Professional Documents
Culture Documents
Basic Life Support
Uploaded by
Florence De ChavezOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Basic Life Support
Uploaded by
Florence De ChavezCopyright:
Available Formats
BASIC LIFE SUPPORT: HEALTHCARE PROVIDER INTRODUCTION Optimal patient care requires that the EMT-I be proficient in Basic
Life Support according to American Heart Association (AHA) Healthcare Provider (HCP) standards, as well as be able to identify situations in which CPR can be withheld according to L.A. County guidelines. The following topics will be discussed during this lesson: Chain of Survival and the Role of the Healthcare Provider Clinical Presentations and Treatment of Heart Disease and Stroke Prudent Heart Living Techniques for Adult and Pediatric CPR and Use of the AED Pathophysiology, Treatment and Prevention of Foreign Body Airway Obstruction Injury Prevention in the Pediatric Age Group L.A. County guidelines for withholding CPR
When to start CPR When to start rescue breathing, including ventilation with a barrier device and bag-mask ventilation (with and without oxygen) How to check for normal breathing or signs of circulation The ABC sequence of CPR When and how to use an AED The signs of severe or complete FBAO How to relieve FBAO in the responsive and unresponsive victim
3. Describe the signs of 5 major emergencies in adults Heart attack Stroke Cardiac arrest Respiratory arrest FBAO 4. Describe strategies to prevent sudden infant death syndrome in infants and injuries in children. 5. Using an adult, child, or infant manikin, demonstrate the following skills: Activation of the emergency response system (phone 911 or other appropriate response system) Rescue breathing using mouth-to mouth and bag-mask ventilation (with and without oxygen) for adult, child, and infant victims 1- and 2-rescuer CPR for adult, child, and infant victims Use of an AED for victims 8 years of age (and approximately 25 kg or more) Relief of FBAO in the responsive and unresponsive victim of any age
LESSON OBJECTIVES At the end of this lesson the participants will be able to: 1. Describe the links in the AHA Chain of Survival, including the importance of: Activating the appropriate emergency response system (phoning 911 or other response system) Performing CPR Using a barrier device Providing bag-mask ventilation Providing early defibrillation Ensuring the arrival of early advanced care by activating the appropriate emergency response system (phoning 911 or other response system) 2. Describe the steps of CPR:
SKILLS One Rescuer: Adult, Child, and Infant CPR Two Rescuer: Adult CPR FBAO Conscious and Unconscious: Adult, Child, and Infant Bag-mask ventilation
KEY VOCABULARY The following terms will be used during this lesson: Adult Greater than eight years of age Child - One year to eight years of age Infant - Less than one year of age Prudent Heat Living a lifestyle that minimizes the risk of future heart disease. Epigastrium - upper mid-portion of abdomen Nitroglycerin - a medication that acts by dilating the coronary arteries, which increases KEY CONCEPTS The following section provides information and space for taking notes on the key concepts discussed by the instructor. American Heart Association Statistics Cardiovascular disease is the leading cause of death in the U.S. Cardiovascular disease accounts for nearly one million deaths per year in the U.S. Approximately million deaths are due to acute myocardial infarction; approximately 50% of these deaths are sudden and occur within the first hour of the onset of symptoms Stroke is the third leading cause of death in the U.S. and the leading cause of brain injury in adults Approximately million suffer a stroke and nearly of these die annually
blood flow to the heart muscle; and lowering the blood pressure and dilating the veins, which decreases the work of the heart and the heart muscle's need for oxygen. Ventricular Fibrillation - a chaotic, uncoordinated quivering of the heart muscle, producing no heartbeat Pneumothorax - collapsed lung Hemothorax - blood in the pleural cavity Fat Emboli - fat bubbles or particles circulating in blood stream as a result of long bone fractures
Includes all responses (prehospital and in-hospital) needed to stabilize the victim or patient who develops life-threatening events affecting the respiratory, cardiovascular, and cerebrovascular systems Ultimate goal is to maximize the outcome for all victim or patients Two components of ECC are BLS and ACLS
Basic Life Support (BLS) Includes interventions that can rapidly be performed by trained laypersons and healthcare providers to ensure recognition of common emergencies, access to ACLS, adequate airway, breathing, and oxygenation, and adequate circulation BLS skills include CPR, use of AED, and relief of foreign body airway obstruction
Emergency Cardiovascular Care (ECC)
Advanced Cardiac Life Support Includes BLS plus the use of adjunctive equipment to support ventilation, establishment of IV access, administration of drugs, use of cardiac monitoring, defibrillation or other control of arrhythmias, and care after resuscitation
The link most likely to improve survival rates Time to defibrillation is the critical variable for successful conversion from VF to a normal rhythm Every minute that passes can reduce the chance for successful conversion by 7-10% Goal of early defibrillation: Within 5 minutes of EMS call receipt to shock
CHAIN OF SURVIVAL Fourth Link: Early Advanced Care Early Access Early CPR Early Defibrillation Early Advanced Care
Designed to prevent cardiac arrest through the use of advanced airway management, administration of medication, and other interventions Include therapies that help First Link: Early Access resuscitate victims of cardiac arrest who are not responding to defibrillation Problem: Long 911 call-to-defibrillation intervals are common Can provide defibrillation if VF Key to effectiveness of this link: Recognition of early warning signs such as chest pain develops and helps stabilize the and shortness of breath so that 911 is called before collapse occurs patient after of resuscitation Early identification of collapse can lead to rapid activation the EMS system, rapid dispatching and arrival of first responders who can bring defibrillation and ACLS capabilities to the patients side EARLY RECOGNITION OF MAJOR EMERGENCIES Second Link: Early CPR CORONARY ARTERY DISEASE (CAD) CPR is most effective when started immediately after collapse Clinical Presentation of Angina Pectoris Bystander CPR has been consistently shown to have a significant positive effect on Angina Pectoris a common symptom of survival a transient pain or discomfort caused Bystander CPR is the best treatment that CAD; a cardiac arrest patient can receive until the by an inadequate blood flow and oxygen arrival of defibrillation and ACLS care delivery to the heart muscle
Third Link: Early Defibrillation
Character: Described as crushing, pressing, constricting, oppressive, or heavy Location: Located behind sternum or throughout front of chest; may radiate to shoulders, arms, neck, jaw, back of chest and upper abdomen Duration: Steady discomfort, usually lasting <15 minutes
muscle is deprived of blood flow and oxygen for a prolonged period (usually more than 20-30 minutes) and the muscle begins to die
Character, location and duration of chest pain or discomfort is similar to angina; usually described as more intense, however, this is not universal Other Accompanying Signs or Symptoms Sweating, nausea, vomiting, shortness of breath or weakness.
Provoking Factors: Any factor that increases myocardial oxygen demand beyond available supply, such as increased heart rate and increased blood pressure Relieving Factors: Reversal of provoking factors Rest Nitroglycerin
Provoking Factors Most episodes occur at rest or with modest daily activity Heavy physical exertion (occurs infrequently) Other factors include emotional stress and illicit drug use (i.e., cocaine) Relieving Factors Not usually relieved with rest and/or nitroglycerin A victim's most common reaction to a heart attack is denial.
Unstable Angina Atypical Presentations of CAD Women, the elderly, and diabetic patients may have severe CAD but present without classic signs and symptoms Symptoms of weakness, shortness of breath, syncope, or light headedness may be the only symptoms in diabetic patients
Actions for Survival (According to American Heart Association)
Clinical Presentation of AMI (or Heart Attack) AMI occurs when an area of the heart
Person with unknown CAD Recognize the signals of a heart attack Stop activity and sit or lie down Wait about 5 minutes to see if the symptoms go away If pain persists, activate EMS If no EMS available, take victim to the nearest 24-hr hospital emergency department.
Directly caused by ventricular fibrillation, which results in the lack of an effective heart beat Best chance for survival: early CPR and early defibrillation
RISK FACTORS AND PRUDENT HEART LIVING Risk Factors of CAD Factors that cannot be changed:
Person with known CAD (using nitroglycerin): Recognize the signals of a heart attack Stop activity and sit or lie down Take 1 nitroglycerin tablet at a time at 3-5 minute intervals (maximum 3 tablets) If pain persists, activate EMS If no EMS available, take victim to the nearest 24-hr hospital emergency department.
Heredity Male gender Race
Factors that can be changed: Cigarette smoking High blood pressure High blood cholesterol levels Physical inactivity Diabetes Obesity Excessive Stress
Prudent Heart Living Sudden Cardiac Death (Cardiac Arrest) Sudden Death occurs when the heart stops beating and breathing ceases abruptly or unexpectedly Weight control Physical fitness Sensible dietary habits Avoidance of cigarette smoking Reduction of cholesterol and triglycerides in diet Control of high blood pressure Control of Diabetes Eliminate obesity
May occur as the initial and only manifestation of CAD Most commonly occurs within one or two hours after the onset of a heart attack Most common cause is CAD
CEREBROVASCULAR DISEASE
Stroke The third leading cause of death in the U.S. Caused by occlusion (ischemic stroke) or rupture (hemorrhagic stroke) of a blood vessel Transient ischemic attack (TIA) produces signs identical to those of a stroke, but they last only a few minutes; indicates a future risk of stroke Early detection of signs and symptoms, rapid transport and hospital triage is necessary in order to initiate timely therapies
the body Loss of speech, slurred or incoherent speech Unexplained dizziness, unsteadiness or sudden falls Dimness or loss of vision, particularly in one eye Altered level of consciousness Unusually severe or sudden intense headache
New Therapies Effective in restoring blood flow and oxygen to the brain May improve outcome and limit neurological insult To be effective, they must be initiated within 3 hours of the onset of the stroke symptoms
General Emergency Therapy Maintain airway patency Basic airway maneuvers, airway adjuncts and suction may be necessary Endotracheal intubation if basic airway maneuvers are unsuccessful Positive-pressure ventilation if inadequate respirations or respiratory arrest Monitor patient for seizures and treat appropriately
CARDIOPULMONARY RESUSCITATION Indications for CPR Cardiac arrest Respiratory arrest Only exceptions: L.A. County Reference #814 Determination/Pronouncement of Death in the Field L.A. County Reference #815 Honoring Prehospital Do-Not-Resuscitate (DNR) Orders
Risk Factors Specific to Stroke Transient ischemic attacks (TIAs) High red blood cell count Heart disease Chain of Survival and Recovery Early recognition and activation of EMS EMS response, treatment and transport Notification of stroke center Early emergency department care Signs of Stroke or TIA Sudden weakness or numbness of the face, arm or leg on one side of
Use of Automated External Defibrillator (AED)
AEDs are considered an important and lifesaving addition to BLS AEDs are included in the sequence of BLS (to be taught in a separate lecture)
Recovery Position Used if victim unresponsive, but breathing with signs of circulation A modified lateral position used to prevent the airway from being obstructed by the tongue, mucus or vomitus Provide Rescue Breathing Required if breathing is absent or inadequate Give 2 slow breaths using the lowest tidal volume sufficient to make the chest rise: Adult: Over 2 seconds Child & Infant: Over 1 1 seconds
The Sequence of BLS Establish Unresponsiveness If head or neck trauma suspected, limit movement or logroll **If no response, activate EMS system by phoning 911 or other emergency response number **Activate EMS system Adult: After determining the victim is unresponsive, exceptionneardrowning, traumatic arrests, & drug overdoses (activate EMS after 1 minute of CPR) Child & Infant: Not done until after 1 minute of CPR, exceptionchildren known to be high risk for cardiac arrest (activate EMS immediately after collapse)
Rescue Breathing Techniques: Mouth-to-Mouth Mouth-to-Nose Mouth-to-Stoma Mouth-to-Barrier Mouth-to-Face Shield Mouth-to Mask * Bag-mask device * *If oxygen available, use smaller tidal volumes over 1-2 seconds. If no oxygen available, use slighter higher tidal volumes over 2 seconds. May use the lateral or cephalic techniques.
Open Airway Victim should be supine Open airway with head tilt-chin lift maneuver Use jaw-thrust maneuver if head or neck trauma suspected Assess Breathing (10 seconds) Look for chest rise and fall Listen for air escaping during exhalation Feel for the flow of air
Cricoid Pressure Pressure applied to the victims cricoid cartilage in order to compress the esophagus between the trachea and the spine; effective in preventing gastric inflation Assess for Circulation (10 seconds) Adult & Child: Palpate carotid pulse
Infant: Palpate brachial pulse If pulse present but no breathing, provide rescue breathing at a rate of: Adult - 1 breath every 4-5 seconds (or 10-12/minute) Child & Infant 1 breath every 3 seconds (or 20/minute)
of breathing and circulation Child & Infant: Perform 20 cycles of 5 compressions and 1 ventilation, activate EMS, then recheck for signs of breathing and circulation Reassessment (10 seconds) Should be performed after the first minute of CPR and every few minutes thereafter If no pulse, resume CPR beginning with chest compressions If pulse and breathing present, place in recovery position If pulse present but no breathing, provide rescue breathing: Adult - 1 breath every 4-5 seconds (or 10-12/minute) Child & Infant 1 breath every 3 seconds (or 20/minute) 2-Rescuer CPR Refer to skills sheet Monitoring the Effectiveness of CPR Chest rise with ventilation Carotid or brachial pulse with compression Complications of CPR Rib fractures Gastric inflation, with or without regurgitation Lacerated spleen and liver Fractured sternum Pneumothorax Hemothorax Lung contusion Fat emboli Minimizing Complications Some of the complications may be minimized by performing CPR
Chest Compressions Adult: Required if no pulse present Child & Infant: Required if no pulse present or HR less than 60 bpm Compression Rate: Adult, Child, & Infant 100/min Compression to Ventilation Ratio: Adult 1- and 2-rescuer CPR 15:2 Infant and child 1- and 2-rescuer CPR 5:1 Proper Hand Placement Adult: Place hands on the sternum between the nipple line Child: Place heel of one hand over lower half of sternum Infant: Place 2 fingers of one hand one fingers width below the nipple line or two-thumb encircling hands technique over the lower half of sternum Depth of Compression Adult: 1 - 2 inches or enough to generate a pulse Child & Infant: 1/3 the depth of the chest or enough to generate a pulse
Adult: Perform 4 complete cycles 15 compressions and 2 ventilations, then recheck for signs
properly, such as using proper hand placement, however, they cannot be entirely prevented Gastric inflation can be minimized by maintaining an open airway and limiting ventilation volumes to the point at which the chest rises adequately
Submersion Burns Firearm injuries
Injury Prevention Injury is the leading cause of death in children and young adults Prevention of these injuries would substantially reduce childhood deaths and disability
Unique Situations CPR should not be interrupted except for endotracheal intubation, when AED being applied/used, or transporting problems Interruptions, if necessary, should be brief and must be avoided if possible If the rescuer is alone, a momentary delay may be necessary to activate EMS CARDIOPULMONARY ARREST IN INFANTS AND CHILDREN
Cardiac arrest in children typically represents the terminal event of progressive shock or respiratory failure Common Causes Injuries Foreign-body airway obstruction Smoke inhalation Sudden infant death syndrome (SIDS) Poisoning Infections of throat and respiratory tract Congenital heart defect Common Childhood Injuries Motor vehicle injuries Pedestrian Injuries Bicycle injuries
SIDS Prevention SIDS typically occurs in infants 1 month to 1 year Increased risks associated with many factors including: prone sleeping position, the winter months, lower family income, males, siblings of SIDS victims To reduce the risk of SIDS: Place infants supine when sleeping Infants placed on their side should be supported to keep them from rolling to the prone position Do not place infants on soft surfaces to sleep FOREIGN BODY AIRWAY OBSTRUCTION Causes of obstruction Common causes: Adults Food, especially meat Attempting to swallow poorly chewed food associated with high blood alcohol levels and dentures Children Toys Balloons Small objects Food (hot dogs, nuts, candies, grapes)
Signs and Symptoms of Obstruction Partial Airway Obstruction Universal distress signal Good air exchange - forceful cough, may have wheezing between coughs Poor air exchange - weak, ineffective cough, high-pitched sounds, increased respiratory difficulty and possibly cyanosis Complete Airway Obstruction Universal distress signal Unable to speak, breathe or cough Progresses to unconsciousness Cyanosis Management of Partial Airway Obstructed Good air exchange - encourage patient to continue coughing until condition progresses to poor air exchange or complete airway obstruction Poor air exchange - manage like complete airway obstruction
object and remove-blind finger sweep permitted Attempt to ventilate Repeat entire sequence
Chest thrusts are recommended for patients in advanced pregnancy or those who are markedly obese
Child
Conscious Child Abdominal thrusts, repeat multiple times as necessary Unconscious Child Attempt to ventilate, if unsuccessful, reposition head and reattempt 5 abdominal thrusts Attempt to visualize foreign object and remove - NO blind finger sweeps Attempt to ventilate Repeat entire sequence
Management of Complete Airway Obstruction (Refer to AHA's BLS Performance Sheets for the following) Adult
Infant
Conscious Infant 5 back blows and 5 chest thrusts, repeat series until successful Unconscious Infant Attempt to ventilate, if unsuccessful reposition head and reattempt 5 back blows and 5 chest thrusts Attempt to visualize foreign object and remove - NO blind finger sweeps
Conscious Adult Abdominal thrusts, repeat multiple times as necessary Unconscious Adult Attempt to ventilate, if unsuccessful, reposition head and reattempt 5 abdominal thrusts Attempt to visualize foreign
Attempts and reattempts to ventilate Repeat entire sequence until successful
Adult Ratio
Note: Managing FBAO for victims who are initially conscious and then become unconscious follow a different sequence. Refer to skills sheet. AHA'S GUIDELINES FOR BLS BREATHING AGE VENTS/MIN DURATIO N Adult 10-12/min 1-2 sec/br eath Child 20/min 1-1 sec/br eath Infant 20/min 1-1 sec/br eath CPR
15:2 (One- and tworescuer) Rate 100/min Depth 1-2 inches to generate a palpable pulse Hand Placement Hands on sternum between the nipple line Child (1-8 years) Ratio Rate Depth
5:1 100/min 1/3-1/2 depth of chest to generate a palpable pulse Hand Placement Heel of one hand over lower of sternum Infant (less than 1 year) Ratio 5:1 Rate at least 100/min Depth 1/3-1/2 depth of chest to generate a palpable pulse Hand Placement 2 fingers one fingers width below the nipple line; or 2 thumbs encircling hands technique RECOVERY POSITION Roll patient laterally to prevent aspiration only if trauma not suspected EMS ACTIVATION Age Over 8 years Activate EMS after assessing unresponsive ness Up to 8 years Activate EMS after 1 min of CPR Note: There are exceptions to this guideline.
You might also like
- First AidDocument26 pagesFirst Aidmih abdouNo ratings yet
- Pocus Med SchoolDocument7 pagesPocus Med SchoolMarco FioreNo ratings yet
- Cleftlipandpalate 111008125422 Phpapp02Document81 pagesCleftlipandpalate 111008125422 Phpapp02samira fatimaNo ratings yet
- Cardiac Emergencies GuideDocument49 pagesCardiac Emergencies Guideraman kumari100% (3)
- ACLS Code Blue Checklist FormDocument8 pagesACLS Code Blue Checklist FormAnastasya Gishella RorongNo ratings yet
- How To Do CPR On An AdultDocument25 pagesHow To Do CPR On An AdultabNo ratings yet
- Case Study-Uterine MyomaDocument5 pagesCase Study-Uterine MyomaEunice Kristia Esteleydes67% (3)
- Midfacial Fracture TreatmentDocument31 pagesMidfacial Fracture TreatmentRizka UtamiNo ratings yet
- Liabilities of HospitalsDocument8 pagesLiabilities of HospitalsRem Alfelor100% (1)
- Combat Life Saver Module 1: OverviewDocument14 pagesCombat Life Saver Module 1: Overviewsrtmedic100% (2)
- Applying A Two-Piece Cervical CollarDocument31 pagesApplying A Two-Piece Cervical CollarAbigail Filio MongeNo ratings yet
- Kompartemen SindromDocument9 pagesKompartemen SindromPutri PratiwiNo ratings yet
- Perioperative Management 1203114432600412 4Document53 pagesPerioperative Management 1203114432600412 4polushkyNo ratings yet
- First Aid: 15 Minutes Presentation at Ald Ersgate CollegeDocument19 pagesFirst Aid: 15 Minutes Presentation at Ald Ersgate CollegeEmmanuel John Dela CruzNo ratings yet
- Kuliah ATLSDocument63 pagesKuliah ATLSDwianggriany Adhetia Piesca Widoretno100% (1)
- Cleft LectDocument76 pagesCleft LectDiandra Puspa WidyasariNo ratings yet
- Hartmann's Procedure: Patient Information - General SurgeryDocument7 pagesHartmann's Procedure: Patient Information - General SurgeryputriNo ratings yet
- American Stroke AssociationDocument1 pageAmerican Stroke AssociationritadoloksaribuNo ratings yet
- Tenosynovitis Treatment and DiagnosisDocument32 pagesTenosynovitis Treatment and DiagnosissultantraNo ratings yet
- WHO Analgesic LadderDocument1 pageWHO Analgesic LadderJhop SantosNo ratings yet
- Basic and Special Suturing Techniques in Surgery. Honlap 2Document57 pagesBasic and Special Suturing Techniques in Surgery. Honlap 2Arif Nurhidayat PrawirohardjoNo ratings yet
- Jurnal Tyroid PDFDocument3 pagesJurnal Tyroid PDFVinnaNo ratings yet
- Disaste Preparedness and ResponseDocument4 pagesDisaste Preparedness and ResponseMuhammad ShahzadNo ratings yet
- AbscessDocument40 pagesAbscessMehlaqaNo ratings yet
- OXYGEN THERAPY OPTIONS FOR RESPIRATORY DISTRESSDocument16 pagesOXYGEN THERAPY OPTIONS FOR RESPIRATORY DISTRESSkpsuanNo ratings yet
- Lower Respiratory Tract InfectionDocument6 pagesLower Respiratory Tract InfectionFlorence De ChavezNo ratings yet
- Wound HealingDocument62 pagesWound HealingRisPerdanaNo ratings yet
- Bleeding Control Basic Instructor GuideDocument3 pagesBleeding Control Basic Instructor GuideAndres ValenciaNo ratings yet
- Odontogenic Keratocyst: - Jayalakshmi Preetha Meyyanathan CRIDocument48 pagesOdontogenic Keratocyst: - Jayalakshmi Preetha Meyyanathan CRIJayalakshmi PreethaNo ratings yet
- Coronectomy: Indications, Outcomes, and Description of TechniqueDocument6 pagesCoronectomy: Indications, Outcomes, and Description of TechniqueHélio FonteneleNo ratings yet
- Dr. Mirza Koeshardiandi ABC of BurnDocument35 pagesDr. Mirza Koeshardiandi ABC of Burnagus susantoNo ratings yet
- Oral Submucous FibrosisDocument5 pagesOral Submucous Fibrosiskunnuve5005100% (1)
- Presentation 1Document25 pagesPresentation 1Nihar ShahNo ratings yet
- Dr. Kiki Update On DCR and DCSDocument39 pagesDr. Kiki Update On DCR and DCSRsud Malinau Ppk Blud100% (1)
- Dental management medically compromisedDocument86 pagesDental management medically compromisedDiki HedrianNo ratings yet
- Indikasi ReplantasiDocument6 pagesIndikasi ReplantasiAngga Restu Pray YouGoNo ratings yet
- Shield UlcerDocument9 pagesShield UlcerAllen SallyNo ratings yet
- Partial Removable Dental Prosthesis GuideDocument37 pagesPartial Removable Dental Prosthesis Guidesarah0% (1)
- Suctioning Techniques and ProceduresDocument28 pagesSuctioning Techniques and ProceduresMJ DacerNo ratings yet
- Medical Emergency in DentistryDocument42 pagesMedical Emergency in Dentistrywaseem quazi100% (3)
- Access PortacathDocument3 pagesAccess Portacathbrigette_lagatNo ratings yet
- Klasifikasi Impaksi Caninus Rahang Atas Pada Pemeriksaan Radiograf Panoramik Dan CBCT Sebagai Penunjang OdontomyDocument8 pagesKlasifikasi Impaksi Caninus Rahang Atas Pada Pemeriksaan Radiograf Panoramik Dan CBCT Sebagai Penunjang OdontomyRahmi WastriNo ratings yet
- Lefort 1 OsteotomyDocument36 pagesLefort 1 OsteotomyNidhi Jayan100% (2)
- Arch Bar and Ernst Ligature for Mandibular Fracture FixationDocument28 pagesArch Bar and Ernst Ligature for Mandibular Fracture FixationFachrul Latif DentistNo ratings yet
- Emergency Management of Chemical BurnsDocument3 pagesEmergency Management of Chemical Burnsnaufal12345No ratings yet
- Infeksi NosokomialDocument29 pagesInfeksi NosokomialAlunaficha Melody KiraniaNo ratings yet
- Nasal Obstruction and Septoplasty Effectiveness ScaleDocument2 pagesNasal Obstruction and Septoplasty Effectiveness ScaleAfroghitaNo ratings yet
- Introduction To Anesthesia: Dr. Kyat Sidharta, SP AnDocument11 pagesIntroduction To Anesthesia: Dr. Kyat Sidharta, SP AnRiyan AndikaNo ratings yet
- Ranula - A Case ReportDocument2 pagesRanula - A Case Reportnnmey20100% (1)
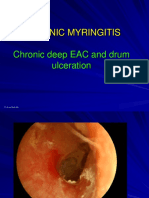
- 3 Chronic MyringitisDocument19 pages3 Chronic MyringitissyahputriNo ratings yet
- Definisi NyeriDocument10 pagesDefinisi NyeriDaniel ZaputraNo ratings yet
- Wound Healing: Santos, Patrick John S., MD First Year Resident Department of Surgery Manila MedDocument60 pagesWound Healing: Santos, Patrick John S., MD First Year Resident Department of Surgery Manila MedJhessie ChingNo ratings yet
- Anatomical LandmarkDocument5 pagesAnatomical Landmarkbagas sitinjakNo ratings yet
- AtelektasisDocument15 pagesAtelektasisMuhammad Ade RahmanNo ratings yet
- Cleft Lip and PalateDocument54 pagesCleft Lip and PalatewidodoNo ratings yet
- Mechanics of Mandibular Movement: OlehDocument44 pagesMechanics of Mandibular Movement: Olehgaluh dharmapatniNo ratings yet
- Rhinosinusitis: Diagnosis and ManagementDocument40 pagesRhinosinusitis: Diagnosis and ManagementMuthia Khanza AbuBakarNo ratings yet
- Anatomi Saraf PeriferDocument57 pagesAnatomi Saraf PeriferErreli K. KhusumawerdanieNo ratings yet
- Jurnal SinusitisDocument25 pagesJurnal SinusitisDwi Ayu NovianaNo ratings yet
- Hanifin and Rajka Diagnostic Criteria For Atopic DermatitisDocument3 pagesHanifin and Rajka Diagnostic Criteria For Atopic DermatitisAlief LeisyahNo ratings yet
- Orthodontic Treatment of Inverted Impacted ToothDocument7 pagesOrthodontic Treatment of Inverted Impacted ToothNiTa DöéMy HarDianaNo ratings yet
- Jurnal TracheostomyDocument17 pagesJurnal TracheostomyLora Angraeni PatodingNo ratings yet
- Smoking Habits and Alcohol Consumption in Patients Diagnosed With Oral Lichen Planus: A Case ReportDocument17 pagesSmoking Habits and Alcohol Consumption in Patients Diagnosed With Oral Lichen Planus: A Case ReportkuntumNo ratings yet
- Modul Utama OtologiDocument21 pagesModul Utama OtologikobexNo ratings yet
- DEHIDRASIDocument7 pagesDEHIDRASISyaqiq balkhy AlwanyNo ratings yet
- Guidelines for Resuscitation of Sepsis: Early Goals-Directed Therapy (EGDTDocument8 pagesGuidelines for Resuscitation of Sepsis: Early Goals-Directed Therapy (EGDTsiti fatmalaNo ratings yet
- Nonkeratinized Oral Mucosa StructureDocument26 pagesNonkeratinized Oral Mucosa StructureShahid EquabalNo ratings yet
- Tugas Jurnal MucoceleDocument7 pagesTugas Jurnal MucoceleshiroemondewaNo ratings yet
- Tehnik A Dan AntisepsisDocument30 pagesTehnik A Dan AntisepsisRyandika Aldilla NugrahaNo ratings yet
- Kanker MulutDocument2 pagesKanker MulutHamba AllahNo ratings yet
- Kista Jaringan Lunak MulutDocument36 pagesKista Jaringan Lunak MulutAndria FadliNo ratings yet
- Causes and Treatment of ChylothoraxDocument8 pagesCauses and Treatment of ChylothoraxMaral Bimanti FebrilinaNo ratings yet
- Metastasis Bone DiseaseDocument11 pagesMetastasis Bone DiseasedrkurniatiNo ratings yet
- BLS Healthcare Provider GuideDocument17 pagesBLS Healthcare Provider GuideBlanche Cleo MayorNo ratings yet
- Pork CalderetaDocument1 pagePork CalderetaFlorence De ChavezNo ratings yet
- Chicken AfritadaDocument1 pageChicken AfritadaFlorence De ChavezNo ratings yet
- United Kingdom PM & CabinetDocument30 pagesUnited Kingdom PM & CabinetFlorence De ChavezNo ratings yet
- Nursing Care of a Patient with Uterine FibroidsDocument37 pagesNursing Care of a Patient with Uterine FibroidsFlorence De ChavezNo ratings yet
- Mam BascoDocument2 pagesMam BascoFlorence De ChavezNo ratings yet
- FROOOONTDocument40 pagesFROOOONTFlorence De ChavezNo ratings yet
- Validation of The Wong-Baker FACES PainDocument5 pagesValidation of The Wong-Baker FACES PainArsya WinaNo ratings yet
- BLS Book (New)Document7 pagesBLS Book (New)Saman FirdousNo ratings yet
- Ensuring Timely Emergency Care for All Through Universal Health CoverageDocument5 pagesEnsuring Timely Emergency Care for All Through Universal Health CoverageJPNo ratings yet
- Daftar PustakaDocument2 pagesDaftar PustakaGenio OscarNo ratings yet
- Andhika Pangestu CVDocument6 pagesAndhika Pangestu CVPangestu DhikaNo ratings yet
- The Nordic Emergency Medical Services 2018Document61 pagesThe Nordic Emergency Medical Services 2018Angel ArreolaNo ratings yet
- Advanced Trauma Life SupportDocument4 pagesAdvanced Trauma Life SupportMd Ahsanuzzaman PinkuNo ratings yet
- Assess Appropriateness For Clinical Condition. Heart Rate Typically 50/min If BradyarrhythmiaDocument1 pageAssess Appropriateness For Clinical Condition. Heart Rate Typically 50/min If BradyarrhythmiaatikaNo ratings yet
- Dieckmann Et Al The PAT 1 PDFDocument4 pagesDieckmann Et Al The PAT 1 PDFLydia ElimNo ratings yet
- Burns: Assistent Professor Kenan KaravdićDocument86 pagesBurns: Assistent Professor Kenan KaravdićNudžejma KadrićNo ratings yet
- Management of Maxillofacial Trauma in Emergency An Update of Challenges and ControversiesDocument17 pagesManagement of Maxillofacial Trauma in Emergency An Update of Challenges and ControversiesHelna AmeliaNo ratings yet
- EuSEM Policy StatementDocument2 pagesEuSEM Policy Statementapi-3726545No ratings yet
- 2023 FHS PG HandbookDocument625 pages2023 FHS PG HandbookAbdullahi A. KNo ratings yet
- Active Surgical Oncology Physician Assistant PA Resume SW Houston TXDocument3 pagesActive Surgical Oncology Physician Assistant PA Resume SW Houston TXRick Whitley100% (1)
- Referência Bibliográfica Trauma CraniofacialDocument2 pagesReferência Bibliográfica Trauma CraniofacialSamira FreitasNo ratings yet
- Als Protocol Dec 2023 FinalDocument84 pagesAls Protocol Dec 2023 FinalRobert MccallumNo ratings yet
- Clinical Practice Procedures:: Trauma/Cervical CollarDocument3 pagesClinical Practice Procedures:: Trauma/Cervical CollardesytrilistyoatiNo ratings yet
- Talal Mohammad Bakheet: Work ExperienceDocument3 pagesTalal Mohammad Bakheet: Work ExperienceOdai BakhetNo ratings yet