Professional Documents
Culture Documents
DM Per
Uploaded by
Emine AlaaddinogluOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
DM Per
Uploaded by
Emine AlaaddinogluCopyright:
Available Formats
J Periodontol 2013;84(4 Suppl.):S106-S112 doi:10.1902/jop.2013.
1340011
Diabetes and periodontal diseases: consensus report of the Joint EFP/AAP Workshop on Periodontitis and Systemic Diseases
Chapple ILC, Genco R, and on behalf of working group 2 of the joint EFP/AAP workshop. Diabetes and periodontal diseases: consensus report of the Joint EFP/ AAP Workshop on Periodontitis and Systemic Diseases.
Iain L. C. Chapple1, Robert Genco2 and on behalf of working group 2 of the joint EFP/AAP workshop*
1 Periodontal Research Group & MRC Centre for Immune Regulation, University of Birmingham School of Dentistry, Birmingham, UK; 2University at Buffalo, Oral Biology and Microbiology and Immunology, Buffalo, NY, USA
Abstract Background: Diabetes and periodontitis are complex chronic diseases with an established bidirectional relationship. There is long-established evidence that hyperglycaemia in diabetes is associated with adverse periodontal outcomes. However, given the ubiquity of periodontal diseases and the emerging global diabetes epidemic, the complications of which contribute to signicant morbidity and premature mortality, it is timely to review the role of periodontitis in diabetes. Aims: To report the epidemiological evidence from cross-sectional, prospective and intervention studies for the impact of periodontal disease on diabetes incidence, control and complications and to identify potential underpinning mechanisms. Epidemiology: Over the last 20 years, consistent and robust evidence has emerged that severe periodontitis adversely affects glycaemic control in diabetes and glycaemia in non-diabetes subjects. In diabetes patients, there is a direct and dose-dependent relationship between periodontitis severity and diabetes complications. Emerging evidence supports an increased risk for diabetes onset in patients with severe periodontitis. Biological mechanisms: Type 2 diabetes is preceded by systemic inammation, leading to reduced pancreatic b-cell function, apoptosis and insulin resistance. Increasing evidence supports elevated systemic inammation (acute-phase and oxidative stress biomarkers) resulting from the entry of periodontal organisms and their virulence factors into the circulation, providing biological plausibility for the effects of periodontitis on diabetes. AGE (Advanced Glycation Endproducts) RAGE (Receptor for AGEs) interactions and oxidative-stress-mediated pathways provide plausible mechanistic links in the diabetes to periodontitis direction. Interventions: Randomized controlled trials (RCTs) consistently demonstrate that mechanical periodontal therapy associates with approximately a 0.4% reduction in HbA1C at 3 months, a clinical impact equivalent to adding a second drug to a pharmacological regime for diabetes. RCTs are needed with larger numbers of subjects and longer term follow-up, and if results are substantiated, adjunctive periodontal therapies subsequently need to be evaluated. There is no current evidence to support adjunctive use of antimicrobials for periodontal management of diabetes patients. Guidelines: Given the current evidence, it is timely to provide guidelines for periodontal care in diabetes patients for medical and dental professionals and recommendations for patients/the public.
Key words: association; complications; diabetes mellitus; gestational diabetes; HbA1C; incident; intervention; mechanisms; periodontal disease; periodontitis; type 2 diabetes Accepted for publication 14 November 2012 The proceedings of the workshop were jointly and simultaneously published in the Journal of Clinical Periodontology and Journal of Periodontology.
S106
2013 European Federation of Periodontology and American Academy of Periodontology
Diabetes and periodontitis
Conict of interest and source of funding
S107
Group participants declare no conict of interest. The workshop was funded by an unrestricted educational grant from ColgatePalmolive to the European Federation of Periodontology and the American Academy of Periodontology. *Working group participants: Tord Berglundh, Sweden; Peter Eickholz, Germany; Steven Engebretson, USA; Dana Graves, USA; Sarah Grossi, USA; Hatice Hasturk, USA; Thomas Kocher, Germany; Evanthia Lalla, USA; Ira Lamster, USA; Niklaus Lang, China; Brian Mealey, USA; Joerg Meyle, Germany; Willem Nesse, The Netherlands; David Paquette, USA; Philip Preshaw, UK; George Taylor, USA; John Taylor, UK; Ubele Van der Velden, The Netherlands; Clemens Walter, Switzerland; Borgnakke Wenstalo, Finland. che, USA; Pekka Ylo
Diabetes and Periodontitis
Diabetes mellitus is emerging as a global epidemic, whose complications impact signicantly on quality of life, longevity and healthcare costs. It is estimated that 346 million people currently suffer from diabetes worldwide and the World Health Organization (WHO) predicts that this will increase to 439 million, almost 10% of adults, by 2030 (WHO 2011). The escalating human and economic burden across both the developed and developing world necessitates a multidisciplinary approach, including adjunctive measures to managing diabetes and its complications. The onset of diabetes is preceded by inammation, which leads to pancreatic beta-cell dysfunction and apoptosis, as well as impacting on the development of insulin resistance and ultimately diabetes. It is logical that comorbidities that contribute to systemic inammation are likely to increase the risk of developing diabetes, and impact on diabetes control and the development of diabetes complications, ulti-
mately affecting diabetes-associated morbidity and mortality. Inammatory periodontal diseases are the most common chronic inammatory conditions of humans worldwide. The destructive form of periodontal disease, periodontitis, affects approximately 50% of adults and over 60% of over 65 year olds, with severe periodontitis impacting 1015% of populations. Periodontal disease is a microbially initiated chronic inammatory disease, in which dysregulated immune-inammatory processes are responsible for the majority of host tissue destruction, and ultimately tooth loss. There is increasing evidence that systemic inammation results from the entry of oral microbial agents and their virulence factors into the circulation. This is evidenced by elevated serum levels of C-reactive protein and other acute-phase reactants and raised biomarkers of oxidative stress. It is therefore biologically plausible that non-resolving chronic inammation derived from periodontal disease impacts on diabetes control (elevated HbA1C) and complica-
tions, as well as beta-cell function, insulin resistance and development of type 2 diabetes. It is well established that hyperglycaemia affects periodontal outcomes. A body of evidence, predominantly over the last 15 20 years supports signicant independent associations between periodontal inammation and glycaemic status (even in individuals without diabetes), and complications of diabetes. There is also emerging evidence for an independent association between periodontitis and incident diabetes. In addition, there is evidence that periodontitis adversely affects diabetes glycaemic control and worsens complications. There is a lack of clarity in the literature regarding the strength of the latter association and the clinical signicance of the effects of periodontal therapy on diabetes and its outcomes. Therefore, it is timely to systematically review the literature on epidemiology of periodontal diseases and diabetes; the impact of periodontal interventions on diabetes outcomes and; potential mechanistic links between these two chronic
2013 European Federation of Periodontology and American Academy of Periodontology
S108
Chapple and Genco
odontitis is associated with increased risk for macroalbuminuria, end-stage renal disease, calcication of atherosclerotic plaques, carotid intimamedial thickness and cardio-renal mortality. Limited evidence exists for an association between periodontal disease and diabetes complications in adults with long-duration insulindependent diabetes mellitus. Incidence Emerging evidence suggests an increased risk for the development of diabetes in individuals with severe periodontitis, relative to no or mild periodontitis after adjustment for potential confounders.
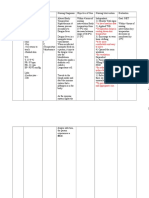
Is there a type and/or threshold of periodontal disease that is associated with increased risk of diabetes complications? Summary
inammatory diseases, consistent with examining biological plausibility. The remit of this working group was to critically examine the current evidence base for the periodontal diseasediabetes paradigm with a view to establishing pragmatic guidelines for patient care, accepting the current state of the eld and the likely need for change as further research emerges. Two reviews have evaluated in a systematic manner the epidemiological evidence for directional associations between periodontal diseases and diabetes stalo, Taylor & (Borgnakke, Yio Genco 2013) and the evidence for benecial effects of periodontal treatment on diabetes outcomes (Engebretson & Kocher 2013). A third narrative review has critically addressed potential mechanistic links between periodontal diseases and diabetes (Taylor, Preshaw & Lalla 2013). While there is only emerging evidence for associations between periodontal disease and type 1 diabetes, and little evidence for the association between periodontitis and gestational diabetes, these elds were excluded from detailed analysis. Therefore, this consensus document focuses specically on the relationship between periodontitis and type 2 diabetes.
Epidemiological Evidence (for type 2 diabetes)
What is the evidence for the effect of periodontal disease on diabetes control, complications and incidence?
Overall, there is consistent and robust evidence that severe periodontitis, adversely affects blood glucose levels expressed as HbA1C in individuals with and without diabetes. Moderate-to-severe periodontitis is associated with an increased risk for the development of diabetes. Evidence supports a dose-dependent role for periodontitis and diabetes complications.
Impact of Periodontal Treatment on Diabetes Outcomes
What is the potential impact of periodontal treatment on diabetes outcomes and what is the clinical signicance of any effect?
Diabetes control and hyperglycaemia Severe periodontitis is associated with increased HbA1C in individuals with and without type 2 diabetes. In people without diabetes, progression of periodontitis over 510 years was associated with increasing HbA1C and impaired glucose tolerance. Those with periodontitis at baseline and demonstrating periodontal disease progression had a larger HbA1C increase than those without periodontitis over a 5-year period (0.143% versus 0.005%). Diabetes complications There is evidence for a direct tionship between the severity of odontitis and complications of 2 diabetes. Moderate-to-severe relaperitype peri-
Studies do not address the issue of a minimal threshold level of periodontal disease at which an effect on risk of complications is likely. Considering the available evidence, subjects with gingivitis are often combined with periodontally healthy subjects in the control/reference group. In one study where subjects with gingivitis was a separate category, there was no evidence that gingivitis was associated with altered glycaemia. Although the denition of periodontitis differs among studies, a consistent nding is that severe periodontitis imparts a signicant risk for diabetes complications. Again based on these studies, the threshold appears to be in the transition between moderate to severe disease. It has to be realized that threshold levels of periodontal disease affecting individuals with diabetes mellitus may be patient dependent.
Which clinical biochemical markers of diabetes are affected by periodontal diseases?
Reduction in HbA1C is an established outcome measure of successful diabetes treatment. Evidence derived from RCTs shows that periodontal treatment results in a mean reduction in HbA1C of 0.36% (95% CI 0.19, 0.54) at 3 months (Engebretson & Kocher 2013). This result is consistent with previous meta-analyses. Levels of HbA1C reduction obtained within the short term following periodontal interventions are equivalent to those achieved by adding a second drug into a pharmacological regime. If such reductions following periodontal therapy can be sustained over the longer term, then this may contribute to reduced diabetes-associated morbidity and mortality.
What is the specic level of periodontal resolution following periodontal therapy that is associated with improvements in diabetes outcome?
While periodontal therapies result in reduction in HbA1C level, diabetes patients on average benet from periodontal therapy. At present, no specic level of disease resolution has been associated with this outcome (HbA1C reduction).
Is there evidence to recommend a specic periodontal treatment regimen over and above mechanical debridement as being more benecial towards diabetes outcomes?
HbA1C has consistently been used as the measure of glycaemia. Occasionally, fasting or random plasma glucose and oral glucose tolerance tests have also been used. Insulin resistance has been evaluated by the homeostasis model assessment. This consensus report therefore focusses on HbA1C as the outcome measure of diabetes control.
While meta-analyses have included studies that employed a wide range of periodontal therapies, professional mechanical debridement was the
2013 European Federation of Periodontology and American Academy of Periodontology
Diabetes and periodontitis
intervention common to all studies. Adjunctive antibiotic therapy does not currently appear to confer additional benets. Therefore, there is insufcient evidence to suggest a specic periodontal treatment regime and we conclude that individuals with type 2 diabetes benet from professional mechanical debridement in conjunction with sustained effective home care.
Given the current evidence base, how should periodontal care feature in the management of diabetes control?
S109
Periodontal therapy in individuals with type 2 diabetes is safe and effective in improving periodontal clinical outcomes. Available short-term evidence suggests that HbA1C levels can be reduced as a result of periodontal therapy. Additional RCTs are needed to make denitive clinical recommendations for periodontal therapy in the management of diabetes. In the meantime, it would be prudent to identify diabetes within the dental setting. Likewise, in the medical setting, patients with diabetes should be evaluated for the presence of periodontitis.
Mechanistic Links Between Periodontal Diseases and Diabetes
Are the periodontal microbiota affected by diabetes control?
role of specic cytokines in the relationship between diabetes and periodontitis. In patients with periodontitis, diabetes is associated with elevated levels of several cytokines and other mediators in saliva and gingival crevicular uid (GCF). Similar ndings are evident in gingival tissue samples from animal models. There is evidence that periodontitis in non-diabetic individuals increases systemic levels of inammatory mediators. Whether this occurs in diabetic subjects remains to be claried. Findings from animal experiments involving the use of specic antagonists support a cause-andeffect relationship between diabetesrelated cytokine dysregulation and periodontal breakdown. Most studies to date, however, have focused on a limited number of mediators.
What is the role of oxidative stress in the mechanistic association between diabetes and periodontitis?
that have been established in animal experiments. The complex effects of hyperglycaemia and insulin resistance on the many different cell types involved in periodontitis are largely unknown. As clinical evidence emerges for a negative impact of periodontitis on diabetes outcomes, there is an imperative for more mechanistic studies to explain this direction of the association.
Bradford Hill Criteria for Evidence of Causality
Hyperglycaemia enhances oxidative stress in periodontal tissues and clinical and experimental studies have demonstrated that periodontitis promotes measures of systemic oxidative stress. Results from animal experiments indicate that the use of antioxidant micronutrients reduces diabetes-enhanced periodontal inammation and bone loss.
What is the role of AGEs in the mechanistic association between diabetes and periodontitis?
The consensus of this group on the issue of causality is that, while the determination of causality is the ultimate goal, it is not central to considerations of the linkage between complex diseases such as periodontitis and diabetes. Risk factors affect incidence, severity and progression of disease by increasing the probability that these outcomes will occur. It is important to determine whether periodontitis is independently associated with adverse diabetes outcomes. It is also critical to demonstrate the impact of periodontal interventions on adverse diabetes outcomes.
Recommendations for Future Research
According to the currently available literature, there is no compelling evidence that diabetes has any signicant impact on the oral microbiota. A major limitation in current knowledge is that existing studies have not examined the entire periodontal microbiome.
What is the impact of the periodontal microbiota on diabetes outcomes?
Whether the periodontal microbiota has any direct impact on diabetes has barely begun to be addressed and there is currently inadequate evidence to support such an effect.
What is the role of cytokines and other mediators in the mechanistic association between diabetes and periodontitis?
Diabetes drives the formation of AGEs, which directly and indirectly promote inammation, including periodontitis. Findings from clinical studies and animal experiments suggest that AGERAGE interaction leads to the exaggerated inammatory response and periodontal tissue destruction seen in diabetes. Animal experiments using RAGE blockade indicate a mechanistic link between RAGE activation and periodontal breakdown.
What are the limitations to the existing evidence base for periodontitisdiabetes links, in either direction?
A strong evidence base exists from epidemiological studies that periodontitis and diabetes are directly associated, and that periodontal interventions provide benecial effects on diabetes outcomes. However, the evidence could be further strengthened by future studies incorporating the following design features:
There is evidence from clinical and experimental studies to support the
It is timely to conrm in clinical trials mechanisms underlying the impact of diabetes on periodontitis
Randomized, multicentre studies that are properly powered; Development of large cohorts to assess the impact of periodontal disease upon macro- and microvascular complications of diabetes; Inclusion of populations with differing characteristics, such as overweight and obese populations with different distributions of adipose tissue, differing ratios of type 1 and type 2 diabetes, race, ethnicity and geographical location, to improve generalizability; Accounting for periodontal disease denitions that include extent, severity and denitions of cases;
2013 European Federation of Periodontology and American Academy of Periodontology
S110
Chapple and Genco
In association studies, consideration of full-mouth periodontal examinations rather than partial mouth sampling and including probing depth and loss of clinical attachment measurements: these are essential in intervention trials; Characterization of baseline diabetes characteristics additional to HbA1C (e.g. duration of diabetes status). Consistency in the recording of details on general medication use and changes in use in all study volunteers; Consistency with respect to the minimum number of teeth required for subject inclusion; Stratication for relevant major risk factors (i.e. obesity, smoking); Documentation of crossover effects on the control group; Denition of periodontal treatment outcomes deemed to characterize successful periodontal therapy; Development of biobanks for biological samples from clinical studies to facilitate subsequent analysis; The recording of information on nutritional and quality-of-life outcomes; Recording and reporting of information on other oral conditions (e.g. periapical periodontitis).
Assessment of the effects of bacteremia on diabetes control and the effect of diabetes on the development of, and response to bacteremia; Investigation of the potential effects of periodontitis on insulin resistance; Exploration of the potential effects of periodontitis on insulin production; Addressing the complexity of local and systemic regulatory pathways affected by diabetes and periodontitis; Examining the effects of diabetes on cellular functions in periodontitis; Application of longitudinal designs in clinical studies employing metagenomic techniques and systems biology to unravel mechanistic links between diabetes and periodontitis in humans.
Mechanistic studies investigating interactions between diabetes and periodontitis should also take into account duration of diabetes, level of glycaemic control and extent and severity of periodontitis.
Guideline A
With respect to studies designed to assess the impact of periodontal interventions on diabetes outcomes, additional design features include:
Comprehensive assessment of changes in clinical measures of periodontal inammation and in biochemical markers of inammation in blood and saliva; Inclusion of type 1, gestational and other types of diabetes; Further interventional studies investigating the impact of different periodontal treatment and prevention protocols on the onset and progression of diabetes and its complications.
[Suggested Guidelines for physicians and other medical health professions for Use in Diabetes Practice] Oral health of my patients Because of the increased risk for developing periodontitis in patients with diabetes the following recommendations are made:
dental professionals) as part of their ongoing management of diabetes. Even if no periodontitis is diagnosed initially, annual periodontal review is recommended. Diabetes patients presenting with any overt signs and symptoms of periodontitis, including loose teeth not associated with trauma spacing or spreading of the teeth and/or gingival abscesses or gingival suppuration, require prompt periodontal evaluation. Patients with diabetes who have extensive tooth loss should be encouraged to pursue dental rehabilitation to restore adequate mastication for proper nutrition. Oral health education should be provided to all patients with diabetes. For children and adolescents diagnosed with diabetes, annual oral screening is recommended from the age of 67 years by referral to a dental professional. Patients with diabetes should be advised that other oral conditions such as dry mouth and burning mouth may occur, and if so, they should seek advice from their dental practitioner. Also patients with diabetes are at increased risk of oral fungal infections and experience poorer wound healing than those who do not have diabetes.
Guideline B
[Suggested guidelines for use in dental practice] My patient with diabetes
In studies designed to explore mechanistic links between periodontal diseases and diabetes, further consideration should be given to:
Addressing the complexity, pathogenic composition and dynamics of the microbial biolm;
Patients with diabetes should be told that periodontal disease risk is increased by diabetes. They should also be told that if they suffer from periodontal disease, their glycaemic control may be more difcult, and they are at higher risk for diabetic complications such as cardiovascular and kidney disease. As part of their initial evaluation, patients with type 1, type 2 and gestational diabetes (GDM) should receive a thorough oral examination, which includes a comprehensive periodontal examination. For all newly diagnosed type 1 and type 2 diabetes patients, subsequent periodontal examinations should occur (as directed by the
Patients with diabetes should be told that they are at increased risk for periodontitis. They should also be told that if they suffer from periodontal disease, their glycaemic control may be more difcult, and they are at higher risk for other complications such as cardiovascular and kidney disease. Patients presenting with a diagnosis of type 1, type 2 or gestational diabetes should receive a thorough oral examination, which includes a comprehensive periodontal evaluation. If periodontitis is diagnosed, it should be properly managed. If no periodontitis is diagnosed ini-
2013 European Federation of Periodontology and American Academy of Periodontology
Diabetes and periodontitis
tially, patients with diabetes should be placed on a preventive care regime and monitored regularly for periodontal changes. Patients with diabetes presenting with any acute oral/periodontal infections require prompt oral/ periodontal care. Patients with diabetes who have extensive tooth loss should be encouraged to pursue dental rehabilitation to restore adequate mastication for proper nutrition. Oral health education should be provided to all patients with diabetes. Patients with diabetes should also be evaluated for other potential oral complications, including dry mouth, burning mouth and candidal infections. For children and adolescents diagnosed with diabetes, an annual oral screening for early signs of periodontal involvement is recommended starting at the age of 6 years. Patients who present without a diabetes diagnosis, but with obvious risk factors for type 2 diabetes and signs of periodontitis should be informed about their risk for having diabetes, assessed using a chair-side HbA1C test, and/or referred to a physician for appropriate diagnostic testing and follow-up care.
S111
Increasing spaces between your teeth; Calculus (tartar) on your teeth.
If you have noticed any of these problems, it is important to see a dentist as soon as possible. Gum disease may be present and get worse with no apparent symptoms to you, so even if you do not think you have gum disease now, you should still get regular dental check-ups as part of managing your diabetes. Your dentist will be able to pick up early signs of gum disease. You also need to clean your teeth and gums very carefully at home. If you have diabetes, you may also suffer from dry mouth, burning mouth, yeast infections of the mouth or poor healing of mouth wounds. It is important to keep your mouth and your whole body as healthy as possible with regular dental and medical care.
Guideline D
Pus from the gums; Foul taste; Longer looking teeth; Loose teeth; Increasing spaces between your teeth; Calculus (tartar) on your teeth.
Guideline C
[Recommendations for patients with diabetes at the physicians practice/ ofce] Why should I have my gums checked? If your physician has told you that you have diabetes, you should make an appointment with a dentist to have your mouth and gums checked. This is because people with diabetes have a higher chance of getting gum disease. Gum disease can lead to tooth loss and may make your diabetes harder to control. You may have gum disease if you have ever noticed:
Red, bleeding or swollen gums; Pus from the gums; Foul taste; Longer looking teeth; Loose teeth;
[Recommendations for patients at the dental surgery/ofce who have diabetes or are found to be at risk for diabetes] You have diabetes or you have been told by your dentist you are at risk for diabetes People with diabetes have a higher chance of getting gum disease. If you have been told by your dentist that you have gum disease, you should follow up with necessary treatment as advised. This may require several appointments. Like diabetes, gum disease is a chronic condition and requires lifelong maintenance. You also need to clean your teeth and gums very carefully at home. If left untreated, gum disease can lead to tooth loss and may also make your diabetes harder to control. Gum disease may be present and get worse with no apparent symptoms to you, so if your dentist told you that you do not have gum disease now, you should still get regular dental check-ups as part of managing your diabetes. Your dentist will be able to pick up early signs of gum disease. You may have gum disease if you ever notice:
People with diabetes may also suffer from dry mouth, burning mouth, yeast infections of the mouth or poor healing of mouth wounds. If you do not have diabetes, but your dentist identied some risk factors for diabetes including signs of gum disease, it is important to get a medical check-up as advised. Your medical doctor can order blood tests to see if you have diabetes and not know it, and can provide proper advice and care based on the results. Make an appointment to see your medical doctor as soon as possible. And remember to inform your dentist about the outcome of your visit to the medical doctor. It is important to keep your mouth and your whole body as healthy as possible with regular dental and medical care.
References
Borgnakke, W. S., Ylostalo, P. V., Taylor, G. W. & Genco, R. J. (2013) Effect of periodontal disease on diabetes: systematic review of epidemiologic observational evidence. Journal of Clinical Periodontology and Journal of Periodontology 40 (Suppl 14), 135152. Engebretson, S. & Kocher, T. (2013) Evidence that periodontal treatment improves diabetes outcomes: a Systematic Review and Meta-analysis. Journal of Clinical Periodontology and Journal of Periodontology 40 (Suppl 14), 153163. Taylor, J. J., Preshaw, P. M. & Lalla, E. (2013) A review of the evidence for pathogenic mechanisms that may link periodontitis and diabetes. Journal of Clinical Periodontology and Journal of Periodontology 40 (Suppl 14), 113134.. World Health Organization (2011) Fact Sheet No. 312. Diabetes [WWW document]. Available at: http://www.who.int/mediacentre/factsheets/ fs312/en/ [accessed on 23 August 2012].
Red, bleeding or swollen gums;
Address: Iain L. C. Chapple School of Dentistry College of Medical and Dental Sciences The University of Birmingham St Chads Queensway Birmingham, B4 6NN, UK E-mail: i.l.c.chapple@bham.ac.uk
2013 European Federation of Periodontology and American Academy of Periodontology
S112
Chapple and Genco
Clinical Relevance
Scientic rationale for the study: Periodontal disease and diabetes are directly and independently associated chronic diseases of high prevalence in the population. Diabetes is predicted to increase in prevalence in the next 15 years to epidemic levels leading to substantial morbidity and premature mortality. Therefore it is timely to systematically review the impact of periodontitis and its treatment upon diabetes control, complications and incidence.
Principal ndings: Severe periodontitis adversely effects diabetes control (HbA1C) and also glycaemia in nondiabetes patients. There is a direct and dose-dependent relationship between periodontitis severity and diabetes complications in diabetes patients and emerging evidence that severe periodontitis may predispose to the development of diabetes. Mechanistic links between periodontitis and diabetes involve AGERAGE interactions, oxidative stress and altered cytokine networks. Periodontal treatment reduces plasma
HbA1C at 3-months by levels equivalent to adding a second drug to a pharmacological regime. Practical implications: Guidelines are documented for physicians, dental surgeons and patients with diabetes or at risk of diabetes, concerning periodontal care and management of oral health. Larger randomised trials are recommended over extended observation periods to strengthen the evidence for this bidirectional relationship and for the impact of periodontal therapy on diabetes control, complications and incidence.
2013 European Federation of Periodontology and American Academy of Periodontology
You might also like
- The Nexus Between Tooth Decay, Liver Disease and Sugar IntakeDocument154 pagesThe Nexus Between Tooth Decay, Liver Disease and Sugar IntakeEmine Alaaddinoglu100% (2)
- Introduction to Periodontics: Definitions, Anatomy, DiseasesDocument33 pagesIntroduction to Periodontics: Definitions, Anatomy, DiseasesEmine Alaaddinoglu100% (1)
- Owbh PDFDocument55 pagesOwbh PDFEmine AlaaddinogluNo ratings yet
- AbDocument12 pagesAbEmine AlaaddinogluNo ratings yet
- Rfe 311 315 Exam BankDocument9 pagesRfe 311 315 Exam BankEmine AlaaddinogluNo ratings yet
- Etiology and Microbiology of Periodontal DiseasesDocument7 pagesEtiology and Microbiology of Periodontal DiseasesEmine AlaaddinogluNo ratings yet
- 1-s2.0-002239137290193X-maiFixed Partial Dentures and Operative DentistrynDocument4 pages1-s2.0-002239137290193X-maiFixed Partial Dentures and Operative DentistrynEmine AlaaddinogluNo ratings yet
- J DENT RES-2012-Miron-736-44Document10 pagesJ DENT RES-2012-Miron-736-44Emine AlaaddinogluNo ratings yet
- Systemic Medication and The Inflammatory CascadeDocument13 pagesSystemic Medication and The Inflammatory CascadeEmine AlaaddinogluNo ratings yet
- The Periodontal Crown - Creating Healthy TissueDocument5 pagesThe Periodontal Crown - Creating Healthy TissueEmine AlaaddinogluNo ratings yet
- J Dent Res 2012 Papapanou 907 8Document3 pagesJ Dent Res 2012 Papapanou 907 8Emine AlaaddinogluNo ratings yet
- Composition and Development of Oral Bacterial CommunitiesDocument20 pagesComposition and Development of Oral Bacterial CommunitiesEmine AlaaddinogluNo ratings yet
- Cid 1Peri-Implantitis Versus Periodontitis: Functional Differences Indicated by Transcriptome Profiling2001Document11 pagesCid 1Peri-Implantitis Versus Periodontitis: Functional Differences Indicated by Transcriptome Profiling2001Emine AlaaddinogluNo ratings yet
- Introduction To Oral PathogensDocument35 pagesIntroduction To Oral PathogensEmine AlaaddinogluNo ratings yet
- Functional Electrical Stimulation Using Microstimulators To Correct Foot Drop: A Case StudyDocument9 pagesFunctional Electrical Stimulation Using Microstimulators To Correct Foot Drop: A Case StudyEmine AlaaddinogluNo ratings yet
- Antibiotic ResistanceDocument32 pagesAntibiotic ResistanceEmine Alaaddinoglu100% (2)
- Crestal Sinus Lift With Sequential Drills And.20Document1 pageCrestal Sinus Lift With Sequential Drills And.20Emine AlaaddinogluNo ratings yet
- Biofilm Dynamics at The GingivalDocument4 pagesBiofilm Dynamics at The GingivalEmine AlaaddinogluNo ratings yet
- 13 Purpose and Problems of Periodontal Disease ClassificationDocument9 pages13 Purpose and Problems of Periodontal Disease ClassificationEmine AlaaddinogluNo ratings yet
- Periodontal Flap Surgery 2Document45 pagesPeriodontal Flap Surgery 2Emine Alaaddinoglu100% (2)
- Academic Ranking of Turkish Universities January 20101Document35 pagesAcademic Ranking of Turkish Universities January 20101Emine AlaaddinogluNo ratings yet
- Armitage 1999 PDFDocument6 pagesArmitage 1999 PDFnydiacastillom2268No ratings yet
- Topics in Neuromodulation TreatmentDocument200 pagesTopics in Neuromodulation TreatmentJosé Ramírez100% (1)
- 2945979248366223753Document6 pages2945979248366223753Emine AlaaddinogluNo ratings yet
- Bacterial Invasion of Host CellsDocument20 pagesBacterial Invasion of Host CellsEmine AlaaddinogluNo ratings yet
- Anova e PrintDocument3 pagesAnova e PrintEmine AlaaddinogluNo ratings yet
- 3D Finite Element Model and Cervical Lesion Formation inDocument7 pages3D Finite Element Model and Cervical Lesion Formation inEmine AlaaddinogluNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Nursing Care Plan for Headache, Dysarthria, and WeaknessDocument4 pagesNursing Care Plan for Headache, Dysarthria, and WeaknessRawan KhateebNo ratings yet
- Nurse's Study Guide To BurnsDocument14 pagesNurse's Study Guide To BurnsCassie GonzalezNo ratings yet
- (Susan G. Kornstein, Anita H. Clayton) Women's Men (BookFi)Document215 pages(Susan G. Kornstein, Anita H. Clayton) Women's Men (BookFi)Ge Nom100% (1)
- Nhs Forth Valley: Management of Acute Inversion of UterusDocument5 pagesNhs Forth Valley: Management of Acute Inversion of UterusMelissa Aina Mohd YusofNo ratings yet
- PID Treatment and CausesDocument17 pagesPID Treatment and CausesGhaliey AzizNo ratings yet
- Craniotomy Procedure and Post-Op CareDocument23 pagesCraniotomy Procedure and Post-Op CareUmar FarooqNo ratings yet
- Acute Lymphoblastic Leukemia - Ontologies - LabDocument6 pagesAcute Lymphoblastic Leukemia - Ontologies - LabAnusha SaiNo ratings yet
- TahbsoDocument42 pagesTahbsoMarlon RoyoNo ratings yet
- CopdDocument11 pagesCopdpkm bungamasNo ratings yet
- Feldman. Oedipus Complex. Manifestations in The Inner World and Therapeutic SituationDocument26 pagesFeldman. Oedipus Complex. Manifestations in The Inner World and Therapeutic SituationTiberiuNo ratings yet
- Krzywosinski PBLsDocument24 pagesKrzywosinski PBLsleahbayNo ratings yet
- HCC 2014 2015 Course CatalogDocument399 pagesHCC 2014 2015 Course Cataloglisa leNo ratings yet
- DENGUE CS NCP 1Document8 pagesDENGUE CS NCP 1Karyl SaavedraNo ratings yet
- Past Exam PaperDocument5 pagesPast Exam PaperDavid Le50% (2)
- Dissociative Identity Disorder (Multiple Personality Disorder) - Psychology TodayDocument3 pagesDissociative Identity Disorder (Multiple Personality Disorder) - Psychology TodayIrzaNo ratings yet
- Peterson, Severin - A Catalog of The Ways People Grow PDFDocument383 pagesPeterson, Severin - A Catalog of The Ways People Grow PDFvivaldioz100% (2)
- Sai Vibrionics Newsletter From The Desk of DR Jit K AggarwalDocument18 pagesSai Vibrionics Newsletter From The Desk of DR Jit K AggarwalSujok Swadesh100% (1)
- 7 PENYAKIT JANTUNG BAWAAN DR - YusraDocument57 pages7 PENYAKIT JANTUNG BAWAAN DR - YusraSurya ArhNo ratings yet
- PT - PR 9996666 OccupiedDocument107 pagesPT - PR 9996666 OccupiedBelal AhmedNo ratings yet
- 2D and 3D Planning in LungDocument83 pages2D and 3D Planning in LungSayan DasNo ratings yet
- Drug Study of Antidiabetic DrugsDocument6 pagesDrug Study of Antidiabetic DrugsLorina Lynne ApelacioNo ratings yet
- High Alert MedicationsDocument17 pagesHigh Alert MedicationsJoanna Marie Datahan EstomoNo ratings yet
- Cellular and Molecular Actions of Methylene Blue in The Nervous System - Oz Et Al.Document25 pagesCellular and Molecular Actions of Methylene Blue in The Nervous System - Oz Et Al.estebanNo ratings yet
- Anemia IntroductionDocument15 pagesAnemia IntroductionNitesh Kotian100% (1)
- Coughs - and How To Treat ThemDocument15 pagesCoughs - and How To Treat Themsimplybr95630% (1)
- Six Minute Walking Distance Cut-Off Point in Indonesian (Mongoloid) PopulationDocument6 pagesSix Minute Walking Distance Cut-Off Point in Indonesian (Mongoloid) PopulationHanif RidhaNo ratings yet
- Hemp As A MedicamentDocument81 pagesHemp As A MedicamentBianca DianaNo ratings yet
- DocetaxelDocument4 pagesDocetaxelfnurdiansah002No ratings yet
- Proliferation Therapy for Tendon and Ligament InjuriesDocument18 pagesProliferation Therapy for Tendon and Ligament InjuriesJason Tutt GinNo ratings yet
- Alfred Adler Individual Psychology Case StudyDocument5 pagesAlfred Adler Individual Psychology Case StudyMadhura Bhat18 054No ratings yet