Professional Documents
Culture Documents
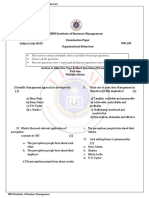
Ob Concept RMR
Uploaded by
Richard S. RoxasOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ob Concept RMR
Uploaded by
Richard S. RoxasCopyright:
Available Formats
1
HEALTH PERIOD
PROMOTION
DURING
INTRAPARTAL
LABOR AND DELIVERY INITIATION OF LABOR - The exact cause that initiates labor is unknown. Theories Include: 1. Uterine Stretch Theory - uterus becomes stretched and pressure increases that results in release of prostaglandin resulting to contractions. 2. Oxytocin Theory - due to gradual rise in the amount of circulating oxytocin. Pressure on the cervix, which stimulates the release of oxytocin from the posterior pituitary. 3. Progesterone Deprivation Theory - as pregnancy advances progesterone contractions. 4. Prostaglandin Theory increased production of prostaglandins by fetal membranes and uterine decidua as pregnancy advances. FETUS produces increased level of cortisol that inhibits progesterone production by the placenta. Placental Age This triggers contractions at a set point. is less effective in controlling uterine
COMPONENTS OF LABOR PROCESS A. Pelvic Dimension (passage) - adequacy of the of the size of the pelvis and contour. B. Fetal Dimension (passenger) - includes fetal size, position, lie, presentation and attitude. C. Uterine Contractions (power) - successful labor depends on uterine contractions occurring at regular interval and adequate intensity. D. Psychological Response (Psyche) must be preserved. PASSAGE Route a fetus must travel from the uterus through the cervix and vagina to the external perineum. The fetus must pass through the bony pelvis because the cervix and vagina are contained inside it. Clinical Pelvimetry: 1. Pelvic Inlet assessed by measuring the diagonal conjugate. The lower pubic border to the sacral promontory is measured. 2. Midpelvis assessed by measuring the bi-ischial diameter. The ischial spines, sacrospinous ligaments and sacrosciatic notch are palpated.
3. Pelvic Outlet assessed by measuring the angle of the pubic arch. The subpubic arch should be assessed and the ischial tuberosities should be palpated. Pelvic Measurements: to determine the adequacy of the pelvic size 1. Diagonal conjugate Anterior-posterior diameter of the inlet. Narrowest diameter of the inlet. 2. Transverse diameter of the outlet Narrowest diameter of the outlet. Clinical Importance: If a disproportion between fetus and the pelvis occur, the infant cannot be born vaginally. Emphasize that it is the pelvis that is too small, not that the head is too big.
PASSANGER 1. Structure of the Fetal Skull 2. Diameters of the Fetal Skull 3. Fetal Presentation and Position 4. Mechanisms of Labor
STRUCTURE OF THE FETAL SKULL Head has the widest diameter of the body part of the fetus. - making it least likely to pass through the pelvic ring. 1. Cranium uppermost portion of the skull 8 bones of the cranium: 1. 4 superior bones Frontal bone (fused) two parietal bones and occipital bone. 2. Sphenoid, ethmoid, two temporal bones. 2. Suture Lines membranous interspaces where the bones of the skull meet. 1. Sagittal suture joins the two parietal bones of the skull. 2. Coronal suture line of juncture of the frontal bones and the two parietal bones. 3. Lambdoid suture line of juncture of the occipital bone and the two parietal bones. Clinical Importance of the suture lines:
They allow the cranial bones to move and overlap (molding) diminishing the size of the skull. Molding is the change in shape of the fetal skull produced by the force of uterine contractions pressing the vertex of the head against the not yet dilated cervix. Assure the parents that molding only lasts a day or two and it not a permanent condition. 3. Fontanelles membrane covered spaces found at the junction of the main suture lines. 1. Anterior fontanelle (bregma) lies at the junction of the coronal and sagittal sutures. - Diamond shaped because it is in the junction of 2 fused frontal bones and two parietal bones. - Anterioposterior diameter measures 3 to 4 cm. - Transverse diameter 2 to 3 cm. 2. Posterior fontanelle lies at the junction of
the lambdoidal and sagittal sutures. - Triangular in shape because it lies between two parietal bones and the occipital bone. - It is smaller than the anterior fontanelle. - Anterioposterior diameter 3 to 4 cm. - Transverse diameter 2 to 3 cm. Clinical Importance: Fontanelle spaces compress during birth to aid in molding of the fetal head. This helps to establish the position of the fetal head and whether it is a favorable position for birth. Vertex space between the two fontanelles. Sinciput area over the frontal bone. Occiput area over the occipital bone. DIAMETER OF THE FETAL SKULL Anteroposterior diameter is wider than in its transverse diameter. Measurements of the Anteroposterior fetal skull:
1.
Suboccipitobregnmatic
diameter
the
narrowest diameter from the inferior aspect of the occiput to the center of the anterior fontanelle. - Approximately 9.5 cm. 2. Occipitofrontal diameter measured from the bridge of the nose to the occipital prominence - Approximately 12 cm. 3. Occipitomental diameter widest anteroposterior diameter, measured from the chin to the posterior fontanelle - Approximately 13.5 cm
Measurements of the Anteroposterior Diameter Diameter Location Measurement Presentation in relation to the Suboccipitobregmatic diameter Narrowest diameter From the inferior Approx. 9.5 cm degree of flexion Full flexion fetal head flexes, the chin rests on the thorax.
aspect center anterior
of of
the the
occiput to the
fontanelle. Moderate Occipitofron From the bridge Approx. tal diameter of the nose to cm. the occipital prominence Occipitome ntal diameter Widest anteroposterior diameter. Measured posterior fontanelle from the chin to the Approx.13.5 cm Poor flexion ( hyperextended) 12 flexion.
Relationship of the Passage and the Passenger Pelvis Fetal Skull Clinical Importance
Pelvic Inlet: Anteroposterior Fetus must present the If diameter narrowest biparietal diameter (11cm). diameter(transverse diameter) narrowest fetal the anteroposterior diameter of the the skull head presented the anteroposterior diameter of the inlet engagement may not occur is to
diameter (9.25cm)
Pelvic Outlet: diameter (11cm)
Must still present its If
the
Transverse narrowest diameter.
anteroposterior diameter of the skull presented is in
the transverse diameter of the outlet Arrest of progress
10
may occur. Clinical importance: The fetus must present the smaller diameter (the transverse diameter) to the smaller diameter of the maternal pelvis; otherwise, progress can be halted and birth may not be accomplished. Good head flexion is important because it follows that a fetal head presenting a diameter of 9.5cm will fit through a pelvis much more readily than if the diameter is 12.0 or 13.5cm FETAL PRESENTATION AND POSITION Different In Utero Fetal Orientation: 1. Attitude 2. Engagement 3. Station 4. Fetal Lie 5. Fetal Presentation 6. Fetal Position
ATTITUDE Describes the degree of flexion a fetus assumes during
11
a labor or the relation of the fetal parts to each other. Attitude Complete Flexion Description Good attitude bowed forward forward. sternum. folded on the chest onto the abdomen 6. Calves pressed against the posterior aspect of the thighs. Moderate Flexion 1. Chin is not Occipital frontal Clinical Importance Normal fetal It helps a fetus
1. Spinal column is position. 2. Head is flexed present the smallest anteroposterior to the pelvis. ovoid smallest shape the space 3. Chin touches the diameter of the skull 4. Arms flexed and The body is in an 5. Thighs are flexed occupying are possible.
touching the chest diameter present to but is in an alert or the birth canal military position Does not interfere with labor. Because
12
during (descent
later and
mechanisms of labor flexion) the fetus is forced to flex the head fully. Partial extension 1. Presents the Occipitomental to the birth canal. is May is which be due to not
brow of the head diameter of the head to the birth canal. Poor flexion 1. 2. The The back neck
arched. extended complete extension.
Oligohydramnios, does allow a fetus for May reflect a
3. The fetus is in adequate movement. neurologic abnormality causing spasticity. ENGAGEMENT Refers to the settling of the presenting part of a fetus far enough into the pelvis to be at the level of the
13
ischial spines. Biparietal diameter in a cephalic presentation or the intertrochanteric diameter in a breech presentation has passed through the pelvis or the pelvic inlet. Floating - a presenting part that is not engaged. Dipping one that is descending but has not yet reached the ischial spine Causes of nonengagement for primipara at the beginning of labor: 1. Abnormal presentation or position 2. Abnormality of the fetal head 3. Cephalopelvic disproportion Multipara, engagement may or may not be present at the beginning of labor. STATION Refers to the relationship of the presenting part of a fetus to the level of the ischial spines. 0 station the presenting part is in the ischial spine, synonymous with engagement -1 to -4 cm minus station. The presenting part is above the ischial spines.
14
+1 to +4 cm plus station. The presenting part is below the ischial spines. +3 and +4 cm the presenting part is at the perineum and can be seen if the vulva is separated. FETAL LIE Relationship between the long (cephalocaudal) axis of the fetal body and the long (cephalocaudal) axis of a womans body. Whether the fetus is lying in a horizontal (transverse) or a vertical (longitudinal) position. FETAL PRESENTATION Denotes the body part that will first contact the cervix or be born first. Types of Fetal Presentation Type Cephalic Presentation 4 Types: 1. Vertex Description 95% most frequent fetal presentation. The fetal head is the body part that Clinical Indications Vertex is the ideal type presenting part because the skull bones are capable of
15
2. Brow 3. Face 4. Mentum (refer to table 18.2 for the types of cephalic presentation)
will first contact the cervix.
molding. Aid in cervical dilatation. Prevents complications such as prolapsed cord. Caput succedaneum area of the skull that contacts the cervix becomes edematous from the it. continued against births the the of pressure often
Breech Presentation 3 Types: 1. Complete Breech 2. Frank Breech 3. Footling Breech
3% of births Either the buttocks or the feet are the first body parts that will contact the
Difficult with influencing degree difficulty.
presenting point
16
cervix. (refer to table 18.3)
Good fetal
attitude knees
up the
against umbilicus
Complete breech Poor knees extended; footling Shoulder Presentation 1% of births The presenting of the shoulders (acromion process), an iliac elbow Fetus is in a horizontally in the pelvis. The longest fetal axis from allow May be caused 1. abdominal Relaxed walls grand which the part is usually one by: attitude are
crest, a hand or an multiparity,
unsupported uterus 2. contraction Pelvic
transverse lie- lies to fall forward.
horizontal space is
17
is perpendicular to that of the mother
greater
than
the
vertical space. 3. Placenta Previa (placenta is located low in the uterus, obscuring some of the vertical space) limit a fetus ability to turn. Most infants in a transverse by birth. lie must be born cesarian
FETAL POSITION Relationship of the presenting part to a specific quadrant of a womans pelvis. 4 Quadrants of Maternal pelvis: 1. Right anterior (RA) 2. Left Anterior (LA) 3. Right Posterior (RP) 4. Left Posterior (LP)
18
4 Fetal Parts as landmarks: 1. Occiput (O) in a vertex presentation 2. Chin or mentum (M) in a face presentation 3. Sacrum (Sa) in a breech presentation 4. Scapula or the acromion (A) in a shoulder presentation LOA most common fetal position ROA second most frequent Middle letter denotes the fetal landmark First letter defines whether the landmark is pointing to the mothers R or L. Last letter defines whether the landmark points anteriorly (A), posteriorly (P) or transversely (T). Clinical Importance of Determining Fetal Presentation and Position: Position influences the process and efficiency of labor. LOA or ROA a fetus is born fastest. ROP or LOP labor is extended and more painful for the mother because the rotation of the fetal head puts pressure on the sacral nerves causing a sharp back
19
pain. Four Methods to Determine Fetal Position, Presentation and Lie: 1. Abdominal inspection and palpation- Leopolds maneuver 2. Vaginal Examination 3. Auscultation of fetal heart tones 4. Sonography
Nomenclature in Utero Fetal Orientation Reference Category Definition Most common Other Subcategory Subcategories
20
Lie
Relationship
Longitudinal
Transverse to
between long (fetal body is (fetal body is axis of fetus vertical to the horizontal and long axis mother). of mother. Presentation Portion fetus underlying pelvic inlet. Position Relationship between reference presenting of Cephalic ( fetal Breech head (longitudinal lie head in uterine fundus). mother).
lies closest to with pelvic inlet)
Direct occiput ROT,LOT,ROP, a anterior (OA) LOP is most at
point on the common fetal part and cephalic maternal bony presentation. pelvis. Attitude Degree flexion extension fetal head. of Vertex or (complete of flexion,
delivery with
Military (partial flexion). chin Brow (partial
against chest). extension). Face
21
(complete extension). Station The degree of Varies descent of the descent presenting part the canal; expressed cm, presenting part is above or below the maternal ischial spine (i.e. station 0). the presenting through part stages in labor. with Prior to of engagement, the station will be -4, moving to of delivery pf the head.
birth throughout the +4 just prior to
MECHANISMS OF LABOR (CARDINAL MOVEMENTS) Movement Descent Definition Purpose Downward movement Most important component
22
of head
the to
biparietal of labor. within the
diameter of the fetal pelvic inlet. Full descent when the fetal beyond head the extrudes dilated
cervix and touches the posterior vaginal floor. Flexion Fetal head reaches the pelvic floor, the head bends forward onto the chest. Allows anteroposterior narrowest diameter
(suboccipito-bregmatic diameter) to present to the birth canal.
Internal Rotation
Rotation of position of fetal head in the midpelvis from transverse to anteroposterior.
Allows the widest diameter of fetal head to present to the widest diameter of mid pelvis. Brings the shoulder, coming next, into the optimal position to enter the inlet.
23
Extension
Movement of fetal chin Directs the axis of the fetal away from the thorax as the fetal head passes through The pelvic outlet. head upward to the pelvic outlet.
External Rotation
Rotation of fetal head AP to transverse after the head has been delivered.
Allows the after coming into position, anteroposterior the outlet. Anterior shoulder is born first.
outside the mother from shoulders
which is best for entering
Expulsion
Delivery of the fetal shoulders and body.
Completes the birth process of the fetus.
POWER Fundus of the uterus supplies the power of labor resulting to uterine contractions. Uterine contraction
24
A process that causes cervical dilatation and then expulsion of the fetus from the uterus. Effective uterine contractions are rhythmic and progressive lengthening and intensity. Origin: Pacemaker point located in the myometrium near one of the uterotubal junctions. Each contraction begins at that point and then sweeps down over the uterus as a wave. Reverse, ineffective contractions cause tightening rather than dilatation of the cervix. Some contractions appear to originate in the lower uterine segment rather than in the fundus ineffective contractions cause tightening rather than dilatation of the cervix. Additional pacemaker sites can cause uncoordinated contractions and may lead to failure to progress and fetal distress. Phases of Uterine Contractions: 1. Increment intensity of the contraction increases 2. Acme contraction is at its strongest 3. Decrement intensity decreases Interval in between contractions the uterus relaxes.
25
- It decreases from 10 minutes early in labor to only 2 to 3 minutes. Duration of contractions changes from 20 to 30 seconds to a range of 60 to 90 seconds. Contour Changes of the Uterus 1. The uterus differentiates into two distinct functioning areas. 2. From round, ovoid structure to an elongated one. 3. Vertical diameter is greater than its horizontal diameter. Serves to straighten the body of the fetus, placing it in better alignment with the cervix and pelvis.
The uterus differentiates itself into two distinct functioning areas: 1. Upper segment - Thicker and active. Exerts the strength necessary to expel the fetus. 2. Lower segment - Thin-walled, supple and passive. Fetus can be pushed out of the uterus easily. Physiologic Retraction Ring A ridge on the inner uterine surface, which is the boundary between the two portions.
26
Pathologic Retraction Ring (Bandls Ring) The normal physiologic retraction ring may become prominent and observable as an abdominal distention. It is a danger sign and it signifies impending rupture of the lower uterine segment if the obstruction to labor is not relieved. CERVICAL CHANGES 1. Effacement 2. Dilatation Effacement Shortening and thinning of the cervical canal Normally, the canal is approximately 1 to 2 cm. The canal virtually disappears because of longitudinal traction from the contracting uterine fundus. Dilatation It refers to the enlargement or widening of the cervical canal from an opening a few milliliters wide to one large enough (Approximately 10 cm) to permit passage of a fetus. Causes of cervical dilatation:
27
1. Uterine contractions pull the cervix up over the presenting part of the fetus. 2. Fluid-filled membranes press against the cervix and serve as an opening wedge. PSYCHE Psychological state
PRELIMINARY SIGNS OF LABOR 1. Lightening 2. Increase level of Activity 3. Braxton Hicks Contractions 4. Ripening of the Cervix 1. Lightening descent of the fetal presenting part into the pelvis. Primipara occur approximately 10 to 14 days before labor. It occurs early because of tight abdominal muscles. Multipara occurs on the day of labor. Effects: A. breathing easier as a relief from the diaphragmatic
28
pressure. B. lordosis if increased C. increased vaginal discharge and urinary frequency because of pressure on the bladder D. leg pains from increased pressure on the sciatic nerve. 2. Sudden burst of energy. a woman awakens on the morning of labor full of energy. This increase in activity is related to an increase in epinephrine release that is initiated by a decrease in progesterone produced by the placenta. 3. Frequent Braxton Hick's contractions. 4. Ripening of the Cervix seen only on pelvic examination. Goodells sign cervix feels softer than normal throughout pregnancy, similar to the consistency of an earlobe. Butter-soft at term the cervix becomes still softer and its tip forward. Other preliminary sign of labor: 1. Weight loss of 1-3 lbs.
29
2. Backache may increase. 3. Diarrhea may occur. SIGNS OF TRUE LABOR 1. Uterine Contractions involuntary, productive uterine contractions. 2. Show - Mucous plug stained with blood discharge, from the cervix. As the cervix softens and ripens, the mucus plug that filled the cervical canal during pregnancy is expelled. 3. Rupture of membranes sudden gush or scanty, slow leaking of clear fluid from the vagina. Risks with early rupture of membranes: 1. Intrauterine infection 2. Prolapse of the umbilical cord
30
TRUE LABOR CONTRACTION Results in progressive cervical Occurs interval. Interval Intensity, between duration and contraction decreases. frequency increases. Felt first in lower back and sweep around to the abdomen in a wave Continue no matter what the womans level of activity. Not affected by sedation. STAGES OF LABOR dilatation at a and effacement. regular
FALSE LABOR CONTRACTION Do not result progressive Occurs interval. Interval same. Intensity, frequency same. Pain located and groin. duration remain and the between contractions remains the at an in
cervical irregular
dilatation and effacement.
Often
disappear
with
ambulation and sleep. Relieved by mild sedation.
Stage 1 (Cervical dilatation) begins with the initiation of dilated.
true
labor contractions and ends when the cervix is fully
31
Stage 2 (Stage of Expulsion) from full dilatation until the infant is born Stage 3 (Placental Stage) from the time the infant is born until after the delivery of the placenta. Stage 4 first to 4 hours after birth of the placenta. - to emphasize the importance of the close observation need at this time.
A. First Stage of Labor (Stage of Cervical Dilatation) - begins with the true labor and ends with complete dilatation of cervix. (10 cm. dilated) PHASES: 1. Latent Phase 2. Active Phase 3. Transition Phase 1. Latent Phase (early/preparatory phase) Begins at the onset of regularly perceived uterine contractions and ends when rapid cervical dilatation begins. Dilates from 0-3 cm. Nullipara 6 hrs. Multipara 4.5 hrs.
32
Contractions are usually 5-10 minutes, lasting 20-40 seconds and of mild intensity. Excited, thoughts center on self, labor and baby; talkative or mute, calm or tense, pain controlled fairly well, alert, follows directions readily, open to instructions. 2. Active Phase (acceleration phase) Cervical dilatation occurs more rapidly. Dilates 4-7 cm. Contractions are usually 3-5 minutes, lasting 40-60 secs. of mild of pain, to moderate intensity. More comprehensive, more serious, doubtful of control desires companionship and encouragement, has some difficulty following instructions. Nullipara last approximately 3 hours Multipara lasts approximately 2 hours 3. Transitional (declaration phase) Contractions reach their peak of intensity. Contractions every 2-3 minutes lasting 60-90 seconds and of moderate to strong intensity. Dilates 8-10 cm. backache common, fear of loss of control, irritable,
33
amnesia between
contractions,
nausea
and
vomiting,
hyperventilating, perspiration on forehead and upper lip, shaking, tremor of thighs, feeling of need to defecate, pressure on anus. B. Second Stage (Stage of Expulsion) Begins with complete dilatation and cervical effacement and ends with the birth of the baby. 1 hour The fetal head becomes visible at the vulva CROWNING. C. Third Stage (Placental Stage) Begins with the delivery of the baby and ends with the delivery of the placenta. 2 Phases: 1. Placental Separation 2. Placental Expulsion Placental Separation Active bleeding on the maternal surface of the placenta begins with separation This bleeding helps to separate the placenta further by pushing it away its attachment site. Signs of Placental Separation:
34
1. Lengthening of the umbilical cord 2. Sudden gush of vaginal blood 3. Change in the shape of the uterus 4. Firm contraction of the uterus 5. Appearance of the placenta at the vaginal opening Schultze placenta placenta separates first at its center and placenta lastly at its edge having a shiny and glistening from the fetal membranes.
Duncan placenta placenta separates firsts at its edges, it slides along the uterine surface and presents at the vagina with the maternal surface. It looks raw, red and irregular with the ridges or cotyledons showing. Shiny with Schultze (fetal membrane surface). Dirty with Duncan (irregular maternal surface) Bleeding occurs as part of the normal consequence of placental separation before the uterus contracts sufficiently to seal maternal sinuses. Normal blood loss is 300 to 500ml. (separate blood collection spaces)
Placental Expulsion
35
After separation, the placenta is delivered either by the natural bearing down effort or by gentle pressure on the contracted uterine fundus. Pressure must not be applied in a noncontracted state, because it may cause uterus to evert and hemorrhage. D. Fourth Stage (Vigilant Stage) Last after delivery of the placenta until one hour postpartum. FRIEDMAN LABOR CURVE Dr. Friedman studied the process of labor extensively He used data to identify two phases of labor on the Friedmans Curve: 1. Latent Phase 2. Active Phase a. Acceleration b. Maximum slope of dilatation c. Deceleration Clinical features of the divisions of labor ( table 18.4) 1. Preparatory division (Latent Phase) 2. Dilatational division (Acceleration and phase of maximum descent) slope) 3. Pelvic division (Deceleration phase and maximum
36
Labor Progress Graph Left sided numbered from 1 to 10 (representing the centimeters of cervical dilatation and usually plots as an S shaped curve) Bottom line numbered to represent the number of hours of labor. Right side numbered from -4 to +4 (representing the station of the presenting part and forms a downward curve). INVASIVE AND NON-INVASIVE ASSESSMENT OF FETAL WELL BEING 1. Electronic Fetal Monitoring 2. Non Stress Test 3. Contraction Stress Test 4. Fetal Biophysical Scoring Electronic Fetal Monitoring 1. External Electronic Monitoring 2. Internal Electronic Monitoring External Electronic Monitoring useful for monitoring both uterine contractions and FHR continuously or intermittently. Contractions are monitored by means of a pressure
37
transducer or tocodynamometer. Place the transducer over the uterine fundus or the area of greatest contractility. The transducer converts the pressure registered by the contraction into an electronic signal that is recorded on graph paper. FHR is monitored with the use of an ultrasonic sensor or monitor also strapped against a womans abdomen at the level of the fetal chest. Internal Electronic Monitoring The most precise method for assessing FHR and uterine contractions. A pressure-sensing catheter is passed through the vagina, into the uterine cavity and alongside the fetus, after the membranes have ruptured and the cervix has dilated to at least 3 cm. FHR recording is obtained from a fetal scalp electrode. Non Stress Test Based on the presence or absence of Fetal Heart Rate Accelerations An adequately oxygenated fetus moves its body and limbs. FHR accelerations are associated with fetal movements after 30 weeks gestation and indicate a normally
38
functioning uteroplacental unit. 1. Too early a gestational age 2. Fetal sleep cycles
A lack of FHR
accelerations can occur with any of the following:
3. Fetal central nervous system (CNS) anomalies 4. Maternal sedative or narcotic administration 5. Fetal hypoxia in a minority of cases Method: The external fetal cardiotocograph and contraction monitor is placed on the mothers abdomen, and the mother is positioned to avoid supine hypotension. Fetal movements and FHR are recorded. Fetal accelerations are defined as an increase in FHR of more than or equal to 15 beats/min over baseline and a duration of acceleration of more than or equal to 15 seconds. Interpretation: NSTs can be interpreted as reactive, nonreactive, or unsatisfactory A. Reactive: Two accelerations noted in a 20-minute interval are reassuring for fetal well being. B. Nonreactive: If any of the following criteria are met, then fetal well being is not assured: 1. Number of accelerations are too few 2. Number of beat/min change in FHR is less than
39
15 3. Duration of accelerations is less than 15 seconds. c. Unsatisfactory: The quality of the FHR tracing was inadequate to assess the criteria. Recommendations 1. If the NST is reactive, the test should be repeated weekly or biweekly. 2. If the NST is nonreactive, any of the following options may be chosen: a. Vibroacoustic stimulation. A healthy fetus will accelerate its heart rate in response to sound stimulation that is directed through the maternal abdominal wall. b. If the test is still nonreactive, then the Contraction Stress Test or the Biophysical Scoring is performed. Contractions Stress Test (CST) Based on the presence or absence of FHR late decelerations. a. Uterine contractions diminish the flow of oxygenated intervillous blood to the fetus. b. A fetus who has adequate metabolic reserve can cope satisfactorily with transient oxygen deprivation (i.e., FHR remains at stable baseline through contractions).
40
c. A compromised fetus will show late decelerations (FHR decelerations persisting after a contraction). Method: An external fetal cardiotocograph and contraction monitor is placed on the mothers abdomen, and the mother is positioned to avoid supine hypotension. Uterine contractions and FHR are recorded. If there are no spontaneous contractions, contractions are induced by nipple stimulation or intravenous oxytocin infusion (oxytocin challenge test). The goal is more than 3 contractions in 10 minutes. Baseline FHR, accelerations and variability are noted, and reactive or nonreactive status is determined. Contraindications: Conditions in which contractions may be hazardous, the CST should not be performed. 1. Previous classic-incision uterine scar 2. Previous myomectomy entering uterine cavity 3. Premature rupture of membranes 4. Incompetent cervix 5. Placenta previa Interpretation a. A negative result (i.e., no late decelerations) is reassuring of fetal well being. b. An equivocal result (nonrepetitive late decelerations) can
41
be interpreted as follows: 1. If the test is reactive the mother can probably be reassured that the fetus is well. 2. If the test is nonreactive there may be evidence of incipient fetal compromise. c. A positive test (i.e., repetitive late decelerations with three consecutive contractions in 10 minutes), is not reassuring of fetal well-beings. A true positive CST can be differentiated from a false-positive CST by assessing reactivity 1. If the test is reactive, the CST may be false positive 2. If the test is nonreactive, the result is more likely to be a true positive CST. d. Hyper stimulation is diagnosed when late decelerations occur after coupled contractions (one contraction after another without relaxation time between) or when there are more than five contractions in 10 minutes, and each contraction lasts longer than 90 seconds. Recommendations a. If the CST is negative, repeat it weekly or biweekly b. The CST is either equivocal or positive and reactive: a. Labor should be induced if the fetus is mature b. The CST should be repeated in 24 hours, or BPP should be performed if the fetus is immature.
42
c. If the CST is positive and nonreactive, the fetus should be delivered expeditiously. A vaginal delivery can be attempted if the cervix is favorable. A cesarean delivery should be A BPP should be performed if the cervix is unfavorable. performed if the fetus is markedly immature. Biophysical Profile (BPP) A healthy fetus moves, thereby accelerating its heart rate. Adequate fetoplacental blood flow will result in normal amniotic fluid volume. Fetal compromise will diminish fetal movements, FHR accelerations and amniotic fluid volume. Method: a. Complete BPP. An NST is performed, then using real-time ultrasound, the following characteristics are assessed: 1. Size of amniotic fluid pockets 2. Presence of fetal breathing movements 3. Presence of gross body movement 4. Presence of extremity extension, flexion and tone. b. Modified BPP has only two components: and NST and an amniotic fluid volume measurement. Interpretation a. Interpreting parameters
43
1. The NST is most predictive for immediate assessment of placental function. 2. The amniotic fluid measurement is most predictive for long-term assessment of placental function.
BPP Parameter Amniotic fluid NST Breathing Gross body motion Extremity tone
Score = 2 points >/= 1x1cm pocket Reactive secs 1 extension/flexion >/= 3
Score = 0 points Oligohydramnios Nonreactive
1 episode of >/= 30 No breathing None
Discrete >/= 2 movements
movements b. Interpretation of the Biophysical Profile (BPP) Total Score Test Result Recommendations
44
0 1 4 5 8 or 10
Positive jeopardy Positive jeopardy Equivocal Equivocal being
= =
fetal 0
to
2,
delivery be of
should fetal expeditious regardless gestational age.
4 to 6 the fetus if it is mature. 8 to 10, the test should be repeated in 1 week.
Negative = fetal well should be delivered
FETAL HEART RATE AND UTERINE CONTRACTION RECORDS Fetal Heart Rate Patterns 3 Parameters in evaluating the FHR: 1. Baseline Rate 2. Variabilities in the baseline rate (long term and short term) 3. Periodic changes in the rate (acceleration and deceleration) Baseline Fetal Heart Rate A baseline FHR is determined by analyzing the range of fetal heartbeats recorded on a 10-minute tracing obtained
45
between contractions. Normal FHR 120 to 160 bpm Fetal bradycardia FHR is lower than 120 bpm for 10 minutes Moderate bradycardia 100 to 119 bpm is not considered serious and is probably due to a vagal response elicited by compression of the fetal head during the labor. Marked bradycardia less than 100bpm is a sign of hypoxia and is considered dangerous. Fetal tachycardia occurs when rate is 160 bpm or faster (for a 10-minute period) may be caused by fetal hypoxia, maternal fever, drugs, fetal arrhythmia, maternal anemia or hyperthyroidism. Variability FHR variability is one of the most reliable indicators of fetal well being. Baseline variability is the variation or differing rhythmicity in the heart rate over time. Reflected on the FHR tracing as a slight irregularity or jitter to the wave. Degree of variability increases when the fetus is stimulated. Degree of variability slows when the fetus is sleep. No variability it indicates that the natural pacemaker
46
activity of the fetal heart (effects of the sympathetic and parasympathetic nervous system) has been affected. It may be a response to narcotics or barbiturates Fetal hypoxia and acidosis must be investigated. Very immature fetuses because of reduced nervous system response to stimulation and immature cardiac node function. Long-term variability fluctuations in the FHR of 6 to 10 bpm that occur 3 to 10 times per minute. Short-term variability or beat-to-beat variability refers to the difference between successive heartbeats, usually about 3 to 5 bpm. Periodic Changes Transitory FHR changes in response to contractions and fetal movements. 4 Periodic changes: 1. Acceleration 2. Early deceleration 3. Late deceleration 4. Variable deceleration Accelerations
47
Always reassuring. Increase in the baseline of 15 or more beats per minute lasting 15 or more seconds/ Caused by fetal movement or compression of the umbilical vein during a contraction. Early Decelerations Not clinically significant Early decelerations are periodic decreases in FHR resulting from pressure on the fetal head during contractions. Parasympathetic stimulation in response to vagal nerve compression brings about a slowing of FHR. It serves as a mirror image of the contraction. Late Decelerations Not reassuring Delayed FHR for 30 to 40 seconds after the onset of a contraction and continue beyond the end of contraction. Ominous pattern in labor It is a response to uteroplacental insufficiency or decreased blood flow through the intervillous spaces of the uterus during uterine contractions. Nursing Actions:
48
1. Stop or slow the rate of oxytocin if it is being used 2. Change the womans position from supine to lateral (to relieve pressure on the vena cave and supply more blood to the uterus.) 3. Administer intravenous fluids or oxygen as prescribed. 4. Prepare for prompt birth of the infant if the late decelerations persist. Variable Decelerations It refers to decelerations that occur at unpredictable times in relation to contractions. Indicate compression of the cord, which can be an ominous development in terms of fetal well being. Cord compression may occur because of a prolapsed cord or the fetus is lying on the cord. ANALGESIA/ANESTHESIA DURING LABOR Types and Indication Table 19.1 Nursing Responsibilities before, during and after administration of anesthesia: 1. Continuously monitor vital signs. 2. Epidural anesthesia can temporary elevate temperature. 3. Continuously monitor blood pressure for the first 20 minutes after each new injection of anesthetic and throughout the time
49
the anesthetic is in effect. placental blood perfusion.
Hypotension will compromise
4. If hypotension occurs, turn the woman to her left side to reduce vena cave compression. 5. Never place a woman in a Trendelenburg position to help restore blood pressure after spinal anesthesia. This could make the anesthetic rise high in her spinal column, causing uterine or respiratory function to cease. 6. With epidural block, the woman loses sensation of her bladder filling. Remind the client to void every 2 hours, monitor intake and output, observe, and palpate for bladder distention to avoid overfilling. 7. Postpartal dural puncture headache (PDPH) or spinal headache is a late complication of spinal anesthesia. This is reduced by using a small gauge needle. It can be relieved by having the woman lie flat and administering an analgesic. If a headache is incapacitating, it can be treated with a blood patch technique. This occurs because of continuous leakage of CSF from the needle insertion site and from irritation of a small amount of air that enters at the injection site. initiating the pain. The shift in pressure of the CSF causes strain on the cerebral meninges,
50
MANAGEMENT DURING FIRST STAGE of LABOR: 1. Admission - provide reassurance; maintain privacy. Name, age, address, occupation, marital status. 2. Assessment- careful evaluation of: ANTEPARTAL HISTORY 1. Current Pregnancy History a. Gravida and Para status b. Description of pregnancy (planned or not, pattern and place of prenatal care, adequacy of nutrition, history of spotting, falls, hypertension of pregnancy, infection, alcohol or drug ingestion) c. Plans for labor d. Future childcare 2. Past Pregnancy History Prior Pregnancies including number, dates, type of birth, any complications and outcomes, including the sex and birth weights of children. Current status of the children. 3. Past Health History Any previous surgeries ( surgical adhesions might interfere with free fetal passage) Heart disease or diabetes (special precautions are required during labor and birth).
51
Anemia ( blood loss at birth may be more important that it is normally) Tuberculosis ( lung lesions may be reactivated at birth by changes in lung contour) Kidney disease or hypertension ( blood pressure must be monitored even more carefully than it is normally) Sexually transmitted infections such as herpes ( the infant may be exposed to the disease by vaginal contact if the disease is still active) High risk for HIV 4. Family Medical History Heredofamilial diseases for adequate preparation can be made for a child who might have special needs. PHYSICAL EXAMINATION Begins as does all physical assessment, with the womans overall appearance and is similar to that for any woman. Enlarge lymph nodes to detect possible infection Inspect for the mucous membrane of the mouth and the conjunctiva of the eyes for color Condition of the womans teeth
52
Herpetic lesions Assess the lungs Normal heart sounds and rhythms. Inspect and palpate the breast Abdominal Assessment Important to estimate fetal size by fundal height Assess presentation and position by Leopolds maneuver Palpate and percuss the bladder area to detect full bladder. If full, may impede the progress of labor or result in trauma in the bladder, check urine for protein. Assess abdominal scars, because abdominal or pelvic surgery can leave adhesions. Assessment of Uterine Contraction Monitor every 15-30 minutes. 1. Place finger tips over the fundus and feel the hardening and tensing. 2. Time and record the following: Duration - time from the beginning to the end of one contraction. Time in seconds. Interval - time from the end of one contraction to
53
the beginning of the next contraction. Frequency - time from the beginning of one contraction contraction. Intensity - strength at the acme. 1. Weak - easily indent fundus with fingers. 2. Moderate - some tension felt, indents slightly with finger pressure. 3. Strong - unable to indent fundus. Fetal Heart Rate Normal - 120-160 bpm 1. Check and record every 15 minutes. 2. If taken with contraction, it is normally decreased due to stimulation to vagal nerve. 3. Observe for signs and symptoms of fetal distress. Bradycardia (mid100- 119 bpm) 30 beats lower from the baseline/min. Tachycardia (moderate 160-179 bpm) or 30 beats per minute higher from the baseline. Meconium stains amniotic fluid in cephalic presentation. Initial Action: Reposition the mother on her side. to the beginning of the next
54
Inspect lower extremities Skin turgor to assess hydration Edema. Suggest hypertension Varicose veins. Women with large varicosities are more prone to Thrombophlebitis after giving birth. Vaginal Examination and Progress of Labor Determine cervical effacement and dilatation and to confirm fetal presentation, position and degree of descent Do not do vaginal examinations in the presence of fresh bleeding, because this may indicate a placenta previa (implantation of the placenta so low in the uterus that it encroaches on the cervical os). Perineum: Signs of imminent delivery like bulging of the perineum (crowning) and cord prolapse. Amount of Show Molding of fetal head Pelvic Adequacy Evaluate pelvic adequacy using internal conjugate and ischial tuberosity.
55
Suprapubic angel is estimated early in labor to determine how readily the fetal head will be born ( if the angle is too steep, the fetal head can lock behind it and perineal tissue may tear during birth as the fetal head is pushed posteriorly). Place the fingers vaginally and press up against the pubic arch. If the fingers cannot be separated in this position, the angle is unusually steep. Sonography To determine the diameters of the fetal skull and to determine presentation, presenting part, position, flexion and degree of descent of a fetus. Vital Signs (Table 18.5) must be taken between contractions. Elevated temperature: Development of infection or reflects dehydration. After rupture of membranes, temperature will be taken every 2 hours because of increase possibility for infection. Increase Pulse and Respiration: nervous, anxious, dehydration or hemorrhage, altered with the use of breathing technique. Measure blood pressure between contractions for
56
accuracy and comfort of the woman. Laboratory Analysis Blood: Hemoglobin, hematocrit, VDRL, hepatitis B antibodies and blood typing for baseline level of health. Urine: To test for protein and glucose, urinary tract infection. Assess the Maternal Response to Labor Care of Woman during the First Stage of Labor: 1. Promote comfort encourage sucking ice chips (maintain hydration) Petroleum jelly on lips (reduce dryness). Apply sacral pressure particularly if the position is occiput posterior (relieves backache). 2. Physical needs Perineal preparation (to promote cleanliness). Enema preparation (to stimulate peristalsis, evacuate lower bowel). Encourage frequent voiding Encourage left sim's position with head elevated to: 1. Promote relaxation
57
2. Promote rotation of the fetal head. 3. Prevents compression of the inferior vena cava thus Preventing SUPINE HYPOTENSIVE SYNDROME. 4. Increase placental perfusion. 3. Emotional Support Encourage verbalization of fears, concerns. inform her on the progress of labor Explain all procedures. 4. Analgesia and Anesthesia May be required for safe and comfortable delivery. 5. Support and reinforce the Lamaze Technique Reinforce appropriate breathing technique based on the status of labor. EARLY PHASE - slow chest pattern. ACTIVE PHASE - rapid chest pattern. TRANSITION - pant, blow pattern. Expulsion of the baby - breathing in - PUSH. Remember: The patient may hyperventilate with the resultant decrease in Pulmonary C02, fetal acidosis and symptoms of vertigo and syncope. NURSING ACTION: 1. Breath into a paper bag.
58
2. Hold's one breath. 3. Reinforce proper breath technique. 6. Watch for signs that second, stage is very near. Contractions strong and expulsive, every 1-3 minutes lasting 60 to 90 seconds. Increase amount of show: signifies progressive dilatation. Nausea and vomiting tremors Anus pouting, vulva gaping. Perineum bulging - surest sign that delivery is imminent because fetal head distends the perineum or crowns. Nursing Diagnoses: 1. Powerlessness related to duration of labor 2. Risk for ineffective breathing pattern related to breathing exercises 3. Anxiety related to stress of labor 4. Risk for fluid volume deficit related to prolonged lack of oral intake and diaphoresis from the effort of labor MANAGEMENT OF THE SECOND STAGE OF LABOR 1. Assist the patient assumes a Dorsal Lithotomy Position. Two legs should be placed on the stirrups at the same time (to
59
prevent strain on her back and lower abdominal muscles) with a pad to protect the calf. 2. Primigravida is transferred to the delivery room when caput is seen at the introitus, for multipara when cervix is fully dilated 10 cm and head is station at 2. 3. Promote effective second stage pushing. Patient is encouraged to push with coupled breathing and relaxation techniques to make effective use of the patient Expulsive efforts. Patient must push with contractions and rest between them. Allow her to push when she feels the urge and to use position and technique she feels are best for her. Advice patient to breathe out during a pushing effort because holding the breath during the contraction could cause a Valsalva maneuver or temporarily impede blood return to the heart because of increased intrathrocic pressure and it can interfere with the blood supply to the uterus. 4. Clean the perineum with a warmed antiseptic and then rinse. 5. Assist in episiotomy. It is a surgical incision of the perineum to prevent tearing of the perineum and to release pressure on the fetal head with birth. 5. Apply pressure against the rectum drawing it downward to aid in flexing the head as the back of the neck escapes the symphysis
60
pubis, the applying upward pressure from the coccygeal region (Modified Ritgens Maneuver) to extend the head during the actual delivery to prevent. 6. As soon as the head of a fetus is prominent at the vaginal opening, place a sterile towel over the rectum and press forward on the fetal chin while the other hand is pressed downward on the occiput. (Ritgen maneuver) It helps a fetus achieve extension, so that the head is born with the smallest diameter presenting Never apply pressure to the fundus of the uterus to prevent uterine rupture. 7. As soon as the head is out, suction the mouth and nose of secretions to clear the air passages. Then baby can breathe on his own. 8. Check the neck cord coil. Insert two fingers and slip over the head. 9. Head is drawn downward and backward to deliver file shoulders, and then gradual traction should now deliver the baby. Suction the mouth and nose and the head is held slightly lower than the baby to promote drainage of secretions. Newborn is held at the level of the mother's uterus until a pulsation ceases which usually happens within second after respiration is initiated.
61
If baby is placed higher than the mothers abdomen. Fetal blood may drain to the placenta. If lower excessive blood may flow to the neonate prior to cessation of pulsation. 10. Baby is placed on her abdomen to promote placental separation thus third stage is shortened. 11. Cord is clamp if pulsation ceases: the baby is shown to the mother and information about sex and the time of birth are given, if mother wishes, newborn is placed to her breast to establish Early lactation and promote eye-to-eye contact thus initiate BONDING. IMMEDIATE CARE OF THE NEONATE 1. Ensure clear airway. Head is held lower at 10 to 15 degrees to drain the secretions and prevent aspiration of amniotic fluid, mucous and blood. Suction the mouth and nose (if sequence is reverse, aspiration may result.) Avoid prolonged and deep suctioning because vagus nerve gets stimulated resulting to bradycardia and laryngospasm. 2. Maintain warmth. Newborn is dried immediately. Wrapped the neonate with warm blankets.
62
Placed newborn under droplight or warmer. * This prevents chilling that may deplete glycogen stores resulting to hypoglycemia and metabolic acidosis. 3. The cord is tied or clamped close to the umbilicus. However if there is a need for transfusion such as in erythroblastosis fetalis, an 8 to 10 cm. proximal length should be left and covered with sterile gauze soak in NSS. The vessel of the cord is counted. 4. The condition of the neonate is assessed at 1 minute and again at 5 minutes = APGAR SCORE. SIGN Heart Rate 0 ABSENT 1 SLOW, BELOW 100/MIN. Respiratory Rate Muscle Tone FLACCID ABSENT SLOW, IRREGULAR SOME FLEXION Reflex Irritability NO RESPONSE CRY GOOD, CRYING ACTIVE MOTION VIGOROUS CRY 2 OVER 100
63
Color
BLUE, PALE BODY PINK, Extremities Blue
Complexity PINK
7. Identification. Identiband, one on the mother's wrist, two others from the infants wrist and ankle. Thumb print of the mother and footprint of the newborn. 8. Administration of Vitamin K A prophylactic injection given to prevent bleeding during the first few days because newborn is not capable of producing his own vitamin K. MANAGEMENT OF THE THIRD STAGE OF LABOR The goal is the prompt separation and recovery of the placenta achieved in easiest and safest way. Normally 5-7 minutes after birth of the baby, placenta separates from the myometrium. If 20 minutes had passed with no signs of separation, the uterus is atonic. Initial actions inform the physician: 1. Signs of placental separation in sequence:
64
a. A firm contracting, rising fundus. b. Globular shape abdomen (from discoid). c. A visible and palpable founded prominence above the symphysis (the placenta if bladder is empty). d. Slight gush of blood. e. Lightening of the cord. f. Vaginal fullness, placenta is noted on the vaginal of rectal examination. MECHANISM OF PLACENTAL EXPULSION 1. If placenta presents by shiny fetal surface resembles in "inverted umbrella" SCHULTZ (80%). 2. If placenta presents by its dark roughed maternal surface resembles a "button entering a buttonhole" = DUNCAN (20%). 2. Deliver the separated placenta using traction (BRANDT ANDREW MANEUVER) holding into the corpus (MODIFIED CREDE' S MANEUVER). 3. Check the placenta for completeness. 4. Check the fundus if contracted: It is hard, firm and fundus is palpable midway between umbilicus and symphysis pubis. If soft boggy and not palpable, uterus is relaxed. Cold compress will help and administer oxytocin as ordered. (increases uterine contractions and thereby minimizing uterine bleeding). 5. Check the perineum. If laceration exists, apply pressure and
65
prepare the patient for suturing. 6. Check the bladder. Full bladder predisposes the patient to uterine atony and urinary tract infection. 7. Vulva is cleansed; gown is changed to make the patient comfortable. MANAGEMENT OF FOURTH STAGE OF LABOR 1. Vital signs are taken and recorded. BP, pulse and respiration are taken every 15 minutes for the first 1-2 hours. Temperature is taken every 4 hours if normal. 2. Check the fundus. It rises at the level of the umbilicus within 24 hours after delivery. It must be hard and palpable. 3. Check the lochia; moderate in amount and appear in order: a. LOCHIA RUBRA - 1-3 days. Consist mainly of blood. Red in color. b. LOCHIA SEROSA - 4-10 days. Pale, pink becoming brown. c. LOCHIA ALBA - yellow to white. 4. Check the perineum. Episiotomy is evaluated for swelling, intactness and bleeding every 15 minutes for the first 2 hours. 5. Rooming - in maternal interaction with newborn and family is also evaluated.
66
6. Check the bladder. If full it may displaced the uterus to the sides. 7. RHOGAM is given if mother is Rh (-) and newborn is (+) to prevent formation of antibodies against Rh +. Thus, the next Rh + is protected from hemolytic disease. REMEMBER: Rhogam should be given within 72 hours after delivery to Rh (-) mother who delivered on Rh positive fetus and had not been sensitized by fetal Rh positive blood. PUERPERIUM This refers to the 6-week period after childbirth or fourth trimester of pregnancy. Retrogressive maternal changes like involution of the uterus and vagina. Progressive maternal changes like production of milk for lactation, restoration of normal menstrual cycle and beginning of a parenting role. PHYSIOLOGIC CHANGES DURING THE POSTPARTAL PERIOD A. UTERUS 1. Remains 1000gms in weight for the first 2 days after delivery. 2. Contraction pinch large vessels at the placental site to prevent
67
hemorrhage. This contraction reduces the size of the uterus. 3. Within 12 hours after delivery fundus is palpable at the level of the umbilicus and located at the midline. Then descends one fingerbreadth per day until the 10 th day when it is no longer palpable because it is in the pelvic cavity. 4. Uterine discharge - LOCHIA. a. Rubra - consist mainly of blood, last for 1-3 days, red in color and should be moderate in amount if excessive it is postpartum hemorrhage. b. Serosa - consist of blood and tissue, 4th to 10th days pink in color to brownish. , c. Alba - consist mainly of mucous and leukocytes, 10th days to 6th weeks colorless or white. The total quantity of lochia discharge is 200 gms. 5. Endometrium is restricted by the end of the 3rd week, and placental site is healed by the end of the 6th week. B. VAGINA 1. Returns to its pre-pregnant state by 3rd or 4th week. 2. Most of the vaginal rugae are flattened.
68
C. CERVIX 1. Involutes by the end of 1 week. 2. Internal os returns to pre-pregnant state but external os remains slightly open and appears slit like or stellate (transverse slit). D. BREAST 1. The breasts are usually soft during the first two post-partum days. On the 3rd to the 5th day, they may become engorged (full and firm). Engorgement is brought about by hormone Prolactin that is stimulated by the baby's sucking to promote lactation. In addition, lactation is stimulated by decrease level of estrogen and progesterone. 2. Colostrum is secreted continuously during pregnancy. 3. Breast feeding relieves breast engorgement. E. BLADDER 1. In early puerperium, the bladder is less sensitive to fullness thereby, overdistention occurs frequently. Urinary tract infection is common. 2. Marked diuresis during first 24-48 hours following delivery as body withdraws large amount of fluid retained caused by increased estrogen and progesterone level during pregnancy. 3. May void 3000 cc. compared to 1000- 1800 cc. normally. F. GASTRO-INTESTINAL TRACT 1. Woman is hungry after delivery.
69
2. Constipation is common due to dehydrating effect of labor, enema and decrease muscle tone in the intestine. G. VASCULAR SYSTEM 1. Continuous increase in fibrinogen level after delivery. 2. Blood volume back to pre-pregnant state on the 3rd week post-partum. 3. Blood loss with vaginal birth 300 to 500 ml. Cesarean birth 500 to 1000 ml. 4. WBC may be as high as 30,000 cells/mm. Part of the bodys defense system. H. ENDOCRINE CHANGES a. Human chorionic gonadotropin(hCG) and Human placental lactogen (hPL) is undetectable 1 day after delivery. b. Progestin, estrone, and estradiol are at pre pregnancy state by 1 week. C. FSH remains low for about 12 days and then begins to rise.
I. VITAL SIGNS 1. Temperature is slightly elevated during the first 24 hours possibly due to dehydrating effect of labor and increase muscular activity.
70
2. Blood pressure has no changes. 3. Pulse rate during postpartal period is usually slightly slower than normal. I. MENSTRUATION 1. Resumes with 6 to 10 weeks in non-breastfeeding mothers. Some during the entire period of lactation. 2. If she is breastfeeding menstruation resumes after 3 to 4 months. J. EMOTIONAL CHANGES (RUBIN'S PHASES) 1. Taking-in phase lasts for two to three days post-partum. The mother is passive and dependent and has difficulty in making decision for herself. Her needs are expressed more in relation to herself and not on her baby. She needs to eat and sleep a great deal not the best time to teach baby care. 2. Taking-hold phase - the mother becomes more independent and autonomous (self-dependent). She begins to make decisions and take the initiative for her own actions. She becomes more interested in the mothering tasks. This phase lasts about 10 days so that most of it will take place after she goes home. Caution overdoing may cause exhaustion. 3. Letting Go phase woman defines and accepts her new role. Post-partum Blues. Often occurs on the third day postpartum.
71
She cries more easily for no reason. More irritable, anorexic and experience loss of sleep. The cause is not definitely known but some possible factors are hormonal, jealousy, unmet needs for sleep. MANAGEMENT OF PUERPERIUM 1. Assessment for evaluation a. Check height, consistency of the fundus every four hours. On delivery, day and less frequent thereafter. b. Check vital signs every four hours. c. Check amount, color and odor of lochia every four hours. d. Check perineum for swelling and bleeding. e. Assess bonding. f. Assess emotional status. g. Assess for pain. 2. Provide comfort measures. A. After pains is more common in multi areas due to poor muscle tone. - Early ambulation - Frequent voiding - Present during breastfeeding, analgesic is given 1/2 hour before breastfeeding. b. Perineal Discomfort. 1. Ice to reduce swelling (first 24 hours). 2. Sitz bath and perineal light (after 24 hours).
72
3. Perineal care after each voiding. 4. Analgesics if measures failed. 5. Perineal exercises Kegel exercise. Contracting and relaxing the muscles of the perineum five to ten times in succession. 6. Provide perineal care C. breast engorgement 1. Well fitting brassiere at all times. 2. Ice pack for non-breast feeders. 3. Warm soaks breast feeders. 4. Analgesics, last resort. 3. Provision of rest. A. planned nursing care. B. regulated visiting hours. 4. Discuss Sexual Relations A. can resume if episiotomy heals and bleeding stops, usually 3-4 weeks. B. use method of contraception except pills if breast-feeding. C. discontinue if bleeding occurs. 5. Discuss Nutrition. * requires 3000 calories if breastfeeding and 2300 or 2400 if not breastfeeding. 6. Breastfeeding
73
- Human milk is the natural food for infants or cow's milk is to calves. Each thrives better in his own natural milk. On the initial breastfeeding of 2-3 times during the day and once or twice during the night. On the first breastfeeding, it should be 2-3 mins. On each breast and May up to 5 minutes at the end of the day. Then add 1 minute on each breast until 10 mins. on each breast. Physiology of Breast Milk Production: Benefits of Breastfeeding: To infants: 1. Provides a nutritional complete food for the young infant 2. Strengthens the infants immune system, preventing many infections. Anti infective properties of breast milk a. Colostrum thin, watery, yellow fluid composed of protein, sugar, fat, water, minerals, vitamins and maternal antibodies. b. Secretory Immunoglobulin A (IgA) acts against bacteria invading or colonizing the mucosae of intestines. c. Lactoferrin binds iron and inhibits the growth of E. coli, Staphylococci and Candida albicans. c. Lysozymes are bacteriostatic against bacteria.
74
d. Leukocytes, macrophages, lymphocytes e. Interferon protein that protects against viruses F. bifidus factor inhibits the growth of man pathogenic or harmful bacteria preventing diarrhea. 3. Safely rehydrates and provides essential nutrients to a sick child, especially to those suffering from diarrheal diseases 4. Increase IQ points To Mother: 1. Serve a protective function in preventing breast cancer. 2. Aids in uterine involution by the release of oxytocin from the posterior pituitary glands. 3. Empowering effect. 4. Reduces the cost of feeding and preparation time. 5. Enhances bonding Contraindications to Breastfeeding: 1. Infant with galactosemia (infants cannot digest the lactose in milk) 2. Herpes lesions on a mothers nipples 3. Maternal diet is nutrient restricted, preventing quality milk production. 4. Maternal medications (lithium, methotrexate)
75
5. Maternal exposure to radioactive compounds 6. Breast cancer PROCEDURES 1. Wash hands and assumes a comfortable position. 2. Start with the breast that was used last. 3. Burp the baby after the first breastfeeding. THE MOTHER SHOULD KNOW: 1. Breast should be dried after each feeding and wash once daily. 2. Pads inside the bra to prevent leaks. 3. Nipple rolling exercise. 4. Well fitted bra. 5. Drugs should be prescribed. 6. Avoid gas forming foods (camote, cucumber, onions, cabbage, etc.). 7. Birth control pills are contraindicated because estrogen suppresses lactation. 8. Increase fluid intake 11/2 quart milk and 1000 cc of additional fluid. 9. Infants stool light, yellow partly and more frequent. 10. One month old baby will nurse 15-20 minutes of each breast.
76
11. Hoffman maneuver for making the nipple more protractile. The nipple becomes erect with tactile stimulation from the thumb and the opposing forefinger, in horizontal plane. The process is repeated in the vertical plane. The procedure, practiced daily, helps to break adhesions at the nipple base, and makes it more suitable for grasping by the baby during nursing. Comparison of Mature Human Milk and Cow Milk In human milk, the ratio of whey proteins to casein is 70:20. The whey proteins of human milk consist mostly of alactalbumin and Lactoferrin. Cows milk protein has whey to casein ration of 20:80. Cows milk whey is mostly B-lactoglobulin with small amounts of a-lactalbumin and lactoferrin, the main proteins of human milk. Digestion of human milk protein is more efficient and faster and absorption is more complete than that of cows milk protein. The fat emulsion in human milk is finer. Carbohydrates: Lactose is the main carbohydrates and is about 7% of human milk vs. 4.8% of cows milk giving the breast milk its sweeter taste.
77
Mineral and electrolyte concentrations in breast milk are lower than cows milk to ensure that sufficient free water is available to the infant.
The fully nursing normal infant requires no extra water even in tropical heat or with febrile illness. Vitamin content depends on the maternal intake. Human milk has more niacin and vitamin C, cows milk more thiamin and riboflavin.
Both human and cows milk contain large amounts of vitamin A and minimal contents of vitamin D.
X. FAMILY PLANNING A. REPRODUCTIVE TECHNOLOGY 1. Attitude toward reproductive technology a. Shaped by religious and cultural background. b. Influenced by family attitude. c. Affected by socio-economic status. d. Influenced by both partners definition of family roles. 2. Influence on effectiveness intrinsic value or method, acceptability of the couple, couple's understanding or method, motivation of couple to use method properly.
78
3. Nursing Intervention a. Explain all available methods. b. Discuss effectiveness, advantages and disadvantages of each method. c. Discuss couple's feeling about reproductive technologies. d. Once a method is chosen, instruct both partners in the use of the method. e. Have the couple return explanation or the method is chosen. f. Clarify any misunderstanding. Methods I .NATURAL Types are as follows: a. RHYTHM Calendar - estimates the date or ovulation based on length of cycle (effectiveness is low). 3 or 4 days before until 3 of 4 days after ovulation. Keep a diary of 6 menstrual cycles Calculate safe days:
79
Subtract
18
from
the
shortest
cycle
documented this represents her first fertile day. Subtract 11 from the longest cycle this represents her last fertile day. b. BASAL BODY TEMPERATURE (BBT) Before the day of ovulation, a womans basal body temperature (BBT) falls about 0.5F. At the time of ovulation, her BBT rises a full degree because of the influence of Progesterone. The woman takes her temperature each morning immediately after waking, before she undertakes any activity. A slight dip in temperature followed by an increase is her ovulation. Refrain from having sex for the next 3 days. Identification on safe periods, considering that ovum must be fertilized within 24 hours and sperm survives within 48-72 hours. c. SYMPTOTHERMAL Self-observed changes in the quality of the cervical mucous are recommended to time of ovulation.
80
When daily observation of cervical mucous combined with the basal body temperature chart this is called SYMPTOTHERMAL METHOD. d. CERVICAL MUCOUS (SPINBARKEIT TEST) The mucous is observed on its viscosity because subsequent to ovulation, mucous becomes more viscous, slippery and stretches at least 1 inch before the strand breaks and is said to be fertile and it is unsafe. e. Lactational Amenorrhea Method (LAM) Natural suppression of ovulation by breast-feeding an infant f. Coitus Interruptus The withdrawal of the penis before ejaculation. II. ARTIFICIAL Types are as follows: A. CHEMICALS Jellies Creams Suppositories Foams * These contraceptives are quite expensive and available without consulting a physician. They are relatively ineffective. However,
81
because the woman cannot be sure of the placement of the retention of the spermicidal agent. These are especially useful for the patient who are contemplating another pregnancy and has been on the pill. She could stop the pill a few months earlier than the time and planned for the use of the reproductive technology she wants (foam, jellies, or the likes) that is less effective until her periods are reestablished. POINTS TO REMEMBER 1. The foam or cream should be placed in the vagina or more than one-half before intercourse. 2. The agents should be inserted before each intercourse. 3. The patient should not douche for at least eight hours after intercourse. B. BARRIERS Diaphragm Cervical caps Condom Female Condom POINTS TO REMEMBER 1. Should be used to conjunction with a chemical agent to increase effectiveness. 2. Needs to be fitted after delivery or weight change more than 10 pounds.
82
ADVANTAGES AND DISADVANTAGES 1. Decreases penile sensation. 2. Hindrance to the time of urge. 3. Can rupture during intercourse. 4. Inexpensive. 5. Available without prescription. 6. Immorality in the Christian concept. C. HORMONE A. Pill - a hormone therapy that suppresses ovulation. 1. Single-hormone therapy a. Estrogen given 2 weeks of each month prevents ovulation by suppressing LH and FSH. b. Progesterone given daily makes cervical mucous impervious to sperm and prevents maturation of endometrium. Ovulation occurs but implantation is prevented. 2. Combined-hormone therapy a. This is a combination of estrogen and progesterone. b. It is taken from day 5 to 25 of cycle. c. Bleeding starts 1 to 4 days after the last pill. CONTRAINDICATION
83
1. Family history of stroke 2. Migraines 3. Hypertension 4. Diabetes 5. Chronic renal disease 6. Thrombophlebitis 7. Heavy Smoking (2 packs). SIDE EFFECTS 1. Nausea and vomiting 2. Edema 3. Weight gain 4. Breakthrough bleeding 5. Thrombophlebitis 6. Pulmonary embolism 7. Stroke D. IMPLANT Subcutaneous Implants six nonbiodegradable Silastic implants that are filled with synthetic progesterone and embedded under the skin on the inside the upper arm. For 5 years, the implants slowly release the hormone suppressing ovulation.
84
Intrauterine Devices small plastic object that is inserted into the uterus through the vagina. Progesterone-impregnated IUD (Progestasert) and Mirena which hold a drug reservoir of progesterone in the stem and releases the medication rapidly. Progestasert must be replaced every year and Mirena is effective for 5 years. Copper IUD (Paragard) which releases the copper slowly, need to be replaced every 7 years. The progesterone in the drug reservoir gradually diffuses into the uterus through the plastic that prevents Endometrium proliferation and thickens cervical mucus. III. PERMANENT (STERILIZATION) Factors to consider: a. Sterilization should be considered permanent; there is low success rate in attempts to reestablish fertility. b. Voluntary sterilization is permitted in all states except Utah, which requires a medical condition that threatens the mother's life. c. Sterilization of minors or mentally incompetent person is restricted by most states. METHODS:
85
1. VASECTOMY (Male) surgical interruption of the Vans deferens. 2. TUBAL LIGATION (Female) - surgical interruption of the continuity of the fallopian tube. 3. OOPHERECTOMY - surgical removal of the ovaries. HYSTERECTOMY - surgical removal of the uterus. This is rarely done unless pathology exists. IV. OTHERS 1. Coitus Interrupts - withdrawal of the penis before ejaculation. This requires concentration and willpower on the part of the male and trust on the part of the female. This trust is not always well founded and creates anxiety. Neither of these factors is conducive to relaxation and pleasure and may leave the couple with a distorted idea of what sexual pleasure is or can be. 2. Abstinence - abstaining from intercourse but continue with the sexual relationship with the wife.
86
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Secrets in NumbersDocument26 pagesSecrets in Numbersmdkafzal100% (5)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Ultimate 30 Day Guide To Going Full Carnivore PDFDocument76 pagesThe Ultimate 30 Day Guide To Going Full Carnivore PDFJanZen100% (1)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Interactive Notebook Pieces PDFDocument15 pagesInteractive Notebook Pieces PDFAshley JohnsonNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Father Seraphim Rose and GeocentrismDocument5 pagesFather Seraphim Rose and GeocentrismDan Constantin67% (6)
- STS Gene TherapyDocument12 pagesSTS Gene Therapyedgar malupengNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Medical-Surgical Nursing ReviewDocument90 pagesMedical-Surgical Nursing Reviewɹǝʍdןnos99% (312)
- Gomez Vs PalomarDocument2 pagesGomez Vs PalomarKim Lorenzo CalatravaNo ratings yet
- Perspective in PharmacyDocument3 pagesPerspective in PharmacyAgniez Hannah Permites100% (4)
- Divorce Bill in The PhilippinesDocument19 pagesDivorce Bill in The PhilippinesNeiqui Aubrey Antaran CañeteNo ratings yet
- KYLE DE VERA BSA-3A (Auditing & Assurance in SPCL Industries MT Exam) AnswersDocument3 pagesKYLE DE VERA BSA-3A (Auditing & Assurance in SPCL Industries MT Exam) AnswersKyree Vlade100% (1)
- How To Love The LORD With All Your Heart, Soul, and StrengthDocument5 pagesHow To Love The LORD With All Your Heart, Soul, and StrengthGodmadeMusic100% (1)
- CancerDocument8 pagesCancerRichard S. RoxasNo ratings yet
- Evidence-Based Medicine: The Basics: Will Olmstadt, MS, MPHDocument14 pagesEvidence-Based Medicine: The Basics: Will Olmstadt, MS, MPHRichard S. RoxasNo ratings yet
- 14 1 1 Blood ConsumptionDocument3 pages14 1 1 Blood ConsumptionRichard S. RoxasNo ratings yet
- Critical+appraisal+RCT Su+May+LiewDocument34 pagesCritical+appraisal+RCT Su+May+LiewRichard S. RoxasNo ratings yet
- 35.5 Inches LengthDocument1 page35.5 Inches LengthRichard S. RoxasNo ratings yet
- AdvanceDocument5 pagesAdvanceRichard S. RoxasNo ratings yet
- EDICDocument13 pagesEDICRichard S. RoxasNo ratings yet
- Villi: RD THDocument2 pagesVilli: RD THRichard S. RoxasNo ratings yet
- Management of Hyperglycemia in Type 2 Diabetes A Patient-Centered ApproachDocument16 pagesManagement of Hyperglycemia in Type 2 Diabetes A Patient-Centered ApproachThawatchai NakkaratniyomNo ratings yet
- Things Needed2Document1 pageThings Needed2Richard S. RoxasNo ratings yet
- UKPDSDocument6 pagesUKPDSRichard S. RoxasNo ratings yet
- DM Update 2012Document64 pagesDM Update 2012Richard S. RoxasNo ratings yet
- AccordDocument2 pagesAccordRichard S. RoxasNo ratings yet
- NOVEMBER 16, 2013 12:00 PM-3:00 PM SVB Room 503: Week 1: Methods of ResearchDocument2 pagesNOVEMBER 16, 2013 12:00 PM-3:00 PM SVB Room 503: Week 1: Methods of ResearchRichard S. RoxasNo ratings yet
- CGM Week 2: Interstitial Fluid & Insulin PumpsDocument3 pagesCGM Week 2: Interstitial Fluid & Insulin PumpsRichard S. RoxasNo ratings yet
- Week 1: Vaccines History of Vaccines: POLIO VACCINE: 1930'sDocument2 pagesWeek 1: Vaccines History of Vaccines: POLIO VACCINE: 1930'sRichard S. RoxasNo ratings yet
- FertilizationDocument3 pagesFertilizationRichard S. RoxasNo ratings yet
- Week 1 Diabetes Pathophysiology and Glycemic ControlDocument10 pagesWeek 1 Diabetes Pathophysiology and Glycemic ControlRichard S. RoxasNo ratings yet
- Excitation CouplingDocument3 pagesExcitation CouplingRichard S. RoxasNo ratings yet
- Virology SyllabusDocument6 pagesVirology SyllabusRichard S. RoxasNo ratings yet
- Week 3: Vaccines RECOMBINANT DNA: Viral Subunit SummaryDocument3 pagesWeek 3: Vaccines RECOMBINANT DNA: Viral Subunit SummaryRichard S. RoxasNo ratings yet
- Ob 1Document61 pagesOb 1Richard S. RoxasNo ratings yet
- Pharmacology Case StudyDocument4 pagesPharmacology Case StudyRichard S. RoxasNo ratings yet
- Disaster Preparedness SyllabusDocument7 pagesDisaster Preparedness SyllabusRichard S. RoxasNo ratings yet
- Schedule of Activities 1st Sem '08-'09Document7 pagesSchedule of Activities 1st Sem '08-'09Richard S. RoxasNo ratings yet
- OB Sked Midterm 2008-09Document2 pagesOB Sked Midterm 2008-09Richard S. RoxasNo ratings yet
- Easy QuestionsDocument8 pagesEasy QuestionsRichard S. RoxasNo ratings yet
- The Nursing Process and Client TeachingDocument15 pagesThe Nursing Process and Client TeachingRichard S. RoxasNo ratings yet
- v072n10p257 PDFDocument8 pagesv072n10p257 PDFLmf DanielNo ratings yet
- Ds Mini ProjectDocument12 pagesDs Mini ProjectHarsh VartakNo ratings yet
- Organizational Behaviour PDFDocument4 pagesOrganizational Behaviour PDFmaria0% (1)
- Fading Memories of Pakistan (Presentation)Document14 pagesFading Memories of Pakistan (Presentation)yfs945xpjnNo ratings yet
- Present Tense Review for Motorcycle RepairDocument2 pagesPresent Tense Review for Motorcycle RepairFaheemuddin Veterans50% (2)
- SAP Training Program Proposal for StudentsDocument2 pagesSAP Training Program Proposal for StudentsAjay KumarNo ratings yet
- NystgmusDocument16 pagesNystgmusCheska Justine San JuanNo ratings yet
- 1.7 The Lagrangian DerivativeDocument6 pages1.7 The Lagrangian DerivativedaskhagoNo ratings yet
- GelSight - Measurement of Surface RoughnessDocument5 pagesGelSight - Measurement of Surface RoughnessXto PeregrinNo ratings yet
- SAP FICO Asset Accounting 1Document3 pagesSAP FICO Asset Accounting 1Ananthakumar ANo ratings yet
- Marketing Management: Amit Pandey +91-7488351996Document15 pagesMarketing Management: Amit Pandey +91-7488351996amit pandeyNo ratings yet
- Flyposting OrdinanceDocument2 pagesFlyposting OrdinanceJunil LagardeNo ratings yet
- Gandhi and Indian Economic Planning (Unit III)Document21 pagesGandhi and Indian Economic Planning (Unit III)Aadhitya NarayananNo ratings yet
- FortiEDR Product Overview TrainingDocument16 pagesFortiEDR Product Overview TrainingRafael Steven Soto del CampoNo ratings yet
- Chapter 16-Analyzing Qualitative DataDocument3 pagesChapter 16-Analyzing Qualitative DataLiko Pah TuafNo ratings yet
- Balay Dako Menu DigitalDocument27 pagesBalay Dako Menu DigitalCarlo -No ratings yet
- 01 Petrolo 224252Document7 pages01 Petrolo 224252ffontanesiNo ratings yet
- New Dll-Math Week 4-1Document3 pagesNew Dll-Math Week 4-1AstroNo ratings yet
- Edgar Allan Poe's "The RavenDocument3 pagesEdgar Allan Poe's "The RavenЖанна ФодееваNo ratings yet
- Executive Summary WynnDocument5 pagesExecutive Summary Wynnapi-505730347No ratings yet