Professional Documents
Culture Documents
Angiogenic Biomarkers Predict The Occurrence of Digital Ulcers in Systemic Sclerosis
Uploaded by
onlyforu_3Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Angiogenic Biomarkers Predict The Occurrence of Digital Ulcers in Systemic Sclerosis
Uploaded by
onlyforu_3Copyright:
Available Formats
Downloaded from ard.bmj.com on November 13, 2012 - Published by group.bmj.
com
Clinical and epidemiological research
EXTENDED REPORT
Angiogenic biomarkers predict the occurrence of digital ulcers in systemic sclerosis
Jrme Avouac,1,2 Christophe Meune,3 Barbara Ruiz,2 Pierre Olivier Couraud,2 Georges Uzan,4 Catherine Boileau,5 Andr Kahan,1 Gilles Chiocchia,2,6 Yannick Allanore1,2
Additional data (supplementary gures and tables) are published online only. To view these les please visit the journal online (http://ard.bmj. com/content/71/3.toc)
1Rheumatology
A department, Paris Descartes University, Cochin Hospital, APHP, Sorbonne Paris Cit, Paris, France 2INSERM U1016 and CNRS UMR8104, Paris Descartes University, Cochin Institute, Sorbonne Paris Cit, Paris, France 3Cardiology department, Paris Descartes University, Cochin Hospital, APHP, Sorbonne Paris Cit, Paris, France 4INSERM U972, Paul Brousse Hospital, Villejuif, France 5Hormonology and Molecular Genetics Department, Biochemistry Department, U.V.S.Q University, Ambroise Par Hospital, APHP, Boulogne, France 6Rheumatology Department, Ambroise Par Hospital, U.V.S.Q University, APHP, Boulogne, France Correspondence to Professor Yannick Allanore, Hpital Cochin, Service de rhumatologie A, 27 rue du Faubourg Saint Jacques, 75014 Paris, France; yannick.allanore@cch.aphp.fr Received 10 May 2011 Accepted 9 October 2011 Published Online First 15 November 2011
ABSTRACT Objective To evaluate the possible merit of endothelial markers for the prediction of ischaemic digital ulcers in patients with systemic sclerosis (SSc). Methods Circulating endothelial progenitor cells (EPC), circulating endothelial cells and serum levels of placental growth factor (PlGF), soluble vascular adhesion molecule and vascular endothelial growth factor were measured in a prospective cohort of 100 SSc patients. The primary outcome was the occurrence of one or more new ischaemic digital ulcers during a planned 3-year follow-up. Results After the follow-up period, 17 patients developed new digital ulcers. By multivariate analysis focused on biomarkers, high PlGF serum levels and low EPC counts were identied as predictors of the occurrence of at least one new digital ulcer. In a secondary model including biomarkers together with clinical SSc characteristics all predictors of digital ulcers dened by p0.1 in univariate analysis, high PlGF serum levels (HR 7.26, 95% CI 1.92 to 27.41) and a history of digital ulcers (HR 9.32, 95% CI 1.51 to 59.83) were identied as independent predictors of a new digital ulcer. In an alternative model excluding patients with a history of digital ulcers at baseline, high PlGF serum levels (HR 13.46, 95% CI 1.58 to 114.73) and low EPC counts (HR 7.95, 95% CI 2.09 to 30.09) remained predictive of new digital ulcer occurrence during follow-up. Conclusion This study identied high PlGF serum levels and low circulating EPC counts as predictors of new digital ulcers in SSc. It highlights the critical role of angiogenesis in this vascular outcome. These markers may improve digital ulcer risk stratication and therefore allow earlier therapeutic intervention.
Systemic sclerosis (SSc) is a severe connective tissue disease characterised by vascular, immune and brotic changes in the skin and some internal organs.1 Peripheral microvascular and cardiovascular alterations are key features of SSc, with outcome depending on the extent and severity of vascular lesions. Microvascular lesions underlie many manifestations of SSc, including ischaemic digital ulcers, pulmonary hypertension, primary heart involvement and scleroderma renal crisis (SRC). Digital ulcers are frequent in SSc, averaging 30% prevalence according to the European League Against Rheumatism (EULAR) Scleroderma Trial and Research Group (EUSTAR) registry, and represent a heavy burden due to their major impact on quality of life.24 In addition, digital ulcers are thought to be a clinical parameter of severe vasculopathy that can be
associated with or predict other vascular lesions.57 Treatment of digital ulcers remains challenging and the identication of reliable predictors of digital ulcers is still an unmet clinical need in SSc.3 4 Endothelial injury and insufcient endothelial repair are strong contributors to the genesis of the vasculopathy underlying digital ulcers. Circulating endothelial cell (CEC) levels in peripheral blood is a direct reection of vascular damage and more specically endothelial injury.8 Vascular damage in SSc is insufciently compensated by endothelial repair processes that relate to angiogenesis and vasculogenesis. Angiogenesis is insufcient in SSc, resulting from defective vascularisation and tissue hypoxia, despite elevated levels of proangiogenic factors in the serum or the skin of SSc patients such as vascular endothelial growth factor (VEGF), placental growth factor (PlGF) or soluble vascular cell adhesion molecule (sVCAM).912 Previous data have also emphasised quantitative perturbations of vasculogenesis.1315 In particular, we reported high circulating endothelial progenitor cell (EPC) levels in SSc, supporting their general mobilisation. However, low EPC numbers in the peripheral blood of SSc patients were associated with the presence of past and/or current digital ulcers, suggesting increased homing during active vascular disease and overall insufcient vasculogenesis to counterbalance vascular damage.14 16 Subsequent to this rst approach, the objective of this study was to determine the possible merit of different endothelial markers reecting endothelial injury, disturbed angiogenesis and vasculogenesis to predict the occurrence of digital ulcers.10 1215 1721 These biomarkers were also secondarily evaluated for the prediction of other cardiac/vascular events that rely on microvascular complications.
PATIENTS AND METHODS
Extended details of the methodology are shown in the supplementary data (available online only).
Study population
We prospectively evaluated 100 consecutive SSc patients who were hospitalised in the Rheumatology A Department, Cochin Hospital, Paris, France, for routine follow-up of the disease from 1 September 2006 to 1 November 2007. SSc was classied as limited cutaneous or diffuse cutaneous subset according to the criteria reported by LeRoy et al.22 Inclusion and exclusion criteria are detailed in the supplementary data (available online only).
394
Ann Rheum Dis 2012;71:394399. doi:10.1136/annrheumdis-2011-200143
Downloaded from ard.bmj.com on November 13, 2012 - Published by group.bmj.com
Clinical and epidemiological research
Follow-up
Once included in the study cohort, patients were seen by his/ her usual physician on a regular basis of 36 month intervals, as indicated by their disease severity, and were hospitalised at least annually for clinical evaluation, including echocardiography and pulmonary function tests. The nal study observation was planned as the last observation of the last trimester of the year 2010 (or the last available observation) or the last observation at the time of death from any cause, with analyses and completion of the database performed during the rst trimester of the year 2011.
RESULTS Baseline characteristics
The meanSD age of the 100 patients (89 women) was 5613 years and the meanSD disease duration was 98 years. Forty patients had the diffuse cutaneous subset, and 60 the limited. Their baseline characteristics are shown in table 1.
Baseline values and correlation between vascular markers
The median (IQR) number of EPC and CEC in peripheral blood of SSc patients was 99 (64164) and 215 (12708)/106 Linmononuclear cells, respectively. The median (IQR) serum levels of VEGF, PlGF and sVCAM were 352 (183474) pg/ml, 61 (3387) pg/ml and 614 (4869819) ng/ml, respectively. Among these vascular markers, only baseline values of EPC and CEC were correlated (r=0.52, p<0.0001).
Outcome measures
The primary outcome was the occurrence of at least one or more ischaemic digital ulcers, dened by a painful area of 2 mm or greater in diameter with visible depth and loss of dermis, amenable to healing and localised by ngertip. Digital ulcers caused by conditions other than SSc and non-ischaemic digital ulcers were not taken into consideration. The secondary outcome was the occurrence of at least one new cardiac or vascular event, as a consequence of the generalised vasculopathy. Cardiac/vascular events were assessed by an exploratory index, dened as the occurrence of at least one of the following events: (1) one or more new ischaemic digital ulcers; (2) pre-capillary pulmonary hypertension conrmed by resting mean pulmonary artery pressure of 25 mm Hg or greater together with a pulmonary capillary wedge pressure of 15 mm Hg or less; (3) left ventricular dysfunction, dened by a left ventricular ejection fraction less than 50%, as determined using the Simpson method; (4) SRC, dened by a sudden and marked increase in systemic blood pressure and acute renal failure, with or without signicant microangiopathic haemolytic anaemia or thrombocytopenia.6 23 We also considered as a secondary outcome the occurrence of death from any cause during the followup period.
Primary outcome, occurrence of ischaemic digital ulcers
During a follow up period of 2913 months (median 36 months), new ischaemic digital ulcers occurred in 17 SSc patients (10 patients with a history of previous digital ulcers and seven patients with no previous digital ulcers). The mean time to the development of new digital ulcers after study inclusion was 18 months (median 17 months). By univariate analysis, low EPC numbers (HR 3.94, 95% CI 1.41 to 11.03, p=0.009), high PlGF (HR 8.25, 95% CI 1.78 to 38.26, p=0.007) and sVCAM (HR 3.14, 95% CI 1.01 to 9.83, p=0.04) serum levels were identied as predictive biomarkers of the occurrence of at least one new digital ulcer (table 2). KaplanMeyer analyses of freedom from the occurrence of new digital ulcers for these three markers are shown in gures 1AC. Multivariate Cox analysis conrmed PlGF levels (HR 7.95, 95% CI 2.09 to 30.10, p=0.002) and EPC levels (HR 2.33, 95% CI 1.44 to 12.22, p=0.03) as independent predictors of the development of digital ulcers (table 2). In a second multivariate Cox model including these two biomarkers and all other predictors of digital ulcers dened by a p value of 0.1 or less in univariate analysis, high PlGF serum levels (HR 7.26, 95% CI 1.92 to 27.41) and a history of digital ulcers (HR 9.32, 95% CI 1.51 to 59.83) were identied in multivariate analysis as independent predictors of new digital ulcers (table 2).
EPC and CEC sorting and ow cytometry quantication
We used a method previously described and validated to enrich mononuclear cells and quantify EPC and CEC by ow cytometry.14 24 This method is described in detail in the supplementary data (available online only).
VEGF, PlGF and sVCAM ELISA
Serum levels of VEGF, PlGF and sVCAM were measured using the quantitative sandwich ELISA technique (Quantikine kits; R&D Systems, Minneapolis, MN).
Table 1
Baseline characteristics of patients with SSc
SSc (n=100) 5613 98 60/40 29 42 22 17 803 89 41 30 27 31 39 100 26 27
Statistical analysis
To estimate the cut-off of each endothelial marker, we compared levels of EPC, CEC, VEGF, PlGF and sVCAM between SSc patients and a group of 20 healthy controls (15 women, 5516 years old), assessed during the same study period. These results revealed that the median value of all the markers for SSc patients were above the 95th percentile of the levels observed in the controls; therefore, to evaluate their predictive value on clinical outcomes, levels of EPC, CEC, VEGF, PlGF and sVCAM were considered as categorical variables, and associations were assessed according to the median value of each endothelial marker. Predictors of digital ulcers and cardiac/vascular outcomes were evaluated by univariate and multivariate Cox proportional hazards models and summarised as HR and 95% CI. Survival was evaluated using the KaplanMeier method.
Ann Rheum Dis 2012;71:394399. doi:10.1136/annrheumdis-2011-200143
Age (years), mean SD Disease duration (years), mean SD Limited/diffuse cutaneous subset, n History of digital ulcers, n Pulmonary brosis on CT scan, n ESR >28 mm H1, n CRP >10 mg/l, n Serum creatinine, moles/l, mean SD Positive antinuclear antibodies (>1/160), n Positive antitopoisomerase 1 antibodies, n Positive anticentromere antibodies, n (%) FVC <75% predicted, n DLCO/AV <75% predicted, n Medsger severity scale >2, n Calcium antagonists, n ACE inhibitors, n Low dose oral prednisone, n
DLCO/AV, diffusing capacity for carbon monoxide/alveolar volume; CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; FVC, forced vital capacity; SSC, systemic sclerosis.
395
Downloaded from ard.bmj.com on November 13, 2012 - Published by group.bmj.com
Clinical and epidemiological research
Table 2 Primary outcome: results of univariate and multivariate analyses of candidate predictors of digital ulcers, by model analysed
Univariate analysis Baseline characteristics p Value HR (95% CI) Multivariate analysis p Value HR (95% CI)
Main model: evaluation of different biomarkers for the occurrence of new ischaemic digital ulcers Low EPC (<99 EPC/106 Lin-mononuclear cells) 0.009* High CEC (215 CEC/106 Lin-mononuclear cells) 0.4 High serum VEGF (352 pg/ml) 0.7 High serum PlGF (61 pg/ml) 0.007* High serum sVCAM (614 ng/ml) 0.04* Alternative model: inclusion of biomarkers and other SSc disease characteristics with a p value 0.1 Low EPC (<99 EPC/106 Lin-mononuclear cells) 0.009* High serum PlGF (61 pg/ml) 0.007* History of digital ulcers 0.0004* ESR >28 mm H1 0.1* Alternate model: exclusion of patients with a history of digital ulcers Low EPC (<99 EPC /106 Lin-mononuclear cells) 0.009* High serum PlGF (61 pg/ml) ESR >28 mm H1 0.007* ESR >28 mm H1 0.1*
3.94 (1.41 to 11.03) 1.47 (0.56 to 3.84) 1.19 (0.44 to 3.07) 8.25 (1.78 to 38.26) 3.14 (1.01 to 9.83) 3.94 (1.41 to 11.03) 8.25 (1.78 to 38.26) 9.96 (2.79 to 35.59) 2.18 (0.8 to 5.61) 3.94 (1.41 to 11.03) 8.25 (1.78 to 38.26) 2.18 (0.89 to 5.61)
0.03 NA NA 0.002 0.1 0.07 0.02 0.01 0.1 0.04 0.03 0.8
2.33 (1.44 to 12.22) 7.95 (2.09 to 30.10) 2.01 (0.43 to 9.42) 2.21 (0.89 to 11.78) 7.26 (1.92 to 27.41) 9.32 (1.51 to 59.83) 4.00 (0.689 to 23.59) 7.95 (2.09 to 30.09) 13.46 (1.58 to 114.73) 1.81 (0.099 to 6.68)
*Variables included in the multivariate Cox regression analysis. CEC, circulating endothelial cells; DLCO/AV, diffusing capacity for carbon monoxide/alveolar volume; EPC, endothelial progenitor cells; ESR, erythrocyte sedimentation rate; NA, not applicable, PlGF, placental growth factor; sVCAM: soluble vascular cell adhesion molecule; VEGF, vascular endothelial growth factor.
In a third model excluding patients with a history digital ulcers at baseline, high PlGF serum levels (HR 13.46, 95% CI 1.58 to 114.73) and low EPC counts (HR 7.95, 95% CI 2.09 to 30.09) were found to be predictors of new digital ulcers (table 2).
Secondary outcomes
During the follow up period, 27 of the 100 patients developed at least one cardiac or vascular event: new ischaemic digital ulcers in 17, precapillary pulmonary hypertension in ve, left ventricular dysfunction in four and SRC in a single patient. The mean time to the development of a cardiac/vascular event was 19 months (median 20 months). Seven patients died during the follow-up period. Causes of death were precapillary pulmonary hypertension in four patients (three patients with pulmonary arterial hypertension and one with pulmonary hypertension secondary to interstitial lung disease), right heart failure secondary to myocardial brosis in one patient, serious infection in one patient and severe inammatory myositis associated with SSc in one patient. According to our exploratory index, low circulating EPC numbers, high PlGF and high sVCAM serum levels were identied in univariate and multivariate Cox analyses as predictors of cardiac and vascular events in SSc (table 3). In a second model including these three biomarkers and other predictors of cardiac/vascular events dened by a p value of 0.1 or less in univariate analysis, low EPC counts (HR 5.14, 95% CI 1.21 to 21.80) and high PlGF serum levels (HR 5.32, 95% CI 1.24 to 22.91) were identied in multivariate analysis as independent predictors of the occurrence of cardiac and vascular events in SSc patients (table 3). In addition, low EPC counts, high PlGF and sVCAM serum levels were predictive in univariate Cox analysis of the occurrence of death during the study period, but this was not conrmed by multivariate analysis.
DISCUSSION
This is the rst prospective study to demonstrate that increased serum PlGF levels and circulating EPC levels predict the subsequent development of digital ulcers in patients with SSc. The identication of relevant predictive biomarkers may allow the detection of a subset of patients who might be candidates for preventive therapeutic strategies.3 4
396
Digital ulcers are a frequent complication in patients with SSc. The origin of ulcers is multifactorial. Ischaemia due to vascular disease, sclerodactily, calcinosis and local trauma may all contribute to ulcer initiation.25 Then, the development of digital ulcers results from poor blood ow and tissue hypoxia. Whatever its origin, digital ulcers are often extremely painful, cause signicant impairment of hand function and activities of daily living, infection, digital resorption, and as a consequence markedly alter quality of life.3 Scarce data are available regarding the incidence of new ischaemic digital ulcers in SSc. The number of patients who developed new digital ulcers was less important in our cohort than in the placebo group of the RAPIDS-1 study (17 of 100 patients with at least one new digital ulcers vs 26 of 43 patients in the RAPIDS-1 study), a study that assessed the preventive effect of bosentan for ischaemic digital ulcers.3 Based on the high number of patients with active digital ulcers (24/43 patients from the placebo group of the RAPIDS-1 study had active digital ulcers at baseline), we assume that the exclusion of patients with active digital ulcers in our study accounts for this difference. Our results have identied high serum PlGF levels as a predictor of the development of digital ulcers in SSc patients with or without a history of digital ulcers. PlGF, a secreted dimeric glycoprotein very similar to VEGF, has been shown to be chemotactic and mitogenic for endothelial cells in vitro and proangiogenic in vivo.18 19 PlGF has been reported to be dysregulated in preeclampsia, a severe vascular complication of pregnancy. Two recent cross-sectional studies have reported elevated serum PlGF levels in SSc patients compared with healthy controls.12 20 Together with our results, these ndings suggest a possible contribution of this proangiogenic protein in SSc vascular disturbances. Increased levels of PlGF, reecting increased angiogenesis, were predictive of the development of digital ulcers, in which there is a loss of vessels. Digital ulcers are associated with a destructive vasculopathy, which is a source of tissue hypoxia, one of the major stimuli of angiogenesis.17 25 Therefore, elevated angiogenic markers, including PlGF, may appear as an attempt at a compensatory response to maintain vascular function with the formation of new vessels, which might lead to enhanced capillary formation. Increased serum levels of angiostatic markers,
Ann Rheum Dis 2012;71:394399. doi:10.1136/annrheumdis-2011-200143
Downloaded from ard.bmj.com on November 13, 2012 - Published by group.bmj.com
Clinical and epidemiological research
Figure 1 (A, B): KaplanMeier analyses of freedom from ischaemic digital ulcers in 100 patients with systemic sclerosis (SSc). Curves are shown for SSc patients who had circulating endothelial progenitor cell (EPC) levels less than 99 and 99/106 or greater Lin-mononuclear cells at study entry (p<0.0001) (A), or in those who had placental growth factor (PlGF) serum levels 61 or greater and less than 61 pg/ml at study entry (p<0.0001) (B), or in those who had vascular cell adhesion molecule (sVCAM) serum levels less than 614 and 614 ng/ml or greater at study entry (C). Table 3 Results of univariate and multivariate analyses of candidate predictors of predened secondary outcomes
Baseline characteristics Cardiac/vascular events (N=27) Evaluation of different biomarkers for the occurrence of cardiac/vascular events Low EPC (<99 EPC/106 Lin-mononuclear cells) High CEC (215 CEC/106 Lin-mononuclear cells) High serum VEGF (352 pg/ml) High serum PlGF (61 pg/ml) High serum sVCAM (614 ng/ml) Inclusion of biomarkers and other SSc disease characteristics with a p value 0.1 Low EPC (<99 EPC/106 Lin-mononuclear cells) High serum PlGF (61 pg/ml) High serum sVCAM (614 ng/ml) History of digital ulcers DLCO/AV <70% ESR >28 mm H1 Evaluation of different biomarkers for the occurrence of death Low EPC (<99 EPC/106 Lin-mononuclear cells) High CEC (215 CEC/106 Lin-mononuclear cells) High serum VEGF (352 pg/ml) High serum PlGF (61 pg/ml) High serum sVCAM (614 ng/ml) Univariate analysis p Value* HR (95% CI) 0.0004* 0.8 0.9 0.0004* 0.02* 0.0004* 0.0004* 0.02* 0.02* 0.07* 0.1* 0.0004* 0.8 0.9 0.0004* 0.02* 4.72 (2.02 to 11.04) 1.09 (0.51 to 2.31) 0.99 (0.47 to 2.11) 10.12 (3.36 to 30.50) 2.81 (1.17 to 6.75) 4.72 (2.02 to 11.04) 10.12 (3.36 to 30.50) 2.81 (1.17 to 6.75) 2.69 (1.21 to 5.97) 1.93 (0.939 to 4.01) 1.80 (0.849 to 3.86) 4.72 (2.02 to 11.04) 1.09 (0.519 to 2.31) 0.99 (0.479 to 2.11) 9.34 (2.70 to 32.26) 2.81 (1.179 to 6.75 Multivariate analysis p Value HR (95% CI) 0.03 NA NA 0.02 0.02 0.03 0.02 0.06 0.8 0.2 0.09 0.1 NA NA 0.9 0.07 3.18 (1.19 to 12.80) 5.01 (1.229 to 20.41) 3.27 (1.19 to 8.97) 5.14 (1.21 to 21.80) 5.32 (1.24 to 22.91) 3.02 (0.98 to 9.27) 1.25 (0.369 to 4.41) 1.46 (0.89 to 3.26) 2.90 (0.84 to 10.03) 9.05 (0.64 to 127.10) 1.09 (0.11 to 10.85) 8.45 (0.82 to 87.12)
Death from any cause (N=7)
*Variables included in the multivariate Cox regression analysis. AV, alveolar volume; CEC, circulating endothelial cells; DLCO, diffusing capacity for carbon monoxide; EPC, endothelial progenitor cells; ESR, erythrocyte sedimentation rate; PlGF, placental growth factor; SSc, systemic sclerosis; sVCAM, soluble vascular cell adhesion molecule; VEGF, vascular endothelial growth factor.
such as thrombospondin 1, endoglin or endostatin, have been reported in SSc and might also contribute to the lack of angiogenesis despite increased levels of angiogenic biomarkers. Our results also show that decreased EPC levels independently predict the occurrence of digital ulcers in SSc patients without any sign of previous digital ulcers. This is in accordance with our previous results, which showed a higher likelihood of digital ulcers in patients with low EPC levels. In contrast to the measurement of a single serum marker for the prediction of risk,
Ann Rheum Dis 2012;71:394399. doi:10.1136/annrheumdis-2011-200143
the use of a cellular marker of risk, such as the level of EPC, unies the complex interactions of multiple negative factors and may yield a better picture of in-vivo mechanisms. While we hypothesise that an accurate identication of highrisk patients using PlGF and EPC levels will hasten the detection of digital ulcers and the introduction of adequate treatment at a time period when they may be of greater efcacy, this remains to be conrmed in dedicated studies. Further explorations are therefore now needed to assess PlGF and EPC as biomarkers of
397
Downloaded from ard.bmj.com on November 13, 2012 - Published by group.bmj.com
Clinical and epidemiological research
digital ulcers in terms of screening, diagnostic evaluation and response to therapy. SSc is the most life threatening of the connective tissue disorders, although survival rates have improved in recent years.26 27 Heart involvement and pulmonary brosis are the main causes of morbidity and mortality.7 2830 Consistent with these observations, ve of seven deaths that occurred in our cohort were related to primary heart involvement and precapillary pulmonary hypertension. The development of new cardiac/vascular events was frequent in our cohort after a mean follow-up of 29 months, with 27 new events. EPC and PlGF levels were also predictive of cardiac/vascular involvement dened as an exploratory composite index. This latter included digital ulcers, pulmonary hypertension, left ventricular dysfunction and SRC, as these complications all rely on the generalised vasculopathy. This observation is sustained by the well-established association between digital ulcers and pulmonary hypertension, as well as the most recent data showing an association between left ventricular dysfunction and digital ulcers.57 31 However, such a composite index, including both cardiac and vascular manifestations, will require further validation. CEC levels have been correlated with endothelial dysfunction and were found to be elevated in patients with atherosclerosis, cancer or SSc.13 15 24 32 Elevated serum VEGF and sVCAM levels, such as elevated skin VEGF levels,10 17 have also been reported in SSc. However, none of these three biomarkers was predictive of the development of digital ulcers in SSc patients. This study should be interpreted within its limitations. We cannot comment on patients with known renal or cardiac failure as they were excluded from the study. Despite the recent elaboration of dedicated recommendations, the detection of EPC by ow cytometry in peripheral blood remains challenging. No consensual technique of cell enrichment before uorescenceactivated cell sorter analysis or a combination of surface markers has yet been validated.33 Therefore, further studies are necessary regarding EPC quantication before being used routinely. Conversely, serum PlGF measurement by quantitative sandwich ELISA is easier to handle and more standardised, which suggests an easier application in routine care. The number of patients who developed precapillary pulmonary hypertension, left ventricular dysfunction and SRC was too low to allow the rm identication of predictors. Further studies with a greater sample size and larger population are thus warranted to assess the predictive value of endothelial biomarkers for the development of these cardiac and vascular complications. This would also allow subgroup analyses according to the different causes of pulmonary hypertension and left ventricular dysfunction. We did not perform a systematic capillaroscopic evaluation at inclusion, which prevented us from determining the value of this examination for the development of ischaemic digital ulcers. However, the merit of capillaroscopy for digital ulcer prediction is now under investigation in a European observational study (CAP study, protocol number AC-052-521). In conclusion, our results suggest that circulating EPC counts and serum PlGF levels can be used to identify SSc patients who are at risk of the development of digital ulcers during a median 36-month follow-up period. This may have important clinical implications, in that non-invasive tests may be used to identify high-risk patients who should undergo more careful evaluation. Further studies assessing the use of these markers in therapeutic strategies aimed at the selection of patients for early treatment or preventive therapy are indicated.
398 Contributors Study design: JA, YA. Acquisition of data: JA, CM, BR. Analysis and interpretation of data: JA, CM, BR, YA. Manuscript preparation: JA, CM, POC, GU, CB, AK, GC, YA. Statistical analysis: JA, CM, YA. Funding This study received nancial support from the Socit Franaise de Rhumatologie, Association des Sclrodermiques de France, Groupe Franais de Recherche sur la Sclrodermie (bourse AMPLI), INSERM, Agence Nationale pour la Recherche (grant no R07094KS) and Fond dEtude et de Recherche du Corps Mdical des Hpitaux de Paris. It was also supported by an investigator-initiated research grant from Pzer Ltd. Competing interests None. Ethics approval Ethics approval was received from CPP Ile de France 3. Provenance and peer review Not commissioned; externally peer reviewed.
REFERENCES
1. Allanore Y, Avouac J, Wipff J, et al. New therapeutic strategies in the management of systemic sclerosis. Expert Opin Pharmacother 2007;8:60715. 2. Avouac J, Walker U, Tyndall A, et al. Characteristics of joint involvement and relationships with systemic inammation in systemic sclerosis: results from the EULAR Scleroderma Trial and Research Group (EUSTAR) database. J Rheumatol 2010;37:1488501. 3. Korn JH, Mayes M, Matucci Cerinic M, et al. Digital ulcers in systemic sclerosis: prevention by treatment with bosentan, an oral endothelin receptor antagonist. Arthritis Rheum 2004;50:398593. 4. Matucci-Cerinic M, Denton CP, Furst DE, et al. Bosentan treatment of digital ulcers related to systemic sclerosis: results from the RAPIDS-2 randomised, double-blind, placebo-controlled trial. Ann Rheum Dis 2011;70:328. 5. Avouac J, Air P, Meune C, et al. Prevalence of pulmonary hypertension in systemic sclerosis in European Caucasians and metaanalysis of 5 studies. J Rheumatol 2010;37:22908. 6. Allanore Y, Meune C, Vonk MC, et al. Prevalence and factors associated with left ventricular dysfunction in the EULAR Scleroderma Trial and Research group (EUSTAR) database of patients with systemic sclerosis. Ann Rheum Dis 2010;69:21821. 7. Steen V, Medsger TA Jr. Predictors of isolated pulmonary hypertension in patients with systemic sclerosis and limited cutaneous involvement. Arthritis Rheum 2003;48:51622. 8. Erdbruegger U, Haubitz M, Woywodt A. Circulating endothelial cells: a novel marker of endothelial damage. Clin Chim Acta 2006;373:1726. 9. Distler O, Del Rosso A, Giacomelli R, et al. Angiogenic and angiostatic factors in systemic sclerosis: increased levels of vascular endothelial growth factor are a feature of the earliest disease stages and are associated with the absence of ngertip ulcers. Arthritis Res 2002;4:R11. 10. Allanore Y, Borderie D, Lemarchal H, et al. Nifedipine decreases sVCAM-1 concentrations and oxidative stress in systemic sclerosis but does not affect the concentrations of vascular endothelial growth factor or its soluble receptor 1. Arthritis Res Ther 2004;6:R30914. 11. Wipff J, Avouac J, Borderie D, et al. Disturbed angiogenesis in systemic sclerosis: high levels of soluble endoglin. Rheumatology (Oxford) 2008;47:9725. 12. Hummers LK, Hall A, Wigley FM, et al. Abnormalities in the regulators of angiogenesis in patients with scleroderma. J Rheumatol 2009;36:57682. 13. Allanore Y, Batteux F, Avouac J, et al. Levels of circulating endothelial progenitor cells in systemic sclerosis. Clin Exp Rheumatol 2007;25:606. 14. Avouac J, Juin F, Wipff J, et al. Circulating endothelial progenitor cells in systemic sclerosis: association with disease severity. Ann Rheum Dis 2008;67:145560. 15. Del Papa N, Colombo G, Fracchiolla N, et al. Circulating endothelial cells as a marker of ongoing vascular disease in systemic sclerosis. Arthritis Rheum 2004;50:1296304. 16. Koch AE, Distler O. Vasculopathy and disordered angiogenesis in selected rheumatic diseases: rheumatoid arthritis and systemic sclerosis. Arthritis Res Ther 2007;9 (Suppl 2):S3. 17. Distler O, Distler JH, Scheid A, et al. Uncontrolled expression of vascular endothelial growth factor and its receptors leads to insufcient skin angiogenesis in patients with systemic sclerosis. Circ Res 2004;95:10916. 18. Maglione D, Guerriero V, Viglietto G, et al. Isolation of a human placenta cDNA coding for a protein related to the vascular permeability factor. Proc Natl Acad Sci U S A 1991;88:926771. 19. Ziche M, Maglione D, Ribatti D, et al. Placenta growth factor-1 is chemotactic, mitogenic, and angiogenic. Lab Invest 1997;76:51731. 20. Hamaguchi Y, Hasegawa M, Tanaka C, et al. Elevated serum placenta growth factor (PlGF) levels in patients with systemic sclerosis: a possible role in the development of skin but not lung brosis. J Dermatol Sci 2010;58:22931. 21. Kahaleh B, Meyer O, Scorza R. Assessment of vascular involvement. Clin Exp Rheumatol 2003;21(3 Suppl 29):S914. 22. LeRoy EC, Black C, Fleischmajer R, et al. Scleroderma (systemic sclerosis): classication, subsets and pathogenesis. J Rheumatol 1988;15:2025. 23. Steen VD, Costantino JP, Shapiro AP, et al. Outcome of renal crisis in systemic sclerosis: relation to availability of angiotensin converting enzyme (ACE) inhibitors. Ann Intern Med 1990;113:3527.
Ann Rheum Dis 2012;71:394399. doi:10.1136/annrheumdis-2011-200143
Downloaded from ard.bmj.com on November 13, 2012 - Published by group.bmj.com
Clinical and epidemiological research
24. Khan SS, Solomon MA, McCoy JP Jr. Detection of circulating endothelial cells and endothelial progenitor cells by ow cytometry. Cytometry B Clin Cytom 2005;64:18. 25. Avouac J, Wipff J, Goldman O, et al. Angiogenesis in systemic sclerosis: impaired expression of vascular endothelial growth factor receptor 1 in endothelial progenitorderived cells under hypoxic conditions. Arthritis Rheum 2008;58:355061. 26. Ioannidis JP, Vlachoyiannopoulos PG, Haidich AB, et al. Mortality in systemic sclerosis: an international meta-analysis of individual patient data. Am J Med 2005;118:210. 27. Ferri C, Valentini G, Cozzi F, et al. Systemic sclerosis: demographic, clinical, and serologic features and survival in 1,012 Italian patients. Medicine (Baltimore) 2002;81:13953. 28. Meune C, Vignaux O, Kahan A, et al. Heart involvement in systemic sclerosis: evolving concept and diagnostic methodologies. Arch Cardiovasc Dis 2010;103:4652. 29. Mukerjee D, St George D, Coleiro B, et al. Prevalence and outcome in systemic sclerosis associated pulmonary arterial hypertension: application of a registry approach. Ann Rheum Dis 2003;62:108893. 30. Kawut SM, Taichman DB, Archer-Chicko CL, et al. Hemodynamics and survival in patients with pulmonary arterial hypertension related to systemic sclerosis. Chest 2003;123:34450. 31. Manetti M, Allanore Y, Revillod L, et al. A genetic variation located in the promoter region of the UPAR (CD87) gene is associated with the vascular complications of systemic sclerosis. Arthritis Rheum 2011;63:24756. 32. Boos CJ, Soor SK, Kang D, et al. Relationship between circulating endothelial cells and the predicted risk of cardiovascular events in acute coronary syndromes. Eur Heart J 2007;28:1092101. 33. Distler JH, Allanore Y, Avouac J, et al. EULAR Scleroderma Trials and Research group statement and recommendations on endothelial precursor cells. Ann Rheum Dis 2009;68:1638. 34. Amanzi L, Braschi F, Fiori G, et al. Digital ulcers in scleroderma: staging, characteristics and sub-setting through observation of 1614 digital lesions. Rheumatology (Oxford) 2010;49:137482.
Ann Rheum Dis 2012;71:394399. doi:10.1136/annrheumdis-2011-200143
399
Downloaded from ard.bmj.com on November 13, 2012 - Published by group.bmj.com
Angiogenic biomarkers predict the occurrence of digital ulcers in systemic sclerosis
Jrme Avouac, Christophe Meune, Barbara Ruiz, et al. Ann Rheum Dis 2012 71: 394-399 originally published online November 15, 2011
doi: 10.1136/annrheumdis-2011-200143
Updated information and services can be found at:
http://ard.bmj.com/content/71/3/394.full.html
These include:
Data Supplement References Email alerting service
"Web Only Data"
http://ard.bmj.com/content/suppl/2011/11/15/annrheumdis-2011-200143.DC1.html
This article cites 34 articles, 13 of which can be accessed free at:
http://ard.bmj.com/content/71/3/394.full.html#ref-list-1
Receive free email alerts when new articles cite this article. Sign up in the box at the top right corner of the online article.
Topic Collections
Articles on similar topics can be found in the following collections Connective tissue disease (2845 articles) Epidemiology (946 articles)
Notes
To request permissions go to:
http://group.bmj.com/group/rights-licensing/permissions
To order reprints go to:
http://journals.bmj.com/cgi/reprintform
To subscribe to BMJ go to:
http://group.bmj.com/subscribe/
You might also like
- NIH Public Access: Author ManuscriptDocument11 pagesNIH Public Access: Author Manuscriptonlyforu_3No ratings yet
- Decision Summary: Decision Memo For Electrodiagnostic Sensory Nerve Conduction Threshold (CAG-00106N)Document12 pagesDecision Summary: Decision Memo For Electrodiagnostic Sensory Nerve Conduction Threshold (CAG-00106N)onlyforu_3No ratings yet
- 1793Document5 pages1793onlyforu_3No ratings yet
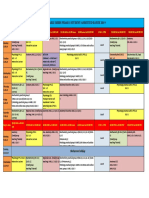
- TIME TABLE MBBS PHASE I STUDENT FinalDocument32 pagesTIME TABLE MBBS PHASE I STUDENT Finalonlyforu_3No ratings yet
- Evaluation of Clinical Tools and Their Diagnostic Use in Distalsymmetric PolyneuropathyDocument8 pagesEvaluation of Clinical Tools and Their Diagnostic Use in Distalsymmetric Polyneuropathyonlyforu_3No ratings yet
- TIME TABLE MBBS PHASE I STUDENT FinalDocument32 pagesTIME TABLE MBBS PHASE I STUDENT Finalonlyforu_3No ratings yet
- Comparing neuropathy tests in diabetes patientsDocument4 pagesComparing neuropathy tests in diabetes patientsonlyforu_3No ratings yet
- 1793Document5 pages1793onlyforu_3No ratings yet
- Long vs short nerve segments for assessing peripheral nerve functionDocument5 pagesLong vs short nerve segments for assessing peripheral nerve functiononlyforu_3No ratings yet
- Usefulness of Monofilament Testing For Detecting Peripheral Neuropathy IDocument5 pagesUsefulness of Monofilament Testing For Detecting Peripheral Neuropathy Ionlyforu_3No ratings yet
- Training Resource Materials PrelimsDocument20 pagesTraining Resource Materials Prelimsonlyforu_3100% (1)
- Preparationofbloodcomponentsandtheirtherapeuticuses 150620135006 Lva1 App6892Document63 pagesPreparationofbloodcomponentsandtheirtherapeuticuses 150620135006 Lva1 App6892onlyforu_3No ratings yet
- Communication SkillsDocument24 pagesCommunication Skillsonlyforu_3No ratings yet
- Busch Bacher 1998Document7 pagesBusch Bacher 1998onlyforu_3No ratings yet
- Professional Blood Pressure Monitors: Minamata Convention On Mercury'Document4 pagesProfessional Blood Pressure Monitors: Minamata Convention On Mercury'onlyforu_3No ratings yet
- Immunity and AllergyDocument72 pagesImmunity and Allergyonlyforu_3No ratings yet
- Spirodoc ENGDocument6 pagesSpirodoc ENGbhushan vichareNo ratings yet
- HX TakingDocument37 pagesHX TakingAya SalahNo ratings yet
- File 1757Document2 pagesFile 1757DanOlteanuNo ratings yet
- Computer Assisted Learning: Perceptions and Knowledge Skills of Undergraduate Medical Students in A Malaysian Medical SchoolDocument5 pagesComputer Assisted Learning: Perceptions and Knowledge Skills of Undergraduate Medical Students in A Malaysian Medical Schoolonlyforu_3No ratings yet
- Cranial NervesDocument0 pagesCranial Nervesjeenath justin dossNo ratings yet
- Simulated Animal Experiments in Teaching and Research PDFDocument7 pagesSimulated Animal Experiments in Teaching and Research PDFonlyforu_3No ratings yet
- Blood Pressure EstimationDocument16 pagesBlood Pressure Estimationonlyforu_3No ratings yet
- Exercise Effects On Systemic ImmunityDocument18 pagesExercise Effects On Systemic Immunityonlyforu_3No ratings yet
- PulseDocument7 pagesPulseonlyforu_3No ratings yet
- FumigationDocument77 pagesFumigationAnsari KashifNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- ABpsych NewpppDocument15 pagesABpsych NewpppMarbie Aliyah B. PagadorNo ratings yet
- Fundamentals of Rheumatoid Arthritis and Various Homoeopathic Trials in Patients of Rheumatoid Arthritis: An UpdateDocument6 pagesFundamentals of Rheumatoid Arthritis and Various Homoeopathic Trials in Patients of Rheumatoid Arthritis: An UpdateHomoeopathic PulseNo ratings yet
- He367t R1 RCDocument2 pagesHe367t R1 RCSedighe VafaieNo ratings yet
- 2014 Fundamentals of Skeletal Radiology, 4eDocument239 pages2014 Fundamentals of Skeletal Radiology, 4eLuís RobertoNo ratings yet
- Suz 183Document29 pagesSuz 183Benny Chris TantoNo ratings yet
- Roleplay Procedure Nasogastric Incubation (NGT)Document3 pagesRoleplay Procedure Nasogastric Incubation (NGT)naimathur rodiyahNo ratings yet
- My SukshamvyamDocument6 pagesMy SukshamvyamsurendermadaanNo ratings yet
- Intubasi Sulit: Nur Hajriya BrahmiDocument26 pagesIntubasi Sulit: Nur Hajriya BrahmiFathiah HusainNo ratings yet
- Nutrition of Aging DogsDocument19 pagesNutrition of Aging DogsBrisbany AlcibarNo ratings yet
- Prostrolane Intra Articular en INGLESDocument6 pagesProstrolane Intra Articular en INGLESjuanNo ratings yet
- Defining The Practice of Medical TechnologyDocument13 pagesDefining The Practice of Medical TechnologyKenneth John Lloyd OrtizNo ratings yet
- The Paleopathology of Specific Infectious Diseases From Southeastern Hungary: A Brief OverviewDocument6 pagesThe Paleopathology of Specific Infectious Diseases From Southeastern Hungary: A Brief OverviewLucía Chavarría RíosNo ratings yet
- Fast Paces Academy - SymptomsDocument21 pagesFast Paces Academy - SymptomsAdil ShabbirNo ratings yet
- Attesta™ DR Mri Surescan™ Atdr01: Dual Chamber Rate Responsive Pacemaker (DDDR)Document42 pagesAttesta™ DR Mri Surescan™ Atdr01: Dual Chamber Rate Responsive Pacemaker (DDDR)mytake100No ratings yet
- Chapter 4 Communicable DiseaseDocument33 pagesChapter 4 Communicable DiseaseAyro Business CenterNo ratings yet
- Cardiovascular DiseaseDocument5 pagesCardiovascular DiseaseJohn SammutNo ratings yet
- Cognitive DisabilitiesDocument4 pagesCognitive Disabilitieshannalee13No ratings yet
- Instructions For Use: Home Sperm Test For Male FertilityDocument2 pagesInstructions For Use: Home Sperm Test For Male FertilityRAVAN ZJNo ratings yet
- 19 GVHDDocument3 pages19 GVHDdokutahNo ratings yet
- Chapter 026 CoagulationDocument7 pagesChapter 026 Coagulationthubtendrolma100% (3)
- TUBERCULOSISDocument16 pagesTUBERCULOSISfranciz CalagoNo ratings yet
- Role of CPAP in ICUDocument21 pagesRole of CPAP in ICUheriNo ratings yet
- MBBS - General Medicine Reg Id: KMC - 142105 RX ID: 406824261Document1 pageMBBS - General Medicine Reg Id: KMC - 142105 RX ID: 406824261Dipam HalderNo ratings yet
- Introduction To Epidemiology of Infection Diseases PDFDocument17 pagesIntroduction To Epidemiology of Infection Diseases PDFRovaidKhanNo ratings yet
- (Current Clinical Urology) Pat F. Fulgham, Bruce R. Gilbert (Eds.) - Practical Urological Ultrasound-Humana Press (2017) PDFDocument360 pages(Current Clinical Urology) Pat F. Fulgham, Bruce R. Gilbert (Eds.) - Practical Urological Ultrasound-Humana Press (2017) PDFIon VasianNo ratings yet
- Predictions Using Data Mining and Case Based Reasoning A Case Study For RetinopathyDocument4 pagesPredictions Using Data Mining and Case Based Reasoning A Case Study For RetinopathyBiraj kumar BholNo ratings yet
- Critical Care Nursing: An OverviewDocument64 pagesCritical Care Nursing: An OverviewProf. Ramsharan Mehta100% (2)
- Unit 4: Medical EmergenciesDocument44 pagesUnit 4: Medical EmergenciesMR々๛ AKMツNo ratings yet
- All Mycoses SGDDocument140 pagesAll Mycoses SGDkashan100% (1)
- Procedures in Obstetrics and Gynaecology TextbookDocument272 pagesProcedures in Obstetrics and Gynaecology TextbookPriyaNo ratings yet