Professional Documents
Culture Documents
Anaphylasis
Uploaded by
Deepu VijayaBhanuOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Anaphylasis
Uploaded by
Deepu VijayaBhanuCopyright:
Available Formats
ANAPHYLAXIS
INTRODUCTION Anaphylaxis is an immediate life threatening hypersensitive allergic reaction. This is sudden and severe allergic reaction occurs within minutes of exposure in hypersensitive patients. It progresses rapidly and results in anaphylactic shock and death within 15 minutes, if medical intervention is not immediately pursued. It can be triggered by exposure to food(peanuts, wheatgemsetc),medications(pencillin,morphine sulphate etc.) ,insect venom(bee stings,spider bites),latex ( gloves,equipment) or other diagnostic agents. DEFINITION Anaphylaxis is a clinical response to an immediate immunologic reaction between a specific antigen and an antibody. The reaction results from a rapid release of IgE mediated chemicals, which can induce a severe, life threatening allergic reaction. TYPES OF HYPERSENSITIVITY The immune system will normally react to protect people in the presence of a foreign antigen. An exaggerated or misdirected immune response to an allergen that results in tissue injury is called a hypersensitive response. Type-I Hypersensitivity The type-I hypersensitivity reaction is an immediate type of hypersensitivity reaction. This reaction occurs when a specific antigen induces an allergic reaction, provoked by re exposure to the same antigen. The contact, inhalation, ingestion or injection of the allergens creates an allergic reaction mediated by specific IgE antibodies, the cellular release of histamine and other vasoactive meditors, resulting in an immediate local or systemic reaction (anaphylaxis).E.g. allergic rhinitis, asthma. Type-2 Hypersensitivity These are cytotoxic reactions where the antibody (IgG or IgM) is directed against antigen on an individuals own cells or against foreign antibody, such as that required after blood transfusion. This may lead to cytotoxic action by killer cells or to lysis mediated by the complement system.E.g. Transfusion reaction. Type-3 Hypersensitivity
These reactions are immune complex reactions where immune complexes (antigen and usually IgG or IgM) are deposited in the tissue. The complement is activated causing local tissue damage and inflammation. The types of diseases encountered are classified into acute and chronic serum sickness and local inflammatory response due to deposition of immune complexes in tissue.E.g. Systemic lupus erythematosus, rheumatoid arthritis. Type-4 Hypersensitivity These reactions are cell mediated reactions, which are also called delayed hypersensitivity. Allergic contact dermatitis after exposure to ointments containing active drugs is the most frequent form of drug mediated delayed hypersensitivity. Various forms of type-4 hypersensitivity are recognized: contact hypersensitivity, tuberculin type hypersensitivity and granulomatous hypersensitivity or Crohns disease, leprosy, tuberculosis etc. E.g. Transplant reaction. ETIOLOGY There are numerous risk factors associated with the incidence and prevalence of anaphylaxis. The non modifiable risk factors include age,gender and race. Modifiable risk factors include the allergens route of entry, atopy and exposure history. NON MODIFIABLE RISK FACTORS Age: Adults have a higher reported rate of reactions to antibiotics,contrast media,aesthetic agents and insect stings,where as children have a higher rate of reported reactions to food antigens. Gender: Anaphylaxis is more frequent in boys than girls under age 15,but among adults,women are more frequently affected than men.Women have a higher incidence of reactions to aspirin,muscle relaxants,contrast material and latex and men have a higher recorded incidence of anaphylaxis to insect sting venom. Race: No differences have been noted. MODIFIABLE RISK FACTORS Route of entry: Anaphylaxis can occur with all route of administration with episodes more frequent and severe if the offending antigen enters through the skin rather than orally.
Atopy: The incidence of anaphylaxis to latex and foods is higher in atopic individuals. The data are conflicting regarding antibiotic reactions with some studies finding anaphylaxis to pencillin more common in atopic patients and others finding no correlation between atopy and pencillin allergy or even a lower risk for pencillin hypersensitivity with atopic individuals. PATHOPHYSIOLOGY It can be induced or aggravated by exercise and some patients have recurrent symptoms for no identifiable reason.Histamine and other substances are generated or released when the antigen reacts with IgE on basophils and mast cells. These substances causes smooth muscle contraction and vascular dilation and characterise anaphylaxis. Vaso dialation and escape of plasma into the tissues causes urticaria and angioedema and result in a decrease in effective plasma volume,which is the major cause of shock. Fluid escapes into the lung alveoli and may produce pulmonary oedema. Obstructive angioedema of the upper airway may also occur. Arrythmias and cardiogenic shock may develop if the reaction is prolonged. CLINICAL MANIFESTATION System Skin Symptom Urticaria and angioedema ,flushing and pruritus . Respiratory Gastro intestinal Cardio VascularSystem Neurological Headaches,dizziness etc. Dyspnea,wheezing etc. Nausea and vomiting, diarrhoea. Tachycardia
DIAGNOSTIC EVALUATION History and physical examination. Laboratory Investigation.
MANAGEMENT Planning and implementation Anaphylactic reactions occurs suddenly in hypersensitive patients following exposure to an offending allergen. The speed of response is the cardinal principle in therapeutic management of anaphylaxis. The following are four areas of primary concern for the crisis management: a) Reconize the signs and symptoms b) Maintain a patent airway c) Prevent the spread of the allergen by using a tourniquet when appropriate and d) Administer appropriate drugs. Inaddition the nurse must place the patient in a recumbent position,elevate the legs,keep the patient warm and provide support for respiration with oxygen. The patient must have maintained BP with IV fluids. Hypovolaemic shock may occur because of fluid moving from IV to interstitial spaces. Hypovolaemic shock, if not treated early, leads to irreversible tissue damage and death. When an allergic disorder is diagnosed, treatment is aimed at reducing exposure, treating symptoms and desensitising the person through immunotherapy. Adjuncts to therapy include medical alert bracelets, bee sting kits with an epipen and education in emergency self administration. MEDICAL MANAGEMENT Pharmaceutical management of anaphylaxis is necessary as an immediate treatment. Epinephrine is the most common medication given in acute care setting during the crisis of anaphylaxis and Benadryl is likely the most typical non prescription medication given to prevent anaphylaxis or to treat the early clinical manifestations of an allergic reaction. Classifications Drugs Indications
Parental adrenergic agents
Epinephrine
Urticaria,angioedema,airway obstruction,bronchospasm.
Inhaled beta antagonists
Bronchospasm. Albuterol
H1 receptor blockers(anti histamines)
Benadryl
Cutaneous lesions.
H2 receptor blockers Corticosteroids
Cimetidine Methylprednisolone
Cutaneous lesions. Bronchospasm,cutaneous lesions.
Oxygen inhalation is administered. Intra venous access. NURSING MANAGEMENT If a patient is experiencing an allergic response,the nurses initial action is to assess the patient for: Signs and symptoms of anaphylaxis. Assess the airway, breathing pattern,and other vital signs. Patient is observed for signs of increasing oedema and respiratory distress. Prompt notification of the physician and preparation for initiation of emergency measures( intubation,administration of emergency medications,insertion of intra venouys lines,fluid administration,oxygen administration) are important to reduce the severity of the reaction and to restore cardiovascular function. The nurse documents the interventions used and the patients response to treatment,vital signs, and laboratory values.
PREVENTION Strict avoidance of potential allergens is an important preventive measure for the patient at risk for anaphylaxis. Patients at risk for anaphylaxis from insect stings should avoid areas populated by insects and should use appropriate clothing, insect repellent,and caution to avoid further stings.
COMPLICATIONS Complications of anaphylaxis include: Respiratory failure Cardiac arrest Shock Airway obstruction SUMMARY Anaphylaxis is sudden and severe allergic reaction occurs within minutes of exposure in hypersensitive patients. It progresses rapidly and results in anaphylactic shock and death within 15 minutes, if medical intervention is not immediately pursued. It can be triggered by exposure to food(peanuts, wheatgemsetc),medications(pencillin,morphine sulphate etc.) ,insect venom(bee stings,spider bites),latex ( gloves,equipment) or other diagnostic agents. CONCLUSION Anaphylaxis is a major life threatening condition. If it is not treated it will leads to death. So anaphylaxis is a major emergency. So it must need medical emergency and seeks attention. BIBLIOGRAPHY 1. Smeltzer C S, Bare B, Text book of medical surgical nursing, 10th edition, Lippincott publishers, page no:312,313,403,424 2.Black M J, Hawks H J, Medical surgical nursing, 6th edition, Saunders publications, Page no:2324-2328 3. Phipps, Long, Woods, Medical surgical nursing and clinical practice, Mosby publications, Page no:399-404. 4. Lewis, Heitkemper, Dirksen, Medical surgical nursing, 6th edition, Mosby publications, Page no:389-394.
You might also like
- Avicenna ADocument17 pagesAvicenna ADeepu VijayaBhanuNo ratings yet
- PhylosophyDocument20 pagesPhylosophyDeepu VijayaBhanuNo ratings yet
- Teacher Role - M.SCDocument9 pagesTeacher Role - M.SCDeepu VijayaBhanuNo ratings yet
- Discipline - M.SCDocument17 pagesDiscipline - M.SCDeepu VijayaBhanuNo ratings yet
- Menstrual Irreglarities 2Document19 pagesMenstrual Irreglarities 2Deepu VijayaBhanuNo ratings yet
- ArdsDocument29 pagesArdsDeepu VijayaBhanuNo ratings yet
- LeptospirosisDocument9 pagesLeptospirosisDeepu VijayaBhanuNo ratings yet
- Discipline - M.SCDocument17 pagesDiscipline - M.SCDeepu VijayaBhanuNo ratings yet
- Source of Infections 1. Endogenous SourceDocument6 pagesSource of Infections 1. Endogenous SourceDeepu VijayaBhanuNo ratings yet
- Critical ThinkingDocument32 pagesCritical ThinkingDeepu VijayaBhanuNo ratings yet
- Student WelfareDocument2 pagesStudent WelfareDeepu VijayaBhanu100% (1)
- Public Relations M.SCDocument9 pagesPublic Relations M.SCDeepu VijayaBhanuNo ratings yet
- BudgetDocument12 pagesBudgetDeepu VijayaBhanu100% (1)
- Adminis-Responsibility For CurriculamDocument12 pagesAdminis-Responsibility For CurriculamDeepu VijayaBhanuNo ratings yet
- Inservice EducationDocument7 pagesInservice EducationDeepu VijayaBhanu97% (30)
- GuidanceDocument13 pagesGuidanceDeepu VijayaBhanuNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Precautionary and Sanitary Practices in Handling FoodDocument31 pagesPrecautionary and Sanitary Practices in Handling FoodBrenNan ChannelNo ratings yet
- Ilovepdf Merged PDFDocument134 pagesIlovepdf Merged PDFhelalNo ratings yet
- Bulacan State University College of Nursing City of Malolos, BulacanDocument2 pagesBulacan State University College of Nursing City of Malolos, BulacanVIRGINIA M. SANTOSNo ratings yet
- Top 50 Global Stem Cell InfluencersDocument25 pagesTop 50 Global Stem Cell InfluencersranasoftNo ratings yet
- Nervous System Brain Retina - QDocument70 pagesNervous System Brain Retina - QVarshLokNo ratings yet
- CHAPTER 11: The History and Physical Examination: An Evidence Based ApproachDocument5 pagesCHAPTER 11: The History and Physical Examination: An Evidence Based ApproachReda SoNo ratings yet
- Katrina D. Varon Bs-Nursing 2Document13 pagesKatrina D. Varon Bs-Nursing 2Marc FresNo ratings yet
- Preventive Resin Restorations: Review ArticlesDocument3 pagesPreventive Resin Restorations: Review ArticlesClaypella MaskNo ratings yet
- Can I Get That in WritingDocument4 pagesCan I Get That in WritingNorische100% (1)
- The Tragedy of Schizophrenia Without PsychotherapyDocument30 pagesThe Tragedy of Schizophrenia Without PsychotherapyRachel AHNo ratings yet
- Sept 3 2017Document7 pagesSept 3 2017Reda SoNo ratings yet
- Psychopharma NotesDocument3 pagesPsychopharma Noteszh4hft6pnzNo ratings yet
- Post Natal ExercisesDocument7 pagesPost Natal ExercisesEvie Dolpin BlueNo ratings yet
- Ast (Sgot) ColorDocument2 pagesAst (Sgot) ColorShribagla MukhiNo ratings yet
- Note Regarding Retiring DoctorsDocument3 pagesNote Regarding Retiring DoctorsnamankumaragrawalNo ratings yet
- Perbedaan Kadar Hbsag Sampel Serum Dan Plasma Metode Clia Pada PendonorDocument7 pagesPerbedaan Kadar Hbsag Sampel Serum Dan Plasma Metode Clia Pada PendonorAAK DHGRiski MaulanaNo ratings yet
- Kainan University ApplicationDocument25 pagesKainan University ApplicationGeraldine RiveraNo ratings yet
- Kansas Foodborne Illness ManualDocument186 pagesKansas Foodborne Illness ManualLeo M. Pedro Jr.No ratings yet
- Menstrual DisordersDocument45 pagesMenstrual DisordersMegat Mohd Azman Adzmi100% (1)
- Status of DNB Seats - Bulletin - StatewiseSpecialitywise - WU26022009Document142 pagesStatus of DNB Seats - Bulletin - StatewiseSpecialitywise - WU26022009raghavagummadiNo ratings yet
- Dental AssistantDocument2 pagesDental Assistantapi-78993102No ratings yet
- Coliform Analysis in Wastewater 2012Document24 pagesColiform Analysis in Wastewater 2012engrbvgNo ratings yet
- Daftar ObatDocument1 pageDaftar ObatPramukadua DepokNo ratings yet
- HistoryDocument47 pagesHistoryRajesh IthaNo ratings yet
- Mendiguchia 2012 Rectus Femoris Muscle Injuries in Football-A Clinically Relevant Review of Mechanisms of Injury, Risk Factors and Preventive Strategies PDFDocument11 pagesMendiguchia 2012 Rectus Femoris Muscle Injuries in Football-A Clinically Relevant Review of Mechanisms of Injury, Risk Factors and Preventive Strategies PDFJuan PalomoNo ratings yet
- Animal Welfare Board of India v. A Nagaraja & Ors PDFDocument117 pagesAnimal Welfare Board of India v. A Nagaraja & Ors PDFBar & Bench100% (1)
- S/N Description UnitDocument16 pagesS/N Description UnitPeccamb SurgicalNo ratings yet
- Computer Addiction Power Point PresentationDocument24 pagesComputer Addiction Power Point PresentationGee A50% (4)
- Vital Signs Vital Signs: Importance: ImportanceDocument6 pagesVital Signs Vital Signs: Importance: ImportanceTyron KristianNo ratings yet
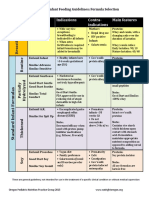
- Formula Selection OPNPGDocument2 pagesFormula Selection OPNPGRina PratiwiNo ratings yet