Professional Documents
Culture Documents
Drug Development Essay
Uploaded by
Doyin AwodeleCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Drug Development Essay
Uploaded by
Doyin AwodeleCopyright:
Available Formats
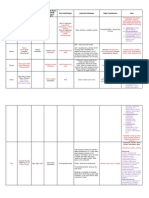
How are biotechnology medicines discovered and developed?
(AMGEN)
The first step in treating any disease is to clarify how the disease is caused. Many questions must be answered to arrive at an understanding of what is needed to pursue new types of treatments.
How does a person get the disease? Which cells are affected? Is the disease caused by genetic factors? If so, what genes are turned on or off in the diseased cells?
What proteins are present or absent in diseased cells as compared with healthy cells? If the disease is caused by an infection, how does the infectious organism interact with the body?
In modern labs, sophisticated tools are used for shedding light on these questions. The tools are designed to uncover the molecular roots of disease and pinpoint critical differences between healthy cells and diseased cells. Researchers often use multiple approaches to create a detailed picture of the disease process. Once the picture starts to emerge, it can still take years to learn which of the changes linked to a disease are most important. Is the change the result of the disease, or is the disease the result of the change? By determining which molecular defects are really behind a disease, scientists can identify the best targets for new medicines. In some cases, the best target for the disease may already be addressed by an existing medicine, and the aim would be to develop a new drug that offers other advantages. Often, though, drug discovery aims to provide an entirely new type of therapy by pursuing a novel target.
Selecting a target The term target refers to the specific molecule in the body that a medicine is designed to affect. For example, antibiotics target specific proteins that are not found in humans but are critical to the survival of bacteria. Many cholesterol drugs target enzymes that the body uses to make cholesterol.
Scientists estimate there are about 8,000 therapeutic targets that might provide a basis for new
medicines. Most are proteins of various types, including enzymes, growth factors, cell receptors, and cell-signaling molecules. Some targets are present in excess during disease, so the goal is to block their activity. This can be done by a medicine that binds to the target to prevent it from interacting with other molecules in the body. In other cases, the target protein is deficient or missing, and the goal is to enhance or replace it in order to restore healthy function. Biotechnology has made it possible to create therapies that are similar or identical to the complex molecules the body relies on to remain healthy.
The amazing complexity of human biology makes it a challenge to choose good targets. It can take many years of research and clinical trials to learn that a new target wont provide the desired results. To reduce that risk, scientists try to prove the value of targets through research experiments that show the targets role in the disease process. The goal is to show that the activity of the target is driving the course of the disease. Selecting a drug Once the target has been set, the next step is to identify a drug that impacts the target in the desired way. If researchers decide to use a chemical compound, a technology called drug screening is typically used. With automated systems, scientists can rapidly test thousands of compounds to see which ones interfere with the targets activity. Potent compounds can be put through added tests to find a lead compound with the best potential to become a drug. In contrast, biologics are designed using genetic engineering. If the goal is to provide a missing or deficient protein, the gene for that protein is used for making a recombinant version of the protein to give to patients. If the goal is to block the target protein with an antibody, one common approach is to expose transgenic mice to the target so as to induce their immune systems to make antibodies to that protein. The cells that produce these specific antibodies are then extracted and manipulated to create a new cell line. The mice used in this process are genetically modified to make human antibodies, which reduces the risk of allergic reactions in patients. Developing the drug Once a promising test drug has been identified, it must go through extensive testing before it can be studied in humans. Many drug safety studies are performed using cell lines engineered to
express the genes that are often responsible for side effects. Cell line models have decreased the number of animals needed for testing and have helped accelerate the drug development process. Some animal tests are still required to ensure that the drug doesnt interfere with the complex biological functions that are found only in higher life-forms.
If a test drug has no serious safety issues in preclinical studies, researchers can ask for regulatory permission to do clinical trials in humans. There are three phases of clinical research, and a drug must meet success criteria at each phase before moving on to the next one. Phase 1: Tests in 20 to 80 healthy volunteers and, sometimes, patients. The main goals are to assess safety and tolerability and explore how the drug behaves in the body (how long it stays in the body, how much of the drug reaches its target, etc.). Phase 2: Studies in about 100 to 300 patients. The goals are to evaluate whether the drug appears effective, to further explore its safety, and to determine the best dose.
Phase 3: Large studies involving 500 to 5,000 or more patients, depending on the disease and the study design. Very large trials are often needed to determine whether a drug can prevent bad health outcomes. The goal is to compare the effectiveness, safety, and tolerability of the test drug with another drug or a placebo. If the test drug shows clear benefits and acceptable risks in phase 3, the company can file an application requesting regulatory approval to market the drug. In the United States, the Food and Drug Administration evaluates new medicines. In the European Union, the European Medicines Agency manages that responsibility. Regulators review data from all studies and decide whether the medicines benefits outweigh any risks it may have. If the medicine is approved, regulators may still require a plan to reduce any risk to patients. A plan to monitor side effects in patients is also required. A company can continue doing clinical trials on an approved medicine to see if it works under other specific conditions or in other groups of patients, and additional trials may also be required by regulatory agencies. These are known as phase 4 studies. The whole drug development process takes 10 to 15 years to complete on average. Very few test drugs are able to clear all the hurdles along the way.
Why is it better to fail early?
Fail early, fail cheap is the goal. No company wants to discover a major problem after millions of dollars and years of research have been invested, once clinical trials are well under way as is the case with Rezulin ( Anti diabetic and anti inflammatory drug) (Varma-OBrien, S., 2009). Biotechnology companies have been attempting to decrease the technical uncertainty surrounding a product before it enters the expensive stages of development in particular Phases II and III, when there are significant costs associated with recruiting patients and monitoring them for extended periods.
Savings realised by avoiding late-stage R&D failures are re-invested in R&D to further enhance R&D productivity through work on candidate selection, first efficacy dose, first human dose, and product decision. Key to the quick win/fast fail approach is a feedback loop in which data gathered at the early proof of concept stage are fed back to discovery scientists for future benefit. Drug developers can remove some of the uncertainty in the outcomes of their research and improve their return on investment substantially. For example, demonstrating in the course of a year that a drug for Alzheimers does or does not alter the disease progression before it becomes symptomatic would produce savings over having to wait perhaps five years for the conclusion of a later-phase study.
What is the rationale for the high costs of medicines developed by Pharma?
Research and development costs vary widely from one new drug to the next. Those costs depend on the type of drug being developed, the likelihood of failure, and whether the drug is based on a molecule not used before in any pharmaceutical product (a new molecular entity, or NME) or instead is an incremental modification of an existing drug. A recent, widely circulated estimate put the average cost of developing an innovative new drug at more than $800 million, including expenditures on failed projects and the value of forgone alternative investments (Marron D.B, The Congress of the United States, 2006).
Clinical research is expensive. This is demonstrated by Phase I and II protocols. They experience the biggest annual growth in complexity and execution as more data is gathered in these earlier phases. Similarly, Phase IV is expensive as more post-marketing data is collected for safety and marketing purposes. But the main expense is failure. AstraZeneca does badly by this measure because it has had so few new drugs hit the market.
You might also like
- Diesel GensetDocument2 pagesDiesel Gensetvega f ankaNo ratings yet
- Drug Discovery Complete NotesDocument5 pagesDrug Discovery Complete NotesSadiqa ForensicNo ratings yet
- Sugar and Starch Specimens and Their Uses in Medicine and IndustryDocument12 pagesSugar and Starch Specimens and Their Uses in Medicine and IndustryGracelyn GatusNo ratings yet
- Case Study Myocardial InfarctionDocument23 pagesCase Study Myocardial InfarctionJester GalayNo ratings yet
- 6 Pharmacists in Public HealthDocument22 pages6 Pharmacists in Public HealthJoanna Carla Marmonejo Estorninos-Walker100% (1)
- Sheiko program training and FAQsDocument34 pagesSheiko program training and FAQsGiovan Maria Catalan BelmonteNo ratings yet
- Standard Patient Counseling ScriptDocument22 pagesStandard Patient Counseling ScriptElleason Joshua G. FranciscoNo ratings yet
- Pharm Care 4 Chapter 1Document25 pagesPharm Care 4 Chapter 1MaraNagaSambarani100% (1)
- CHAPTER 4 Helping Patients With Adherence and Decision Making CommskillsDocument5 pagesCHAPTER 4 Helping Patients With Adherence and Decision Making CommskillsKacie YsulatNo ratings yet
- (90-55-3000) BIOLIS 50i - Operator's M - V5.7 PDFDocument498 pages(90-55-3000) BIOLIS 50i - Operator's M - V5.7 PDFMatrix100% (1)
- Module 3: Hospital Pharmacy: Prepared By: Alexandra D. Atienza RPHDocument135 pagesModule 3: Hospital Pharmacy: Prepared By: Alexandra D. Atienza RPHJojo DelosreyesNo ratings yet
- (Dispensing 1 Laboratory) Review NotesDocument12 pages(Dispensing 1 Laboratory) Review NotesZen HeartNo ratings yet
- Exploratory Study of Self-Medication Practices Among StudentsDocument5 pagesExploratory Study of Self-Medication Practices Among StudentsN SNo ratings yet
- Nurse RetentionDocument9 pagesNurse Retentionapi-273066575No ratings yet
- Introduction To PharmacologyDocument2 pagesIntroduction To PharmacologyJoy Ann Akia PasigonNo ratings yet
- Masonry QuizDocument12 pagesMasonry QuizJoanne Jose Castro0% (1)
- Pharmacognosy Prelim ExperimentsDocument18 pagesPharmacognosy Prelim ExperimentsMello Diax100% (1)
- Trusted Quality Healthcare ExperienceDocument9 pagesTrusted Quality Healthcare ExperienceRuel Vincent AsubarNo ratings yet
- (PHA6129 LAB) PrescriptionDocument5 pages(PHA6129 LAB) PrescriptionNotfor TaoNo ratings yet
- Household Poisnous MaterialsDocument4 pagesHousehold Poisnous MaterialsTarfha AbduhalimNo ratings yet
- Activity No. 1: Name: - DateDocument3 pagesActivity No. 1: Name: - DateMauren Crestine Delos Santos0% (1)
- Eng Shs Mod3 EAPP Techniques v1 ForprintingDocument14 pagesEng Shs Mod3 EAPP Techniques v1 ForprintingJoshua Vernon AtipNo ratings yet
- APPLICATION PROJECT 3: Drug Procurement & Inventory Control Kaye Erin B. Nadonga PH 4-ADocument5 pagesAPPLICATION PROJECT 3: Drug Procurement & Inventory Control Kaye Erin B. Nadonga PH 4-APrincess TiongsonNo ratings yet
- 21 40Document6 pages21 40Ira YaoNo ratings yet
- Types and Classifications of Hospitals ExplainedDocument1 pageTypes and Classifications of Hospitals ExplainedKimberley Anne SeeNo ratings yet
- Bulk CompoundingDocument1 pageBulk Compoundingsamanchandravithanage4122No ratings yet
- Philippines Department of Health issues order on drug manufacturing practicesDocument11 pagesPhilippines Department of Health issues order on drug manufacturing practicesAisushiNo ratings yet
- COMPRE - MODULE 3 (Practice of Pharmacy) : Attempt ReviewDocument39 pagesCOMPRE - MODULE 3 (Practice of Pharmacy) : Attempt ReviewLance RafaelNo ratings yet
- MSPH 600 Ao 64 S. 1989 ReportDocument6 pagesMSPH 600 Ao 64 S. 1989 ReportShynne RPhNo ratings yet
- The Antibiotic Self-Medication Practices of Residents of Iloilo CityDocument17 pagesThe Antibiotic Self-Medication Practices of Residents of Iloilo CityLALANo ratings yet
- Bioethics Animal Paper PresentationDocument14 pagesBioethics Animal Paper Presentationtimar iaNo ratings yet
- Prescriptions Labelling Latin Terms FA 20120222Document24 pagesPrescriptions Labelling Latin Terms FA 20120222SherazButtNo ratings yet
- Intro Drug DiscoveryDocument32 pagesIntro Drug Discoveryapi-19965961No ratings yet
- B Pharmaceutical ChemistryDocument29 pagesB Pharmaceutical ChemistryZllison Mae Teodoro MangabatNo ratings yet
- Wine Production ProcessDocument2 pagesWine Production ProcessJanice Malafu De GuiaNo ratings yet
- Physicochemical IncompatibilitiesDocument20 pagesPhysicochemical Incompatibilitiesvicbart11No ratings yet
- Chapter 8 PLACE MIX Decisions and StrategiesDocument2 pagesChapter 8 PLACE MIX Decisions and StrategiesAel Xyandreiz LacsonNo ratings yet
- Philippine Pharmacy ActDocument63 pagesPhilippine Pharmacy ActpsyarjavierNo ratings yet
- Dispensing ChecklistDocument2 pagesDispensing Checklistsafia321No ratings yet
- Hospital pharmacy journal insightsDocument7 pagesHospital pharmacy journal insightsMa Victoria ChuaNo ratings yet
- Appendix C2 Cover Letter ASUBARDocument2 pagesAppendix C2 Cover Letter ASUBARRuel Vincent AsubarNo ratings yet
- CPM18th Allergic RhinitisDocument10 pagesCPM18th Allergic RhinitisMa Katherina ArellanoNo ratings yet
- Lab Activity #1Document5 pagesLab Activity #1Meg Angela Cirunay-Decena0% (1)
- Mobile Apps for Pharmacy InformationDocument3 pagesMobile Apps for Pharmacy InformationJannah Grace VergaraNo ratings yet
- Pharmaceutical BotanyDocument5 pagesPharmaceutical BotanyCyril CathercoleNo ratings yet
- Nica Chua - Hospital Pharmacy Internship Daily Activity Report-Day 27 MajorDocument3 pagesNica Chua - Hospital Pharmacy Internship Daily Activity Report-Day 27 MajorMa Victoria ChuaNo ratings yet
- Allergy: DR Panini Patankar Guide: DR Shirish JoshiDocument53 pagesAllergy: DR Panini Patankar Guide: DR Shirish JoshiPanini PatankarNo ratings yet
- 1 Herbs and Health ProductsDocument29 pages1 Herbs and Health ProductsanavyaledzurcNo ratings yet
- 2 Public Health For Primary Health CareDocument32 pages2 Public Health For Primary Health CarehervwNo ratings yet
- Unit 1: Introduction: Intended Learning OutcomesDocument7 pagesUnit 1: Introduction: Intended Learning Outcomesalibel caballeroNo ratings yet
- Unit Operations in Secondary ManufacturingDocument11 pagesUnit Operations in Secondary ManufacturingJoyce Marian BelonguelNo ratings yet
- Toxicology Course Outline - CompletedDocument4 pagesToxicology Course Outline - Completedtpetronellah mandishona100% (1)
- Internship5 12Document7 pagesInternship5 12Jerel MarquezNo ratings yet
- Patient Medication ProfileDocument4 pagesPatient Medication ProfileLaura HernandezNo ratings yet
- Superintendent and Supervising Pharmacists Guidance On RolesDocument3 pagesSuperintendent and Supervising Pharmacists Guidance On RolessefrounfNo ratings yet
- Activity 7 DISPENSING PRICE With AnswersDocument3 pagesActivity 7 DISPENSING PRICE With AnswersChristine DelmendoNo ratings yet
- Modified Systematic Approach To Answering QuestionsDocument5 pagesModified Systematic Approach To Answering QuestionsromeofatimaNo ratings yet
- Statement of Principle Self-Care Including Self-Medication - The Professional Role of The PharmacistDocument5 pagesStatement of Principle Self-Care Including Self-Medication - The Professional Role of The PharmacistAprilia R. Permatasari0% (1)
- Lecture-9: Components of Therapeutics Planning ProcessDocument19 pagesLecture-9: Components of Therapeutics Planning ProcessLayla100% (1)
- JURIS Laws PDFDocument3 pagesJURIS Laws PDFuypaul97No ratings yet
- Lower Urinary Tract Infection GuideDocument4 pagesLower Urinary Tract Infection GuideReen ChavezNo ratings yet
- Hospital and Its OrganizationsDocument11 pagesHospital and Its Organizationssaloni patel100% (1)
- Notes in PharmacologyDocument95 pagesNotes in PharmacologyMylz MendozaNo ratings yet
- Mechanisms of Drug Toxicity: Proceedings of the Third International Pharmacological MeetingFrom EverandMechanisms of Drug Toxicity: Proceedings of the Third International Pharmacological MeetingH. RaškováNo ratings yet
- FDA Drug Development ProcessDocument96 pagesFDA Drug Development ProcessSheena GagarinNo ratings yet
- CBR A Drug DevelopDocument2 pagesCBR A Drug DevelopAlfieNo ratings yet
- ImagesDocument2 pagesImagesDoyin AwodeleNo ratings yet
- 4th SC Phar 40060-Renal-2webDocument24 pages4th SC Phar 40060-Renal-2webDoyin AwodeleNo ratings yet
- Science ReviewDocument10 pagesScience ReviewDoyin AwodeleNo ratings yet
- 13 Lecture2 RD-AMD TherapiesDocument15 pages13 Lecture2 RD-AMD TherapiesDoyin AwodeleNo ratings yet
- StatDocument10 pagesStatDoyin AwodeleNo ratings yet
- Gli Co Protein ADocument40 pagesGli Co Protein AOmar Cruz BadilloNo ratings yet
- Science 284, 1322Document7 pagesScience 284, 1322Doyin AwodeleNo ratings yet
- StatDocument10 pagesStatDoyin AwodeleNo ratings yet
- Ramsey Et Al 2011Document10 pagesRamsey Et Al 2011Doyin AwodeleNo ratings yet
- Technical Logical Exam AnswersDocument6 pagesTechnical Logical Exam AnswersDoyin AwodeleNo ratings yet
- TypeII Secretion and PathogenesisDocument13 pagesTypeII Secretion and PathogenesisDoyin AwodeleNo ratings yet
- Yersinia PestisDocument6 pagesYersinia PestisDoyin AwodeleNo ratings yet
- Putative AD Wit Fast OnsetDocument9 pagesPutative AD Wit Fast OnsetDoyin AwodeleNo ratings yet
- New Developments in Antidepressant TherapyDocument5 pagesNew Developments in Antidepressant TherapyDoyin AwodeleNo ratings yet
- Cassidy Et Al., 2010 - Reelin PFCDocument10 pagesCassidy Et Al., 2010 - Reelin PFCDoyin AwodeleNo ratings yet
- Chemokine ReviewDocument6 pagesChemokine ReviewDoyin AwodeleNo ratings yet
- Guidelines For Submitting Online Applications - Research PostsDocument4 pagesGuidelines For Submitting Online Applications - Research PostsDoyin AwodeleNo ratings yet
- Science ReviewDocument10 pagesScience ReviewDoyin AwodeleNo ratings yet
- Fluoxetine TreatmentDocument6 pagesFluoxetine TreatmentDoyin AwodeleNo ratings yet
- Englehardt Et AlDocument10 pagesEnglehardt Et AlDoyin AwodeleNo ratings yet
- BDNF TraffikingDocument11 pagesBDNF TraffikingDoyin AwodeleNo ratings yet
- John Cryan PaperDocument8 pagesJohn Cryan PaperDoyin AwodeleNo ratings yet
- Teaching Assistant Life Sciences 10 Month ContractDocument1 pageTeaching Assistant Life Sciences 10 Month ContractDoyin AwodeleNo ratings yet
- Scully Et Al., 2012 - D-VDocument10 pagesScully Et Al., 2012 - D-VDoyin AwodeleNo ratings yet
- Weiberg Review Cell PDFDocument29 pagesWeiberg Review Cell PDFThyago CardimNo ratings yet
- Ketamine Induced Release of BDNFDocument5 pagesKetamine Induced Release of BDNFDoyin AwodeleNo ratings yet
- Onset of ActionDocument13 pagesOnset of ActionDoyin AwodeleNo ratings yet
- It Sligo Careers Office Covering Letter Information SheetDocument1 pageIt Sligo Careers Office Covering Letter Information SheetDoyin AwodeleNo ratings yet
- عقد الحج - ENGLISH 2012Document8 pagesعقد الحج - ENGLISH 2012Doyin AwodeleNo ratings yet
- Lakshmanarishtam - YogamruthamDocument6 pagesLakshmanarishtam - YogamruthamRahul KirkNo ratings yet
- Nursing Care PlanDocument3 pagesNursing Care PlanMarielle SorianoNo ratings yet
- Ujjwala Saga PDFDocument84 pagesUjjwala Saga PDFRishi ModiNo ratings yet
- Cholesteatoma and Congenital Cholesteatoma Important PointsDocument6 pagesCholesteatoma and Congenital Cholesteatoma Important PointsSuprit Sn100% (1)
- Isak 1 2 ViennaDocument6 pagesIsak 1 2 Viennanifej15595No ratings yet
- DelegationDocument24 pagesDelegationJP FernandezNo ratings yet
- Team Performance ModelDocument17 pagesTeam Performance ModelAdewumi Samson Segun100% (1)
- Principles of Eye Management in Stevens-Johnson Syndrome: Mittanamalli S. SridharDocument5 pagesPrinciples of Eye Management in Stevens-Johnson Syndrome: Mittanamalli S. SridharFarah RNo ratings yet
- BoltonDocument26 pagesBoltonDryashpal SinghNo ratings yet
- Classic Series Price List Effective February 2023Document1 pageClassic Series Price List Effective February 2023Yusuf Patria SandiNo ratings yet
- Good Governance IndexDocument112 pagesGood Governance IndexWilliam ObengNo ratings yet
- Therapeutic Communication: Prepared By: Mark Angelo C. Collado Kenneth Carl C. Roque Janella Rose Y. SusaDocument15 pagesTherapeutic Communication: Prepared By: Mark Angelo C. Collado Kenneth Carl C. Roque Janella Rose Y. SusaNashNo ratings yet
- Ward D - Freida McFaddenDocument239 pagesWard D - Freida McFaddenHassan ZayanNo ratings yet
- Discussion of Dr. John Bowlby's PaperDocument11 pagesDiscussion of Dr. John Bowlby's PaperFrancisCevallosNo ratings yet
- How To Conduct A Mock Recall NelsonDocument18 pagesHow To Conduct A Mock Recall Nelsonelmalo100% (1)
- Full Download Test Bank For Pharmacology 9th Edition by Mccuistion PDF Full ChapterDocument36 pagesFull Download Test Bank For Pharmacology 9th Edition by Mccuistion PDF Full Chapterpotshardmonied5cuc100% (19)
- Improving Workplace Safety Behavioral Based Safety: ThroughDocument32 pagesImproving Workplace Safety Behavioral Based Safety: ThroughYursNo ratings yet
- PAws Samsha PDFDocument8 pagesPAws Samsha PDFAnonymous JS9PXY2100% (1)
- Patient Confidentiality Part BDocument6 pagesPatient Confidentiality Part BSojiNo ratings yet
- Truvivity by NutriliteDocument10 pagesTruvivity by Nutriliteโยอันนา ยุนอา แคทเธอรีน เอี่ยมสุวรรณNo ratings yet
- Exploratory Data Analysis of Electric Tricycle AsDocument13 pagesExploratory Data Analysis of Electric Tricycle AsNiño E. EvangelioNo ratings yet
- # Category Image Product Name Producer Package Hs Code Remark Key FeaturesDocument9 pages# Category Image Product Name Producer Package Hs Code Remark Key Featuresiq_dianaNo ratings yet
- Geog 102 Topic 3Document41 pagesGeog 102 Topic 3Nikolamladenovac9No ratings yet
- Comm 602 Assignment 1Document4 pagesComm 602 Assignment 1hamiltjw2No ratings yet