Professional Documents
Culture Documents
153
Uploaded by
Dike Novalia AnggrainiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
153
Uploaded by
Dike Novalia AnggrainiCopyright:
Available Formats
153
Journal of Oral Science, Vol. 45, No. 3, 153-159, 2003 Original
Efficacy of Gamadent toothpaste on the healing of gingival tissues: a preliminary report
Tara Bai Taiyeb-Ali, Siti Lailatul Akmar Zainuddin, Dasan Swaminathan and Hashim Yaacob
Department of Oral Pathology, Oral Medicine and Periodontology, Faculty of Dentistry, University of Malaya, Kuala Lumpur, Malaysia
(Received 21 August 2002 and accepted 10 September 2003)
Abstract: The aim of this randomised, parallel, double-blind study, in which 28 adult patients diagnosed with chronic gingivitis or early stages of chronic periodontitis were recruited, was to evaluate the efficacy of Gamadent toothpaste compared to a placebo toothpaste. Gamadent toothpaste has all the basic constituents of a toothpaste with the addition of a sea cucumber extract (SCE) of the species Stichopus sp. 1 to improve the healing potential of tissues. The placebo has the same basic constituents minus the extract. Out of the 28 patients, 14 were placed in the test group who used the Gamadent toothpaste, and 14 patients were placed in the control group (2 control subjects defaulted and were excluded), who brushed using the placebo toothpaste. The longitudinal study was carried out over a period of 3 months with assessments made at baseline, 1 month, 2 months and 3 months after conventional therapy at the baseline visit. The clinical parameters used during the trial were Plaque Index (PI), Gingival Index (GI), Papilla Bleeding Index (PBI) and Probing Pocket Depth (PPD). A predetermined number of sites on a molar, premolar, canine and an incisor were examined and evaluated in each quadrant. After the baseline assessment, the patients had full mouth scaling and debridement as well as oral hygiene instructions. Patients were instructed to brush their teeth twice a day with the toothbrush provided (OralB plus, size 35) and toothpaste (test or control), using the Bass technique. At the 1-month assessment, there
Correspondence to Dr. Tara Bai Taiyeb-Ali, Department of Oral Pathology, Oral Medicine and Periodontology, Faculty of Dentistry, University of Malaya, 50603 Kuala Lumpur, Malaysia Tel: +60-3-79674554 Fax: +60-3-79674531 E-mail: tara@um.edu.my
were significant mean reductions to baseline mean values in PI (P < 0.005) and GI (P < 0.001) in the test group as compared to the control group. At the end of the 2-month interval, significant reductions were observed in PI, PBI and PPD (P < 0.001). By the end of 3 months, there were significant differences in the mean reduction of all the parameters i.e. PI, PBI, GI and PPD (P < 0.001), between the test and control sites. In conclusion, Gamadent toothpaste provided noteworthy benefits, producing statistically significant improvement in all clinical parameters compared to the placebo during the healing phase after conventional initial therapy. (J. Oral Sci. 45, 153-159, 2003)
Key words: sea cucumber; gingival/periodontal tissue; toothpaste.
Introduction
It has been known for at least several thousand years that marine organisms contain substances capable of exhibiting patent biological activity. Undoubtedly, we are aware that most of the currently available therapeutic agents stem either directly or indirectly from naturally occurring organic molecules derived from terrestrial plants and or animals as food for daily consumption. One of these marine living beings, particularly popular in some parts of Asia is the sea cucumber (1). Sea cucumbers are flexible, cylindrical-bodied creatures which move sluggishly over the ocean floor using their feeding tentacles to pick up food. These marine invertebrates are known as echinoderms, meaning they are spiny-skinned, and are close relatives of the sea urchin and sea star. For hundreds of years, the golden sea cucumber of species Stichopus sp. 1, locally known as gamat has
154
been prized by villagers for its healing properties. This marine creature is also commonly eaten as a side dish among the Malays in the northern part of Malaysia. In fact, villagers on Langkawi Island swear by the water extract of gamat as a remedy for cuts, peptic ulcers, chest pain, sores, inflammation and asthma. The ointment derived from the lipid soluble part of this marine animal is also used for the treatment of back and joint pain in communities living along the east and west coast of Peninsular Malaysia (1). Research on sea cucumbers began when the Filipino and Indonesian immigrants heavily depended on marine resources as a source of income and food. In Peninsular Malaysia, gamat (Stichopus sp. 1) is mainly used as a remedy for the treatment of asthma, hypertension and wound healing. Interest is currently being focused on identification of gamat species, taxonomy, ecological work, distribution, growth, edible species, nutrition, antibacterial and antifungal activity, anti-anaphylactic properties, wound healing, nerve muscle blocking action, histamine content, antihypertensive, antimicrobial and cytotoxic studies. Studies done on Air Gamat a local Malay name for the extract obtained from the sea cucumber of species Stichopus sp. 1, reported that it exhibited anti-inflammatory and analgesic properties (2,3). It was also shown to promote wound healing in rabbits (4) and guinea pigs (5) and antibacterial effects (6). In a study on rats, sea cucumber extract (SCE) at a dosage of 300 mg/kg also showed antiinflammatory properties with efficacy similar to indomethacin (7). The anti-nociceptive activity of SCE evaluated in mice when compared to morphine, aspirin and paracetamol showed efficacy of 50% of the peak analgesic response of morphine without its dependence and tolerance properties, and was equipotent to aspirin. SCE, unlike paracetamol, consistently showed marked analgesic effects in all the animal models used (8). Besides the abovementioned properties, SCE also exhibited antipruritic, anti-anaphylactic, gastroprotective and antipyretic effects (1). The heavy metal content analysis of crude SCE demonstrated levels of Fe, Mn, Cu and Zn (Fe > Mn > Cu > Zn), which were far below safety levels, and no Pb, Ni or Co were present (1). Hence, thus far, SCE from Stichopus sp. 1 has proven to be a safe therapeutic product. It has been used as a traditional form of medication which has withstood the test of time among the Malay people. Using this knowledge, a toothpaste incorporating the extract of this species of sea cucumber was formulated. The toothpaste Gamadent was formulated on the assumption that it wound be able to exert these therapeutic
properties on the gingival tissues to reduce gingival inflammation which usually manifests as gingival bleeding and gingival / periodontal pockets. A clinical trial was conducted to study the effect of this toothpaste on plaque removal and resolution of gingival inflammation in patients who had either gingivitis or early stages of periodontitis.
Materials and Methods
This was a double blind study where clinical measurements were taken longitudinally at baseline and the 4th, 8th and 12th week. Subjects for the study were selected from a population who had been seen at the Primary Care Dental Unit at the Faculty of Dentistry of University of Malaya, Kuala Lumpur. Patients chosen met a set of inclusion and exclusion criteria. Patients with a diagnosis of chronic gingivitis or early chronic adult periodontitis (periodontal pockets 5 mm and initial alveolar bone loss) were selected. They agreed to attend for treatment and clinical measurements required for the study, and consented to the protocol of the study. Patients with medical conditions such as heart disease, respiratory disease, blood dyscrasia, liver disease and kidney disease were excluded as well as those who had had antibiotics in the last 3 months, and pregnant patients. Twenty-eight subjects were included. Fourteen received the test toothpaste, Gamadent (Manufacturer: American Lion Toothpaste Manufacturing Sdn. Bhd. Company No.: 321149 T and SCE produced by Hexagon Pharmaceuticals (M) Sdn. Bhd. Company No.: 450453 D) (Table 1) and the other 14 were given a placebo toothpaste (identical toothpaste minus SCE). However 2 control subjects defaulted and were excluded from the study, leaving 12 in the control group. Standard Oral-B plus, size 35 toothbrushes were dispensed with the toothpastes. The subjects were matched closely by age, sex, ethnicity and disease status. Toothpastes were dispensed in unmarked white tubes for both test and placebo samples by one of the dental surgery assistants, who kept the records. The examiners were blind to these records. In this study, 4 teeth from each quadrant, making a total of 16 teeth, were selected in each patient: 1st or 2nd molars, 1st or 2nd premolars, canines, and central or lateral incisors. An alternative tooth was used if the first choice was missing or had crowns or defective restorations. The disto-buccal, mid-buccal, mesio-lingual and mid-lingual surfaces were scored for PI and GI, while the 6 surfaces scored for PPD were disto-buccal, mid-buccal, mesiobuccal, mesio-lingual, mid-lingual and disto-lingual. Serial measurements and treatment for each patient were
155
undertaken by the same examiner throughout the study. Scaling was done with an ultrasonic scaler for all subjects. Oral hygiene instructions including flossing and the Bass technique of tooth brushing were demonstrated to all subjects by the 3 examiners using charts, models and an Oral-B toothbrush. Subjects were instructed to avoid using mouthrinses or taking antibiotics. The sequence of treatment is illustrated as follows: Baseline Consent forms signed Clinical measurements (GI, PI, PBI, PPD) taken Full mouth scaling and polishing Oral hygiene instruction (Bass technique of toothbrushing + flossing) Assigned toothpastes and standard toothbrushes given 4th week Clinical measurements + RPC + assigned toothpastes and toothbrushes given 8th week Clinical measurements + RPC + assigned toothpastes and toothbrushes given 12th week Clinical measurements + RPC + assigned toothpastes and toothbrushes given
The clinical measurements made during this clinical trial were: 1. Gingival Index (GI) (9) 2. Plaque Index (PI) (10,11) 3. Papilla Bleeding Index (PBI) (12) 4. Probing Pocket Depth (PPD) The probing pocket depth measurements were carried out with a Williams periodontal probe.
Reproducibility measurements
Reproducibility of the clinical parameters was checked to obtain information on the errors of these measurements. Intra-examiner and inter-examiner reproducibility of clinical measurements were recorded for a total of 28 teeth per subject in the same 3 patients for the 3 examiners (the first 3 authors) for the indices used in the study. The intra-examiner and inter-examiner reproducibility results were calculated based on the acceptable figure of percentage agreement values (13). The agreement values of two researchers were counted sum of all the values 100%. The reproducibility of the plaque, gingival and papillary bleeding indices and pocket depth measurements were between 88 - 94%, 93.6 - 97.1% and 88.5 - 96.8% respectively amongst the 3 examiners. The intra-examiner reproducibility measurements for the 3 examiners were done on 3 other patients. The results were as follows: first author: PI = 96.9%, GI = 100%, PBI = 100%, and PPD = 95%; second author: PI = 96.9%, GI = 93.8%, PBI = 100%, and PPD = 92%; third author: PI = 100%, GI = 90%, PBI = 100%, and PPD = 85%.
RPC - Reinforced plaque control
Table 1 Formulation of Gamadent Toothpaste
Contents Sodium Benzoate Sodium Lauryl Ether Sulphate Purified Sea Cucumber Extract Glycerine Sorbitol Allantoin Thymol Flavour Silica CMC Phosphoric acid Sodium Saccharine SMFP Deionised Water
Percentage 500ppm 12.0% 10.0% 7.0% 4.0% 4.0% 2.0% 1.0% 1.0% 1.0% 0.2% 0.2% 0.1% Qs 100%
156
Table 2 Baseline mean values and standard deviation for the various indices in the test and control groups
Mean Values SD Indices Test (N = 15) Plaque Index Papilla Bleeding Index Gingival Index Probing Pocket Depth * Significant Difference 2.80 1.51 1.23 1.03 1.58 0.82 1.86 0.93 Control (N = 12) 2.33 1.38 1.20 1.21 1.42 0.75 1.74 1.18
Mean Difference (95% CI)
P-value
0.47 (0.33, 0.61) 0.03 (-0.14, 0.20) 0.16 (0.08, 0.24) 0.12 (0.03, 0.21)
< 0.001* 0.076 < 0.001* 0.005*
Table 3 Statistical analysis of differences in the mean reductions of plaque index SD from baseline measurements for test and control groups
1st month Test Group (N = 14) Control Group (N = 12) Mean Difference (95% CI) P-value * Significant Difference 1.54 1.43 1.26 1.35 0.28 (0.14, 0.41) < 0.001*
2nd month 1.59 1.41 1.10 1.29 0.52 (0.38, 0.65) < 0.001*
3rd month 1. 87 1.46 1.06 1.44 0.81 (0.66, 0.96) < 0.001*
Table 4 Statistical analysis of differences in the mean reductions of papilla bleeding index SD from baseline measurements for test and control groups
1st month Test Group (N = 14) Control Group (N = 12) 0.78 1.00 0.64 1.10
2nd month 0.91 0.87 0.40 1.55
3rd month 0.77 1.10 0.42 0.82
Mean Difference (95% CI) P-value * Significant Difference
0.14 (-0.02, 0.30) 0.078
0.51 (0.31, 0.70) < 0.001*
0.35 (0.20, 0.50) < 0.001*
157
Results
The data was subjected to statistical analysis using SPSS 9.0 and comparison of the results between the test and control subjects was done using an independent t-test. All the calculations were based on 5% significance level. The final group of subjects assessed consisted of 26 persons, 14 in the test group and 12 in the control group. There were 14 males and 12 females, with a mean age of 39.6 13.2 years (age range of 19-60 years). A total 796 surfaces in the test subjects and 624 surfaces in the control group were assessed for PI and GI. A total of 1104 surfaces in the test subjects and 930 surfaces in the control group were assessed for PPD, and 306 papillae of test subjects and 261 papillae of control subjects were studied for the PBI.
The baseline mean values for the various indices are depicted in Table 2. With the exception of the PBI, the rest of the mean values of the indices were significantly higher in the test subjects than in the control group in spite of matching the subjects and taking into consideration the 2 control patients who dropped out. Hence in the subsequent visits, mean reductions from baseline in the various indices were compared between the test and control groups to assess the effect of the SCE-containing toothpaste. The mean reduction in the PI as shown in Table 3 was observed in both test and control sites throughout the study period, although this was consistently and significantly greater at the test sites at the 1-, 2- and 3-month intervals from baseline (P < 0.001) in comparison to the control sites.
Table 5 Statistical analysis of differences in the mean reductions of gingival index SD from baseline measurements for test and control groups
1st month Test Group (N = 14) Control Group (N = 12) 1.21 0.99 1.05 0.73
2nd month 1.05 0.87 1.00 0.91
3rd month 1.18 0.86 0.83 0.81
Mean Difference (95% CI) P-value * Significant Difference
0.16 (0.08, 0.25) < 0.001*
0.05 (-0.03, 0.14) 0.235
0.35 (0.27, 0.44) < 0.001*
Table 6 Statistical analysis of differences in the mean reductions of pocket depth SD from baseline measurements for test and control groups
1st month Test Group (N = 14) Control Group (N = 12) 0.75 0.84 0.81 1.04
2nd month 0.68 1.02 0.51 1.15
3rd month 0.62 0.95 0.40 0.90
Mean Difference (95% CI) P-value * Significant Difference
0.06 (-0.13, 0.02) 0.139
0.17 (0.09, 0.26) < 0.001*
0.22 (0.15, 0.30) < 0.001*
158
The mean reduction in PBI in the test and control groups throughout the study period is shown in Table 4. The reduction in bleeding on probing was significantly greater at the test sites in comparison to the control sites at the 2and 3-month intervals (P < 0.001). At the 1-month interval the reduction was greater at test sites but this is not statistically significant (P = 0.5). Analysed data for the mean reduction of the GI from baseline is presented in Table 5. Throughout the study period, there was improvement in gingival inflammation in both the test and control group after conventional treatment of scaling and prophylaxis at baseline. At the 1- and 3-month intervals this improvement was statistically significantly greater in the test group as compared to the control group (P < 0.001), although the increase was not significant at the end of the 2nd month. The mean reduction in probing pocket depth is shown in Table 6. Probing pocket depths decreased in both the test and control groups during the period of the study. However the mean reduction was greater in the control group at the 1-month interval than the test group, although not significantly. At the 2-month and 3-month intervals the mean PPD reductions were significantly greater at the test sites (P < 0.001).
Discussion
The results of the present study demonstrated that improvement in plaque control and gingival conditions can be obtained after oral hygiene instruction and full mouth scaling in patients with gingivitis and early stages of chronic adult periodontitis. This was shown in both the test and control subjects and is consistent with numerous previous studies (14-16). It was observed that control of plaque or reduction in accumulation of plaque (as reflected by the mean reduction in the PI) was consistently and significantly better at the test sites throughout the study period. Whether this is a direct effect of SCE on the accumulation or adherence of plaque to the tooth surfaces is an interesting issue to investigate to rule out a coincidental finding. This effect could be verified by further research and by increasing the sample size. Gradual reduction of the papilla bleeding scores, GI scores and probing pocket depths occurred during the subsequent months at statistically significant levels more frequently at the test sites, possibly indicating that the rate of healing was greater at sites where SCE toothpaste was used. The SCE could have improved the rate of the healing process in the test group. As the subjects included in this study were mainly patients with early stages of periodontal disease, mainly
gingivitis and early periodontitis, the mean PPD of sites initially or at baseline were low, being 1.86 at the test sites and 1.74 at the control sites. Hence the dynamic range for healing or improvement is low in this group. Better appreciation of healing could occur where initial PPD scores are higher, and a greater dynamic range or potential for healing is present. This could be investigated in future studies to verify the effect of SCE on healing of pathological pockets. No side effects were reported by the patients and no clinical pathology was observed. In conclusion, the results of the preliminary report of this study must be interpreted within the limitations of the methodology and sample size used. A limited number of patients were used in this study. We suggest a larger sample size be used in future studies investigating this toothpaste. However the preliminary observations do indicate that plaque control seemed to improve in the group using Gamadent toothpaste containing SCE. In addition, this extract also appeared to increase the rate of healing during the first couple of months after initial therapy in the test group. These encouraging results could be confirmed with a larger sample size. An extension of this study to patients with more advanced disease status (moderately advanced and advanced periodontitis) could also be initiated and these clinical benefits could be further verified.
Acknowledgments
This study was supported by Vote F, University of Malaya, Kuala Lumpur, Malaysia and Hexagon Pharmaceuticals Sdn. Bhd., Malaysia.
References
1. Yaacob H, Kim KH, Shahimi M, Aziz NS, Sahil SM (1997) Malaysian sea cucumber (Gamat): a prospect in health food and therapeutic. Proceeding in Asian Food Technology Seminar, 6 2. Kim KH, Chin KY, Chin KC, Yaacob HB (2001) Anti-anaphylactic shock properties of sea cucumber water extract (Air Gamat). Proceedings of Malaysian Science and Technology Congress 2001, 89 (Abstract) 3. Yaacob H, Shahimi MM, Kim KH, Christina GY, Yeap N (1994) The effect of sea cucumber water extract on writhing induced by acetic acid in mice. J Biosci 5, 1-4 4. Ridzwan BH, Mohd Nor BI, Norhayati BI, Kaswandi MD, Rozali MBO, Fasihuddin BA (1990) Timun Laut (holoturoid) Sabah: Jus kasar beberapa species sebagai pemudah penyembuhan luka aruhan. Symposium on Applied Biology of Malaysia,
159
Universiti Kebangsaan Malaysia, Serdang, 48 (Abstract) 5. Yaacob HB, Kim KH, Shahimi MM, Jamalulail SMS (1994) Water extract of Stichopus sp 1 (Gamat) improves wound healing. Jurnal Perubatan Universiti Kebangsaan Malaysia 16, 19-29 6. Ridzwan BH, Kaswandi MA, Azman Y, Faud M (1995) Screening for antibacterial agents in three species of sea cucumber from coastal areas of Sabah. Gen Pharmacol 26, 1539-1543 7. Yaacob HB, Kim KH, Shahimi MM (1994) Antinociceptive effect of the water extract of Malaysian sea cucumber, Stichopus sp. 1. Asia Pac J Pharmacol 9, 23-28 8. Yaacob HB, Kuraishi Y (1995) Emergence of biologically active histidine-containing peptides in golden sea cucumber extract. Jpn J Pharmacol 198, 98 (Proceeding) 9. Silness J, Loe H (1964) Periodontal disease in pregnancy II. Correlation between oral hygiene and periodontal condition. Acta Odont Scandinavian 22, 121-135 10. Quigley GA, Hein JW (1962) Comparative cleansing
efficiency of manual and power brushing. J Am Dent Assoc 65, 26-29 11.Turesky S, Gilmore ND, Glickman I (1970) Reduced plaque formation by the chloromethyl analogue of vitamin C. J Periodontol 47, 41-43 12. Saxer U, Muhlemann H (1975) Motivation und Aufklarung. Schweiz Monatsschr Zahnheilkund 85, 905-919 13. Polson AM (1997) The research team, calibration, and quality assurance in clinical trials in periodontics. Ann Periodontol 2, 75-82 14. Morrison EC, Ramfjord SP, Hill RW (1980) Shortterm effects of initial, nonsurgical periodontal treatment (hygienic phase). J Clin Periodontol 7, 199211 15. Greenstein G (1992) Periodontal response to mechanical non-surgical therapy: a review. J Periodontol 63, 118-30 16. Cercek JF, Kiger RD, Garett S, Egelberg J (1983) Relative effects of plaque control and instrumentation on the clinical parameters of human periodontal disease. J Clin Periodontol 10, 46-56
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Indian Institute OF Management, BangaloreDocument20 pagesIndian Institute OF Management, BangaloreGagandeep SinghNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- EPF Passbook Details for Member ID RJRAJ19545850000014181Document3 pagesEPF Passbook Details for Member ID RJRAJ19545850000014181Parveen SainiNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Universal Robina Co. & Bdo Unibank Inc.: Research PaperDocument25 pagesUniversal Robina Co. & Bdo Unibank Inc.: Research PaperSariephine Grace ArasNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- UT Dallas Syllabus For Ee3311.002.07f Taught by Gil Lee (Gslee)Document3 pagesUT Dallas Syllabus For Ee3311.002.07f Taught by Gil Lee (Gslee)UT Dallas Provost's Technology GroupNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Mba Project GuidelinesDocument8 pagesMba Project GuidelinesKrishnamohan VaddadiNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Principles of Cost Accounting 1Document6 pagesPrinciples of Cost Accounting 1Alimamy KamaraNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Genre Worksheet 03 PDFDocument2 pagesGenre Worksheet 03 PDFmelissaNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hastrof Si Cantril. 1954. The Saw A Game. A Case StudyDocument6 pagesHastrof Si Cantril. 1954. The Saw A Game. A Case Studylandreea21No ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- MVJUSTINIANI - BAFACR16 - INTERIM ASSESSMENT 1 - 3T - AY2022 23 With Answer KeysDocument4 pagesMVJUSTINIANI - BAFACR16 - INTERIM ASSESSMENT 1 - 3T - AY2022 23 With Answer KeysDe Gala ShailynNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- Fundamental Managerial Accounting Concepts 9th Edition Edmonds Solutions ManualDocument35 pagesFundamental Managerial Accounting Concepts 9th Edition Edmonds Solutions ManualDrMichelleHutchinsonegniq100% (15)
- Assessing Eyes NCM 103 ChecklistDocument7 pagesAssessing Eyes NCM 103 ChecklistNicole NipasNo ratings yet
- Donny UfoaksesDocument27 pagesDonny UfoaksesKang Bowo D'wizardNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- All MeterialsDocument236 pagesAll MeterialsTamzid AhmedNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Electrocardiography - Wikipedia, The Free EncyclopediaDocument18 pagesElectrocardiography - Wikipedia, The Free Encyclopediapayments8543No ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Caribbean Examinations Council Caribbean Secondary Certificate of Education Guidelines For On-Site Moderation SciencesDocument9 pagesCaribbean Examinations Council Caribbean Secondary Certificate of Education Guidelines For On-Site Moderation SciencesjokerNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Mama Leone's Profitability AnalysisDocument6 pagesMama Leone's Profitability AnalysisLuc TranNo ratings yet
- English Skills BookDocument49 pagesEnglish Skills BookAngela SpadeNo ratings yet
- Ilham Bahasa InggrisDocument12 pagesIlham Bahasa Inggrisilhamwicaksono835No ratings yet
- SIM5320 - EVB Kit - User Guide - V1.01 PDFDocument24 pagesSIM5320 - EVB Kit - User Guide - V1.01 PDFmarkissmuzzoNo ratings yet
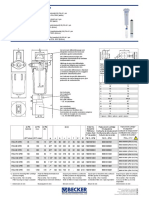
- Medical filter performance specificationsDocument1 pageMedical filter performance specificationsPT.Intidaya Dinamika SejatiNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Front Cover Short Report BDA27501Document1 pageFront Cover Short Report BDA27501saperuddinNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- HU675FE ManualDocument44 pagesHU675FE ManualMar VeroNo ratings yet
- Main Hoon Na - WikipediaDocument8 pagesMain Hoon Na - WikipediaHusain ChandNo ratings yet
- Panasonic TC-P42X5 Service ManualDocument74 pagesPanasonic TC-P42X5 Service ManualManager iDClaimNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Power Bi ProjectsDocument15 pagesPower Bi ProjectssandeshNo ratings yet
- Lec 10 - MQueues and Shared Memory PDFDocument57 pagesLec 10 - MQueues and Shared Memory PDFUchiha ItachiNo ratings yet
- STERNOL Specification ToolDocument15 pagesSTERNOL Specification ToolMahdyZargarNo ratings yet
- The Invisible Hero Final TNDocument8 pagesThe Invisible Hero Final TNKatherine ShenNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- T23 Field Weld Guidelines Rev 01Document4 pagesT23 Field Weld Guidelines Rev 01tek_surinderNo ratings yet
- Types of LogoDocument3 pagesTypes of Logomark anthony ordonioNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)