Professional Documents
Culture Documents
Nursing Care Plan The Child With A Major Burn Injury
Uploaded by
Pamela Soledad Delgado SuárezOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nursing Care Plan The Child With A Major Burn Injury
Uploaded by
Pamela Soledad Delgado SuárezCopyright:
Available Formats
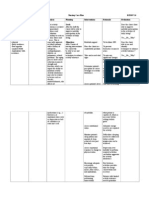
NURSING CARE PLAN
GOAL 1. Pain related to physical injury agents
The Child with a Major Bur n Injury
RATIONALE EXPECTED OUTCOME
INTERVENTION
NIC Priority Intervention: Pain Management: Alleviation of pain or a reduction in pain to a level of comfort that is acceptable to the patient. The child will verbalize adequate relief from pain and will be able to perform activities of daily living (ADLs).
NOC Suggested Outcome: Comfort Level: Feelings of physical and psychological ease.
Assess the level of pain frequently using pain scales (see Chapter 9).
Pain scale provides objective measurement. Pain is always present, but changes location; intensity may indicate complications. Temperature changes or movement of air causes pain. Reduces joint stiffness and prevents contractures. Provides outlet for emotions and helps the child cope. Helps lessen focus on pain. Sleep deprivation can increase pain perception. Helps to reduce pain and decreases anxiety for subsequent dressing changes.
The child verbalizes adequate relief from pain and is able to perform ADLs.
Cover burns as much as possible. Change the childs position frequently. Perform range-ofmotion exercises. Encourage verbalization about pain. Provide diversional activities. Promote uninterrupted sleep with use of medications. Use analgesics before all dressing changes and burn care.
2. Risk for Infection related to trauma and destruction of skin barrier NIC Priority Intervention: Infection Protection: Prevention and early detection of infection in a patient at risk. The child will be free of infection during healing process.
NOC Suggested Outcome: Risk Control: Actions to eliminate or reduce actual, personal, and modifiable health threats.
Take vital signs frequently. Use standard precautions (gown, gloves, mask) when wounds of a major burn are exposed. Limit visitors (no one with an upper respiratory infection or other contagious disease). Clip hair around burns. Keep biosynthetic burn dressing dry. Do not place the IV in any burned area. Administer oral or IV antibiotics for diagnosed infections as prescribed.
Increased temperature is an early sign of infection. Reduces risk of wound contamination.
The child either stays free of secondary infection, or has infection diagnosed and treated early.
Hair harbors bacteria. Helps reduce the number of bacteria introduced to the burn site. Reduces risk of wound contamination. Antibiotics administered as prescribed help to clear the infection quickly.
3. Risk for Fluid Volume Imbalance related to loss of fluids through wounds and to subsequent excess fluid intake NIC Priority Intervention: To be developed. The child will maintain adequate urine output.
NOC Suggested Outcome: To be developed.
Monitor vital signs, central venous pressure, capillary refill time, pulses.
The child is initially at risk for hypovolemic shock and needs fluid resuscitation (see Chapter 10).
The child maintains normal urine output and burn site edema is not excessive. (continued)
NURSING CARE PLAN
GOAL
The Child with a Major Burn Injury
RATIONALE
(continued)
INTERVENTION
EXPECTED OUTCOME
3. Risk for Fluid Volume Imbalance related to loss of fluids through wounds and to subsequent excess fluid intake (continued)
Administer IV and oral fluids as ordered. Estimate insensible fluid losses.
Careful calculation of fluid needs and ensuring proper intake help keep the child properly hydrated. Losses are increased during the first 72 hours after burn injury; may need replacement. Plasma is lost through burn site because of capillary damage. The child is at risk for fluid overload during hydration, and for edema in the tissues at the burn site. Significant weight loss or gain can help determine fluid imbalances. Helps maintain accurate output measurement during critical care stage. Sodium is lost with burn fluid and potassium is lost from damaged cells, causing electrolyte imbalances.
Monitor intake and output.
Weigh child daily. Insert urinary catheter.
Monitor for hyponatremia and hypercalcemia (see Chapter 10).
4. Altered Peripheral Tissue Perfusion related to mechanical reduction of venous and/or arterial blood flow (edema) of circumferential burns NIC Priority Intervention: Circulatory Care: Promotion of arterial and venous circulation. NOC Suggested Outcome: Tissue Perfusion (Peripheral): Extent to which blood flows through the small vessels of the extremities and maintains tissue function.
The child will maintain adequate perfusion in burned extremities.
Elevate extremities. Perform hourly distal pulse checks. Notify the physician of decreased or absent pulses. Check eschar.
Elevation helps to reduce dependent edema by promoting venous return. Dependent edema can constrict peripheral circulation. Eschar can constrict peripheral circulation in edematous extremity.
The child has no episodes of poor perfusion in the burned extremity.
5. Ineffective Breathing Pattern related to respiratory muscle fatigue due to smoke inhalation and airway edema NIC Priority Intervention: Respiratory Monitoring: Collection and analysis of patient data to ensure airway patency and adequate gas exchange. The child will maintain or demonstrate improvement in breathing pattern.
NOC Suggested Outcome: Vital Signs Status: Temperature, pulse, respiration, and blood pressure within expected range for the individual.
Closely monitor quality of respirations, breath sounds, mucous secretions, pulse oximetry. Provide thorough pulmonary care. Elevate head of bed. Keep intubation tube at bedside. Administer corticosteroids, as prescribed.
Excess fluid replacement can cause pulmonary edema; toxins from burning products can cause airway inflammation. Pulmonary care assists in removal of secretions to prevent infection. Dyspnea, nasal flaring, air hunger (respiratory distress) may develop. Reduces airway edema.
The child has regular and unlabored breathing pattern.
6. Impaired Physical Mobility related to joint stiffness due to burns NIC Priority Intervention: Exercise Therapy, Joint Mobility: Use of active or passive body movement to maintain or restore joint flexibility. NOC Suggested Outcome: Joint Movement (Active): Range of motion of joints with self-initiated movement.
NURSING CARE PLAN
GOAL The child will maintain maximum range of motion.
Alterations in Skin Integrity 895 The Child with a Major Burn Injury (continued)
RATIONALE
INTERVENTION Arrange physical and occupational therapy twice daily for stretching and range-of-motion exercises. Splint as ordered. Encourage independent ADLs.
EXPECTED OUTCOME The child maintains maximum range of motion without contractures.
Good positioning, range-of-motion exercises, and alignment prevent contractures.
7. Altered Nutrition: Less than Body Requirements related to high metabolic needs NIC Priority Intervention: Nutrition Management: Assistance with or provision of balance dietary intake of foods and fluids. The child will maintain weight and demonstrate adequate serum albumin and hydration.
NOC Suggested Outcome: Nutritional Status: Extent to which nutrients are available to meet metabolic needs.
Provide an opportunity to choose meals. Offer a variety of foods. Provide snacks. Encourage the child to have meals with other children. Provide a multivitamin supplement. Substitute milk and juices for water. Provide nasogastric feedings as needed. Weigh the child daily.
Encourages intake. General malaise and anorexia lead to poor healing. Socialization improves intake. Vitamin C aids zinc absorption; zinc aids in healing. A child with a burn greater than 10% of BSA cannot usually meet nutrition requirements without assistance. Provides objective evaluation.
The child maintains weight, adequate hydration, normal serum albumin.
8. Anxiety (Child) related to threat to or change in health status NIC Priority Intervention: Anxiety Reduction: Minimizing apprehension, dread, foreboding, or uneasiness related to an unidentified source of anticipated danger. The child will verbalize reduced anxiety.
NOC Suggested Outcome: Coping: Actions to manage stressors that tax an individuals resources.
Provide continuity of care providers. Encourage parents to stay with the child; calls from home; pictures from classmates. Group tasks and activities.
Helps to build a trusting relationship. Familiar surroundings, people, and items encourage relaxation. Reduces overstimulation and encourages rest.
The child expresses and shows signs of reduced anxiety.
9. Anxiety (Parent) related to situational crisis NIC Priority Intervention: Anxiety Reduction: Minimizing apprehension, dread, foreboding, or uneasiness related to an unidentified source of anticipated danger. Parents will verbalize decreased anxiety.
NOC Suggested Outcome: Anxiety Control: Ability to eliminate or reduce feelings of apprehension and tension from an unidentified source.
Provide educational materials about healing, grafting, dressing changes, and course of action. Be flexible when teaching parents about wound care. Provide referral to social services or parent support group
Knowledge reduces anxiety.
Parents state decreased anxiety.
Adults learn in many different ways. Allows for venting of fears and guilt feelings, and provides exchange of ideas on dealing with hospitalization and long-term care.
You might also like
- Child - Major Burn PDFDocument3 pagesChild - Major Burn PDFAldith GrahamNo ratings yet
- Nursing Management HydrocephalusDocument4 pagesNursing Management HydrocephalusPrecious Mae Benologa100% (1)
- Post Assessment PediatricsDocument4 pagesPost Assessment Pediatricscuicuita100% (4)
- Icu ReqDocument9 pagesIcu Reqzygote_23100% (1)
- Pediatric RemediationDocument5 pagesPediatric RemediationAlvin L. Rozier67% (3)
- Nursing Care Plan FeverDocument9 pagesNursing Care Plan FeverVincent Quitoriano85% (47)
- DiagnosisDocument12 pagesDiagnosisHCX dghhqNo ratings yet
- Nursing Management of PatientDocument32 pagesNursing Management of PatientNoky KiaNo ratings yet
- Nursing Care of at Risk/ High Risk/ Sick ClientDocument256 pagesNursing Care of at Risk/ High Risk/ Sick ClientAaron ConstantinoNo ratings yet
- HIGH RISK INFANT (1 Month - 12 Months) : 1. Failure To ThriveDocument14 pagesHIGH RISK INFANT (1 Month - 12 Months) : 1. Failure To ThriveRosaree Mae PantojaNo ratings yet
- Altered Level of Consciousness (LOC)Document28 pagesAltered Level of Consciousness (LOC)snowflakes21No ratings yet
- Child - Otitis MediaDocument2 pagesChild - Otitis MediawanyaminNo ratings yet
- HydrocephalusDocument22 pagesHydrocephalusyen1988No ratings yet
- Child Bronchiolitis 1Document2 pagesChild Bronchiolitis 1sarooah1994100% (2)
- NCPDocument17 pagesNCPShayne Jessemae AlmarioNo ratings yet
- Postnatal CareDocument19 pagesPostnatal Carejomarie gamiao0% (1)
- Ov Ov OvDocument15 pagesOv Ov OvHayyana Mae Taguba LadiaNo ratings yet
- NCPDocument8 pagesNCPJose Benit DelacruzNo ratings yet
- Assessment and Diagnostic FindingsDocument7 pagesAssessment and Diagnostic FindingsAlmustapha Babangida DanganiNo ratings yet
- Nursing Bullets 4Document12 pagesNursing Bullets 4kate annNo ratings yet
- The Use of ThrombolyticsDocument9 pagesThe Use of ThrombolyticsNestleNo ratings yet
- Maternal ATIDocument6 pagesMaternal ATIGeorgeNo ratings yet
- Christ John S. Pajarillaga BSN Iv - Block 13Document5 pagesChrist John S. Pajarillaga BSN Iv - Block 13Cj PajarillagaNo ratings yet
- 1) Nursing Careplan For FeverDocument9 pages1) Nursing Careplan For FeverY. Beatrice AbigailNo ratings yet
- Nursing Outline and Discharge PlanningDocument3 pagesNursing Outline and Discharge PlanningEugene Gian-Mendro Alcoseba ZabateNo ratings yet
- Andal - Pharma Other OrgansDocument6 pagesAndal - Pharma Other OrgansCarlos Miguel AndalNo ratings yet
- Uworld & Kaplan Nclex RN CardsDocument19 pagesUworld & Kaplan Nclex RN CardsOlgaK100% (1)
- Poisoning, DrowningDocument24 pagesPoisoning, DrowningThilaga RamNo ratings yet
- NCP Icu-CcuDocument6 pagesNCP Icu-CcuJohn CenasNo ratings yet
- Flaccid BladderDocument29 pagesFlaccid BladderphotosaurusrapNo ratings yet
- CVA Nursing Management BANGDocument4 pagesCVA Nursing Management BANGAna Louise BatallaNo ratings yet
- Trauma in Children. Initial Assessment and ManagementDocument39 pagesTrauma in Children. Initial Assessment and ManagementDrTushar GoswamiNo ratings yet
- Nursing Care PlanDocument23 pagesNursing Care PlanLorielle HernandezNo ratings yet
- NCP CSDocument9 pagesNCP CSFreida Marie PiczonNo ratings yet
- Surgical ManagementDocument3 pagesSurgical ManagementTiffany AdriasNo ratings yet
- ReportDocument4 pagesReportKyle DapulagNo ratings yet
- Care of Sick ChildDocument38 pagesCare of Sick ChildahmedNo ratings yet
- Diarrhea Drug StudyDocument12 pagesDiarrhea Drug StudyCeelin Robles0% (1)
- Management of Dengue Hemorrhagic FeverDocument7 pagesManagement of Dengue Hemorrhagic FeverjoycevillamorNo ratings yet
- New Born NCPDocument8 pagesNew Born NCPCarl Vincent Marrion Rejuso100% (1)
- Diagno SIS Planni NG Intervention Rationale Evaluati ONDocument3 pagesDiagno SIS Planni NG Intervention Rationale Evaluati ONAnn Nicole G. NeriNo ratings yet
- Cap NCPDocument6 pagesCap NCPMarlo Parayno100% (2)
- LCPDDocument7 pagesLCPDakoismeNo ratings yet
- Peds HESI Dec 2018 PDFDocument11 pagesPeds HESI Dec 2018 PDFMariya ZafraniNo ratings yet
- Nursing Care Plan For Master Shyne With AllDocument17 pagesNursing Care Plan For Master Shyne With AllsreekalaNo ratings yet
- Nursing Care PneumoniaDocument26 pagesNursing Care PneumoniaIsaac Kipkemoi100% (1)
- Managing Birth Asphyxia August 2022Document21 pagesManaging Birth Asphyxia August 2022f.abrahamNo ratings yet
- Drug StudyDocument17 pagesDrug Studyjlg513No ratings yet
- Select All That ApplyDocument10 pagesSelect All That ApplyJohnasse Sebastian NavalNo ratings yet
- Nursing Intervention (Oncology)Document3 pagesNursing Intervention (Oncology)Gibe BebitaNo ratings yet
- IVH Prevention Guidleines1Document3 pagesIVH Prevention Guidleines1YogeshRavalNo ratings yet
- Scope of Practice and Roles and ResponsibilitDocument3 pagesScope of Practice and Roles and ResponsibilitshaNo ratings yet
- NSG 1405 Care PlansDocument3 pagesNSG 1405 Care PlansAshley CyriacNo ratings yet
- MCN LECTURE Final Coaching 2223Document37 pagesMCN LECTURE Final Coaching 22239tfvnv4ghzNo ratings yet
- Neonatal Danger SignsDocument6 pagesNeonatal Danger Signsmarkus_danusantosoNo ratings yet
- Checklist For Student Newborn CareDocument7 pagesChecklist For Student Newborn CarePrecious SorianoNo ratings yet
- Presentation1 Sick ChildDocument29 pagesPresentation1 Sick Childsyed askariNo ratings yet
- Presentation 3Document15 pagesPresentation 3judii01No ratings yet
- Dental Management of the Pregnant PatientFrom EverandDental Management of the Pregnant PatientChristos A. SkouterisNo ratings yet
- Basic Life Support (BLS) Provider HandbookFrom EverandBasic Life Support (BLS) Provider HandbookRating: 5 out of 5 stars5/5 (2)
- Pulmonary EdemaDocument47 pagesPulmonary Edemamaeliszxc kimNo ratings yet
- SbarDocument3 pagesSbarCharlie65129No ratings yet
- Sindrome Nefrotico - Etiology, Clinical Manifestations, and Diagnosis of Nephrotic Syndrome in ChildrenDocument13 pagesSindrome Nefrotico - Etiology, Clinical Manifestations, and Diagnosis of Nephrotic Syndrome in ChildrenAiled HerediaNo ratings yet
- Fetal AnasarcaDocument7 pagesFetal Anasarcaraviks34No ratings yet
- Acute Pulmonary OdemaDocument9 pagesAcute Pulmonary OdemaAnonymous ysrxggk21cNo ratings yet
- 212 Cupping Proof PDFDocument7 pages212 Cupping Proof PDFWilyanto YangNo ratings yet
- 8 Goat Diseases Basics Part 1Document1 page8 Goat Diseases Basics Part 1Ramesh BeniwalNo ratings yet
- Chemotherapy Side Effects WorksheetDocument6 pagesChemotherapy Side Effects Worksheetreny hartikasariNo ratings yet
- Acute Glomerulonephritis - AGN - Nursing Care PlanDocument2 pagesAcute Glomerulonephritis - AGN - Nursing Care PlanCyrus De Asis80% (10)
- Nursing Care Plan of Mr. B: A Patient With CardiomegalyDocument12 pagesNursing Care Plan of Mr. B: A Patient With CardiomegalyWindasariNo ratings yet
- H. Pathophysiology I. Definition of Diagnosis A) Pregnancy Induced HypertensionDocument9 pagesH. Pathophysiology I. Definition of Diagnosis A) Pregnancy Induced HypertensionEmmy Flor ValmoriaNo ratings yet
- Lymphatic System N Body DefenseDocument23 pagesLymphatic System N Body Defensehafiz amriNo ratings yet
- Maintaining Fluid & Electrolyte Balance in The BodyDocument124 pagesMaintaining Fluid & Electrolyte Balance in The BodyKingJayson Pacman06100% (1)
- Human Anatomy Chapter 26Document10 pagesHuman Anatomy Chapter 26jinni0926No ratings yet
- Burn InjuryDocument59 pagesBurn Injuryvina zulfianiNo ratings yet
- Ethics For The Information Age 7th Edition Quinn Solutions ManualDocument34 pagesEthics For The Information Age 7th Edition Quinn Solutions Manualoutcourt.unownedqagy100% (35)
- 2023 MayDocument36 pages2023 MayReshma Shaji PnsNo ratings yet
- Jasmin Bernadette Villaver - PRELIMINARY TERM EXAM PMLS 2 (LAB)Document12 pagesJasmin Bernadette Villaver - PRELIMINARY TERM EXAM PMLS 2 (LAB)Frankenstein MelancholyNo ratings yet
- Greeshma Rhutu 2012 English PDFDocument16 pagesGreeshma Rhutu 2012 English PDFAjayAsthanaNo ratings yet
- Hypothyroidism Type 2 - The Epid - Mark Starr MD-lin PDFDocument280 pagesHypothyroidism Type 2 - The Epid - Mark Starr MD-lin PDFLi Lin100% (3)
- Test Bank For Comprehensive Radiographic Pathology 7th Edition Ronald Eisenberg Nancy JohnsonDocument15 pagesTest Bank For Comprehensive Radiographic Pathology 7th Edition Ronald Eisenberg Nancy JohnsonJames Cunningham100% (33)
- 533 Module 2 Fluid Electrolyte Disorders Acid Base QuizDocument7 pages533 Module 2 Fluid Electrolyte Disorders Acid Base QuizSara FNo ratings yet
- This Study Resource WasDocument3 pagesThis Study Resource WasCarlito AglipayNo ratings yet
- The Problem Oriented Medical Record: (Pomr or Povmr)Document27 pagesThe Problem Oriented Medical Record: (Pomr or Povmr)04lubna_869632400No ratings yet
- Problem-Oriented Medical Diagnosis 7thDocument228 pagesProblem-Oriented Medical Diagnosis 7thnhtoan3286% (7)
- Diane Kazer Loving On Our LymphDocument22 pagesDiane Kazer Loving On Our LymphKátia BárbaraNo ratings yet
- J.H. Cerilles State CollegeDocument5 pagesJ.H. Cerilles State Collegeyamie sulongNo ratings yet
- MalariaDocument9 pagesMalariaNitesh Bhura100% (5)
- 15.chronic - Venous - Insufficeincy (Sukrita 22.8.60)Document17 pages15.chronic - Venous - Insufficeincy (Sukrita 22.8.60)Juli VlogNo ratings yet
- An Approach To A Child With OedemaDocument14 pagesAn Approach To A Child With OedemaAdlina PutriantiNo ratings yet