Professional Documents
Culture Documents
Poster Eecmid 2012 KPC
Uploaded by
Liana CarballoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Poster Eecmid 2012 KPC
Uploaded by
Liana CarballoCopyright:
Available Formats
P1513
Analytical and Clinical Validation of Real Time PCR for Rapid Detection of KPC carbapenemase from Rectal ESwab
Talita Trevizani Rocchetti1,2, Liana Carballo Menezes1,2, Karen de Castro Bauab1,2 ,Luiz Roberto Chirotto Filho1,2, Milene Gonalves Quiles1,2, Ana Cristina Gales1,2, Antonio Carlos Campos Pignatari1,2.
2 1UNIFESP - Federal University of So Paulo Brazil Special Clinical Microbiology Laboratory (LEMC), Federal University of So Paulo/UNIFESP
Federal University of So Paulo So Paulo - SP, Brazil Phone/Fax: +55 11 5081 2965 talita.rocchetti@lemc.br
Abstract
Rapid detection of KPC-producing Enterobacteriaceae is of great importance in infection control and in controlling the spread of these microorganisms. The application of molecular methods in clinical samples requires analytical and clinical validation .l. The aim of this study was to perform the analytical and clinical validation of real time PCR for rapid detection of gene blaKPC from direct rectal sample collected in liquid ESwab (Copan, USA). Methods: The limit of detection (LoD) and cutoff were evaluated using positive and negative control sample according to CLSI documents EP-17, EP-12. The clinical sensitivity and specificity were calculated in a ROC curve using rectal swabs samples from 156 patients hospitalized with suspected colonization by enterobacteria producing carbapenemase KPC during an clinical outbreak in 2010 at the So Paulo University Hospital. The 16S rRNA gene was used as internal control. Bacterial DNA was extracted using 200L of liquid ESwab using the QIAamp DNA Mini Kit (Qiagen, Germany) and amplification of gene blaKPC was analyzed by the real time PCR using the Platinum SYBR Green qPCR Kit Super Mix (Invitrogen , CA, USA) and 7500 Real Time PCR System equipament (Applied Biosystems, CA, USA). Results: The Cycle Threshold (Ct) delimitated to LoD and cutoff of molecular assay were 36.67 and 37.98 respectively. The clinical sensitivity and specificity were 100% and 87.5% respectively. A total of 156 samples analyzed 17.30% (27/156) were positive for blaKPC and one was negative for 16S rRNA PCR. Conclusion: These results suggest that real time PCR for ESwab direct detection from blaKPC gene in Enterobacteria can be useful in identifying patients colonized with bacteria producing carbapenemase KPC specially for control of nosocomial outbreaks.
Results
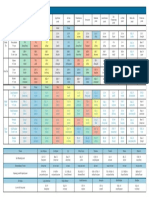
Figure 1 show the plot of the amplification of samples for gene blaKPC . We can observe the number of cycles (Ct) against Delta RN. The temperatures of desnaturation (Tm ) obtained for each sample tested was also observed,, allowing the establishment of a range of Tm experimental possible. The Tm varied 90.97861-91.3558. The mean was 91.27442 (figure 2). The values of the Cycle Threshold (Ct) determined by LoD and cutoff were 36.67 and 37.98 respectively. Figure 3 shows the ROC area, and the clinical sensitivity and specificity were 100% and 87.5% respectively.
Introduction and Purpose
Infections by Enterobacteriaceae resistant to carbapenems and/or carbapenemase producers emerging as an important challenge in the context of health care (Schwaber et al. 2008). Since the first report in 1999, North Carolina, K. pneumoniae strains resistant to carbapenems and producing the enzyme KPC ("Klebsiella pneumoniae carbapenemases") have been identified in various parts of the world: South America (Pasteran et al. 2008), China (Wei et al. 2007) and Israel (Samra et al. 2007), France (Nass et al. 2005), Greece (Cuzon et al. 2008), UK (Woodford et al. 2008), Italy (Fontana et al. 2010) and Germany (Wendt et al. 2010). In Brazil, the first report was made by Miller et al in 2009 in a strain of K. pneumoniae isolated in Recife hospital in 2006. This enzyme is strictly plasmid and confers resistance to all cephalosporins and monobactams, and reduced sensitivity to carbapenems. KPC-producing organisms often have other resistance mechanisms associated, which greatly limits the therapeutic approach, resulting in high mortality rates, particularly in debilitated patients exposed to invasive procedures and prolonged hospitalization time (CDC 2010). The use of PCR, including real-time PCR, established a new era in the processing of clinical samples. This technique decreases the release time results and is more sensitive when compared with the phenotypic method. The introduction of a new diagnostic method in clinical laboratory requires an analytical and clinical validation, to ensure greater reliability to the protocol of choice, and thus prevent the interpretation of questionable results (Stals et al., 2009). The purpose of this study was the standardization of real-time PCR for rapid detection of gene blaKPC directly EswabTM liquid (Copan, USA) rectal and perform the analytical and clinical validation of these reactions. Of the total 156 samples tested, only one sample was PCR negative for the internal control 16S rRNA and 27 (17.30%) were PCR positive for the gene blaKPC Table 1 show the results of validation for 16S Gram probes and blaKPC detection. All the specificity were almost 100%. Table 1- Values delimited for analytical validation Figure 1 - Amplification curve for the gene blaKPC Figure 2 - Tm for the gene blaKPC Figure 3 - ROC curve for the gene blaKPC
Microorganism
or
Cut
o Resistance
gene a 40 GP
16S
rDNA
GN
16S
rDNA
bla KPC
b
LoD 38,6 34,4 36,67
Tm
SD Tm
Eciency % 109,1 94,73 81,2
36,6 37,9
91,31
0,07
Area under curve ROC 0,995 0,998 0,984
Sencibility Specicity % % 87,5 99,97 76,5 82,7 99,99 99,96
GP Gram positive; GN- Gram negative; Tm - Melting temperature; LoD- Limit of detection; Ct- Threshold cycle
Conclusions
Methods
Samples We analyzed 156 rectal ESwabTM fluid samples from patients hospitalized at the Hospital with suspected colonization with KPCproducing Enterobacteriaceae in the period from 11 March to 9,April 2010. Extraction of DNA DNA extraction was performed from 200 L liquid ESwabTM, using the QIAamp DNA Mini Kit (Qiagen) according the manufacturer's instructions. Real-Time PCR For reaction internal control was used 16S rRNA gene the following primers: sense 5'ATGCAAGTCGAGCGAAC3 'and antisense 5'TGTCTCAGTTCCAGTGTGGC3'. For blaKPC resistance gene detection primers were used: sense 5'GATGACCAGCTGTTCGTGTTC3' and antisense 5'CCACATCTGGCTTGAAATTCTACTG3'. The reactions were performed with a final volume of 25 L containing 12.5 L of SYBR Green kit Platinum qPCR Super Mix (Invitrogen, California), 0.75 L (10 M) of each primer, 6 L of ultra pure water and 5 L of template DNA in the product Real Time PCR System 7500 (Applied Biosystems, CA) using the following program: 2 min at 50 C, 10 min at 95 C followed by 40 cycles of 15 sec, 95 C and 60 s, 60 C. The reaction temperature was gradually increased to 95 C to generate dissociation curves. These curves were used to assess the specificity of the PCR product. Fluorescence was quantified on-line and end with the software sequence detection system (version 2.0, Applied Biosystems). The values of Threshold Cycle (Ct) were obtained based on a predetermined limit at 0.20. Validation of Real-Time PCR The limit of detection (LOD) and the cutoff were calculated according to EP- 17 and EP-12 documents of Clinical and Laboratory Standards Institute (NCCLS) using positive and negative control samples. A producing bacterial strain well characterized enzyme KPC-2 (A28006) and ATCC controls for the 16S RNA were suspended in ultra pure water in the range 0.5 McFarland turbidity (1.5 x 108 CFU / mL). The sensitivity and specificity of the reaction were calculated by Curve Receiver Operating Characteristics (ROC curve) using the Statistical Package for Social Sciences, version 17.0 for Windows (SPSS Inc., Chicago, IL).
Conclusions
The Real-Time PCR for gene blaKPC proved to be an excellent method for detection of reduced susceptibility to carbapenems in Enterobacteriaceae. Only one sample obtained indeterminate results due to failure of internal control by the probable presence of PCR inhibitors. The Real-Time PCR direct ESwabTM is useful in the investigation of patients colonized by Enterobacteriaceae producing blaKPC gene, which contributes to the control of hospital outbreaks.
References
Centers for Disease Control and Prevention. Guidance for Control of Infections with Carbapenem-Resistant or Carbapenemase-Producing Enterobacteriaceae in Acute Care Facilities. MMWR 2010;58: (256-260). Cuzon G, Naas T, Demachy MC, Nordmann P. Plasmid mediated carbapenem-hydrolyzing beta-lactamase KPC-2 in Klebsiella pneumoniae isolate from Greece. Antimicrob Agents Chemother 2008: 52:7967. Fontana C, Favaro M, Sarmati L, Natoli S, Altieri A, Bossa MC, Minelli S, Leonardis F, Favalli C. Emergence of KPC-producing Klebsiella pneumoniae in Italy. BMC Res Notes 2010: 3: 40. Monteiro J, Santos AF, Asensi MD, Peirano G, Gales AC. First Report of KPC-2-Producing Klebsiella pneumoniae Strains in Brazil. Antimicrob Agents Chemother 2009; 53(1):333-4 Naas T, Nordmann P, Vedel G, Poyart C. Plasmid-mediated carbapenem-hydrolyzing beta-lactamase KPC in a Klebsiella pneumoniae isolate from France. Antimicrob Agents Chemother 2005: 49:44234. Pasteran FG, Otaegui L, Guerriero L, Radice G, Maggiora R, Rapoport M, Faccone D, Di Martino A, Galas M Klebsiella pneumoniae carbapenemase-2, Buenos Aires, Argentina.Emerg Infect Dis 2008:14:117880. Samra Z, Ofir O, Lishtzinsky Y, Madar-Shapiro L, Bishara J. Outbreak of carbapenem-resistant Klebsiella pneumoniae producing KPC-3 in a tertiary medical centre in Israel. Int J Antimicrob Agents 2007:30:5259. Schwaber,M.J., Klarfeld-Lidji,S., Navon-Venezia,S., Schwartz,D., Leavitt,A. and Carmeli,Y. (2008) Predictors of carbapenem-resistant Klebsiella pneumoniae acquisition among hospitalized adults and effect of acquisition on mortality. Antimicrob. Agents Chemother. 52, 1028-1033. Stals,A., Werbrouck,H., Baert,L., Botteldoorn,N., Herman,L., Uyttendaele,M. and Van Coillie,E. (2009) Laboratory efforts to eliminate contamination problems in the real-time RT-PCR detection of noroviruses. J. Microbiol. Methods 2009; 77: 72-76. Wei ZQ, Du XX, Yu YS, Shen P, Chen YG, Li LJ. Plasmid mediated KPC-2 in a Klebsiella pneumoniae isolate from China. Antimicrob Agents Chemother 2007: 51:7635. Wendt C, Krause C, Xander LU, Loffler D, Floss H. Prevalence of colonization with vancomycin-resistant enterococci in various population groups in Berlin, Germany. J Hosp Infect 1999; 42:193-200. Woodford N, Zhang J, Warner M, Kaufmann ME, Matos J, Macdonald A, Brudney D, Sompolinsky D, Navon-Venezia S, Livermore DM. Arrival of Klebsiella pneumoniae producing KPC carbapenemase in the United Kingdom. J Antimicrob Chemother 2008: 62: 1261- 4.
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Medical TranscriptionDocument34 pagesMedical TranscriptionAS MBee50% (2)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Instant Healing Meditation (Basic) - David Alan RamsdaleDocument31 pagesInstant Healing Meditation (Basic) - David Alan Ramsdaledeichem88% (8)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- 2021-08-16 MD Anderson RecordsDocument83 pages2021-08-16 MD Anderson RecordsjeffreybodinNo ratings yet
- Idio KinesisDocument4 pagesIdio KinesisdracoscribdNo ratings yet
- Your Health Book - Sampler by Joseph Pilates PDFDocument28 pagesYour Health Book - Sampler by Joseph Pilates PDFMacsim Alexandra50% (2)
- Sieff D.F. 2017 Trauma Worlds and The Wisdom of Marion Woodman AuthorsDocument18 pagesSieff D.F. 2017 Trauma Worlds and The Wisdom of Marion Woodman AuthorsMelissa Viana100% (1)
- Enoxaparin (Lovenox)Document1 pageEnoxaparin (Lovenox)ENo ratings yet
- Points From Accupuncture AtlasDocument1 pagePoints From Accupuncture AtlasdishkuNo ratings yet
- Bikram Yoga MustDocument5 pagesBikram Yoga Mustratnesh vaviaNo ratings yet
- Juvenile Idiopathic ArthritisDocument14 pagesJuvenile Idiopathic ArthritisLuis Enrique Jara Romero100% (1)
- Precautionary and Sanitary Practices in Handling FoodDocument31 pagesPrecautionary and Sanitary Practices in Handling FoodBrenNan ChannelNo ratings yet
- Yoga and Hyperthyroidism PDFDocument16 pagesYoga and Hyperthyroidism PDFRaushan Kumar MishraNo ratings yet
- (Final Proposal) 20181220 Beauttah Migiro Akuma - Research Proposal - Right To Health - Version 1.0Document14 pages(Final Proposal) 20181220 Beauttah Migiro Akuma - Research Proposal - Right To Health - Version 1.0Brian BeauttahNo ratings yet
- Cancer Bush 2013Document2 pagesCancer Bush 2013mghaffarzadehNo ratings yet
- Patient Medical Records: Discharge and Home-Care InstructionsDocument27 pagesPatient Medical Records: Discharge and Home-Care InstructionsAnamaria ManceraNo ratings yet
- Biocare GuidelinesDocument3 pagesBiocare GuidelinesnsjunnarkarNo ratings yet
- List of Instruments For 2nd Year BDSDocument17 pagesList of Instruments For 2nd Year BDSMohammad ShoebNo ratings yet
- A. Instructions Are Available in The Professional Classification Guide As Well As On Our WebsiteDocument2 pagesA. Instructions Are Available in The Professional Classification Guide As Well As On Our WebsiteShamsa JabeenNo ratings yet
- HHS Public AccessDocument16 pagesHHS Public AccessintanNo ratings yet
- The 100 Most Influential Publications in Paracetamol Poisoning TreatmentDocument81 pagesThe 100 Most Influential Publications in Paracetamol Poisoning TreatmentPetrov MihaelaNo ratings yet
- Dealing With PatientDocument14 pagesDealing With PatientAnggih PriyantoNo ratings yet
- 4th Regional Pneumococcal Symposium - DownloadableDocument64 pages4th Regional Pneumococcal Symposium - DownloadablesabinvaccineNo ratings yet
- Orthodontic Appliances: General Requirements of An Orthodontic ApplianceDocument20 pagesOrthodontic Appliances: General Requirements of An Orthodontic ApplianceSafaa GhobNo ratings yet
- AA Dermatologia in MCC 2018Document61 pagesAA Dermatologia in MCC 2018marviNo ratings yet
- Status of DNB Seats - Bulletin - StatewiseSpecialitywise - WU26022009Document142 pagesStatus of DNB Seats - Bulletin - StatewiseSpecialitywise - WU26022009raghavagummadiNo ratings yet
- Animal Welfare Board of India v. A Nagaraja & Ors PDFDocument117 pagesAnimal Welfare Board of India v. A Nagaraja & Ors PDFBar & Bench100% (1)
- Republic of Kenya: Application For Registration of A Health InstitutionDocument13 pagesRepublic of Kenya: Application For Registration of A Health InstitutionianNo ratings yet
- Food Safety HandoutsDocument8 pagesFood Safety HandoutsNurul MaisyaraNo ratings yet
- Ebook Atlas of Interventional Orthopedics Procedures Essential Guide For Fluoroscopy and Ultrasound Guided Procedures PDF Full Chapter PDFDocument68 pagesEbook Atlas of Interventional Orthopedics Procedures Essential Guide For Fluoroscopy and Ultrasound Guided Procedures PDF Full Chapter PDFcharles.schmidt276100% (26)
- Alcoholnew 120916093616 Phpapp02 PDFDocument82 pagesAlcoholnew 120916093616 Phpapp02 PDFNihal S KiranNo ratings yet