Professional Documents
Culture Documents
ESSA Exercise and Asthma
Uploaded by
Muhammad TausifCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ESSA Exercise and Asthma
Uploaded by
Muhammad TausifCopyright:
Available Formats
Available online at www.sciencedirect.
com
Journal of Science and Medicine in Sport 14 (2011) 312316
Review
Australian Association for Exercise and Sports Science position statement on exercise and asthma
Alan R. Morton a, , Kenneth D. Fitch a,b
a
School of Sport Science, Exercise & Health, University of Western Australia, Australia b International Olympic Medical Commission, Switzerland
Received 30 August 2010; received in revised form 13 December 2010; accepted 4 February 2011
Abstract Asthma, a chronic inammatory disorder of the airways is associated with variable obstruction to the airways and is provoked by many triggers including exercise. The management of asthma is primarily pharmacological, but exercise, despite causing bronchoconstriction in almost all asthmatics, is an important adjunct to treatment. With adequate control of the hyperresponsive airways obtained with inhaled corticosteroids (ICS) and inhaled beta 2 agonists (IBA), used as both a pre-exercise preventive agent and a reliever if necessary, all asthmatics should benet from an exercise program. Some have realised this benet with such success as to become Olympic and world champions in many sports. Exercise programs should be individually tailored, follow established guidelines and result in similar benets to those obtained by non-asthmatics. However asthmatics must try to avoid or minimise triggers whenever possible. A specic benet of a physical training program is that it allows asthmatics to exercise with less bronchoconstriction at the same exercise stress, although it does not abolish or reduce airway hyperresponsiveness (AHR). 2011 Sports Medicine Australia. Published by Elsevier Ltd. All rights reserved.
Keywords: Exercise; Asthma; Asthma medications; Exercise-induced asthma; Physical activity
Contents
1. 2. 3. 4. 5. 6. 7. Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Role of exercise in the treatment of asthma . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Exercise prescription . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Special considerations . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Contra-indications . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Gaps in the literature . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Conclusions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 312 314 314 315 315 315 316 316
1. Introduction What is asthma? Asthma is dened as a chronic inammatory disorder of the airways involving many cells and cellular elements. The chronic inammation is associated with airway
hyperresponsiveness (AHR) that leads to recurrent episodes of wheezing, breathlessness, chest tightness and coughing. These episodes are commonly associated with widespread, variable obstruction to airow that is mostly reversible either spontaneously or with treatment.1 The airways may be narrowed by one or more of the following: Contraction of the airway smooth muscle (bronchoconstriction), airway swelling (oedema).
Corresponding author. E-mail address: amorton@cyllene.uwa.edu.au (A.R. Morton).
1440-2440/$ see front matter 2011 Sports Medicine Australia. Published by Elsevier Ltd. All rights reserved. doi:10.1016/j.jsams.2011.02.009
A.R. Morton, K.D. Fitch / Journal of Science and Medicine in Sport 14 (2011) 312316
313
Increased production of mucus coupled with inammatory exudates. Thickening of the airways (remodelling) as a consequence of structural changes that are not fully reversible. There are over 2 million asthmatics in Australia including: 1 in 7 primary school children, 1 in 8 teenagers, 1 in 9 adults; and 385 Australians died of asthma in 2007.2 Asthma is a world-wide problem affecting an estimated 300 million persons.1 The prevalence of asthma is greatest in the rst decade of life, occurs amongst members of all races and the rst episode may occur at any age. It is more common in boys than girls (3:2 ratio) and in older women than older men.3 Many factors or triggers provoke asthma including: allergens, cold air, exercise, infections, pollutants, and some drugs. Allergens may be indoor, including house-dust mites, pets notably cats and dogs, fungi and specic foods or outdoor, especially pollens. The primary indoor pollutant is cigarette smoke, both passive and active (smokers) and also chloramines in indoor swimming pools. Outdoor pollutants are predominately air pollutants such as particulate matter (PM) from combustion engines and dust from the construction industry. Others include ozone, nitrogen oxides, sulphur dioxide and carbon monoxide. Drugs that can provoke bronchoconstriction include beta blockers and non steroidal anti-inammatory drugs (NSAID). The response to these triggers varies amongst asthmatics and even in the same asthmatic at different times. The severity of asthma can range from occasional episodes of breathing discomfort to frequent serious life-threatening bouts of airways obstruction. The vast majority of asthmatics will experience bronchoconstriction provoked by exercise which for many years was termed exercise induced asthma (EIA). A small minority develop bronchoconstriction only after exercise which some authorities have called exercise-induced bronchoconstriction (EIB). However, EIB, which is a self-explanatory term, is employed by most experts for both and will be used throughout. There has been debate as to whether respiratory heat loss or water loss is the primary cause of EIB with the latter now generally accepted as having the major role.4 Because of the hyperpnoea that accompanies exercise, the lungs are unable to adequately humidify these increased volumes of inspired air, resulting in evaporative water loss with drying and cooling of the airways. This releases inammatory mediators and over time results in damage to the airways. These mediators, including prostaglandins and cysteinyl-leukotrienes, cause contraction of airway smooth muscle and altered vascular permeability.5 The resultant bronchoconstriction is assessed by measuring the forced expiratory volume in one second (FEV1) which is compared with baseline FEV1 prior to an exercise challenge. EIB is accepted by the American Thoracic Society6 as a fall of 10% or greater from the baseline FEV1 after a standard exercise challenge of 68 min duration. Currently, exercise challenge tests are being superseded by indirect bronchial provocation tests such as mannitol,
eucapnic voluntary hyperpnoea (EVH) and hypertonic saline challenge tests.7 Airway hyperresponsiveness can also be conrmed by a bronchodilator test, positive if a 12% or greater increase in FEV1 occurs after inhaling a rapidly acting IBA.8 Because breathlessness is normal after all but lowintensity exercise, many asthmatics are unaware that they develop EIB post exercise. They assume that their dyspnoea is just lack of tness, fail to seek medical advice, and exercise at a disadvantage because of a lack of appropriate medication. Because of asthma and EIB, many asthmatics avoid exercise which results in low aerobic tness and at times, obesity. By contrast, there is evidence that a number of elite athletes have been mistakenly diagnosed with asthma and treated but do not have either asthma or EIB.9 Of the 266 athletes in the 2004 British Olympic team, asthma was misdiagnosed in 21% but undiagnosed in 2.6%.10 How is asthma managed? Poorly treated asthma can be a very debilitating condition. However, by following a suitably prepared management program, developed with a knowledgeable physician, an asthmatic can lead a full and active life. An Asthma Action Plan11 is a written set of instructions developed for each asthmatic assisting him/her to recognise worsening asthma symptoms, promptly modify treatment as the plan instructs and seek appropriate medical assistance. The asthmatic and his/her family must understand how to provide asthma rst-aid. Brochures covering the rst-aid procedures are available from all State Asthma Foundations. It is recommended that physicians also develop an EIB Action Plan in addition to the general Asthma Action Plan for their patients and emphasize that it is difcult to prevent EIB if asthma is not adequately controlled. As part of the Asthma Action Plan, it is recommended that asthmatics purchase an inexpensive peak ow meter or FEV1 meter and monitor their lung function on a regular basis. Change in peak ow values or FEV1 values may signal the need to modify dosage or type of medication. Asthma medications are categorized by Global Initiative for Asthma (GINA)1 into two main groups: (i) Controllers and (ii) Relievers. Controllers are usually taken daily with the aim of reducing the inammatory mechanisms associated with asthma. Inhaled glucocorticosteroids (ICS) including beclomethasone, budesonide, ciclesonide and uticasone are the mainstay and are assisted by the long acting inhaled beta 2 adrenoceptor agonists (IBA) formoterol and salmeterol, and at times, add-on agents, the leukotriene receptor antagonists (LTRA) such as oral montelukast and/or the cromones, inhaled cromoglicate and nedocromil. Other controller medications include oral anti-IGE therapy with omalizumab which is expensive and of value only in severe IGE-mediated allergic asthma and oral theophylline, rarely used today.6 Relievers of which the principal group are the rapidly acting IBA such as inhaled salbutamol and terbutaline are effective in relieving bronchoconstriction and should be inhaled only when needed and in the lowest dose necessary. Increased need and use of these agents is indicative of loss
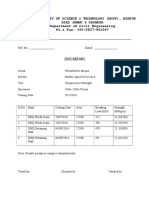
314 Table 1 Prevention of EIA/EIB.
A.R. Morton, K.D. Fitch / Journal of Science and Medicine in Sport 14 (2011) 312316
Obtain good control of asthma with ICS Add LABA and when necessary LTRA, chromones, anticholinergics (rarely) Ensure appropriate care of MDI and spacers Pre-exercise warm-up Pre-exercise medication SABA LTRAs and/or chromones (uncommonly) Avoid unfavourable environmental conditions when possible Reduce the effects of cold air with masks during training Key: ICS, inhaled corticosteroids; LABA, long acting IBA; LTRA, leukotriene receptor antagonists; SABA, short (and rapid) acting IBA.
level of exercise can be carried out at a reduced percentage of his or her VO2 max , so providing a lesser stimulus for EIB.16 Psychological benets follow and countless asthmatics have become elite athletes, and world and Olympic champions despite some having severe asthma. Between episodes of asthma, in many asthmatics the cardiorespiratory system is normal and does not interfere with physical performance. However, if an asthmatic exercises with signicant airways constriction, exercise performance will be impaired.
3. Exercise prescription With the benet of pre-exercise medication, the majority of asthmatics can participate equally with non-asthmatics of similar size, skill and tness level. As the training programme for an elite athlete in any given sport is the same regardless of whether he/she is asthmatic or non-asthmatic, only a general aerobic tness programme will be outlined here. The management of asthma in the elite athlete, with the many additional problems caused by long-term intense endurance training, particularly in unfavourable environments, has been recently detailed.8 Warm-up. All training sessions and games should be preceded by a warm-up, which continues at least until mild sweating occurs. The warm-up should consist of rhythmic low-level activity such as walking progressing to jogging or equivalents for other modes of activity. This should be followed by some light exibility exercises for major muscle groups, with a special emphasis on those muscles involved in the specic activity or event. A period of strengthening exercises for the same muscles can also be included. An early warm-up session may produce a refractory period which is considered to be a useful preventive time during which a person has a reduced propensity to develop EIB.17 The aerobic segment. Exercise should begin at a low level of intensity and gradually increase in severity as the tness level improves. The aim should be to stress the system without straining it. The activity should utilize large muscle groups in a rhythmic fashion such as in walking, jogging, running, cycling, swimming and various endurance game activities. The intensity should be such that it exceeds the threshold required for cardiorespiratory improvement; thus an intensity of 4060% of ones Oxygen Uptake Reserve is recommended. When prescribing exercise it is recommended that the guidelines provided by the American College of Sports Medicine are observed.18 Duration and frequency. Each session should last between 20 and 60 min and 35 times a week is adequate. Initially, the very unt may need to limit sessions to 20 min but should aim to increase the duration to a minimum of 30 min. Greater improvement will occur with more frequent sessions. Exercise loading. If the asthmatic is unt, the programme should commence with continuous walking, as this has a low asthmagenicity and prepares the muscles for future higher
of control of asthma and a review of the treatment regime is essential. Other relievers include anticholinergics such as inhaled ipratropium and systemic glucocorticosteroids, which are mostly taken orally for severe exacerbations of asthma that are unresponsive to inhaled therapy.1 A third category, preventers, may be added when discussing EIB. These are the rapidly acting IBA which are inhaled pre-exercise and are very effective in preventing EIB in the majority of persons. Long acting IBA are useful in physical or sporting activities of longer than 90120 min duration. Other medications with a lesser role as preventers include cromones and LTRA. Daily use of IBA, both rapid acting and long acting, can induce tolerance with loss of their effectiveness as preventers of EIB and relievers of asthma and EIB and additionally, increased severity of asthma and EIB.12 This tolerance which is not prevented by concomitant use of ICS, is rapidly reversed by ceasing daily IBA for a few days.13 Long acting IBA should never be prescribed as monotherapy and must be inhaled in association with an ICS.14 Because most medications for asthma and EIB are inhaled, optimum use of inhalers is important, but it is not commonly achieved. Asthmatics must be taught how to use their metered dose inhaler (MDI) to ensure that all of the drug(s) is administered into the lungs and not deposited in the oropharynx. The use of a spacer with an MDI will assist. Care of the MDI including regular washing of the mouth piece and the spacer is important but is often neglected6 (Table 1). For asthmatics participating in elite sporting events, drug therapy must meet the requirements of the World Anti-Doping Agency.15
2. Role of exercise in the treatment of asthma The primary management of asthma and EIB is pharmacological with exercise having a secondary role. The role of exercise is to assist asthmatics to lead as normal a physical lifestyle as possible, which should allow participation in sports. Regular exercise should be part of the lifestyle of all humans to maintain health and tness. A major benet of regular exercise for asthmatics is improved aerobic tness (i.e. Increased VO2 max ) which means that a given
A.R. Morton, K.D. Fitch / Journal of Science and Medicine in Sport 14 (2011) 312316
315
intensity exercise. As the tness level improves, especially of the musculoskeletal system, one can increase the intensity by progressing to low-level interval training consisting of walking and jogging and later continuous running. One can progress to high intensity exercise, using training intervals of 1030 s followed by 3090 s rest periods. Many team sports are ideal, as they require an intermittent pattern of energy expenditure. Regular or frequent participation in tness programs necessitates an adequate level of enjoyment and such activities that are predominately aerobic and interesting are therefore preferred. In general, the prescription of training for individual asthmatics should be based on the types of exercise they prefer. Because it is less asthmagenic and benets the respiratory system, swimming remains an excellent activity for asthmatics although problems of breathing air contaminated with chloramines in indoor pools remains a concern. Whenever possible non-chlorinated indoor pools should be used. If only chlorinated pools are available, outdoor locations are better. Warm-down. Every training session or game should be followed by a warm-down (or cool-down) segment. This can be accomplished by continuing light rhythmic activities such as walking until the heart rate returns to within about 20 beats min1 of the pre-exercise level. The warm-down segment should conclude with a repetition of the exibility exercise regime performed during warm-up.
5. Contra-indications It is important to exercise only if controller and preventive medications have been administered pre-exercise. Reliever medication, rapid acting IBA, should always be available to reverse EIB should it occur. Should this be unsuccessful, asthmatics should cease exercise or continue with caution. The availability of a peak ow meter or FEV1 meter is prudent and if the peak ow value or FEV1 value is less than 75% of normal, exercise is unwise. Performing vigorous physical activities while the airways are signicantly constricted can lead to a severe drop in the arterial oxygen saturation, accumulation of carbon dioxide and hyperination of the lungs with an increased residual volume. Severe dyspnoea and worsening of the bronchoconstriction with fatigue of the respiratory muscles may ensue. Death from asthma during exercise is rare but can occur.22 Scuba diving is a sport that poses signicant dangers for all participants and this is especially true for asthmatics who are generally advised to avoid it. Those with chronic or poorly controlled or labile asthma should never dive. In Australia, it is necessary for all intending scuba divers to pass a diving medical examination performed by a diving medical doctor before being certied as t to scuba dive. Recently some persons with mild to moderate well controlled asthma have been permitted to dive. Spirometry must not reveal chronic airways obstruction and a negative bronchial provocation test with hypertonic saline is mandatory for some authorities.23 The physical exertion involved with scuba, the inhalation of dry, cold compressed air and the possibility of inhaling salt or fresh water can cause airways obstruction, air trapping and hyperination of the lungs. This increases the chance of pulmonary barotrauma and pneumothorax as the diver returns to the surface. Barotrauma allows air to be introduced directly into the blood and travel to the brain and can cause a fatal air embolism.24
4. Special considerations Road cyclists and runners are at risk of developing airway hyperresponsiveness due to inspiring signicant quantities PM from vehicle emissions while ice athletes including skaters and ice hockey players have been demonstrated to be prone to AHR from inhaling PM from diesel powered zambonis (ice resurfacing machines).19 Although swimming has been long favoured as the optimal exercise for asthmatics because it provokes less EIB than running and cycling, research has demonstrated that interaction between chlorine gas and inorganic compounds causes the production of chloramines, notably nitrogen trichloride which is highly irritating to the lungs. These have been incriminated as a likely factor in increased asthma in very young children20 and adolescents21 who are exposed to these gases in indoor swimming pools. Endurance athletes training in cold climates are at risk of sustaining injury to their airways because of breathing large volumes of cold dry air when respiratory heat loss is superimposed on water loss. Over time, this may result in remodelling of the airways. Avoiding training in extremely cold conditions and using surgical face masks and similar devices have been benecial during training sessions to warm and humidify the inspired air but cannot be used in competition.5 Occasionally weather alerts advise asthmatics not to exercise outdoors and should be heeded.
6. Gaps in the literature Since a swimming study examining the effects of ve months swimming training (mostly in outdoor pools) on 46 asthmatic children was published more than three decades ago,25 few comparable studies have followed,26 with only one27 that can be construed as including an adequate period of training. There is a major need for others. Recent studies appear to demonstrate that many elite endurance athletes in sports where training is performed in an environment which is challenging to the respiratory system such as road cyclists, swimmers, skaters, ice hockey players, triathletes, cross country skiers and biathletes may develop asthma and/or AHR as a consequence of years of training.8 Indeed, asthma is the most common medical condition experienced by Olympic athletes with >7% of athletes have been conrmed to have asthma at each Olympic Games 2006, 2008 and 2010.28 Further research is necessary and also to determine if after cessation of endurance training in such
316
A.R. Morton, K.D. Fitch / Journal of Science and Medicine in Sport 14 (2011) 312316 9. Turcotte H, Langdeau JB, Thibault G, et al. Prevalence of respiratory symptoms in an athlete population. Respir Med 2003;97:95563. 10. Dickinson JW, Whyte GP, McConnell AK, et al. Impact of changes in the IOC-MC asthma criteria: a British perspective. Thorax 2005;60:62932. 11. National Asthma Council Australia. Asthma Management Handbook 2006, South Melbourne. The National Asthma Council of Australia; 2006. 12. Haney S, Hancox RJ. Rapid onset of tolerance to beta-agonist bronchodilation. Respir Med 2005;99(5):56671. 13. Haney S, Hancox RJ. Recovery from bronchoconstriction and bronchodilator tolerance. Clin Rev Allergy Immunol 2006;31(23):8196. 14. Chowdhury BA, Dal Pan G. The FDA and safe use of long acting beta 2 agonists in the treatment of asthma. NEJM 2010;362(13):116971. 15. http://www.wada-ama.org/en/Science-Medicine/Prohibited-List/ [accessed 18.3.10]. 16. Henriksen JM, Nielsen TT. Effect of physical training on exerciseinduced bronchoconstriction. Acta Paediatr Scand 1983;72(1):316. 17. McKenzie DC, McLuckie SL, Stirling DR. The protective effects of continuous and interval exercise in athletes with exercise-induced asthma. Med Sci Sports Exerc 1994;26(8):9516. 18. American College of Sports Medicine. ACSMs guidelines for exercise testing and exercise prescription. 8th ed. Baltimore: Lippincott, Williams &Wilkins; 2009. 19. Rundell KW. Pulmonary function decay in women ice hockey players: is there a relationship to ice rink air quality? Inhal Toxicol 2004;16(3):11723. 20. Weisel CP, Richardson SD, Nemery B, et al. Childhood asthma and environmental exposures at swimming pools; state of the science and research recommendations. Environ Health Perspect 2009;117(4):5007. 21. Bernard A, Nickmilder M, Voisin C. Outdoor swimming pools and the risks of asthma and allergies during adolescence. Eur Respir J 2008;32:97988. 22. Becker JM, Rogers J, Rossini G, et al. Asthma deaths during sports: report of a 7-year experience. J Allergy Clin Immunol 2006;113(2):2647. 23. Joos GF, OConnor B, Anderson SD, et al. Indirect airway challenges. Eur Respir J 2003;21:195868. 24. Lynch JH, Bove AA. Diving medicine: a review of current evidence. J Am Board Fam Med 2009;22(4):399407. 25. Fitch KD, Morton AR, Blanksby BA. Effect of swimming training on children with asthma. Arch Dis Childh 1976;51(3):1904. 26. Ram FS, Robinson SM, Black PN, et al. Physical training for asthma. Cochrane Data Base Syst Rev 2005;(October (4)):CD001116. 27. Arandelovo c M, Stabkovi c I, Nikoli c M. Swimming and persons with mild persistent asthma. Sci World J 2007;7(August):11828. 28. Boulet LP, Hancox RJ, Fitch KD. Exercise challenge and asthma: beta 2 agonists and the competitive athlete. Breathe 2010;7:647. 29. Helenius I, Rytil P, Sarna S, et al. Effect of continuing or nishing highlevel sports on airway inammation, bronchial hyperresponsiveness, and asthma: a 5-year prospective follow-up study of 42 highly trained swimmers. J Allergy Clin Immunol 2002;109(6):96280.
environments, the AHR will cease, as shown in elite Finnish swimmers.29
7. Conclusions Although exercise can induce EIB, regular physical activity is an important component in the management of asthma. It is critical to obtain adequate control of asthma with controller medication to minimise EIB. All asthmatics should have and adhere to a personalised Asthma Action plan and monitoring the state of their airways with a peak ow meter or FEV1 meter is recommended. The use of pre-exercise medication allows most asthmatics to perform in exercise and sporting events with mild or no disadvantage. The success of asthmatics at the highest levels, in almost all sports, is testimony to the benets of exercise in overcoming their disability and a stimulus for others to include physical activity and sports in their daily lives.
References
1. Global Initiative for Asthma. Global strategy for asthma management and prevention; 2009. http://www.ginasthma.org [cited 17.3.10]. 2. The Australian Government Health Institute Newsletter 11 February 2010. 3. Morton AR, Fitch KD. Asthma. In: Skinner JS, editor. Exercise testing and exercise prescription for special cases. 3rd ed. Philadelphia: Lea & Fibiger; 2005 [chapter 16]. 4. Anderson SD, Kippelen P. Airway injury as a mechanism for exerciseinduced bronchoconstriction in elite athletes. J Allergy Clin Immunol 2008;122(2):22535. 5. Fitch KD. Pharmacotherapy for exercise-induced asthma: allowing normal levels of activity and sport. Exp Rev Clin Pharmacol 2010;3(1):13952. 6. Crapo RO, Casaburi R, Coates AL, et al. Guidelines for methacholine and exercise challenge testing 1999. Ofcial statement of the American Thoracic Society. Am J Respir Crit Care Med 2000;161(1): 30929. 7. Rundell KW, Slee JB. Exercise and other indirect challenges to demonstrate asthma or exercise-induced bronchoconstriction in athletes. J Allergy Clin Immunol 2008;122(2):23846. 8. Fitch KD, Sue-Chu M, Anderson SD, et al. Asthma and the elite athlete: summary of the International Olympic Committees consensus conference, Lausanne, Switzerland, January 2224, 2008. J Allergy Clin Immunol 2008;122(2):25460, 260.e17.
You might also like
- The Chairman, Civil Engineering Department, MUSTDocument1 pageThe Chairman, Civil Engineering Department, MUSTMuhammad TausifNo ratings yet
- Scanned by TapscannerDocument15 pagesScanned by TapscannerMuhammad TausifNo ratings yet
- Payment Sectaxpayer - NTN Taxpayer - Cnic Taxpayer - Name Taxpayer - City Taxpayer - Addr Taxpayer - Sta Taxpayer - Taxable - Amount Tax - AmountDocument7 pagesPayment Sectaxpayer - NTN Taxpayer - Cnic Taxpayer - Name Taxpayer - City Taxpayer - Addr Taxpayer - Sta Taxpayer - Taxable - Amount Tax - AmountMuhammad TausifNo ratings yet
- Zircon Sales Tax 1Document1 pageZircon Sales Tax 1Muhammad TausifNo ratings yet
- University of Engineering & Technology Taxila: Admission NoticeDocument1 pageUniversity of Engineering & Technology Taxila: Admission NoticeMuhammad TausifNo ratings yet
- Mirpur University of Science & Technology (Must), Mirpur Azad Jammu & Kashmir Department of Civil Engineering PH & Fax: +92-5827-961047Document2 pagesMirpur University of Science & Technology (Must), Mirpur Azad Jammu & Kashmir Department of Civil Engineering PH & Fax: +92-5827-961047Muhammad TausifNo ratings yet
- DedicationDocument1 pageDedicationMuhammad TausifNo ratings yet
- DedicationDocument1 pageDedicationMuhammad TausifNo ratings yet
- Answer - Darul Ifta Deoband IndiaDocument1 pageAnswer - Darul Ifta Deoband IndiaMuhammad TausifNo ratings yet
- Introduction 1Document3 pagesIntroduction 1Muhammad TausifNo ratings yet
- Experimental Work CHP 7Document47 pagesExperimental Work CHP 7Muhammad TausifNo ratings yet
- Method For Reducing of Noise by ImprovingDocument6 pagesMethod For Reducing of Noise by ImprovingMuhammad TausifNo ratings yet
- 70-c0807 C c810 C c820 C Rev 5 GB 13 Lug 2005Document47 pages70-c0807 C c810 C c820 C Rev 5 GB 13 Lug 2005Muhammad Tausif0% (1)
- Ferrocement ReferencesDocument2 pagesFerrocement ReferencesMuhammad TausifNo ratings yet
- Introduction To Molecular Spectroscopy: By: M.Z.IqbalDocument24 pagesIntroduction To Molecular Spectroscopy: By: M.Z.IqbalMuhammad TausifNo ratings yet
- Chapter No 3Document13 pagesChapter No 3Muhammad TausifNo ratings yet
- Chapter No 5Document15 pagesChapter No 5Muhammad TausifNo ratings yet
- Consumables Are Goods That Require Recurrent Replacement Because They Are Used Up or Transformed in Their UseDocument12 pagesConsumables Are Goods That Require Recurrent Replacement Because They Are Used Up or Transformed in Their UseMuhammad TausifNo ratings yet
- Unit 5 LipidsDocument71 pagesUnit 5 LipidsMuhammad TausifNo ratings yet
- Advanced Vibration and Overpressure Monito R: Easy To UseDocument3 pagesAdvanced Vibration and Overpressure Monito R: Easy To UseMuhammad TausifNo ratings yet
- Presentation 1Document20 pagesPresentation 1Muhammad TausifNo ratings yet
- Daily AllowanceDocument31 pagesDaily Allowanceshafek100% (1)
- Signal-to-Noise RatioDocument5 pagesSignal-to-Noise RatioMuhammad TausifNo ratings yet
- Chapter No 2 Introduction To FerrocementDocument19 pagesChapter No 2 Introduction To FerrocementMuhammad TausifNo ratings yet
- WaxDocument5 pagesWaxMuhammad TausifNo ratings yet
- Board of Intermediate & Secondary Education Rawalpindi: Result of SSC Annual Examination 2014Document2 pagesBoard of Intermediate & Secondary Education Rawalpindi: Result of SSC Annual Examination 2014Muhammad TausifNo ratings yet
- Board of Intermediate & Secondary Education Rawalpindi: Result of SSC Annual Examination 2014Document2 pagesBoard of Intermediate & Secondary Education Rawalpindi: Result of SSC Annual Examination 2014Muhammad TausifNo ratings yet
- Semester Registration 2K10Document12 pagesSemester Registration 2K10Muhammad TausifNo ratings yet
- Short Questions Ch-3Document3 pagesShort Questions Ch-3Muhammad TausifNo ratings yet
- Mcqs Chapter 7Document1 pageMcqs Chapter 7Muhammad TausifNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Manipulating Reps For Gains in Size and Strength by Charles PoliquinDocument6 pagesManipulating Reps For Gains in Size and Strength by Charles Poliquinnam nguyenNo ratings yet
- SSTT X Jamal Browner 12 Week Vol. 4Document349 pagesSSTT X Jamal Browner 12 Week Vol. 4Uggleklockan54% (13)
- Session-13 0810 LDocument30 pagesSession-13 0810 Lcarhuazrca9226No ratings yet
- A Systematic Review of Rehabilitation Exercises To Progressively Load Gluteus Medius - 2016Document36 pagesA Systematic Review of Rehabilitation Exercises To Progressively Load Gluteus Medius - 2016Bruno HenriqueNo ratings yet
- Module 1 and 2 Path Fit 3Document9 pagesModule 1 and 2 Path Fit 3Julius Orquillas PatrollaNo ratings yet
- Metabolic Condition 2003Document4 pagesMetabolic Condition 2003Crischentian BrinzaNo ratings yet
- 100 Tabata Workouts PDFDocument33 pages100 Tabata Workouts PDFharris81No ratings yet
- Nutrition PresentationDocument25 pagesNutrition PresentationChris KaskyNo ratings yet
- 60 Min Beginner Yoga ClassDocument2 pages60 Min Beginner Yoga ClassTerapie logopedica100% (1)
- 2019 KPREAA Elementary Track and Field Meet Board-Wide ResultsDocument30 pages2019 KPREAA Elementary Track and Field Meet Board-Wide ResultsPeterborough Examiner0% (1)
- Westside Barbell ProgramDocument11 pagesWestside Barbell ProgramhelmetheadbobNo ratings yet
- 800 and 1600 Training PDFDocument15 pages800 and 1600 Training PDFsashiNo ratings yet
- Book 5 Obesity - in - Youth - Causes - Consequences - and - Cures PDFDocument255 pagesBook 5 Obesity - in - Youth - Causes - Consequences - and - Cures PDFAnomali RebornNo ratings yet
- 3x5 Squat 3x5 Bench Press 1x5 Deadlift 3x15 Chin-Up: Workout ADocument1 page3x5 Squat 3x5 Bench Press 1x5 Deadlift 3x15 Chin-Up: Workout ADavid AbrahamsNo ratings yet
- Penn State Club Track RecordsDocument8 pagesPenn State Club Track Recordsapi-610935042No ratings yet
- Social Dance An Dance MixersDocument15 pagesSocial Dance An Dance MixersMargarita AmascualNo ratings yet
- Full Body WorkoutDocument1 pageFull Body WorkoutNuman FarooqiNo ratings yet
- The Crossfit Kids Startup CurriculumDocument107 pagesThe Crossfit Kids Startup Curriculumsimserum100% (3)
- Projek PJK 2015Document22 pagesProjek PJK 2015Ethan Tai Hao XianNo ratings yet
- Built by Science Daily Trainer - Day 3, BackDocument7 pagesBuilt by Science Daily Trainer - Day 3, BackAlbert TamaiNo ratings yet
- Health-Related Fitness Components PDFDocument4 pagesHealth-Related Fitness Components PDFCzar Paulo DabonNo ratings yet
- Obesity and PregnancyDocument39 pagesObesity and PregnancyxxdrivexxNo ratings yet
- Shiva SamhitaDocument1 pageShiva SamhitanieotyagiNo ratings yet
- Functional Training ManualDocument25 pagesFunctional Training Manualsanselmi92% (12)
- 2018 05 01 Shape SingaporeDocument108 pages2018 05 01 Shape SingaporeMitch YeohNo ratings yet
- Path Fit 2 Course Outlinedocx PDF FreeDocument2 pagesPath Fit 2 Course Outlinedocx PDF FreeNickaela Marie SenoraNo ratings yet
- Piano Exercises Book 1 Introduction: TH THDocument6 pagesPiano Exercises Book 1 Introduction: TH THArmin ParvinNo ratings yet
- 01 - Beyond 5-3-1 - Jim Wendler ProgramDocument7 pages01 - Beyond 5-3-1 - Jim Wendler ProgramVinicius BittencourtNo ratings yet
- GRADES 1 To 12 Daily Lesson Plan: MAPEH (P.E.)Document4 pagesGRADES 1 To 12 Daily Lesson Plan: MAPEH (P.E.)KenotNotsniwOnaromNo ratings yet
- Hypertension - PPT RKDocument31 pagesHypertension - PPT RKseetaramanath100% (1)