Professional Documents
Culture Documents
Case Narrative
Uploaded by
Roeder Max PangramuyenOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Case Narrative
Uploaded by
Roeder Max PangramuyenCopyright:
Available Formats
Quezon Medical Mission Group Hospital and Health Services Cooperative Roeder Max R. Pangramuyen CI -Mrs. Melena V.
. Quintos Related Learning Experience BSN IV SLSU Group 7
CASE NARRATIVE August 04, 2013 is the first day of our exposure and actual handling of patient at QMMG HHSC. From August 04, 2013 August 06, 2013 I handle pt from room 238 A. The patient was Mr. Amador Santiago an 81 y/o male, born on May 1, 1932, Roman Catholic, widowed man, with chief complaint upon admission of pain/numbness on right upper extremities. He was admitted last July 30, 2013 under the service of Dr. Guinto with initial diagnosis of HTN stage II t/c CVA, and low salt low fat diet was ordered.
Upon assessment the patient looks slightly weak in appearance, conscious and coherent oriented to person, place and time with reports of numbness of lower extremities. The patient had increased blood pressure, with productive cough, whitish to yellowish in color, moderate in amount, crackles sound was heard on right lung field upon auscultation and reports of pain upon coughing. The patient due to old age had blurring of vision and hearing impairment. Although the diagnosis was CVA, aside from weakness, there is no marked impairment on patients extremities.
During history taking, the relative reveals that few years ago the patient underwent of surgery due to ulceration intestine. The patient was a drinker, smoker and fond of eating fatty and salty foods on his early years not until her wife died. The patient also had been hypertensive since middle age.
Different treatment was done and different medications had been administered to patient. The patient refused CT scan however medications for CVA were given. Citicoline 500 mg 1 cap TID which acts as brain stimulant was given; ASA 80 mg/tab 1tab OD p/c was given after meals for its Non opiod analgesic, antipyretic and to prevent thrombosis due to CVA and prevent further attacks; Clexane 0.4ml subqutaneous q12 an anticoagulant which deactivates thrombin and prevent coagulation of blood. Fecalysis was ordered to observe for signs of bleeding; it shows
Case Narrative Page 1
Quezon Medical Mission Group Hospital and Health Services Cooperative on the fecalysis result that there was residue of occult blood. Careful monitoring of changes in pts level of consciousness was done.
On x-ray result on July 31, 2013 it reveals that the patient have pneumonia right, cardiomegaly, and atheromatous aorta. Since that the patient had pneumonia, had productive cough and pain upon coughing, the following medications had been administered. Acetylcysteine 60mg 1 tad OD which is dissolved in glass of water was given which act as mucolytic that makes the secretions less viscous; Sinecod Forte 1tab TID was given to suppress cough; Doxofyline 400 mg tab BID, Prednisone 20mg P.O. BID a corticosteroid, both act as bronchodilator. Atrovent q6 was given by respiratory therapist was also given and act as bronchodilator. Zenith 1tab 500mg OD act as anti-infective and bacteriostatic was given to fully eliminate causes of formation of mucus secretions. Deep breathing, coughing was demonstrated to patient for full lung expansion and expels respiratory secretions. Pt was placed on semi fowlers position and head of bed elevated for optimal breathing, back tapping and rubbing was also provided. Pt was encouraged to keep back dry at all times and to increase oral fluid intake but only at least 1l/ day to avoid fluid overload and increase in blood pressure.
Lipid profile results were as follows: cholesterol 166.33mg/dl, triglyceride 101.16mg/dl, HDL 42.44mg/dl and LDL 103.7 mg/dl. CPK-MB result was 9.50 and Trop1 as positive both indicators of heart damaged (related to cardiomegaly and atheromatous aorta). Medications for hypertension and angina were given. Transdermal patch 50mg ACW OD an antianginal (nitroglycerine) and ISMN 30mg 1 tab OD in AM, both reduces oxygen demand by decreasing left ventricular end diastolic pressure and also increases flow through the collateral artery vessels. Amlodipine of 5mg P.O. BID an anti angina inhibits calcium ion influx thus decreasing oxygen demand and also dilates coronary arteries and arterioles and also given for hypertension. Losartan 50mg 1tab OD pm and Catapres 75mg/tab 1tab SL PRN for BP >140/90 was given for hypertension. Clopidogrel hinders platelet aggregation was given to reduce thrombotic events in pt with atherosclerosis documented by recent CVA. Nursing interventions was done such as Monitoring BP and observed for complaints of blurring of vision and
Case Narrative Page 2
Quezon Medical Mission Group Hospital and Health Services Cooperative dizziness, placing client on semi fowlers position to decrease cardiac overload, encouraged to limit oral fluid intake up to 1L/day to minimize or limit increase of blood volume, instructed on low salt low fat diet, instructed to limit or avoid strenuous activities and provided quiet environment, and adequate rest and sleep.
CBC indicates altered tissue perfusion with result of Hgb 100mg/dl, Hct 0.30, RBC 3.4 10^12, and WBC 4.6 10^g/L. Patient was encouraged to do deep breathing exercises and lip pursed breathing, to increase food rich in iron and vitamin C, to perform ROM exercises and to avoid strenuous activities. IVF was regulated on prescribed rate.
SGOT result was 50u/l, which indicates impaired liver function. The patient was administered with Lactulose 20ml ODHS PRN to eliminate feces and to possibly to eliminate ammonia.
FBS show normal result of 100.11mg/dl and Blood uric acid 7.4mg/dl which is slightly elevated. Pt. was encouraged to avoid foods containing large amount of sugar such as soft drinks and chocolates and limit carbohydrates intake; as well as foods rich in uric acid such as organ meat and limit intake of nuts and beans.
Other laboratory results were BUN 4.0 mmol/L which is within normal limits and
Crea 1.7mg/dl which is risk for impaired renal function. The pt was currently on low salt low fat diet and instructed on regular urine elimination and to prevent urine stasis.
On August 05, 2013 final diagnoses were: ACS NSTEMI, CAP moderate risk, COPD acute exacerbation, TIA, HTN stage II, and the patient was ordered may go home, health teachings was given and instructed of take home medications. August 06, 2013 the patient was finally discharged @ 1:30pm in good condition.
Case Narrative
Page 3
You might also like
- Drug Cards CNSDocument23 pagesDrug Cards CNSChristine Schroeder100% (2)
- Womens Gynecologic Health Third EditionDocument912 pagesWomens Gynecologic Health Third Editionmandy nations100% (4)
- Feeding and Eating Disorders GuideDocument42 pagesFeeding and Eating Disorders GuideCharlaine BacasnoNo ratings yet
- DR Walsh Autism Ocd Pandas Depression MethylationDocument6 pagesDR Walsh Autism Ocd Pandas Depression MethylationAnupama PouloseNo ratings yet
- RESUMEDocument4 pagesRESUMERoeder Max PangramuyenNo ratings yet
- RESUMEDocument4 pagesRESUMERoeder Max PangramuyenNo ratings yet
- Cetirizine drug study summaryDocument1 pageCetirizine drug study summaryArthur Christopher Corpuz100% (1)
- Gallstones Case StudyDocument70 pagesGallstones Case StudyIrize DenagaNo ratings yet
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- BFCDocument8 pagesBFCIrene GunongNo ratings yet
- Appendicitis Case StudyDocument35 pagesAppendicitis Case StudyWilliam Soneja CalapiniNo ratings yet
- SLSU College of Allied Medicine Case Study on Bilateral Subdural HematomaDocument27 pagesSLSU College of Allied Medicine Case Study on Bilateral Subdural HematomaRoeder Max Pangramuyen100% (4)
- CASE STUDY TablesDocument9 pagesCASE STUDY TablesMicah MagallanoNo ratings yet
- Family Case StudyDocument32 pagesFamily Case StudyRoeder Max PangramuyenNo ratings yet
- HemodialysisDocument2 pagesHemodialysisjustin_saneNo ratings yet
- Chronic GastritisDocument7 pagesChronic GastritisDivina AquinoNo ratings yet
- A Case Study of Pulmonary TuberculosisDocument28 pagesA Case Study of Pulmonary TuberculosisDyanne BautistaNo ratings yet
- Propranolol 1 PresentationDocument17 pagesPropranolol 1 Presentationapi-284092317100% (1)
- Addison'sDocument4 pagesAddison'sKoRnflakesNo ratings yet
- Nursing Care Acute PancreatitisDocument2 pagesNursing Care Acute PancreatitisJamaica SaranquinNo ratings yet
- Metro Manila Development Screening TestDocument3 pagesMetro Manila Development Screening TestMae PonceNo ratings yet
- Choledolithiasis Cs 103 1Document34 pagesCholedolithiasis Cs 103 1Merlene Sarmiento SalungaNo ratings yet
- NCP GeDocument14 pagesNCP GeSuluhTriUtomoNo ratings yet
- Chronic Obstructive Pulmonary DiseaseDocument76 pagesChronic Obstructive Pulmonary DiseasedidinNo ratings yet
- Case CHFDocument10 pagesCase CHFAgnes Erlita Distriani Patade50% (2)
- ASSESSMENTDocument2 pagesASSESSMENTColeen PequitNo ratings yet
- DP Discharge Plan@@@@@@@@Document6 pagesDP Discharge Plan@@@@@@@@Maemae SumalinogNo ratings yet
- Case Study 1 (Pneumonia)Document13 pagesCase Study 1 (Pneumonia)Kate EscotonNo ratings yet
- Case Report - Deep Vein ThrombosisDocument12 pagesCase Report - Deep Vein ThrombosisAndi Meidin AnugerahNo ratings yet
- Risk For Bleeding - Cirrhosis NCPDocument2 pagesRisk For Bleeding - Cirrhosis NCPPaula AbadNo ratings yet
- Thyroid Lobectomy and IsthmusectomyDocument12 pagesThyroid Lobectomy and IsthmusectomyAgustina100% (1)
- Nursing Care Plan for Hypertension ManagementDocument5 pagesNursing Care Plan for Hypertension Managementbhavana100% (1)
- Tatz Pa ToolDocument23 pagesTatz Pa Toolian_mendoza_3No ratings yet
- Final Case StudyDocument18 pagesFinal Case Studyapi-487702467100% (1)
- Nursing Physical AssessmentDocument5 pagesNursing Physical AssessmentApril Louise PaluganNo ratings yet
- Case Study - Dengue Fever V - S UtiDocument12 pagesCase Study - Dengue Fever V - S UtiHarlene Joyce ReyNo ratings yet
- Managing Electrolyte Imbalances: A Case of Self-Induced HyperkalemiaDocument3 pagesManaging Electrolyte Imbalances: A Case of Self-Induced HyperkalemiaPaul JacksonNo ratings yet
- Managing Fever in a Child with PoliomyelitisDocument4 pagesManaging Fever in a Child with PoliomyelitisMonica RamboyongNo ratings yet
- Case Scenerio Nephrotic SyndromeDocument4 pagesCase Scenerio Nephrotic SyndromeEllen AngelNo ratings yet
- Lesson Plan On HyperlipidemiaDocument4 pagesLesson Plan On HyperlipidemiaBinita Shakya100% (1)
- Liver Cirrhosis Care PlanDocument3 pagesLiver Cirrhosis Care PlanWendy EscalanteNo ratings yet
- A Family Case Study of Real FamilyDocument43 pagesA Family Case Study of Real Familyneo quarto0% (1)
- Pa Tho Physiology PrintDocument4 pagesPa Tho Physiology Printaiconjucea0% (1)
- Course in The WardDocument1 pageCourse in The WardGeevee Naganag VentulaNo ratings yet
- Scribd 020922 Case Study-Oncology A&kDocument2 pagesScribd 020922 Case Study-Oncology A&kKellie DNo ratings yet
- NCP Risk InfectionDocument1 pageNCP Risk InfectionEni RahmawatiNo ratings yet
- Physical Evaluation Checklist For NurseDocument3 pagesPhysical Evaluation Checklist For NurseGiridhar RagavasimhanNo ratings yet
- Nursing Theory: Asthma (Presentation)Document13 pagesNursing Theory: Asthma (Presentation)vinda astri permatasari100% (1)
- PathophysiologyDocument9 pagesPathophysiologySuzette PipoNo ratings yet
- Relationship Between CKD Stage and Pulmonary Edema on Chest X-RayDocument6 pagesRelationship Between CKD Stage and Pulmonary Edema on Chest X-RayAnnisa RabbaniNo ratings yet
- Group B1 (Cholera)Document66 pagesGroup B1 (Cholera)Krisianne Mae Lorenzo FranciscoNo ratings yet
- Cva Case StudyDocument31 pagesCva Case StudyZoe AnnaNo ratings yet
- Experiment 7Document7 pagesExperiment 7kimber_gado100% (2)
- NCP2 - DengueDocument4 pagesNCP2 - DengueSummer SuarezNo ratings yet
- Drug StudyDocument2 pagesDrug Studymegreen GamingNo ratings yet
- Nursing Care PlanDocument13 pagesNursing Care Planyumiko0% (1)
- Case Study in KidneyDocument3 pagesCase Study in KidneyVenice VelascoNo ratings yet
- Hypertensive Cardiovascular DiseaseDocument5 pagesHypertensive Cardiovascular DiseaseAna Katrina OcanaNo ratings yet
- Case Presentation On Chronic Kidney Disease1Document18 pagesCase Presentation On Chronic Kidney Disease1d100% (1)
- SEMINAR On New FilariaDocument50 pagesSEMINAR On New FilariaArun JvNo ratings yet
- Biomedical Case StudyDocument5 pagesBiomedical Case StudyHannan AtharNo ratings yet
- NCP HyperthermiaDocument3 pagesNCP HyperthermiaDhonabelleVanessaFetalinoAdona100% (1)
- NCPDocument15 pagesNCPCamille PinedaNo ratings yet
- Case 1 - Pneumonia (Final)Document4 pagesCase 1 - Pneumonia (Final)Joegie ArioNo ratings yet
- Coughs and Colds Nurse Management of Upper Respiratory Tract InfectionDocument3 pagesCoughs and Colds Nurse Management of Upper Respiratory Tract InfectionMichael Anthony ErmitaNo ratings yet
- Decreased Cardiac OutputDocument4 pagesDecreased Cardiac OutputAdnan Khan100% (1)
- Biliary AtresiaDocument8 pagesBiliary AtresiaBrooke MauriNo ratings yet
- Rectal Mass Prob CADocument26 pagesRectal Mass Prob CARoeder Max PangramuyenNo ratings yet
- Armed Forces of The Philippines Medical CenterDocument5 pagesArmed Forces of The Philippines Medical CenterRoeder Max PangramuyenNo ratings yet
- Communicable Disease According To CuevasDocument2 pagesCommunicable Disease According To CuevasRoeder Max PangramuyenNo ratings yet
- Patient's Name/ Diagnosis Diet IVF Remarks MedicationsDocument7 pagesPatient's Name/ Diagnosis Diet IVF Remarks MedicationsRoeder Max PangramuyenNo ratings yet
- To Identify The Demographic Profile of The Respondents With Regards To: 1.1 Age 1.2 GenderDocument22 pagesTo Identify The Demographic Profile of The Respondents With Regards To: 1.1 Age 1.2 GenderRoeder Max PangramuyenNo ratings yet
- Communicable Disease According To CuevasDocument2 pagesCommunicable Disease According To CuevasRoeder Max PangramuyenNo ratings yet
- Sing and DanceDocument14 pagesSing and DanceRoeder Max PangramuyenNo ratings yet
- Coam Voice OverDocument5 pagesCoam Voice OverRoeder Max PangramuyenNo ratings yet
- Communication 2Document19 pagesCommunication 2Roeder Max PangramuyenNo ratings yet
- COPAR community organizing researchDocument8 pagesCOPAR community organizing researchRoeder Max Pangramuyen0% (1)
- QMMG Hospital CVA Case (38Document4 pagesQMMG Hospital CVA Case (38Roeder Max PangramuyenNo ratings yet
- Case Narrative 3Document4 pagesCase Narrative 3Roeder Max PangramuyenNo ratings yet
- Southern Luzon State University College of Allied Medicine Lucban, QuezonDocument2 pagesSouthern Luzon State University College of Allied Medicine Lucban, QuezonRoeder Max PangramuyenNo ratings yet
- ScienceDocument27 pagesScienceRoeder Max PangramuyenNo ratings yet
- Frequency of Hyponatraemia and Hypokalaemia in Malnourished Children With Acute DiarrhoeaDocument4 pagesFrequency of Hyponatraemia and Hypokalaemia in Malnourished Children With Acute DiarrhoeaRaja Bajak LautNo ratings yet
- HSYLCSyllabus Beijing 2016Document5 pagesHSYLCSyllabus Beijing 2016Akshay SwaminathanNo ratings yet
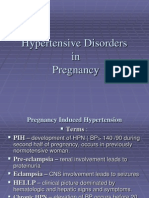
- 001hypertensive Disorders in Pregnancy PDFDocument23 pages001hypertensive Disorders in Pregnancy PDFRosechelle Bas SamsonNo ratings yet
- Golden Rules in OncologyDocument76 pagesGolden Rules in OncologyDragonNo ratings yet
- A Review On The Diseases and Treatments That Affect The Bone Physiology and StrengthDocument17 pagesA Review On The Diseases and Treatments That Affect The Bone Physiology and StrengthErnest Gabriel Cruz AdvinculaNo ratings yet
- Hygiene (NCLEX) Flashcards - QuizletDocument5 pagesHygiene (NCLEX) Flashcards - QuizletA.No ratings yet
- SBAR Communication GuidelinesDocument2 pagesSBAR Communication GuidelinesmonabertNo ratings yet
- Fever: Clinical DescriptionDocument6 pagesFever: Clinical DescriptionNama ManaNo ratings yet
- Clinical Abstract: Bañag, Daraga, Albay Contact Nos.: (Globe) 09271684061 (Smart) 09475160066Document1 pageClinical Abstract: Bañag, Daraga, Albay Contact Nos.: (Globe) 09271684061 (Smart) 09475160066kolintang1No ratings yet
- Emanation of CovidDocument4 pagesEmanation of Covidmarion sebastianNo ratings yet
- Package Insert - BOOSTRIXDocument40 pagesPackage Insert - BOOSTRIXmiguelNo ratings yet
- Poster Ramesh MMDocument5 pagesPoster Ramesh MMRameshKrishnanNo ratings yet
- Seddon and Sunderland Nerve Injury ClassificationDocument8 pagesSeddon and Sunderland Nerve Injury ClassificationAndres AcostaNo ratings yet
- Antibiotic Sensitivity TestDocument10 pagesAntibiotic Sensitivity TestJ.A. LauronNo ratings yet
- Large Databases in Anaesthesiology: ReviewDocument6 pagesLarge Databases in Anaesthesiology: ReviewSoumya DasNo ratings yet
- Magnet Therapy For The Relief of Pain and in Ammation in Rheumatoid Arthritis (CAMBRA) : A Randomised Placebo-Controlled Crossover TrialDocument18 pagesMagnet Therapy For The Relief of Pain and in Ammation in Rheumatoid Arthritis (CAMBRA) : A Randomised Placebo-Controlled Crossover TrialAmr ElDisoukyNo ratings yet
- MS Set 1Document6 pagesMS Set 1Julienne ManabatNo ratings yet
- Bilateral Variation in The Branching Pattern of The Axillary Artery - A Case ReportDocument5 pagesBilateral Variation in The Branching Pattern of The Axillary Artery - A Case ReportIJAR JOURNALNo ratings yet
- POZ 2022 HIV Drug Chart HighDocument5 pagesPOZ 2022 HIV Drug Chart HighManuel S PlasenciaNo ratings yet
- Surveillance of Healthcare-Associated Infections in Indonesian HospitalsDocument12 pagesSurveillance of Healthcare-Associated Infections in Indonesian HospitalsRidha MardiyaniNo ratings yet
- Karsto Akmeņu Masāža INGLIŠ - KopijaDocument10 pagesKarsto Akmeņu Masāža INGLIŠ - KopijaAlise KoblinecaNo ratings yet
- Mendelson's SyndromeDocument17 pagesMendelson's SyndromeYuvetha IndranNo ratings yet
- HPNDocument32 pagesHPNkaren GoNo ratings yet
- Management of The Infant With Atypical Genitalia (Disorder of Sex Development) - UpToDateDocument31 pagesManagement of The Infant With Atypical Genitalia (Disorder of Sex Development) - UpToDateNicolle SchioNo ratings yet
- Hypertensive Renal DiseaseDocument2 pagesHypertensive Renal DiseaseHenry KaweesaNo ratings yet