Professional Documents
Culture Documents
Malignant Nonodontogenic Tumors: Ewing's Sarcoma
Uploaded by
ahmed mohammed refaiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Malignant Nonodontogenic Tumors: Ewing's Sarcoma
Uploaded by
ahmed mohammed refaiCopyright:
Available Formats
324
PDQ ORAL DISEASE
Malignant Nonodontogenic Tumors
Ewings Sarcoma
Etiology Unknown Chromosomal translocations t(11;22), t(7;22), t(7;21) noted Gene rearrangement often noted, that is, (22;q12) and expression of the MIC2 gene Genetically related to primitive peripheral neuroectodermal tumor via translocations t(11;22), (q24;q12) Clinical Presentation 60% in males; over 95% in those under 20 years of age Chiefly in bone and soft tissues Highly malignant Pain, numbness, and swelling often early complaints Diffuse, irregular, lytic bone lesion Cortical expansion variable Second most common bone tumor of children/adolescents Soft tissues of head and neck account for 11% of extraskeletal sites Diagnosis Radiographs often show moth-eaten appearance and laminar periosteal bone reaction Cortex may be eroded or expanded Differential Diagnosis Osteosarcoma Lymphoma Peripheral neuroectodermal tumor of bone Primitive rhabdomyosarcoma Neuroectodermal tumor of infancy
Malignant Nonodontogenic Tumors
325
Treatment Radiation and multiagent chemotherapy Prognosis 54 to 74% 5-year survival rate in localized osseous form Late relapse not uncommon
326
PDQ ORAL DISEASE
Metastatic Cancer
Etiology Spread of a primary malignancy to the oral cavity structures or jaws (usually from lung, breast, prostate, colon, kidney) Accounts for < 1% of oral malignancies Clinical Presentation Usually manifests in the jaws with pain and swelling Not uncommon is loosening of teeth or pathologic jaw fracture Soft tissue location is rare. Most frequent sites of primary neoplasms are kidney, lung, breast, colon, prostate, stomach Intraosseous lesions with lytic, ill-defined radiolucencies Microscopic Findings As with the primary tumor Tumor marker studies (immunohistochemical) may be necessary to define the site of origin. Diagnosis Radiographic findings Biopsy Differential Diagnosis Primary soft tissue tumor Primary osseous tumor Periodontitis (localized) Osteoradionecrosis Treatment Local radiation Combination chemoradiotherapy Prognosis Poor
Malignant Nonodontogenic Tumors
327
328
PDQ ORAL DISEASE
Osteosarcoma
Etiology May be associated with pre-existing bone disease such as the following: Pagets disease (10 to 15%) Fibrous dysplasia (0.5%) Mutation/amplification of p53, c-myc, c-JUN, c-fos, MOM2, CDK4, SAS Clinical Presentation May present with pain paresthesia, trismus, nasal or paranasal sinus obstruction May masquerade as an odontogenic infection Intraoral signs are as follows: Tooth mobility (vertical) Periapical radiolucency (teeth vital) Distal displacement of terminal molar Jaw mass may be ulcerated. Radiographic Findings Early intraoral findings Displacement of teeth Root resorption Absent or attenuated lamina dura Uniformly widened periodontal membrane space Later jaw bone findings Lytic, moth-eaten destruction Cortical destruction Soft tissue extension Erosion of mandibular canal 25% of cases have sunburst effect (radiating radiopaque spicules) Microscopic Findings Sarcomatous stroma Osteoid production by neoplastic cells Four basic patterns (no prognostic significance) are as follows: Osteoblastic Fibroblastic Chondroblastic Telangiectatic
Malignant Nonodontogenic Tumors
329
Diagnosis Correlation of clinical, radiographic, pathologic findings Differential Diagnosis Fibro-osseous lesion Osteomyelitis Osteoradionecrosis Metastatic tumor Other form of sarcoma Treatment Radical ablative surgery Hemimandibulectomy Partial maxillectomy orbital exenteration Adjuvant chemotherapy/radiotherapy Prognosis Survival ranges from 12 to 58% at 5 years Mandibular lesions are associated with a greater survival rate than are maxillary lesions.
You might also like
- Oral CancerDocument31 pagesOral Cancergita_kamath100% (1)
- PDF Nutrition CM 1 Cu 2 Lab Week 2 1Document6 pagesPDF Nutrition CM 1 Cu 2 Lab Week 2 1HERLIN HOBAYANNo ratings yet
- Chronic Vs Aggressive PeriodontitisDocument7 pagesChronic Vs Aggressive PeriodontitisSvnessa VanessaNo ratings yet
- Apple Snail Health Problems and SolutionsDocument11 pagesApple Snail Health Problems and SolutionsDonya Quick86% (7)
- Odontogenic TumorsDocument14 pagesOdontogenic Tumorskavin_sandhuNo ratings yet
- Non Odontogenic Tumors: Dental ScienceDocument68 pagesNon Odontogenic Tumors: Dental ScienceRealdy PangestuNo ratings yet
- 12-Giant Cell LesionDocument78 pages12-Giant Cell Lesionفراس الموسويNo ratings yet
- AmeloblastomaDocument35 pagesAmeloblastomaAstrid M.No ratings yet
- Odontogenic Keratocyst: or KOTDocument44 pagesOdontogenic Keratocyst: or KOTDrMayank Vermani100% (1)
- Tumors of The Jaw and Oral MucosaDocument18 pagesTumors of The Jaw and Oral MucosaDaniela LeonteNo ratings yet
- Jaw Tumors: DR - Sudipta Bera PDT 1 Year Plastic and Reconstructive Surgery SSKM & IpgmerDocument28 pagesJaw Tumors: DR - Sudipta Bera PDT 1 Year Plastic and Reconstructive Surgery SSKM & Ipgmerdevinchi09No ratings yet
- Odontogenic CystsDocument63 pagesOdontogenic CystsshabeelpnNo ratings yet
- Benign Non-Odontogenic Tumors of Oral CavityDocument64 pagesBenign Non-Odontogenic Tumors of Oral CavityvannaputriwNo ratings yet
- Odontogenic Keratocyst: - Jayalakshmi Preetha Meyyanathan CRIDocument48 pagesOdontogenic Keratocyst: - Jayalakshmi Preetha Meyyanathan CRIJayalakshmi PreethaNo ratings yet
- Basic and Special Suturing Techniques in Surgery. Honlap 2Document57 pagesBasic and Special Suturing Techniques in Surgery. Honlap 2Arif Nurhidayat PrawirohardjoNo ratings yet
- Odontomes & Odontogenic Tumors II (Slide 18+19)Document39 pagesOdontomes & Odontogenic Tumors II (Slide 18+19)JustDen09No ratings yet
- Enamel: DR Saqlain Bin SyedDocument22 pagesEnamel: DR Saqlain Bin SyedNatasha BalochNo ratings yet
- Fasiitis Nekrotikan Tipe Ii: Oktavia R. L. Sondakh Damayanti Tangkidi Herry E. J. PandalekeDocument6 pagesFasiitis Nekrotikan Tipe Ii: Oktavia R. L. Sondakh Damayanti Tangkidi Herry E. J. PandalekemazayaNo ratings yet
- Pharyngeal Arches and Its DerivativesDocument57 pagesPharyngeal Arches and Its DerivativesDr Toqeer AhmedNo ratings yet
- Adenomatoid Odontogenic Tumor: Dr. Ansar Uddin Ahmed Assistant Professor and Head Periodontology and Oral PathologyDocument18 pagesAdenomatoid Odontogenic Tumor: Dr. Ansar Uddin Ahmed Assistant Professor and Head Periodontology and Oral PathologyTas DidNo ratings yet
- Benign Odontogenic Tumors of Jaws (AmeloblastomaDocument70 pagesBenign Odontogenic Tumors of Jaws (Ameloblastomagalina poberezhnikNo ratings yet
- Dentigerous CystDocument25 pagesDentigerous CystDr. Deepanshi SutariaNo ratings yet
- EnamelDocument61 pagesEnamelRehab NaeemNo ratings yet
- Oral LymphangiomaDocument8 pagesOral LymphangiomasevattapillaiNo ratings yet
- A Review of AmeloblastomaDocument23 pagesA Review of Ameloblastomagustian_ballack0% (1)
- Development of Face and TongueDocument51 pagesDevelopment of Face and TongueDR NASIMNo ratings yet
- Verruciform Xanthoma of The Orall CavityDocument3 pagesVerruciform Xanthoma of The Orall CavityLjubomirErdoglijaNo ratings yet
- AbscessDocument40 pagesAbscessMehlaqaNo ratings yet
- Oncology: Study of TumorsDocument32 pagesOncology: Study of TumorsGeorge CherianNo ratings yet
- Clasification of Odontogenic Tumours A ReviewDocument6 pagesClasification of Odontogenic Tumours A ReviewJuan Carlos MeloNo ratings yet
- Giant Cell ReparativeDocument3 pagesGiant Cell ReparativeMedrechEditorialNo ratings yet
- Cleft Lip and PalateDocument54 pagesCleft Lip and PalatewidodoNo ratings yet
- Anestesi LokalDocument12 pagesAnestesi LokalKurniatiKhasanahQhafisaQurratul'ainNo ratings yet
- Neck Dissection PPs PresentationDocument139 pagesNeck Dissection PPs PresentationDrMohmd ZidaanNo ratings yet
- Space InfectionsDocument60 pagesSpace InfectionsDan 04No ratings yet
- Radical Neck Dissection: (RND) Classification, Indication and TechniquesDocument42 pagesRadical Neck Dissection: (RND) Classification, Indication and TechniquesPatrycyaNo ratings yet
- Skin Graf Dan FlapDocument28 pagesSkin Graf Dan FlapAlparisyi MuhamadNo ratings yet
- Fibrous Dysplasia of MaxillaDocument4 pagesFibrous Dysplasia of Maxillasachender_rocksNo ratings yet
- RhabdomyosarcomaDocument12 pagesRhabdomyosarcomaAnonymous 8QktfX9sZ6No ratings yet
- Neck Swellings (Compatibility Mode)Document49 pagesNeck Swellings (Compatibility Mode)vihang146No ratings yet
- Coronectomy TranslaDocument10 pagesCoronectomy TranslaFikri D'el FinzNo ratings yet
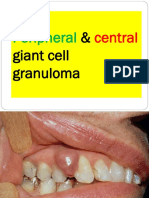
- Peripheral Central Giant Cell Granuloma NXPowerLiteDocument18 pagesPeripheral Central Giant Cell Granuloma NXPowerLiteAFREEN SADAF100% (1)
- Osteomyelitis: Dr. Sunil Pahari 2 Year Resident Department of Orthopedics Yangtze UniversityDocument48 pagesOsteomyelitis: Dr. Sunil Pahari 2 Year Resident Department of Orthopedics Yangtze UniversityPercy Linares MorilloNo ratings yet
- Facial FlapsDocument72 pagesFacial FlapsDrMohmd Zidaan100% (1)
- Anatomy and Physiology of Lacrimal Apparatus: Dr.M.keerthana Dept of OphthalmologyDocument54 pagesAnatomy and Physiology of Lacrimal Apparatus: Dr.M.keerthana Dept of OphthalmologykeerthanaNo ratings yet
- Ossifying FibromaDocument28 pagesOssifying FibromaAkhsanal FauziNo ratings yet
- Auric Recon Slides 070516Document92 pagesAuric Recon Slides 070516Yudhistira AdeNo ratings yet
- Scancleft Speech Assessment PDFDocument16 pagesScancleft Speech Assessment PDFMersal LogeshNo ratings yet
- Bone Tumors and Tumorlike Conditions: Analysis With Conventional RadiographyDocument73 pagesBone Tumors and Tumorlike Conditions: Analysis With Conventional RadiographyViskaNo ratings yet
- Advantages of Uv LedDocument6 pagesAdvantages of Uv LedFatriaNo ratings yet
- Cellinjury 151004125508 Lva1 App6892Document147 pagesCellinjury 151004125508 Lva1 App6892Ajmal RockzzNo ratings yet
- Oral Pathology Lec - 1Document11 pagesOral Pathology Lec - 1مصطفى محمدNo ratings yet
- Anatomi Otot Head & NeckDocument23 pagesAnatomi Otot Head & NeckdanarNo ratings yet
- Cyst Neck Tumor (DR Bob Andinata)Document33 pagesCyst Neck Tumor (DR Bob Andinata)Intan Eklesiana NapitupuluNo ratings yet
- Wound Healing: Santos, Patrick John S., MD First Year Resident Department of Surgery Manila MedDocument60 pagesWound Healing: Santos, Patrick John S., MD First Year Resident Department of Surgery Manila MedJhessie ChingNo ratings yet
- Maxillofacail InjuryDocument37 pagesMaxillofacail InjuryFarhan AliNo ratings yet
- Tarrson Family Endowed Chair in PeriodonticsDocument54 pagesTarrson Family Endowed Chair in PeriodonticsAchyutSinhaNo ratings yet
- Parotid Gland NeoplasmDocument107 pagesParotid Gland NeoplasmigorNo ratings yet
- Needle CricothyroidotomyDocument9 pagesNeedle Cricothyroidotomyhatem alsrour100% (2)
- Spinal Tumors Intra-Extra (Turgut Tali)Document92 pagesSpinal Tumors Intra-Extra (Turgut Tali)Drbaddireddy RayuduNo ratings yet
- Benign Nonodontogenic Tumors: Carotid Body TumorDocument14 pagesBenign Nonodontogenic Tumors: Carotid Body TumorAyeshaNo ratings yet
- Bone Tumours and MalignanciesDocument55 pagesBone Tumours and MalignanciesFreeburn SimunchembuNo ratings yet
- الهامDocument18 pagesالهامmoh.ahm3040No ratings yet
- Anti Microbes in EndodonticsDocument12 pagesAnti Microbes in Endodonticsahmed mohammed refaiNo ratings yet
- Endodontic MicrobiologyDocument12 pagesEndodontic Microbiologyahmed mohammed refaiNo ratings yet
- Endodontic MicrobiologyDocument12 pagesEndodontic Microbiologyahmed mohammed refaiNo ratings yet
- Endodontic MicrobiologyDocument12 pagesEndodontic Microbiologyahmed mohammed refaiNo ratings yet
- ICD-10 Common Codes: Diagnostic ServicesDocument6 pagesICD-10 Common Codes: Diagnostic ServicesAnasNo ratings yet
- Principles of KinesioTaping 2014Document29 pagesPrinciples of KinesioTaping 2014Wijaya Krisna I NyomanNo ratings yet
- Professional BehaviorDocument14 pagesProfessional BehaviorMahmasoni MasdarNo ratings yet
- Epidemiology and Clinical Features of Multiple Sclerosis in Adults Uptodate3Document11 pagesEpidemiology and Clinical Features of Multiple Sclerosis in Adults Uptodate3Régulo RafaelNo ratings yet
- Risk ReportingDocument3 pagesRisk ReportingMiguel TagustosNo ratings yet
- Pompy and IPMA V MBT Et Al Second Amended Compalint 6-23Document60 pagesPompy and IPMA V MBT Et Al Second Amended Compalint 6-23Neil AnandNo ratings yet
- BonvieDocument1 pageBonvieTony Peterz KurewaNo ratings yet
- Acute StressDocument4 pagesAcute StressRafael MadureiraNo ratings yet
- 5stress Can Be Characterized As ''A Condition of Mental or Enthusiastic Strain orDocument5 pages5stress Can Be Characterized As ''A Condition of Mental or Enthusiastic Strain orAravindhan AnbalaganNo ratings yet
- ECTDocument8 pagesECTRoshita G PillaiNo ratings yet
- The Mediterranean DietDocument2 pagesThe Mediterranean DietLuis Miguel Martinez GarciaNo ratings yet
- Development and Initial Validation of The EDIN Scale, A New Tool For Assessing Prolonged Pain in Preterm InfantsDocument6 pagesDevelopment and Initial Validation of The EDIN Scale, A New Tool For Assessing Prolonged Pain in Preterm InfantsmustafasacarNo ratings yet
- 3 Nyc PydpDocument13 pages3 Nyc PydpYang RheaNo ratings yet
- Cancer Research DKFZ 2013 PDFDocument146 pagesCancer Research DKFZ 2013 PDFEvgeniKushchNo ratings yet
- PR2 Chapter1 SleepqualityDocument9 pagesPR2 Chapter1 SleepqualityhoneypiecreamyteaNo ratings yet
- Universidad Abierta para Adultos Escuela:: Ingeniería y TecnologíaDocument3 pagesUniversidad Abierta para Adultos Escuela:: Ingeniería y Tecnologíapolicia nacionalNo ratings yet
- Speech Contest - Stunting in Indonesia2Document2 pagesSpeech Contest - Stunting in Indonesia2Hermawan ChenNo ratings yet
- NCPDocument5 pagesNCPMark John Dela CruzNo ratings yet
- 3a DnDestiny - BestiaryoftheWilds - v0.5Document46 pages3a DnDestiny - BestiaryoftheWilds - v0.5HectorNo ratings yet
- Natural Remedies Encyclopedia (PDFDrive) - 1Document30 pagesNatural Remedies Encyclopedia (PDFDrive) - 1angelobuffalo100% (1)
- Bsnlmrs FormsDocument5 pagesBsnlmrs FormsdurgendraNo ratings yet
- Format of Research ProtocolDocument8 pagesFormat of Research ProtocolCecile Melisse P. DerechoNo ratings yet
- Homework Policy ScotlandDocument9 pagesHomework Policy Scotlandafmtdenav100% (1)
- Recent Advances in The Development of Anti-Tuberculosis Drugs Acting On Multidrug-Resistant Strains: A ReviewDocument18 pagesRecent Advances in The Development of Anti-Tuberculosis Drugs Acting On Multidrug-Resistant Strains: A Reviewmalik003No ratings yet
- Capstone Interview 2Document1 pageCapstone Interview 2api-543753405No ratings yet
- Fri 2022Document95 pagesFri 2022Barbara AsunkaNo ratings yet
- Covid 19 Vaccine Locations Walmart and Sams Clubs Georgia 2-9-21Document3 pagesCovid 19 Vaccine Locations Walmart and Sams Clubs Georgia 2-9-21Michael King50% (4)