Professional Documents
Culture Documents
CHN Process
Uploaded by
Omie TumanguilOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
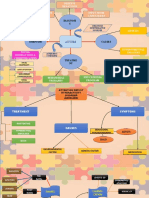
CHN Process
Uploaded by
Omie TumanguilCopyright:
Available Formats
COMMUNITY HEALTH NURSING PROCESS INTRODUCTION: The CHNurse gets to work with different types of client in her practice
(fams, grps, subgrps or popa/communities). Each has different characteristics that the nurse must recognize. However in CHN, community is not only merely an existence of families or populations. The community is our primary client reasons: 1. It has a direct influence on the health of the indvidual, families, grps and populations 2. It is in this level that most health service provision occurs CHNurse must know the defining characteristics of a community this set the stage in understanding the different aspects that directly/indirectly affect/influence the health status of the community THE COMMUNITY DIAGNOSIS Introduction: Caring for the community starts with determining its health status. The nurse collects data in order to identify the different factors that may influence the health of the population. Then she proceeds to analyze and seek explanations for the occurrence of health needs and problems of the community. Community diagnoses are then derived and will become the bases for developing and implementing interventions and strategies. This process is called community diagnosis, community assessment or situational analysis. The health status of a cmmty is a product of the various elements population, physical/topographical characteristics, socio-economic, cultural factors, basic health services and power structure. TYPES OF COMMUNITY DIAGNOSIS Introduction: In assessment, the nurse considers the degree of detail or depth she should go into. There are times when situation calls for comprhensive assessment (general info abt the cmmnty). Oftentimes, the nurse is confronted with with specific problem (disaster) problem-oriented assessment will have to be conducted. Sometimes, she can conduct both (specific pop-comprehensive; problem -problem-oriented). It is important to decide on objectives, resources and time to implement it. I. COMPREHENSIVE COMMUNITY DIAGNOSIS aims to obtain a general information about the community. The following are the elements: A. Demogrphic Variables size, composition and geographical distribution of the population as indicated by the following; 1. Total population, geographical distribution (urban-rural), density 2. Age and sex composition 3. Vital indicators growth rate, CBR, CDR, life expectancy 4. Patterns of migration 5. Population projections
- also impt to know population grps that need special attention (indigenous people, refugees, dislocated people/evacuees) B. Socio-Ecocnomic and Cultural Variables there are no limits as to the list of socio-economic and cultural factors thath may effect the health status of the community. 1. Social indicators a. Communication network formal or informal; necessary for disseminating health info or facilitating referral of clients b. Transporitation system - road networks, accesibilty of of the people to health facilities c. Educational level may be indicative of poverty, may reflect on health perception and utilization patterns d. Housing conditions which may suggest health hazards 2. Economic indicators a, Poverty level income b. Unemployment and uneremployment c. Proportion of salaried and wage earners to total economically active populations d. Types of industries present e. Occupations common 3. Environmental indicators a. Physical/geographical/topographical characteristics: - land areas that contribute to vector problems; terrains accidents/hazards - land usage on industry; climate/season b. Water supply - % population with access to safe, adequate water supply; source c. Waste disposal -% served by daily garbage collection; % population with safe ecreta disposal system; types of disposal system d. Air, Water, Land pollution - industries with hazards 4. Cultural factors a. Variables that may break up peple into groups (ethnecity, class, language, religion, race, political orientation) b. Cultural beliefs and practices that affect health c. Concepts on health and illness C. Health and Illness patterns - nurse may collect primary data about leading causes of illness and deaths with rates of occurrence - secondary data may also be used; mortality, morbidity, infant/maternal mortality, hospital admission D. Health Resources - important element essential ingredients in DBHS; manpower, money, machineries, material 1. Manpower resources - categories, distribution, population ratio, distriburionj accdg to facilities/organization (gov't, NGO, private); polcies 2. Material resources - budget and expenditures, fundings, institutions, bed ratio, services
E. Political/leadership Patterns - vital element in achieving high level of wellness among the people. It reflects the people's potential to address health needs and problems. It also mirrors the sensitivity of the government. - power structures, attitudes of the people, conditions/events/issues that cause conflict or unification
II. PROBLEM-ORIENTED COMMUNITY DIAGNOSIS - type of assessment that responds to particular need. The nurse proceeds with the identification of the population who were affected by the hazards/problems. Then the nurse proceeds on to characetrize the factors which are relevant to the specific problem being investigated. COMMUNITY DIAGNOSIS: THE PROCESS collecting, organizing, synthesizing, analyzing and interpreting health data before data gathering, the nurse must formulate objectives this will dictate the scope or depth of the diagnosis. STEPS IN COMMUNITY DIAGNOSIS in order to generate a broad range of useful data, cmmty dx must be carried out in an organized and systmatic manner community should take an active part in identifying community needs and problems 1. Determining the objectives - CHNurse decides on the depth and scope of the data she needs to gather - the nurse must determine the occurrence and distribution of selected conditions important to disease control and wellness promotion 2. Defining the study population nurse identifies the population group to be included in the study either entire population or specific 3. Determining the data to be collected - objectives will guide the in identifying the specific data needed, sources ( 4. Collecting the data - different methods are used depends on type of data - example: ocular survey physical/topographical characteristics; interview people health beliefs; review records a. Records review reviewing data compiled by health or non-health agencies b. Surveys and observation qualitative and quantitative c. Interviews first hand information d. Participant observation qualitative data, allowing the nurse to actively participate 5. Developing the instrument - tools - survey questionnaire, interview guide, observation checklist 6. Actual data gathering - before the actual data gathering, thenurse must meet the people instruments are discussed and analyze. It can be modified or simplified (not to overburden the
people -education or time to finish) pre-testing is highly recommended data collectors must be given orientation and trainings how to use (can do role-play) during actual data gathering nurse supervises by checking the instruments (completeness, accuracy, reliability) 7. Data collation -after collection, the data is put together. Two types of data my be generated numerical (counted) or descriptive (described) - categorize or classify data exclusive (choices do not overlap) or exhaustive (anticipate all possible answers may be given) - in fixed response questions, choices must be provided - after categorizing, the responses will be to summarize the data (manually or by computer) 8. Data presentation - depend on the type of data obtained; descriptive data narrative reports - numerical table or graph 9. Data analysis - aims to establish trends and patterns in terms of health needs and problems of the community; allows comparison of obtained data with standard values. - determining the interrelationship of factors will help the nurse view the significance of the problems and their implications on health status of the community 10. Identifuing the CHN problems - CHN problems are categorized as: a. health status problems they may be described in terms of increased/decreased morbidity, mortality or fertility b. health resources problems lack of 4 M's c. health-related problems factors that aggravate the illness-inducing situations 11. Priority-setting -after problems have been identified, next is to prioritize which health problems can be attended to considering the resources available at the moment Criteria: a. nature of the problem presented classified as health status, health resources, healthrelated problems b. magnitude of the problem severity of the problem c. modifiability of the problem this refers to the probability of reducing, controlling or eradicating the problem d. preventive potential refers to the probability of controlling or reducing the effects posed by the problem e. social concern refers to the perception of the population or community as they are affected by the problem CRITERIA NATURE OF THE PROBLEM Health status Health resources Health-related 3 2 1 WEIGHT 1
MAGNITUDE OF THE PROBLEM 75%-100% effected 4 50%-74% affected 3 25%-49% affected 2 <25% affected 1 MODIFIABILITY OF THE PROBLEM High 3 Moderate 2 Low 1 Not modifiable 0 PREVENTIVE POTENTIAL High Moderate Low SOCIAL CONCERN Urgent community concern Recognized as problem but not needing urgent attention Not a community concern 3 2 1
1 2 1 0
Each problem will be scored according to each criteria and divided by the highest possible score multiplied by the weight. Then the final score for each criteria will be added to give the total score for the problem. The problem with the highest total score is given hihg priority.
You might also like
- Community As ClientDocument13 pagesCommunity As ClientVirus50% (2)
- ETP Flexible Eating GuideDocument61 pagesETP Flexible Eating Guidecoachhand100% (1)
- CHN - Community DiagnosisDocument45 pagesCHN - Community DiagnosisStudentnurseMj100% (1)
- 3 Heart InternetNewDocument55 pages3 Heart InternetNewCoral Srinivasa RamaluNo ratings yet
- Community Assessment and DiagnosisDocument25 pagesCommunity Assessment and DiagnosisVince Patrick LeonidaNo ratings yet
- Fetus & Neoborn-3Document25 pagesFetus & Neoborn-3Mateen Shukri100% (1)
- Community Health Nursing ProcessDocument23 pagesCommunity Health Nursing ProcessMaureen A. Bawang0% (1)
- CHNIMODULEIDocument44 pagesCHNIMODULEIlagumbayjoviann1No ratings yet
- Shape Shifter Yoga Starter ManualDocument25 pagesShape Shifter Yoga Starter ManualVernetteNg100% (1)
- Learning Material-Community Health Nursing ProcessDocument52 pagesLearning Material-Community Health Nursing Processzebzeb STEMANo ratings yet
- Mind MapDocument3 pagesMind MapaziemNo ratings yet
- ASA Physical Status ClassificationDocument1 pageASA Physical Status ClassificationАндрій ДанильцівNo ratings yet
- Assessing Community Health NeedsDocument17 pagesAssessing Community Health NeedsClarissa Isuriña100% (2)
- Elements of A Comprehensive Community DiagnosisDocument6 pagesElements of A Comprehensive Community DiagnosisAila Hinlog100% (8)
- CHN 005Document14 pagesCHN 005betiful100% (5)
- Diseases of Poultry A Colour AtlasDocument213 pagesDiseases of Poultry A Colour AtlasShakil Mahmod100% (1)
- The Community DiagnosisDocument11 pagesThe Community DiagnosisAize Francisco100% (2)
- NCM 113 - Community Health Nursing 2 Community DiagnosisDocument10 pagesNCM 113 - Community Health Nursing 2 Community DiagnosisFrancheska Kyla GomezNo ratings yet
- Community Health Nursing ProcessDocument6 pagesCommunity Health Nursing ProcessAmiel Francisco ReyesNo ratings yet
- CHN NotesDocument65 pagesCHN Noteslanie_jecielNo ratings yet
- Cirrhosis of LiverDocument35 pagesCirrhosis of LiverShazia Parveen100% (1)
- Community DiagnosisDocument30 pagesCommunity DiagnosisPaulo Galang83% (6)
- Disease Emergence and Resurgence: The Wildlife-Human ConnectionDocument402 pagesDisease Emergence and Resurgence: The Wildlife-Human ConnectionMaíra100% (1)
- Community Health Nursing Ii NUR204: Population Groups and Community As Clients)Document31 pagesCommunity Health Nursing Ii NUR204: Population Groups and Community As Clients)ZairaNo ratings yet
- WEEK 1 - Concept of CommunityDocument5 pagesWEEK 1 - Concept of Communitypoleene de leonNo ratings yet
- Community Health Nursing ReviewerDocument24 pagesCommunity Health Nursing ReviewergilpogsNo ratings yet
- CHN Lec Activity 1Document9 pagesCHN Lec Activity 1RickNo ratings yet
- The Community DiagnosisDocument5 pagesThe Community DiagnosisEries Lacanlale Lumba50% (4)
- New Health Systems: Integrated Care and Health Inequalities ReductionFrom EverandNew Health Systems: Integrated Care and Health Inequalities ReductionNo ratings yet
- Community Health Nursing ProcessDocument69 pagesCommunity Health Nursing ProcessDharylle CariñoNo ratings yet
- Birth AsphyxiaDocument27 pagesBirth AsphyxiaJaya Prabha100% (5)
- Epidemiology methods guide for researchDocument183 pagesEpidemiology methods guide for researchBekele AtnafuNo ratings yet
- Continuing Education in NursingDocument22 pagesContinuing Education in NursingOmie TumanguilNo ratings yet
- CommunityDocument6 pagesCommunityMyrrha TaganasNo ratings yet
- Micro TeachingDocument52 pagesMicro TeachingMatetzky Sapiter Bueno0% (1)
- Community Phc2 RleDocument12 pagesCommunity Phc2 Rleefermin_lovely100% (1)
- Community DiagnosisDocument27 pagesCommunity DiagnosislouvvhartNo ratings yet
- Community Needs Assessment HRDP COPAR 2013Document6 pagesCommunity Needs Assessment HRDP COPAR 2013Amiel Francisco Reyes100% (1)
- 2 Community AssessmentDocument35 pages2 Community AssessmentDrshahira MohamedNo ratings yet
- COMMUNITY HEALTH DIAGNOSISDocument22 pagesCOMMUNITY HEALTH DIAGNOSISkuruvagadda sagarNo ratings yet
- Community Health Nursing Process AssessmentDocument44 pagesCommunity Health Nursing Process AssessmentApril FlorendoNo ratings yet
- COMMUNITY HEALTH PROFILEDocument39 pagesCOMMUNITY HEALTH PROFILELuo Miyanda100% (1)
- Community-Diagnosis ReferenceDocument45 pagesCommunity-Diagnosis ReferenceAnonymous h2EnKyDbNo ratings yet
- Community Health Nursing ProcessDocument9 pagesCommunity Health Nursing ProcessJohn Lawrence YbanezNo ratings yet
- CHN Assignment (Answer)Document10 pagesCHN Assignment (Answer)buttercup_chrissieNo ratings yet
- CSAB Community Health NSG Process Com DiagnosisDocument36 pagesCSAB Community Health NSG Process Com DiagnosisG26 Panaguiton, JairaNo ratings yet
- CHN 2 NUR 1214 Week 5 Module 5 Assessment and DiagnosisDocument12 pagesCHN 2 NUR 1214 Week 5 Module 5 Assessment and DiagnosisLorraine Jazmine AquinoNo ratings yet
- COPAR Community Assessment 1Document3 pagesCOPAR Community Assessment 1Winter KimNo ratings yet
- The ROLE OF The Public Health Nurse-AnnievadneDocument39 pagesThe ROLE OF The Public Health Nurse-AnnievadneDolores BeeNo ratings yet
- Fa18-Fsn-016 Ans A4Document11 pagesFa18-Fsn-016 Ans A4Mehwish MughalNo ratings yet
- Community Assessment: Prepper by Nariman NOUHDocument25 pagesCommunity Assessment: Prepper by Nariman NOUHN NNo ratings yet
- A Community Is A Cluster of People With at Least One Common CharacteristicDocument7 pagesA Community Is A Cluster of People With at Least One Common CharacteristicWilliam Ezekiel JUju CustodioNo ratings yet
- Community Assessment and Community DiagnosisDocument4 pagesCommunity Assessment and Community DiagnosisLaurence ZernaNo ratings yet
- Study Guide For ExamDocument36 pagesStudy Guide For ExamCatherine Drew SimsNo ratings yet
- CHN Chapter 6Document6 pagesCHN Chapter 6Paulo Marie TanNo ratings yet
- Community Diagnosis:: Community Health Nursing ProcessDocument44 pagesCommunity Diagnosis:: Community Health Nursing Processlaydomingo11No ratings yet
- Planning Community Health InterventionsDocument5 pagesPlanning Community Health InterventionsJanisse CalaguiNo ratings yet
- Community DiagnosisDocument12 pagesCommunity DiagnosisRichard Onen100% (1)
- 6) Community Diagnosis 2011Document33 pages6) Community Diagnosis 2011Dinar Kartika HapsariNo ratings yet
- CHN II - ReviewerDocument34 pagesCHN II - ReviewerKarina Blanca Sanico AdranedaNo ratings yet
- Principles of CHN New UpdatedDocument4 pagesPrinciples of CHN New Updatediheart musicNo ratings yet
- BaliteDocument5 pagesBaliteRaymond Lee Montilla BaliteNo ratings yet
- PHC Community DiagnosisDocument27 pagesPHC Community DiagnosisCassandra_Maca_6324No ratings yet
- CHN2Document43 pagesCHN2Sidney Bon LuceroNo ratings yet
- Community Health Diagnosis GuideDocument2 pagesCommunity Health Diagnosis GuidekimerellaNo ratings yet
- Community Health Nursing Diagnosis & InterventionsDocument17 pagesCommunity Health Nursing Diagnosis & InterventionsMarthy BollenaNo ratings yet
- Community Diagnosis 2016-2Document14 pagesCommunity Diagnosis 2016-2wanjohiisaac84No ratings yet
- Community HealthDocument30 pagesCommunity HealthKeyceeleen Guevarra LimNo ratings yet
- Carmel Marie Venezuela - Nursing Process in The Care of Population Groups and Community ActivityDocument5 pagesCarmel Marie Venezuela - Nursing Process in The Care of Population Groups and Community ActivityCarmel Venezuela100% (1)
- Community AssessmentDocument9 pagesCommunity Assessmentرانيا احمد عبد الكريمNo ratings yet
- Meeting the Needs of Older Adults with Serious Illness: Challenges and Opportunities in the Age of Health Care ReformFrom EverandMeeting the Needs of Older Adults with Serious Illness: Challenges and Opportunities in the Age of Health Care ReformAmy S. KelleyNo ratings yet
- Nurse's Guide to Patient CareDocument30 pagesNurse's Guide to Patient CareOmie TumanguilNo ratings yet
- Drug Calculation SkillsDocument13 pagesDrug Calculation SkillsOmie TumanguilNo ratings yet
- Managing Diabetes and ComplicationsDocument35 pagesManaging Diabetes and ComplicationsOmie TumanguilNo ratings yet
- Reqtmsn PreDocument11 pagesReqtmsn PreOmie TumanguilNo ratings yet
- 01Document13 pages01Omie TumanguilNo ratings yet
- The National Health Plan-OutlineDocument9 pagesThe National Health Plan-OutlineOmie TumanguilNo ratings yet
- The National Health Plan-OutlineDocument9 pagesThe National Health Plan-OutlineOmie TumanguilNo ratings yet
- Problems 10th Revision (ICD-10) Is A Coding of Diseases and Signs, Symptoms, AbnormalDocument10 pagesProblems 10th Revision (ICD-10) Is A Coding of Diseases and Signs, Symptoms, AbnormalOmie TumanguilNo ratings yet
- Fields of NursingDocument8 pagesFields of NursingOmie TumanguilNo ratings yet
- Funda Bullet FormDocument11 pagesFunda Bullet FormannherreraNo ratings yet
- Ob DXDocument12 pagesOb DXOmie TumanguilNo ratings yet
- CNS Pathology StrokeDocument11 pagesCNS Pathology StrokeKamran Khan KhalilNo ratings yet
- Quaratine Isolation Center DesignDocument6 pagesQuaratine Isolation Center DesignYeabtsega ZelalemNo ratings yet
- Approach To Anemia Chalk Talk NotesDocument2 pagesApproach To Anemia Chalk Talk NotesMarl KarxNo ratings yet
- CIcloyd Psychosis Peralta CuestaDocument10 pagesCIcloyd Psychosis Peralta CuestaJuan IgnacioNo ratings yet
- Manual Muscle Test (MMT) : Ajith C Student of Department of Physio Kmch-CoptDocument80 pagesManual Muscle Test (MMT) : Ajith C Student of Department of Physio Kmch-Coptayesha solNo ratings yet
- Prevalence of Seizure and Prescribing Patterns of Aed in Patients With NeuroDocument120 pagesPrevalence of Seizure and Prescribing Patterns of Aed in Patients With NeurosnigdhaNo ratings yet
- Lecture 15 Cardiovascular DiseaseDocument19 pagesLecture 15 Cardiovascular DiseaseHHGV JGYGUNo ratings yet
- Reflexology Research PapersDocument10 pagesReflexology Research Paperskyle atienzaNo ratings yet
- Endocrinology: Differences Between Nervous and Endocrine SystemDocument34 pagesEndocrinology: Differences Between Nervous and Endocrine SystemRezaul RazibNo ratings yet
- Bakteri Anaerob: Morfologi, Fisiologi, Epidemiologi, Diagnosis, Pemeriksaan Sy. Miftahul El J.TDocument46 pagesBakteri Anaerob: Morfologi, Fisiologi, Epidemiologi, Diagnosis, Pemeriksaan Sy. Miftahul El J.TAlif NakyukoNo ratings yet
- Ate PatDocument31 pagesAte PatJerry ChioNo ratings yet
- MF2 - Spinal Cord InjuryDocument43 pagesMF2 - Spinal Cord InjuryAnnbe BarteNo ratings yet
- Pathomorphology FinalDocument216 pagesPathomorphology FinalAugustine A. KollieNo ratings yet
- 1st Bi PediaDocument19 pages1st Bi PediaBeo Adelynn - AiiyuNo ratings yet
- Granuloma Annulare TreatmentDocument2 pagesGranuloma Annulare Treatmentjohn martenNo ratings yet
- Common Medical AbbreviationsDocument4 pagesCommon Medical AbbreviationsApril Joy de LimaNo ratings yet
- Diet Prevents Polio by Maintaining Normal Blood SugarDocument69 pagesDiet Prevents Polio by Maintaining Normal Blood SugarIyemhetepNo ratings yet
- 04 InfectionDocument18 pages04 InfectionMalinda KarunaratneNo ratings yet