on the upper body, legs, arms, palms, hands, or feet o May involve the face or lips o Usually even on both sides (symmetrical) Other symptoms that may occur with this disease: Bloodshot eyes, Dry eyes, Eye burning, itching, and discharge, Eye pain, Mouth sores, Vision problems Exams and Tests The diagnosis is based mainly on the appearance of the skin lesion, especially if there is a history of risk factors or related diseases. Tests may include: Nikolsky's sign Skin lesion biopsy and microscopic examination of the tissue Treatment Treatment goals include: Controlling the illness that is causing the condition Preventing infection Treating the symptoms Stop taking any suspected medications, with your doctor's approval. Treatment of mild symptoms may include: Medications such as antihistamines to control itching Moist compresses applied to the skin Oral antiviral medication if it is caused by herpes simplex Over-the-counter medications (such as acetaminophen) to reduce fever and discomfort Topical anesthetics (especially for mouth lesions) to ease discomfort that interferes with eating and drinking Treatment of severe symptoms may include: Antibiotics to control any skin infections Corticosteroids to control inflammation Hospitalization and treatment in an intensive care or burn care unit for severe cases, Stevens-Johnson syndrome, and toxic epidermal necrolysis Intravenous immunoglobulins (IVIG) to stop the disease process Practicing good hygiene and staying away from other people may help prevent secondary infections. Skin grafting may be helpful in cases in which large areas of the body are affected. Outlook (Prognosis) Mild forms of erythema multiforme usually get better in 2 - 6 weeks, but they may return. More severe forms may be difficult to treat. Stevens-Johnson syndrome and toxic epidermal necrolysis have high death rates.
Mansaj
Epithelioma of lips i.e. cancer Epithelioma is an abnormal growth of the epithelium, which is the layer of tissue that covers the surfaces of organs and other structures of the body. Epitheliomas can be benign growths or malignant carcinomas. They are classified according to the specific type of epithelial cells that are affected.
The most common epitheliomas are basal cell carcinoma and squamous cell carcinoma (skin cancers). Treatment usually involves surgically removing the tumor and affected tissue. #Epithelioma of the lip# is of the squamous-celled variety, and is met with either as a fungating wart-like projection, or as an indurated ulcer. It almost exclusively occurs on the lower lip of men over forty years of age. The growth begins about midway between the middle line and the angle of the mouth, either as a horny epidermal thickening, or as a warty excrescence, which bleeds readily and soon ulcerates. The affection is said to be especially common in those who smoke short clay pipes, and it is a suggestive fact that, while epithelioma of the lip is rare in women, the majority of those who do suffer are smokers. The ulceration spreads along the lip, chiefly towards the angle of the mouth, and downwards towards the chin, and the substance of the lip becomes swollen and indurated (Figs. 242, 243). The edges are characteristically raised and hard, and the raw surface is extremely painful, especially when irritated by hot food or fluids. The growth is liable to spread to the mucous membrane and gum, and to invade the mandible. The disease spreads early to the submental and submaxillary glands, which are best felt with one finger inside the mouth, under the tongue, and another outside, behind the mandible. The infected glands tend to become fixed to the bone, and while at first extremely hard, so much so that they simulate a bony tumour of the jaw, they later soften, liquefy, and fungate Metastasis to internal organs is rare. Unless removed by operation, the disease usually proves fatal in from three to three and a half years. The _treatment_ consists in removing a wedge-shaped portion of the swelling on the same lines as for "strumous lip," or in employing electrolysis. _Mucous cysts_ occur as small rounded tumours, projecting from the inner surface of the lip. They are of a bluish colour, and contain a glairy fluid. They are treated by removal of the cyst wall, together with the overlying portion of mucous membrane. The _treatment_ consists in early and free removal of the affected portion of lip and of all the lymphatic connections in the submaxillary region and neck. Recurrence in the scar is rare; it is nearly always located in the glands. The operation of cleaning out the glands below the mandible on both sides in men who are advanced in years is not free from risk to life, especially from respiratory complications which may or may not be traceable to the anaesthetic. In inoperable cases benefit may follow the use of the X-rays, or of radium. _Epithelioma of the upper lip_ is less common. It occurs with equal frequency in the two sexes, progresses more slowly, and is, on the whole, less malignant. It sometimes appears to be due to contact infection from the lower lip. It is treated on the same lines as cancer of the lower lip. http://www.freefictionbooks.org/books/m/11393-manual-of-surgery-volume-second-extremities%E2%80%94hea? start=278
Medoj Leukoplakia are patches on the tongue, in the mouth, or on the inside of the cheek that occur in response to long-term irritation a condition where patches of keratosis appear as adherent white patches on the mucous membranes of the oral cavity Macrocheilia[1] is a condition of permanent swelling of the lip that results from greatly distended lymphatic spaces. This causes an abnormal largeness of the lips. This is sometimes seen in leprosy patients Abhighaataj Cleft lip and cleft palate are facial and oral malformations that occur very early in pregnancy, while the baby is developing inside the mother. Clefting results when there is not enough tissue in the mouth or lip area, and the tissue that is available does not join together properly. A cleft lip is a physical split or separation of the two sides of the upper lip and appears as a narrow opening or gap in the skin of the upper lip. This separation often extends beyond the base of the nose and includes the bones of the upper jaw and/or upper gum.
A cleft palate is a split or opening in the roof of the mouth. A cleft palate can involve the hard palate (the bony front portion of the roof of the mouth), and/or the soft palate (the soft back portion of the roof of the mouth). Cleft lip and cleft palate can occur on one or both sides of the mouth. Because the lip and the palate develop separately, it is possible to have a cleft lip without a cleft palate, a cleft palate without a cleft lip, or both together.
Cleft lip (cheiloschisis) and cleft palate (palatoschisis), which can also occur together as cleft lip and palate, are variations of a type of clefting congenital deformity caused by abnormal facial development during gestation. A cleft is a fissure or openinga gap. It is the non-fusion of the body's natural structures that form before birth. Approximately 1 in 700 children born have a cleft lip and/or a cleft palate.
Signs and symptoms
Cleft lip and palate If the cleft does not affect the palate structure of the mouth it is referred to as cleft lip. Cleft lip is formed in the top of the lip as either a small gap or an indentation in the lip (partial or incomplete cleft) or it continues into the nose (complete cleft). Lip cleft can occur as a one sided (unilateral) or two sided (bilateral). It is due to the failure of fusion of the maxillary and medial nasal processes (formation of the primary palate).
Unilateral incomplete
Unilateral complete
Bilateral complete
A mild form of a cleft lip is a microform cleft.[2] A microform cleft can appear as small as a little dent in the red part of the lip or look like a scar from the lip up to the nostril.[3] In some cases muscle tissue in the lip underneath the scar is affected and might require reconstructive surgery.[4] It is advised to have newborn infants with a microform cleft checked with a craniofacial team as soon as possible to determine the severity of the cleft.[5]
6 month old girl before going into surgery to have her unilateral complete cleft lip repaired.
The same girl, 1 month after the surgery.
Same girl, age 8. Note how the scar is almost gone. Cleft palate Cleft palate is a condition in which the two plates of the skull that form the hard palate (roof of the mouth) are not completely joined. The soft palate is in these cases cleft as well. In most cases, cleft lip is also present. Cleft palate occurs in about one in 700 live births worldwide.[6] Palate cleft can occur as complete (soft and hard palate, possibly including a gap in the jaw) or incomplete (a 'hole' in the roof of the mouth, usually as a cleft soft palate). When cleft palate occurs, the uvula is usually split. It occurs due to the failure of fusion of the lateral palatine processes, the nasal septum, and/or the median palatine processes (formation of the secondary palate). The hole in the roof of the mouth caused by a cleft connects the mouth directly to the nasal cavity. Note: the next images show the roof of the mouth. The top shows the nose, the lips are colored pink. For clarity the images depict a toothless infant.
Incomplete cleft palate
Unilateral complete lip and palate
Bilateral complete lip and palate A result of an open connection between the oral cavity and nasal cavity is called velopharyngeal inadequacy (VPI). Because of the gap, air leaks into the nasal cavity resulting in a hypernasal voice resonance and nasal emissions while talking.[7] Secondary effects of VPI include speech articulation errors (e.g., distortions, substitutions, and omissions) and compensatory misarticulations and mispronunciations (e.g., glottal stops and posterior nasal fricatives).[8] Possible treatment options include speech therapy, prosthetics, augmentation of the posterior pharyngeal wall, lengthening of the palate, and surgical procedures.[7] Submucous cleft palate (SMCP) can also occur, which is a cleft of the soft palate with a classic clinical triad of a bifid, or split, uvula which is found dangling in the back of the throat, a furrow along the midline of the soft palate, and a notch in the back margin of the hard palate.[9]
What Causes a Cleft Lip and Cleft Palate? In most cases, the cause of cleft lip and cleft palate is unknown. These conditions cannot be prevented. Most scientists believe clefts are due to a combination of genetic and environmental factors. There appears to be a greater chance of clefting in a newborn if a sibling, parent, or relative has had the problem. Another potential cause may be related to a medication a mother may have taken during her pregnancy. Some drugs may cause cleft lip and cleft palate. Among them: anti-seizure/anticonvulsant drugs, acne drugs containing Accutane, and methotrexate, a drug commonly used for treating cancer, arthritis, and psoriasis.
Cleft lip and cleft palate may also occur as a result of exposure to viruses or chemicals while the fetus is developing in the womb. In other situations, cleft lip and cleft palate may be part of another medical condition. How Are Cleft Lip and Cleft Palate Diagnosed? Because clefting causes very obvious physical changes, a cleft lip or cleft palate is easy to diagnose. Prenatal ultrasound can sometimes determine if a cleft exists in an unborn child. If the clefting has not been detected in an ultrasound prior to the baby's birth, a physical exam of the mouth, nose, and palate confirms the presence of cleft lip or cleft palate after a child's birth. Sometimes diagnostic testing may be conducted to determine or rule out the presence of other abnormalities. What Problems Are Associated With Cleft Lip and/or Palate?
Eating problems. With a separation or opening in the palate, food and liquids can pass from the mouth back through the nose. Fortunately, specially designed baby bottles and nipples that help keep fluids flowing downward toward the stomach are available. Children with a cleft palate may need to wear a man-made palate to help them eat properly and ensure that they are receiving adequate nutrition until surgical treatment is provided. Ear infections/hearing loss. Children with cleft palate are at increased risk of ear infections since they are more prone to fluid build-up in the middle ear. If left untreated, ear infections can cause hearing loss. To prevent this from happening, children with cleft palate usually need special tubes placed in the eardrums to aid fluid drainage, and their hearing needs to be checked once a year. Speech problems. Children with cleft lip or cleft palate may also have trouble speaking. These children's voices don't carry well, the voice may take on a nasal sound, and the speech may be difficult to understand. Not all children have these problems and surgery may fix these problems entirely for some. For others, a special doctor, called speech pathologist, will work with the child to resolve speech difficulties. Dental Problems. Children with clefts are more prone to a larger than average number of cavities and often have missing, extra, malformed, or displaced teeth requiring dental and orthodontic treatments. In addition, children with cleft palate often have an alveolar ridge defect. The alveolus is the bony upper gum that contains teeth. A defect in the alveolus can (1) displace, tip, or rotate permanent teeth, (2) prevent permanent teeth from appearing, and (3) prevent the alveolar ridge from forming. These problems can usually be repaired through oral surgery.
Causes: The cause of these abnormalities can only be theorized as they are not actually known. So far as research has shown, one of the causes is multiple gene defects with both parents having contributed.
Research shows that factors in the environment play a role as well since there are higher rates in certain areas of the world with hardly any in other areas. It is speculated that both genetics and environment play a role in the development of this abnormality. Those who are born with this abnormality have a higher chance of having a child with the same condition.
Parents who did not have this abnormality and gave birth to a child who did are about 8% more likely to have another child with the same issue. Parents who have had this abnormality are around 6% sure to have a child with it as well. It has been found that if a child born with this abnormality to a parent who had it as well, the chance of future children being affected is great and genetic counseling should be sought out.
Risk Factors: Genetics and family history Ethnicity
Gender- boy children are two times are likely to be born with this abnormality than are girl children. Environment- some research points in the direction of the use of certain drugs to be a possible cause. It has been shown that if the mother is obese then the risk for having a child with this abnormality is increased by a low percentage.
Symptoms and signs
Signs are clearly present at birth with little room for doubt of what the problem is. Upon first examination, the abnormality is clear. The lip may present with a tiny notch or reach from its place on the lip all the way to the upper gum, with the palate reaching the bottom part of the nose. Sucking may not be possible depending on the severity of the abnormality Possible malnutrition due to feeding issues Speech and hearing can be affected if not properly treated
Treatment
When a child is born with this condition there are many steps in getting the proper treatment including. Pre-surgery treatments: OrthoCleft retainer to help decrease the open gap within the mouth. This is also helpful in stretching out the lip muscles, reshaping the nose, and helping to improve the ability to suck, drink and eat. A surgical procedure: It is highly successful in closing the cleft. It also repairs the problems with the nose and lip that are connected to the cleft. Repair of the lip is typically done at 3 months of age but will likely require surgery in the future. Repair of the palate is more complicated and is typically done at 9 months, but no later than 18 months. In addition to the original procedure to fix the palate, more surgeries will likely be needed for the purpose of improving the outer appearance and help the patient with any breathing difficulties. These additional procedures can occur from the age of 18 months up to the age of 4 years.
Speech therapy: Those who have had this condition suffer from speech impediments. Speech therapy is used to help develop better and more age appropriate speech patterns.
Complications Of Disease
Dental problems due to teeth that are not positioned properly Delay and speech High risk of infection of the ear Hearing loss secondary to infection Problems with feeding when still at suckling stage
Prevention
While there is currently no preventive measures that can be taken to ensure that this condition will not affect your child, research suggests that taking prenatal vitamins and eating foods high in folic acid during pregnancy may reduce the chances of giving birth to a child with this condition.
You might also like
- A Simple Guide to Bad Breath and Mouth DiseasesFrom EverandA Simple Guide to Bad Breath and Mouth DiseasesRating: 5 out of 5 stars5/5 (3)
- ProDentim Review - How To Cure Gum Disease ?: How To Cure Tooth Decay Naturally....!!From EverandProDentim Review - How To Cure Gum Disease ?: How To Cure Tooth Decay Naturally....!!No ratings yet
- Ulcerative Lesions A Primary Aspect: Dr. Kanak KumarDocument5 pagesUlcerative Lesions A Primary Aspect: Dr. Kanak KumarArunabha SenguptaNo ratings yet
- Oral Lichen Planus GuideDocument5 pagesOral Lichen Planus GuideDr.Tina PaulNo ratings yet
- Tongue Conditions: ThrushDocument3 pagesTongue Conditions: Thrushdwi vaniNo ratings yet
- What Is A Dental Abscess?Document3 pagesWhat Is A Dental Abscess?Nabila RizkikaNo ratings yet
- GINGIVITISDocument43 pagesGINGIVITISRamyaNo ratings yet
- Oral Disorder Drug Classifications and TreatmentsDocument36 pagesOral Disorder Drug Classifications and TreatmentsAyeza DuaNo ratings yet
- Cara Perawatan Gigi Tiruan LepasanDocument3 pagesCara Perawatan Gigi Tiruan LepasanBayyin Bunayya CholidNo ratings yet
- Git DisordersnewDocument401 pagesGit DisordersnewstaceyatienoomaNo ratings yet
- XerostomiaDocument9 pagesXerostomiaSurya Navisa YunidNo ratings yet
- Vanya FionaDocument3 pagesVanya FionaVanya FionaNo ratings yet
- Oral Thrush CausesDocument7 pagesOral Thrush CausesMichael Eka PutraNo ratings yet
- EBL Case 4Document4 pagesEBL Case 4T LolaNo ratings yet
- Oral Surgery and InfectionsDocument32 pagesOral Surgery and InfectionsTheSuperJayR100% (1)
- Oral ThrushDocument29 pagesOral ThrushTushar KhuranaNo ratings yet
- What Are Mucous CystsDocument10 pagesWhat Are Mucous CystsNena TamaraNo ratings yet
- Oral DisordersDocument24 pagesOral DisordersHayat AL AKOUMNo ratings yet
- Acute Necrotizing Ulcerative GingivitisDocument7 pagesAcute Necrotizing Ulcerative GingivitisdonnyNo ratings yet
- StomatitisDocument17 pagesStomatitis4A - Hazel Ann G. EspinolNo ratings yet
- Riaz Gul AHN Unit 1Document106 pagesRiaz Gul AHN Unit 1Riaz Gul RindNo ratings yet
- Oral Path Flipchart 3Document7 pagesOral Path Flipchart 3api-397871513No ratings yet
- Oral Pathology in Pediatric DentistryDocument48 pagesOral Pathology in Pediatric DentistryHanin AbukhiaraNo ratings yet
- Date-58954846779f70 45433502 PDFDocument3 pagesDate-58954846779f70 45433502 PDFernestohiggins02No ratings yet
- Xerostomia Is The Medical Term For The Subjective Complaint of Dry Mouth Due To A Lack of SalivaDocument2 pagesXerostomia Is The Medical Term For The Subjective Complaint of Dry Mouth Due To A Lack of Salivaandy whiteNo ratings yet
- StomatitisDocument74 pagesStomatitisZahoor ZaidiNo ratings yet
- Mouth Sores: Symptoms and Treatment MethodsDocument1 pageMouth Sores: Symptoms and Treatment Methodslashes everafterNo ratings yet
- STOMATITISDocument12 pagesSTOMATITISninroseNo ratings yet
- A. What Is Perio-Endo Lesion?Document6 pagesA. What Is Perio-Endo Lesion?Emeka NnajiNo ratings yet
- Managing Dry Mouth and Oral Health in Sjogren's SyndromeDocument2 pagesManaging Dry Mouth and Oral Health in Sjogren's SyndromeShree ElangovanNo ratings yet
- Perawatan Mulut Pada Pasien PaliatifDocument20 pagesPerawatan Mulut Pada Pasien PaliatifFayruz Zahrotin Niswah100% (1)
- Management of Patients With Oral and Esophageal DisordersDocument81 pagesManagement of Patients With Oral and Esophageal DisordersEdmond ChanNo ratings yet
- Oral MoniliasisDocument16 pagesOral MoniliasisMel Izhra N. MargateNo ratings yet
- StomatitisDocument44 pagesStomatitisNessa Layos Morillo100% (1)
- (Health) Natural Remedies For Toothache and GumDocument4 pages(Health) Natural Remedies For Toothache and Gumcleverized100% (1)
- Complications in Complete Denture: Prosthodontic 5th Class DR - Mithaq Radhi Lecture (7,8)Document4 pagesComplications in Complete Denture: Prosthodontic 5th Class DR - Mithaq Radhi Lecture (7,8)ابراهيم منعم حسينNo ratings yet
- Xerostomia (Also Termed Dry Mouth: Xero-StomDocument6 pagesXerostomia (Also Termed Dry Mouth: Xero-Stomnazirrasheed123No ratings yet
- BSOM PiDocument6 pagesBSOM PiSai MonyNo ratings yet
- STOMATITISDocument17 pagesSTOMATITISTeguh Adi PartamaNo ratings yet
- Toothache and InfectionDocument31 pagesToothache and Infectionishaaadam114No ratings yet
- Herpes Simplex Oral: EpidemiologyDocument5 pagesHerpes Simplex Oral: EpidemiologyFariz RamadhanNo ratings yet
- 4 Cold Sores and Mouth UlcersDocument41 pages4 Cold Sores and Mouth UlcersLQYNo ratings yet
- Saliva DiseaseDocument8 pagesSaliva DiseaseJemuel Bucud LagartoNo ratings yet
- Management of Patients With Oral and Esophageal Disorders PDFDocument85 pagesManagement of Patients With Oral and Esophageal Disorders PDFNixi Mbuthia100% (1)
- Dry Mouth (Xerostomia)Document18 pagesDry Mouth (Xerostomia)dr_jamal1983No ratings yet
- Name: Nadia Yasmin NPM: 1810070110023 10 Questions and Answers Beside From Article Xerostomia (Dry Mouth) : Symtoms. Causes, Diagnosis, and TreatmentDocument4 pagesName: Nadia Yasmin NPM: 1810070110023 10 Questions and Answers Beside From Article Xerostomia (Dry Mouth) : Symtoms. Causes, Diagnosis, and TreatmentnadiaNo ratings yet
- Affected Sites: Ulcers Affecting Oral Cavity (Mouth)Document3 pagesAffected Sites: Ulcers Affecting Oral Cavity (Mouth)alexNo ratings yet
- E BulletinDocument3 pagesE BulletinNaresh SinghNo ratings yet
- Bad BreathDocument6 pagesBad BreathInternational Organization of Scientific Research (IOSR)No ratings yet
- Abses DentalDocument13 pagesAbses DentalQaulan SyahidaNo ratings yet
- XerostomiaDocument6 pagesXerostomiaAmira Pradsnya ParamitaNo ratings yet
- StomatitisDocument7 pagesStomatitisSang Ayu ArindaNo ratings yet
- Doctor Franke OtitisDocument6 pagesDoctor Franke OtitisMelanie McguireNo ratings yet
- Oral Complications of Cancer TreatmentDocument68 pagesOral Complications of Cancer TreatmentFarisha RasheedNo ratings yet
- Instruction Sheet: Salivary Gland Infections: (Parotitis Sialadenitis)Document1 pageInstruction Sheet: Salivary Gland Infections: (Parotitis Sialadenitis)azzam zhafranNo ratings yet
- TONSILLITIS AND TONSIL STONE EdittedDocument5 pagesTONSILLITIS AND TONSIL STONE EdittedNineja NinejaNo ratings yet
- Swollen Gums: Prepared By: Alaa AbdulkareemDocument9 pagesSwollen Gums: Prepared By: Alaa Abdulkareemمحمد عبدالهادي إسماعيلNo ratings yet
- Simple Mouth Odour Solutions That Guarantees Quick Results In 1 WeekFrom EverandSimple Mouth Odour Solutions That Guarantees Quick Results In 1 WeekNo ratings yet
- Rail Travel ConcessionDocument5 pagesRail Travel ConcessionfrdmaniacNo ratings yet
- R Reessuum Mee F Foorrm Maatt && C Coonntteenntt: Carol TecherDocument9 pagesR Reessuum Mee F Foorrm Maatt && C Coonntteenntt: Carol Techerhiteshtanwer13No ratings yet
- R Reessuum Mee F Foorrm Maatt && C Coonntteenntt: Carol TecherDocument9 pagesR Reessuum Mee F Foorrm Maatt && C Coonntteenntt: Carol Techerhiteshtanwer13No ratings yet
- BAMS AllDocument36 pagesBAMS AllKnr GannuNo ratings yet
- Good Practice in Pediatric and Adolescent Gynecology - Anna Maria Fulghesu - 2018Document256 pagesGood Practice in Pediatric and Adolescent Gynecology - Anna Maria Fulghesu - 2018Tan ManNo ratings yet
- Mouth Sores: Symptoms and Treatment MethodsDocument1 pageMouth Sores: Symptoms and Treatment Methodslashes everafterNo ratings yet
- THE PREVALENCE OF ORAL MUCOSAL LESIONS in MORADABAD - UTTAR PRADESH BY - DR. ANAND PRATAP SINGH SPONSERED BY: - RURAL DENTAL SOCIETY FOR ORAL DISEASE PREVENTION AND CURE - LUCKNOWDocument123 pagesTHE PREVALENCE OF ORAL MUCOSAL LESIONS in MORADABAD - UTTAR PRADESH BY - DR. ANAND PRATAP SINGH SPONSERED BY: - RURAL DENTAL SOCIETY FOR ORAL DISEASE PREVENTION AND CURE - LUCKNOWanandsingh001100% (4)
- Jurnal Traumatic Ulcerative GranulomaDocument3 pagesJurnal Traumatic Ulcerative Granulomagundul123No ratings yet
- DiseasesDocument52 pagesDiseasesKapil MathurNo ratings yet
- ENT in A Nutshell 2Document28 pagesENT in A Nutshell 2Gyleen ElegioNo ratings yet
- Clinical Practice Guidelines For Management of Recurrent Aphthous StomatitisDocument9 pagesClinical Practice Guidelines For Management of Recurrent Aphthous Stomatitislauren pangestuNo ratings yet
- Viral ExanthemsDocument67 pagesViral ExanthemsKay HanNo ratings yet
- Review of Oral Ulcerative Lesions in COVID-19 Patients: A Comprehensive Study of 51 CasesDocument8 pagesReview of Oral Ulcerative Lesions in COVID-19 Patients: A Comprehensive Study of 51 CaseselbertNo ratings yet
- 10 Common Superficial Tongue LesionsDocument9 pages10 Common Superficial Tongue LesionsAngga NNo ratings yet
- Oral Ulcer, Part 2Document32 pagesOral Ulcer, Part 2Mohammed abdalmenemNo ratings yet
- Oral UlcersDocument141 pagesOral UlcersKamal-Eldin Ahmed Abou-Elhamd100% (1)
- 2006 - Oral Medicine PDFDocument185 pages2006 - Oral Medicine PDFEcateryna Gianina100% (7)
- A Colour Handbook of Oral Medicine - M. Lewis, R. Jordan (Manson, 2004) WW PDFDocument177 pagesA Colour Handbook of Oral Medicine - M. Lewis, R. Jordan (Manson, 2004) WW PDFAdrian Tirla100% (1)
- Aphthous StomatitisDocument10 pagesAphthous StomatitisLjubomirErdoglijaNo ratings yet
- Oral Pathology in The Pediatric PatientDocument149 pagesOral Pathology in The Pediatric PatientDuONo ratings yet
- 4 Ways To Treat Canker Sores or Mouth Ulcers - WikiHowDocument11 pages4 Ways To Treat Canker Sores or Mouth Ulcers - WikiHowbnatarajNo ratings yet
- Types of Stomatitis: Sleep TongueDocument2 pagesTypes of Stomatitis: Sleep TongueBagus AnomNo ratings yet
- Anu Omr Long CaseDocument29 pagesAnu Omr Long CaseAnurtha AnuNo ratings yet
- Diseases of Oral Cavity ICD 10Document4 pagesDiseases of Oral Cavity ICD 10PKMKUNIRNo ratings yet
- Effect of Sodium Lauryl Sulfate On Recurrent Aphthous Stomatitis - A Randomized Controlled Clinical Trial.Document6 pagesEffect of Sodium Lauryl Sulfate On Recurrent Aphthous Stomatitis - A Randomized Controlled Clinical Trial.Jesús De Santos AlbaNo ratings yet
- StomatitisDocument3 pagesStomatitiswidya RDNo ratings yet
- Oral MedicineDocument136 pagesOral Medicineganang19No ratings yet
- Pharmacological Management of Common Soft Tissue Lesions of The Oral CavityDocument16 pagesPharmacological Management of Common Soft Tissue Lesions of The Oral CavityAcisum2No ratings yet
- Management Considerations For Pediatric Oral Surgery and Oral PathologyDocument10 pagesManagement Considerations For Pediatric Oral Surgery and Oral PathologyIrmayanti Meitrieka AmriNo ratings yet
- Oral Ulceration Causes and DiagnosisDocument10 pagesOral Ulceration Causes and Diagnosisمحمد حسنNo ratings yet
- Smoking and The Skin: Review ArticleDocument12 pagesSmoking and The Skin: Review ArticleAngie BecerraNo ratings yet
- Differential Diagnosis of Tongue LesionsDocument12 pagesDifferential Diagnosis of Tongue LesionsKartikakhairaniNo ratings yet
- Oral Cavity Genetic Disorders Affecting The Oral Mucosa and LipsDocument17 pagesOral Cavity Genetic Disorders Affecting The Oral Mucosa and LipsLakshya J BasumataryNo ratings yet
- Test Bank For Oral Pathology 7th Edition by RegeziDocument11 pagesTest Bank For Oral Pathology 7th Edition by RegeziSteve Isola100% (23)