Professional Documents
Culture Documents
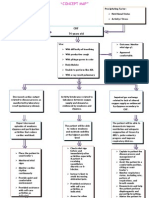
Assessment Nursing Diagnosis Scientific Explanation Planning Nursing Intervention Rationale Evaluation Subjective
Uploaded by
banyenye25Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Assessment Nursing Diagnosis Scientific Explanation Planning Nursing Intervention Rationale Evaluation Subjective
Uploaded by
banyenye25Copyright:
Available Formats
NURSING DIAGNOSIS Impaired gas Subjective: exchange related Nahihirapan ako to ventilationhuminga.
AVB the perfusion mother of the patient inequality secondary to COPD Objective: VS: T: 36.9C RR: 28 cpm PR: 120 bpm BP: 140/90 (+) Dyspnea Weak in appearance Pallor
ASSESSMENT
SCIENTIFIC EXPLANATION Inhalation of pathogens Activation of circulating macrophages Injury due to Inflammatory response Narrowing of the small peripheral airways Injury-repair prcess scar tissue fomation Impaired gas exchange Narrowing of the airway lumen
PLANNING
After 7 hours of effective nursing intervention, the patient will be able to: Assess the contributing factors that aggravates verbalize patients breathing normal pattern. respiration or normal Place the patient in breathing Semi-Fowlers pattern as position. evidenced by: Encourage the pt to do deep breathing and Vital signs coughing exercises. within the normal range particularly the Encourage patient to respiratory rate maintain calm attitude. from 15-20 cpm. Participate in treatment Observe proper visit regimen such hours and give the as: patient enough time to rest - Breathing exercises Provide well ventilated room
(-) dyspnea
NURSING INTERVENTION Assess the rate and depth of respiration.
RATIONALE For baseline data
EVALUATION After 7 hours of effective nursing intervention, goal was met AEB: The patient verbalized normal respiration or normal breathing pattern as evidenced by:
(-) dyspnea
To eradicate or minimize these contributing factors To facilitate maximum expansion of the lungs
To promote expectoration of secretions and relaxation To promote wellness and decreases metabolic demand. To avoid disturbance and the pt could rest
Vital signs within the normal range RR= 20cpm Participated in treatment regimen such as: Breathing exercises
Airway obstruction
ventilationperfusion inequality
To promote
ventilation Impaired gas exchange Health teaching on proper hygiene particularly in oral. COLLABORATIVE: Administer nebulization as ordered.
To promote hygiene and fresh breath.
To promote bronchodilation
ASSESSMENT Subjective: Mabilis akong mapagod, as verbalized by the patient Objective: Weak Pallor (+) dyspnea cold clammy skin changes in HR and BP w/ activity VS: T: 36.9 C P: 95 bpm R: 25 cpm BP: 140/90 mmHg
NURSING DIAGNOSIS Activity intolerance r/t imbalance between myocardial oxygen supply and demand
SCIENTIFIC EXPLANATION Imbalance of blood supply and demand
Myocardial Ischemia
Decrease of Myocardial oxygen supply
Increase of cellular hypoxia
Altered cell membrane int.
NURSING INTERVENTION After 7 hours of Record HR and BP effective nursing changes before, intervention, the during and after patient will be able activity to: Position the patient Participate in a semi-fowlers willingly in position necessary/desi Encourage bed rest red activities Use identified techniques to Instruct patient to enhance avoid increase activity abdominal pressure intolerance like straining during defecation Encourage to limit strenuous activities Explain pattern of graded increase of activity level like progressive ambulation and resting after meals Ascertain ability to stand and move about and degree of assistance necessary/use of
PLANNING
RATIONALE To determine pts response to activity To allow for rest and increase available oxygen Reduces myocardial workload and oxygen consumption Activities that require holding breath and bearing down can result in bradycardia and rebound tachycardia w/ elevated BP Because strenuous activities increase cardiac work Progressive activity provides a controlled demand on the heart, increase strength and preventing overexertion To determine current status and needs associated with participation in needed/desired
EVALUATION After 7 hours of effective nursing intervention, goal was met AEB: Patient participated willingly in necessary/desi red activities Used identified techniques to enhance activity intolerance
Decrease of myocardial contractility
Decrease of cardiac output
Decrease of arterial pressure
Stimulation of Baroreceptors
equipment Promote comfort measures and provide for relief of pain
activities To enhance ability to participate in activities
Stimulation of sympathetic receptors
Increase Increase myocardial Peripheral constriction contractility
Increase HR Increase after load
Decrease diastolic filling Decrease myocardial tissue perfusion
Increase myocardial oxygen demand
ASSESSMENT Subjective: Mabilis akong mapagod AVB the patient Objective: Bipedal edema (+) dyspnea Weak in appearance
NURSING DIAGNOSIS Decreased cardiac output r/t altered stroke volume
SCIENTIFIC EXPLANATION Increased blood pressure
PLANNING After 7 hours of effective nursing interventions, the patient will be able to: Verbalize knowledge of the disease process, individual risk factors and treatment regimen. Report decreased episodes of dyspnea Participate in activities that reduce the workload of the heart such as: - Stress management - Rest plan - Cessation of smoking - Treatment regimen
NURSING INTERVENTION Monitor and record BP and pulse. Institute bedrest with client in lateral position. instruct patient to avoid food high in cholesterol and sodium discuss significant signs and symptoms that needs to be reported immediately to a health care provider such as muscle cramps headache, dizziness teach home monitoring of weight, pulse and blood pressure
RATIONALE For baseline data
EVALUATION After 7 hours of effective nursing interventions, goal was met AEB: Patient verbalized knowledge of the disease process, individual risk factors and treatment regimen. Reported decreased episodes of dyspnea Participated in activities that reduce the workload of the heart such as: - Stress management - Rest plan - Cessation of smoking - Treatment regimen
Vasospasm
Increased vascular resistance Difficulty of the heart to pump blood
Increases venous return, cardiac output, and renal perfusion. this types of food can worsen the patients disease condition This can prevent worsening the patients condition because this may be signs of mineral losses to detect changes and allow immediate and timely
VS: T: 36.9C RR: 28 cpm PR: 120 bpm BP: 140/90 Increased cardiac workload
Decreased cardiac output
interventions Administer Furosemide as ordered If BP does not respond to conservative measures, short-term medication may be necessary in conjunction with other therapies
You might also like
- Managing Breathlessness in the CommunityFrom EverandManaging Breathlessness in the CommunityRating: 3.5 out of 5 stars3.5/5 (2)
- A Simple Guide to Oxygen Therapy, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Oxygen Therapy, Diagnosis, Treatment and Related ConditionsNo ratings yet
- NCP Rheumatic Heart DiseaseDocument3 pagesNCP Rheumatic Heart DiseaseAdrian Mallar71% (28)
- NCPDocument2 pagesNCPDidith AbanNo ratings yet
- NCPDocument3 pagesNCPKrizelle Abadesco Libo-on50% (2)
- Decreased Cardiac OutputDocument9 pagesDecreased Cardiac OutputChinita Sangbaan75% (4)
- CHF Concept MapDocument4 pagesCHF Concept MapLisaSanders99No ratings yet
- Ineffective Airway ClearanceDocument6 pagesIneffective Airway ClearanceBenly Grace Rebuyon MosquedaNo ratings yet
- Nursing Care and Drug Study of EpinephrineDocument6 pagesNursing Care and Drug Study of EpinephrineuserringpointNo ratings yet
- NCPDocument5 pagesNCPRose AnnNo ratings yet
- HypertensionDocument3 pagesHypertensionAgnes Marie RendonNo ratings yet
- Cardiac ComplicationDocument12 pagesCardiac ComplicationResa ShotsNo ratings yet
- NCP For COPD and Acute PainDocument7 pagesNCP For COPD and Acute PainLenny SucalditoNo ratings yet
- Managing COPD: Nursing Care for Breathing Issues, Nutrition, Infection RiskDocument2 pagesManaging COPD: Nursing Care for Breathing Issues, Nutrition, Infection RiskAl RizkyNo ratings yet
- Assessment Nursing Diagnosis Analysis Goals and Objectives Nursing Interventions Rationale Evaluation EffectivenessDocument3 pagesAssessment Nursing Diagnosis Analysis Goals and Objectives Nursing Interventions Rationale Evaluation EffectivenessYnah Sayoc75% (4)
- Nursing Care Plan-AnemiaDocument1 pageNursing Care Plan-AnemiaAdrian Mallar100% (2)
- Managing Acute Renal PainDocument22 pagesManaging Acute Renal PainMaricris S. Sampang100% (1)
- Manage Cor Pulmonale with Oxygen, Meds & Lifestyle ChangesDocument29 pagesManage Cor Pulmonale with Oxygen, Meds & Lifestyle ChangesdaisyNo ratings yet
- NCP-Case Presentation (CHF)Document4 pagesNCP-Case Presentation (CHF)Jessamine EnriquezNo ratings yet
- NCP Activity IntoleranceDocument2 pagesNCP Activity IntoleranceJill Catherine CabanaNo ratings yet
- CHRONIC HEART FAILURE CASE STUDYDocument12 pagesCHRONIC HEART FAILURE CASE STUDYMary Cris CanonNo ratings yet
- NCP For CHF 3 Activity IntoleranceDocument2 pagesNCP For CHF 3 Activity IntoleranceAngelyn ArdinesNo ratings yet
- Which It Is A Process Whereby Pancreatic Enzymes Destroy Its Own Tissue Leading ToDocument8 pagesWhich It Is A Process Whereby Pancreatic Enzymes Destroy Its Own Tissue Leading ToAriane-Gay Cristobal DuranNo ratings yet
- NCP Proper 1Document6 pagesNCP Proper 1Noreen PinedaNo ratings yet
- Cardiac NSG DiagnosisDocument5 pagesCardiac NSG DiagnosisShreyas WalvekarNo ratings yet
- © 2009 by Lippincott Williams & Wilkins. All World Rights ReservedDocument24 pages© 2009 by Lippincott Williams & Wilkins. All World Rights Reservedachsan tudhonnnyNo ratings yet
- Acid BaseDocument29 pagesAcid BaseOlivia LowellNo ratings yet
- Hypertension - Docx NCPDocument9 pagesHypertension - Docx NCPMarjorie BelanteNo ratings yet
- NCP PROPER Pain and Decreased Cardiac OutputDocument3 pagesNCP PROPER Pain and Decreased Cardiac OutputErienne Lae Manangan - CadalsoNo ratings yet
- Nursing Care Plan for Respiratory IssuesDocument10 pagesNursing Care Plan for Respiratory IssuesMykel Jake VasquezNo ratings yet
- Care PlanDocument6 pagesCare PlanDavina MartinNo ratings yet
- Heart Failure Care PlanDocument2 pagesHeart Failure Care PlanJonathon100% (1)
- Promote Health for Dyspneic Patient with Cardiac ConditionsDocument3 pagesPromote Health for Dyspneic Patient with Cardiac ConditionsDylle Lorenzo ClaudioNo ratings yet
- Mrs. MM Nursing Care PlanDocument34 pagesMrs. MM Nursing Care PlanIsobel Mae JacelaNo ratings yet
- NCPDocument6 pagesNCPSarah Younes AtawnehNo ratings yet
- Nursing Care Plan HF FinalDocument10 pagesNursing Care Plan HF FinalCristina L. JaysonNo ratings yet
- Assessment Nursing Diagnosis Scientific Explanation Planning Implementation Rationale EvaluationDocument4 pagesAssessment Nursing Diagnosis Scientific Explanation Planning Implementation Rationale EvaluationVince DinsayNo ratings yet
- Hypertensive Cardiovascular DiseaseDocument16 pagesHypertensive Cardiovascular DiseaseTintin Ponciano100% (1)
- Nursing Care Plan for Impaired Gas Exchange and Breathing PatternsDocument22 pagesNursing Care Plan for Impaired Gas Exchange and Breathing Patternsaln00550% (2)
- Decrease Cardiac Output Related To Altered Stroke VolumeDocument3 pagesDecrease Cardiac Output Related To Altered Stroke VolumeRalph PelegrinoNo ratings yet
- And Release of Pancreatic Enzyme: Which It Is A Process Whereby Pancreatic Enzymes Destroy Its Own Tissue Leading ToDocument15 pagesAnd Release of Pancreatic Enzyme: Which It Is A Process Whereby Pancreatic Enzymes Destroy Its Own Tissue Leading ToAriane-Gay Cristobal DuranNo ratings yet
- NCPDocument2 pagesNCPSunshine IslaNo ratings yet
- Concept Map - Abby !Document2 pagesConcept Map - Abby !Abegail Abaygar100% (3)
- Goals and OrdersDocument31 pagesGoals and OrdersMAKINo ratings yet
- NCPDocument9 pagesNCPLeolene Grace BautistaNo ratings yet
- Nursing DiagnosisDocument16 pagesNursing DiagnosisSi Bunga JonquilleNo ratings yet
- NURSING CARE PLAN For Myocardial InfarctionDocument13 pagesNURSING CARE PLAN For Myocardial Infarctionbanyenye2593% (14)
- Impaired Tissue PerfusionDocument2 pagesImpaired Tissue PerfusionLyka Mae Imbat - PacnisNo ratings yet
- Activity Intolerance NCPDocument6 pagesActivity Intolerance NCPDoo NahNo ratings yet
- Impaired kidney function nursing careDocument21 pagesImpaired kidney function nursing careKate ManalastasNo ratings yet
- Decreased Urine OutputDocument3 pagesDecreased Urine OutputSj 斗力上No ratings yet
- NCP PTBDocument6 pagesNCP PTBJay Dela VegaNo ratings yet
- Fatigue and weakness assessmentDocument18 pagesFatigue and weakness assessmentBob Joyce Dela PeñaNo ratings yet
- NCM 106 Acute Biologic CrisisDocument142 pagesNCM 106 Acute Biologic CrisisEllamae Chua88% (8)
- PIHDocument2 pagesPIHTed Cipriano VistaNo ratings yet
- NCPDocument9 pagesNCPEjie Boy Isaga67% (3)
- Ncp'sDocument8 pagesNcp'sDuchess Kleine RafananNo ratings yet
- Monitoring Fever and Breathing PatternsDocument4 pagesMonitoring Fever and Breathing PatternsMarc AnchetaNo ratings yet
- Endocrine Hypertension: From Basic Science to Clinical PracticeFrom EverandEndocrine Hypertension: From Basic Science to Clinical PracticeJoseph M. PappachanNo ratings yet
- Obesity Hypoventilation Syndrome: From Physiologic Principles to Clinical PracticeFrom EverandObesity Hypoventilation Syndrome: From Physiologic Principles to Clinical PracticeAiman TulaimatNo ratings yet
- Virginia Henderson TheoryDocument6 pagesVirginia Henderson Theorybanyenye25No ratings yet
- A G E - PathoDocument1 pageA G E - Pathoranee dianeNo ratings yet
- Clinical Instructor Cover LetterDocument1 pageClinical Instructor Cover Letterbanyenye25No ratings yet
- Patho MIDocument2 pagesPatho MIbanyenye25100% (2)
- Electro Cardiograph yDocument14 pagesElectro Cardiograph ybanyenye25No ratings yet
- Nursing Interventions CHFDocument3 pagesNursing Interventions CHFbanyenye25100% (1)
- Pathophysiology of Congestive Heart Failure: Cardiovascular SystemDocument3 pagesPathophysiology of Congestive Heart Failure: Cardiovascular Systembanyenye25No ratings yet
- Laboratory Assessment CHFDocument3 pagesLaboratory Assessment CHFbanyenye25No ratings yet
- Com Epi PaperDocument25 pagesCom Epi Paperbanyenye25No ratings yet
- Acute Bronchitis PathoDocument3 pagesAcute Bronchitis Pathobanyenye25No ratings yet
- Patho MIDocument2 pagesPatho MIbanyenye25100% (2)
- EndometriosisDocument7 pagesEndometriosisbanyenye25No ratings yet
- NCP BurnDocument9 pagesNCP Burnbanyenye2533% (3)
- Philippines Population Pyramid For 2010Document4 pagesPhilippines Population Pyramid For 2010banyenye25No ratings yet
- Principles of BioethicsDocument5 pagesPrinciples of Bioethicsbanyenye25No ratings yet
- Nursing Care for Fracture PatientDocument2 pagesNursing Care for Fracture Patientbanyenye25No ratings yet
- NCP Risk For InfectionDocument3 pagesNCP Risk For Infectionbanyenye25No ratings yet
- Philippine healthcare laws overviewDocument5 pagesPhilippine healthcare laws overviewbanyenye25100% (3)
- NCPDocument4 pagesNCPbanyenye25No ratings yet
- Pa Tho PhysiologyDocument2 pagesPa Tho Physiologybanyenye25No ratings yet
- NURSING CARE PLAN For Myocardial InfarctionDocument13 pagesNURSING CARE PLAN For Myocardial Infarctionbanyenye2593% (14)
- NCP Risk For InfectionDocument3 pagesNCP Risk For Infectionbanyenye25No ratings yet
- Weekly-DLL-Science G9 WK 2Document6 pagesWeekly-DLL-Science G9 WK 2Liway Nieles Umaclap CuerdoNo ratings yet
- CARDIAC ARRHYTHMIA GUIDEDocument44 pagesCARDIAC ARRHYTHMIA GUIDEChinenye Akwue100% (1)
- Faradic: Reference ManualDocument19 pagesFaradic: Reference ManualrobertNo ratings yet
- Acitivty Sheets Q1W1 W2Document8 pagesAcitivty Sheets Q1W1 W2Christian BejarinNo ratings yet
- Plastinated Dog Heart Dorsal SectionDocument3 pagesPlastinated Dog Heart Dorsal SectionRoger CallNo ratings yet
- Chi Nei Tsangi 2 - Internal Organs Chi Massage PDFDocument66 pagesChi Nei Tsangi 2 - Internal Organs Chi Massage PDFAlexandra Ioana NiculescuNo ratings yet
- Pharmacology of Antiarrhythmic DrugsDocument51 pagesPharmacology of Antiarrhythmic DrugsselflessdoctorNo ratings yet
- Nursing Practice Threesoko Na Ito Cgena... Kainis 1Document16 pagesNursing Practice Threesoko Na Ito Cgena... Kainis 1JayCesarNo ratings yet
- Orange Data Mining Tool: PresentationDocument57 pagesOrange Data Mining Tool: PresentationWinda RizkiaNo ratings yet
- Journal-Of-Hypertension 2Document2 pagesJournal-Of-Hypertension 2Basema HashhashNo ratings yet
- 2010 Integrated Updated Circulation ACLS Tachycardia AlgorithmDocument1 page2010 Integrated Updated Circulation ACLS Tachycardia AlgorithmRyggie ComelonNo ratings yet
- Modified Valsalva Manoeuvre for SVTDocument3 pagesModified Valsalva Manoeuvre for SVTJyotirmayeeNo ratings yet
- Clinical Worksheet Mary RichardsDocument3 pagesClinical Worksheet Mary RichardsJasmyn RoseNo ratings yet
- 12 CR Use of Tenecteplase For PDFDocument4 pages12 CR Use of Tenecteplase For PDFsameeNo ratings yet
- Suz 183Document29 pagesSuz 183Benny Chris TantoNo ratings yet
- ECG QuizDocument3 pagesECG QuizRonnie LimNo ratings yet
- Cardiovascular Diseases in PregnancyDocument27 pagesCardiovascular Diseases in PregnancyAlphine DalgoNo ratings yet
- Acute Biologic Crisis For University of Mindanao 100 ItemsDocument12 pagesAcute Biologic Crisis For University of Mindanao 100 ItemsRhea Ravelo100% (2)
- Heart Rhythm Interpretation ECG Strips 2019Document21 pagesHeart Rhythm Interpretation ECG Strips 2019daniel situngkirNo ratings yet
- Blood Circulation Self-AssessmentDocument2 pagesBlood Circulation Self-AssessmentMiran El-MaghrabiNo ratings yet
- Managemen Disritmia: Dr. Rofika Hanifa, SPPDDocument20 pagesManagemen Disritmia: Dr. Rofika Hanifa, SPPDavivlabirdNo ratings yet
- Understanding Hepatitis C Discharge InstructionsDocument24 pagesUnderstanding Hepatitis C Discharge InstructionsKatherine Joy ApquisNo ratings yet
- Cabg 130102113345 Phpapp01Document29 pagesCabg 130102113345 Phpapp01md.dascalescu2486No ratings yet
- Aldesleukin 18MIU (Proleukin Inj Sol)Document2 pagesAldesleukin 18MIU (Proleukin Inj Sol)asdwasdNo ratings yet
- EkgppDocument93 pagesEkgppLindsay WishmierNo ratings yet
- Adult Cardiac Arrest Circular Algorithm: Monitor CPR QualityDocument1 pageAdult Cardiac Arrest Circular Algorithm: Monitor CPR QualityAlexis HospitalNo ratings yet
- CARDIOVASCULAR EXAMINATION Human DiseaseDocument4 pagesCARDIOVASCULAR EXAMINATION Human DiseaseVictoria MedfordNo ratings yet
- BSC Nursing: Medical Surgical Nursing - I Unit V - Disorders of The Cardio Vascular SystemDocument36 pagesBSC Nursing: Medical Surgical Nursing - I Unit V - Disorders of The Cardio Vascular SystemPoova RagavanNo ratings yet
- Aps 100Document5 pagesAps 100Omair marohomNo ratings yet
- Citirea in PalmaDocument7 pagesCitirea in PalmaAndrei AndelescuNo ratings yet